Abstract
Drug users have been found to be at high risk of mortality but the mortality experience of Hispanic drug users remains understudied. This study assessed mortality among Puerto Rican injection drug users (IDUs) in New York City (NY), and in Puerto Rico (PR). Study subjects were 637 IDUs from NY and 319 IDUs from PR. Mortality was ascertained using data from the National Death Index. Annual mortality rate of the NY cohort was 1.3 per 100 person years compared to the PR cohort with a rate of 4.8. Compared to the Hispanic population of New York City, the standardized mortality ratio (SMR) of the NY cohort was 4.4. Compared to the population of Puerto Rico, the SMR of the PR cohort was 16.2. The four principal causes of death were: NY—HIV/AIDS (50.0%), drug overdoses (13.3%), cardiovascular conditions (13.3%), and pulmonary conditions (10.0%); PR—HIV/AIDS (37.0%), drug overdoses (24.1%), sepsis (13.0%), and homicide (11.1%). Modeling time to death using Cox proportional hazards regression, the relative risk of mortality of the PR cohort as compared to the NY cohort was 9.2. The other covariates found to be significantly associated with time to death were age, gender, education, social isolation, intoxication with alcohol, and HIV seropositivity. The large disparity in mortality rates found in this study suggests that health disparities research should be expanded to identify intra-group disparities. Furthermore, these results point to an urgent need to reduce excess mortality among IDUs in Puerto Rico.
Keywords: Injection drug users, Mortality, New York City, Puerto Rico.
Introduction
The mortality of drug users have been found to be substantially higher than that of the general population.1–4 Excess risk of mortality among drug users has been attributed to HIV infection, drug overdosing, and violence.5–7 Fluctuations over time in the relative influence of different causes of death have also been noted. During the 1990s, several studies reported decreasing death rates due to HIV infection among drug users and attributed the downward trends to the new HIV medication regimens.8,9 However, during the same period, other studies documented significant increases in drug overdose deaths in several countries.10–15
Notwithstanding these studies, the rates and causes of mortality of Hispanic drug users in the U.S. remain understudied. For the most part, mortality among drug users has been examined among non-Hispanic white and African-American groups.16 Furthermore, the few studies that have assessed mortality among Hispanic drug users have generally not distinguished among Hispanics of different national origins.8,17 There is ample evidence that Hispanics of different national origins have widely divergent drug use patterns and differ also in the consequences of their drug use.18–20 A study conducted by Selik21 on mortality due to HIV infection among U.S. Hispanics found large disparities in death rates by national origin. Hispanics of Puerto Rican origin had a significantly higher rate of death due to HIV diseases than those of Cuban, Central/South American or Mexican origin.
Among Hispanics, Puerto Ricans have been one of the groups most severely affected by the drug abuse and HIV/AIDS epidemics.22 There is evidence that the drug use rates of Puerto Ricans living in the U.S. mainland are among the highest of all Hispanic populations.18,23,24 Moreover, Puerto Rico is one of the AIDS epicenters of the Americas with annual incidence rates consistently among the ten highest in the U.S.25 and cumulative per capita rates among the highest in the Central America and Caribbean region.26 Drug injection is the main HIV/AIDS transmission category in Puerto Rico27 and among Puerto Ricans living in the U.S. mainland.28 Not surprisingly, Puerto Rican drug users have consistently been found to have a greater overall HIV risk than drug users of other ethnic/racial backgrounds and other Hispanic/Latino groups.22,29 Yet little is known about the mortality risks of Puerto Rican drug users.
This study assessed the mortality rates of Puerto Rican injection drug users (IDUs) residing in two urban settings: East Harlem, New York (NY), and Bayamon, Puerto Rico (PR). We had previously examined the mortality rate of a group of IDUs in Puerto Rico30 but had been unable to compare the data to that of a sample from the U.S. mainland. In the present study, two samples of street-recruited Puerto Rican IDUs were recruited and prospectively followed-up with similar methodologies to assess differences in mortality rates and causes of death.
