Abstract
Because of the extensile nature and familiarity of the standard posterior-lateral approach to the hip, a family of “micro-posterior” approaches has been developed. This family includes the Percutaneously-Assisted Total Hip (PATH) approach, the Supercapsular (SuperCap) approach and a newer hybrid approach, the Supercapsular Percutaneously-Assisted Total Hip (SuperPATH) approach. Such approaches should ideally provide a continuum for the surgeon: from a “micro” (external rotator sparing) posterior approach, to a “mini” (external rotator sacrificing) posterior approach, to a standard posterior approach. This could keep a surgeon within his comfort zone during the learning curve of the procedure, while leaving options for complicated reconstructions for the more practiced micro-posterior surgeons. This paper details one author’s experiences utilizing this combined approach, as well as permutations of this entire micro-posterior family of approaches as applied to more complex hip reconstructions.
Keywords: SuperPATH, PATH, SuperCap, Micro-superior, Hip, Total, Arthroplasty, Minimally-invasive, Micro-posterior, Micro-invasive, Replacement, Percutaneous, Assisted, Direct-posterior, Direct
Introduction
Multiple minimally-invasive approaches have been described in an effort to improve short-term results of total hip arthroplasty (THA). Despite the success of such approaches, many minimally-invasive options may present with specific associated complications or shortcomings. Depending on the approach, these may include: peri-prosthetic fractures, trochanteric fractures, component malposition, implant selection restrictions, dislocations, gait alterations, bleeding, expensive equipment, extended learning-curves and lack of extensibility of the approach [1•, 2–23].
A family of “micro-posterior” approaches has been developed in an attempt to address these shortcomings [24••, 25, 26, 27••, 28••, 29••]. Because of the extensile nature and familiarity of the standard posterior-lateral approach to the hip, efforts have been made to utilize this approach in a muscle-sparing fashion. Additional special attention has been directed to preserving external-rotator musculature, the prime soft-tissue restraint to posterior dislocation. Such an approach would ideally provide a continuum from a “micro” (external rotator sparing) posterior approach, to a “mini” (external rotator sacrificing) posterior approach, to a standard posterior approach. This could keep a surgeon within his comfort zone during the learning curve of the procedure, while leaving options for complicated reconstructions for the more practiced micro-posterior surgeons.
One such micro-posterior technique, the Percutaneously-Assisted Total Hip (“PATH”, Wright Medical Technology, Inc.—Memphis, TN) approach, created by Dr. Brad Penenberg, utilizes the interval between the gluteus medius and the conjoined tendon of the external rotators to perform a THA. The piriformis is released from the greater trochanter to create this window, and the hip is dislocated through a capsular flap to expose the femur for femoral preparation. The femur is prepared in standard fashion. Depth of the broach is measured from the greater trochanter, since the lesser trochanter is not readily accessible without further dissection. Using specialized retractors, the femoral neck osteotomy creates the space necessary to prepare the acetabulum. This is done with the assistance of an accessory percutaneous portal, through which power and impaction tools are introduced to be assembled inside the acetabular cup for preparation and implantation.
Another technique, the Supercapsular (“SuperCap”, Wright Medical Technology, Inc.—Memphis, TN) approach, created by Dr. Stephen Murphy, utilizes a similar interval to gain access to the femur. In order to reduce potential dissection caused by the dislocation maneuver used in the posterior approach, the femur is prepared in-situ, leaving the patient’s leg resting on a Mayo stand for the entire procedure. To do this, the capsular incision is moved slightly superiorly, providing a “micro-superior” access to the joint space. The superior femoral neck is “canoed out” to allow for passing of the femoral broaches. Much like PATH, depth of the broach is measured from the greater trochanter. The final broach is then left in place and is used as an internal cutting guide to fashion the femoral neck osteotomy. The native head is removed from the intra-articular space and the acetabulum is fashioned through the incision utilizing specialized reamers and impactors. No accessory portal is used.
The PATH and SuperCap approaches each have had over 7 years of clinical success with published results reporting extremely low complication and dislocation rates and accelerated recoveries. In an effort to streamline these techniques, decrease necessary tooling, and improve operating room workflow, elements of both techniques have been combined. This hybridization is referred to as “SuperPATH” (Supercapsular Percutaneously-Assisted Total Hip).
SuperPATH utilizes powerful elements of both procedures. Preparing the hip in-situ allows the operative leg to rest on a Mayo stand during the entire procedure, obviating the need for a second assistant. Additionally, since the hip is not dislocated, the interval between the gluteus medius and piriformis is utilized, and the piriformis can be preserved in a majority of cases. Utilizing the percutaneous accessory portal for acetabular preparation keeps the wound visualization un-obscured by tooling. This allows the procedure to be done safely through the smaller window created by an intact piriformis. The accessory portal also provides in-line access to the cup, simplifying the insertion of screws, and facilitating impaction of bone-ingrowth components.
A common element to all three of these approaches is that any available implant can be used, including both press-fit and cemented styles for either the femoral or acetabular components. This allows the surgeon to guide implant choice based on the patient’s disease and deformity, without bias from the incision choice. While the authorship favors modular neck implants, non-modular neck implants can easily be used through this approach. The authors have collectively performed many different styles of implants successfully through this approach, many of which have not had modular necks.
This paper details one author’s (JC) experiences utilizing this combined approach, as well as permutations of this entire micro-posterior family of approaches as applied to more complex hip reconstructions.
Data
The two- year follow up of the first 110 SuperPATH total hips (including learning-curve) performed by a single surgeon (JC) has been presented and is currently under peer review. This data includes a third party radiographic evaluation of 66 consecutive hips in the series, with a mean acetabular component inclination of 40.13° (SD = 6.30) and with all femoral & acetabular components well-seated. In this series, mean hospital stay was 1.7 days.
Standard for this technique, all patients received an accelerated post-operative care regimen, which included anticipatory medical care, oral pain control and a standard physical therapy protocol. No hip precautions were used. No IV narcotics were used.
To date, this single-surgeon series includes over 330 primary total hip replacements using the SuperPATH technique. Of those hips, there have been nine complications evenly distributed over the 3 year time period, and without bias to the beginning, or “learning curve”, cases.
Four complications are directly related to the primary THA surgeries: two femur fractures, one acetabular fracture and one loss of acetabular fixation. All occurred in patients with poor bone stock and with a documented history of osteoporosis. Both femur fractures were peri-prosthetic calcar femur fractures (one intra-operative requiring cerclage fixation at the time of surgery, and one found at 1 week post-op, requiring revision to a distal fixation stem to bypass the fracture). Both femur fractures occurred in patients taking continuous bisphosphonate treatment for over 8 years. The acetabular failures consisted of one non-displaced acetabular fracture (recognized intra-operatively and treated with additional fixation screws through the acetabular component), and one failure of fixation at 5 weeks (requiring revision of acetabular component).
Two complications that occurred were potentially unrelated to the THA surgeries. One was a greater trochanteric fracture found intra-operatively and treated with a claw and cables. Atypically, the fracture was found during soft-tissue dissection, prior to any bony work. Further discourse with the patient and critical evaluation of the pre-operative films raised a high suspicion of an un-diagnosed, non-displaced greater trochanteric fracture that existed pre-operatively. The second complication was also a greater trochanteric fracture found at 3 weeks post-operatively. This fracture was not seen on intra-operative, immediate post-operative or one-week post-operative radiographs. A questionable traumatic history was cited, but the patient was a poor historian due to a poorly-controlled psychiatric disorder. The patient denied symptoms, and was treated non-operatively.
Three complications were caused by high-energy trauma unrelated to surgery, but occurring in the early post-operative period: one peri-prosthetic femoral fracture occurring 3 weeks after surgery (requiring ORIF and revision to a distal fixation stem to bypass the fracture); one pelvic fracture occurring 2 weeks after surgery (requiring ORIF); and one traumatic posterior dislocation occurring 1 week after surgery (requiring re-operation to a hooded liner and primary repair of capsule and external rotator musculature).
No instability, neurovascular injuries, infections or peri-operative mortalities have yet occurred.
Case 1
54 year old workman’s compensation male patient presented with startup pain on his right, multiply-operated hip (Fig. 1.1). Patient had initially had his primary THA at age 24 for a severe work-related trauma. Patient has had a total of 6 prior hip replacement surgeries, a primary THA and 5 subsequent revision THAs. This patient is over 450 lb and has aseptic loosening of his acetabular component with a massive posterior deficiency and pelvic defect.
Fig. 1.
1 Pre-operative radiograph. The patient’s acetabular component has shifted, and the THA has recurrent anterior dislocations. 2 Intra-operative photo showing custom cage-cup implanted. Probe is pointing to intact external rotator complex. 3 Post-operative radiograph. The patient’s cage-cup has been implanted according to pre-operative plan. Additional offset was used to adjust for patient’s prior instability
Because this reconstruction was done with the operative leg positioned on the Mayo stand the entire case, only one assistant and one scrub were needed. A 30 cm incision was used in-line with the femur for adequate exposure. The proximal body of the prior revision stem was removed to provide access to the pelvic defect. The previously repaired external rotators were found to be well-healed to the greater trochanter. These were left completely intact (Fig. 1.2). Total operative time was 3 h with an estimated blood loss of 500 cm3.
This patient was discharged on post-operative day 2 without hip precautions. A hip abduction pillow was not used. The patient was kept touchdown weight-bearing due to his obesity and bone loss. He was progressed to full weight-bearing over a 6 week period (Fig. 1.3).
Case 2
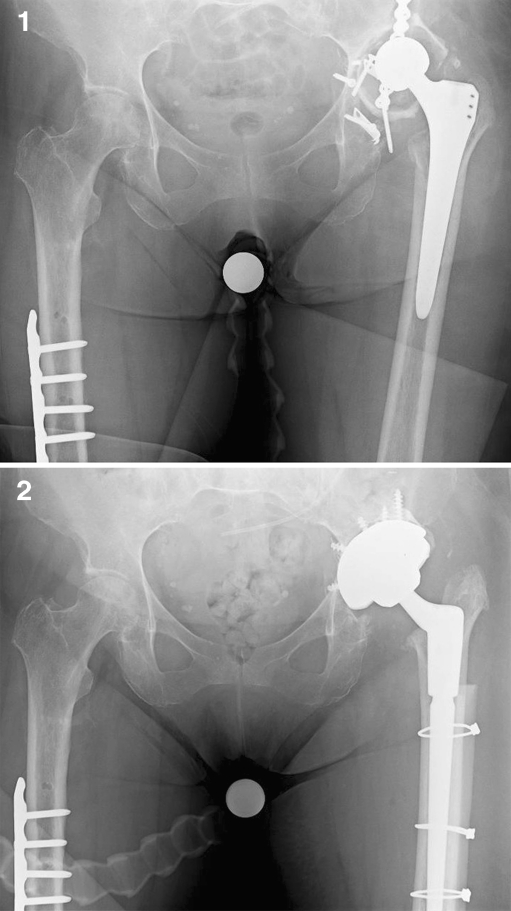
77 year old woman presented with an infected THA after a failed acetabular ORIF (Fig. 2.1). The patient has been wheelchair bound for 2 years due to left hip pain. The patient had significant chronic shortening of the affected limb as well. The THA was explanted without disturbing the previously repaired and healed external rotator mass. Staged revision was done with a non-articulating antibiotic spacer due to poor acetabular bone stock.
Fig. 2.
1 Initial radiograph. Note the cemented acetabular component and retained pelvic hardware. 2 Re-implantation radiographs. Allograft struts were used for the femur, and an augment was used in the acetabulum
After the infection was treated, re-implantation was done through the same micro-superior interval. A fracture was recognized in the femur during distal reaming for preparation of a revision stem. This was fixed using strut allografts and cables (Fig. 2.2). The incision was easily extended down the length of the femur for exposure without violating the external rotators. Incision length was 45 cm.
Acetabular reconstruction required maintaining a high center of rotation due to available bone stock and previous shortening. Multiple screws and a Trabecular Metal augment (Zimmer—Warsaw, IN) were used.
No abduction pillow or post-operative precautions were used. Estimated blood loss was 600 cm3, and the patient required a 1 unit transfusion on post-operative day 1. The patient was discharged to inpatient rehab on post-operative day 3 due to pre-operatively decreased ambulatory status. She was transitioned to full weight-bearing at 6 weeks post-operatively.
Conclusion
Regardless of the approach used to perform hip reconstruction surgery, it is the quality of the reconstruction that dictates long-term success. Most surgeons would agree that this long-term success should not be compromised for the allure of short-term gains. However, appropriate placement of components with the addition of maximal soft tissue preservation creates the opportunity not only to improve short term results, but to further reduce dislocation rates and to optimize the soft tissue envelope for the future, thus potentially improving both short and long-term outcomes.
The authorship believes that the micro-posterior family of hip approaches (PATH, SuperCap & SuperPATH) provides a versatile alternative to the currently popular minimally-invasive approaches without “pigeon-holing” the surgeon into other, less-extensile intervals. The short-term and long-term gains of being truly muscle-sparing are easily attainable, and are unrelated to the size of the incision. Nonetheless, the average incision length was 7.4 cm for the author’s (JC) early series, a convenient side-effect of the nature of the approach.
The entire micro-posterior family of approaches is low-cost, requiring no additional special tables or equipment other than the tooling supplied with the implants for this technique. SuperPATH specifically builds on this by requiring less reliance on support staff, thus improving operative workflow. Since the surgery is done with the operative leg resting on a Mayo stand, the procedure can easily be done without a second assistant. One scrub tech and one assistant were used by the author (JC) in this series, with no request for additional help.
The early results of this modified micro-invasive approach demonstrate safety and reliability in the short-term, with results better or comparable to those reported by studies regarding other hip approaches. Clinical results are comparable to those published for both original techniques from which this technique was derived. Radiographic results have been demonstrated to be consistent, and are comparable to those reported with other approaches.
Longer term follow-up is necessary and is currently being collected.
Acknowledgments
Disclosure J. Chow: consultant to Wright Medical Technology, Inc., Smith & Nephew; B. Penenberg: patents and royalties from Wright Medical Technology, Inc.; S. Murphy: Consultant to Ceramtec, GmbH; patents and royalties from Wright Medical Technology, Inc.; holds stock/stock options in Surgical Planning Associates, Inc.
Contributor Information
James Chow, Phone: +1-602-5533113, Email: jimmy@ChowHipAndKnee.com.
Brad Penenberg, Phone: +1-310-8603470, Email: hipkneemd@gmail.com.
Stephen Murphy, Phone: +1-617-2323040, Email: stephenbmurphymd@gmail.com.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Jewett BA, Collis DK. High complication rate with anterior total hip arthroplasties on a fracture table. Clin Orthop Relat Res. 2011;469(2):503–7. doi: 10.1007/s11999-010-1568-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mouilhade F, Matsoukis J, Oger P, Mandereau C, Brzakala V, Dujardin F. Component positioning in primary total hip replacement: a prospective comparative study of two anterolateral approaches, minimally invasive versus gluteus medius hemimyotomy. Orthop Traumatol Surg Res. 2011;97(1):14–21. doi: 10.1016/j.otsr.2010.05.013. [DOI] [PubMed] [Google Scholar]
- 3.Restrepo C, Mortazavi SM, Brothers J, Parvizi J, Rothman RH. Hip dislocation: are hip precautions necessary in anterior approaches? Clin Orthop Relat Res. 2011;469(2):417–22. doi: 10.1007/s11999-010-1668-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Foucher KC, Wimmer MA, Moisio KC, Hildebrand M, Berli MC, Walker MR, et al. Time course and extent of functional recovery during the first postoperative year after minimally invasive total hip arthroplasty with two different surgical approaches–a randomized controlled trial. J Biomech. 2011;44(3):372–8. doi: 10.1016/j.jbiomech.2010.10.026. [DOI] [PubMed] [Google Scholar]
- 5.Oldenrijk J, Hoogland PV, Tuijthof GJ, Corveleijn R, Noordenbos TW, Schafroth MU. Soft tissue damage after minimally invasive THA. Acta Orthop. 2010;81(6):696–702. doi: 10.3109/17453674.2010.537804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fink B, Mittelstaedt A, Schulz MS, Sebena P, Singer J. Comparison of a minimally invasive posterior approach and the standard posterior approach for total hip arthroplasty a prospective and comparative study. J Orthop Surg Res. 2010;5:46. doi: 10.1186/1749-799X-5-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mayr E, Nogler M, Benedetti MG, Kessler O, Reinthaler A, Krismer M, et al. A prospective randomized assessment of earlier functional recovery in THA patients treated by minimally invasive direct anterior approach: a gait analysis study. Clin Biomech. 2009;24:812–8. doi: 10.1016/j.clinbiomech.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 8.Parratte S, Pagnano MW. Muscle damage during minimally invasive total hip arthroplasty: cadaver-based evidence that it is significant. Instr Course Lect. 2008;57:231–4. [PubMed] [Google Scholar]
- 9.Meneghini RM, Pagnano MW, Trousdale RT, Hozack WL. Muscle damage during MIS total hip arthroplasty. Smith-Petersen versus posterior approach. Clin Orthop Relat Res. 2006;453:293–8. doi: 10.1097/01.blo.0000238859.46615.34. [DOI] [PubMed] [Google Scholar]
- 10.Mardones R, Pagnano MW, Nemanich JP, Trousdale RT. Muscle damage of total hip arthroplasty done with the two-incision and mini-posterior techniques. Clin Orthop Relat Res. 2005;441:63–7. doi: 10.1097/01.blo.0000194727.55372.04. [DOI] [PubMed] [Google Scholar]
- 11.Dorr LD, Maheshwari AV, Long WT, Wan Z, Sirianni LE. Early pain relief and function after posterior minimally invasive and conventional total hip arthroplasty. J Bone Joint Surg. 2007;89-A:1153–60. doi: 10.2106/JBJS.F.00940. [DOI] [PubMed] [Google Scholar]
- 12.Procyk S. Initial results with a mini-posterior approach for total hip arthroplasty. Int Orthop. 2007;31(Suppl):S17–20. doi: 10.1007/s00264-007-0435-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sculco TP, Boettner F. Minimally invasive total hip arthroplasty: the posterior approach. Instr Course Lect. 2006;55:205–14. [PubMed] [Google Scholar]
- 14.O’Brien DA, Rorabeck CH. The mini-incision direct lateral approach in primary total hip arthroplasty. Clin Orthop Relat Res. 2005;441:99–103. doi: 10.1097/01.blo.0000193812.31329.3a. [DOI] [PubMed] [Google Scholar]
- 15.Inaba Y, Dorr LD, Wan Z, Sirainni L, Boutary M. Operative and patient care techniques for posterior mini-incision total hip arthroplasty. Clin Orthop Relat Res. 2005;441:104–14. doi: 10.1097/01.blo.0000193811.23706.3a. [DOI] [PubMed] [Google Scholar]
- 16.Ogonda L, Wilson R, Archbold P, Lawlor M, Mumphreys P, O’Brien S, et al. A minimal-incision technique in total hip arthroplasty does not improve early postoperative outcomes. A prospective, randomized, controlled trial. J Bone Joint Surg Am. 2005;87-A:701–10. doi: 10.2106/JBJS.D.02645. [DOI] [PubMed] [Google Scholar]
- 17.Berger RA, Jacobs JJ, Meneghini M, Della Valle C, Paprosky W, Rosenberg A. Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Rel Res. 2004;429:239–47. doi: 10.1097/01.blo.0000150127.80647.80. [DOI] [PubMed] [Google Scholar]
- 18.Bertin KC, Rottinger H. Anterolateral mini-incision hip replacement surgery: a modified Watson-Jones approach. Clin Orthop Rel Res. 2004;429:248–55. doi: 10.1097/01.blo.0000150294.81825.8c. [DOI] [PubMed] [Google Scholar]
- 19.Goldstein WM, Banson JJ, Berland KA, Gordon AC. Minimal-Incision total hip arthroplasty. J Bone Joint Surg. 2003;85-A:33–8. doi: 10.2106/00004623-200300004-00004. [DOI] [PubMed] [Google Scholar]
- 20.Sculco TP, Jordan LC, Walter WL. Minimally invasive total hip arthroplasty: the Hospital for Special Surgery experience. Orthop Clin North Am. 2004;35:137–42. doi: 10.1016/S0030-5898(03)00116-0. [DOI] [PubMed] [Google Scholar]
- 21.Siguier T, Siguier M, Brumpt B. Mini-incision anterior approach does not increase dislocation rate: A study of 1037 total hip replacements. Clin Orthop Rel Res. 2004;426:164–73. doi: 10.1097/01.blo.0000136651.21191.9f. [DOI] [PubMed] [Google Scholar]
- 22.Woolson ST, Mow CS, Syquia JF, Lannin JV, Schurman DJ. Comparison of primary total hip replacements performed with standard incision or a mini-incision. J Bone Joint Surg Am. 2004;86-A:1353–8. doi: 10.2106/00004623-200407000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Wright JM, Crockett HC, Delgado S, Lyman S, Madsen M, Sculco TP. Mini incision for total hip arthroplasty: a prospective, controlled, investigation with 5 year follow-up evaluation. J Arthroplasty. 2004;19:538–45. doi: 10.1016/j.arth.2003.12.070. [DOI] [PubMed] [Google Scholar]
- 24.••Murphy SB. Tissue-Preserving, minimally invasive total hip arthroplasty using a superior capsulotomy. In: Hozack W, editor. Minimally invasive total hip and knee arthroplaty. Springer-Verlag; 2004. p. 101–107. Detailed description of the SuperCap technique and clinical rationale.
- 25.Murphy SB, Tannast M. Evolution in total hip arthroplasty: computer assisted, minimally invasive techniques combined with alumina ceramic-ceramic bearings. In: D’Antonio J, Dietrich M, editors. Bioceramics in joint arthroplasty. Darmstadt: Steinkopff Verlag; 2005. pp. 119–29. [Google Scholar]
- 26.Murphy SB, Ecker TM, Tannast M. THA performed using conventional and navigated tissue-preserving techniques. Clin Orthop Relat Res. 2006;453:160–7. doi: 10.1097/01.blo.0000246539.57198.29. [DOI] [PubMed] [Google Scholar]
- 27.••Murphy SB, Tannast M. Conventional vs minimally invasive total hip arthroplasty. A prospective study of rehabilitation and complications. Orthopäde. 2006;(35):761-8. This article is in German with an abstract in English. [DOI] [PubMed]
- 28.Penenberg BL, Bolling WS, Riley M. Percutaneously assisted total hip arthroplasty (PATH): a preliminary report. J Bone Joint Surg Am. 2008;90(Suppl 4):209–20. doi: 10.2106/JBJS.H.00673. [DOI] [PubMed] [Google Scholar]
- 29.••Chow J, Kurtz W, Chadha B, Penenberg B, Murphy S. Paper #353: modified superior approach for THA with percutaneous assistance: technique and early results. AAOS Annual Meeting, San Diego, CA. February 15–19, 2011. This paper outlines the SuperPATH technique step-by-step and provides a detailed analysis of a single surgeon’s experience through the learning curve of the technique.