Materials and Methods
Sampling and Subjects
Data for this study were collected as part of the parent ARIBBA project (Alliance for Research in El Barrio and Bayamon). Detailed descriptions of the study design, sampling and instrumentation of the ARIBBA project have been published elsewhere.31 The catchment areas of the ARIBBA project comprised the East Harlem area of New York City and the urban section of the municipality of Bayamon in the San Juan metropolitan area in Puerto Rico. Ethnographic mapping procedures were conducted to locate the drug copping areas and divide the catchment areas into sectors.32 Potential participants were identified through random visits to the sectors. To be eligible, subjects had to self-identify as Puerto Rican, have injected drugs or smoked crack during the last 30 days, and be 18 years old or more. An informed consent previously approved by the IRBs of both research groups was verbally explained. The approved informed consents included a provision enabling investigators to inquire among third parties about the whereabouts of participants lost to follow-up. Consenting subjects were tested with the OnTrak urinalysis TestStik system (Roche Diagnostic Systems, Inc., Branchburg, NJ) to confirm recent use of heroin or cocaine. Participants were then assessed with a structured interview and offered HIV testing and counseling. Sampling and recruitment of both cohorts was conducted between January 1998 and August 1999, and 1,199 drug users completed the baseline assessment: 800 in New York City and 399 in Puerto Rico. Of these, 956 participants reported ever having injected drugs: 637 in NY and 319 in PR. Participants not reporting a history of drug injection were excluded from the analyses. Participants were followed-up and re-assessed 6, 36, and 42 months after recruitment.
Interviewing and Measures
The interview protocol was designed in English by both teams of researchers and was then translated into Spanish. The accuracy of the translation was verified through back translation. The protocol was pilot tested in both sites and field personnel conducted periodic cross-site visits to ensure the comparability of recruitment and interviewing. The baseline assessment interview lasted, on average, 90 minutes.
Depression was measured using the Center for Epidemiologic Studies Depression scale (CESD33). We used the cut-off point recommended for the population of Puerto Rico (a score of 20 or more34). History of victimization included questions about ever having been beaten, mugged or robbed, stabbed with a knife, or shot with a weapon. Respondents were questioned about lifetime experiences of sexual abuse or rape. Respondents indicating they had no close relative or friend with whom they spent time were classified as socially isolated. Engagement in income-generating illicit activities was ascertained by asking respondents if during the last 30 days they had made money in the drug trade, prostitution, stealing or selling stolen goods or by forgery or fraud. Several measures of drug use were used in this study. Respondents were asked if they had used alcohol until intoxicated, had smoked crack cocaine, had used heroin mixed with cocaine (“speedballs”), and the number of times they had injected. These questions were asked of the 30-day period prior to the baseline interview. History of drug overdosing was also asked of respondents. Respondents were asked if they had exchanged syringes in a needle exchange program (NEP), if they had received any drug treatment, and if they had been covered by health insurance during the previous 30 days. HIV serostatus was measured using Orasure (OraSure Technologies Inc., Bethlehem Pennsylvania). The Orasure sample collection stick was administered by project personnel trained in its proper use in the two sites, and the samples were tested in the same laboratory. HIV-positive samples were confirmed with a Western-blot assay. HIV-positive participants were asked if they were receiving antiretroviral medications.
Mortality Data
Mortality was determined through the National Death Index (NDI) of the National Center for Health Statistics. The National Death Index receives electronic records of deaths from all U.S. states and territories following a standardized reporting protocol. NDI officials estimate a lag of one year from the occurrence of a death to its record being available in NDI's datasets. A separate IRB panel at NDI reviewed and approved the mortality ascertainment study. Upon completion of the 36- and 42-month follow-ups, lists of participants who had not been re-interviewed were compiled and sent to NDI. Two separate lists were submitted, a first one after the end of year 2001 and a second one after 2002 (when subjects had been in the study a period of approximately four years). The lists included gender, first and last names, social security numbers, and birth dates. NDI matched the lists against all the deaths records reported nationwide and returned a computer print-out with all possible matches. Possible matches whose year of birth was within 2 years of our information and whose last name and gender were a complete match were considered to represent a deceased participant (86 cases).
Cause of death data was then compiled through the health departments of the states where the subjects had died using the death certificate number provided by NDI. Causes of death were examined and grouped into broader categories each one including at least three cases. On initial review three groups of deaths were defined—HIV/AIDS-related, drug overdoses, and homicide. HIV/AIDS-related causes were defined as those deaths whose first cause was ‘HIV disease’ (ICD9 codes 042-044, ICD10 codes B20-B23.8) or whose first cause was an AIDS-defining disease and the second cause was HIV disease or “Laboratory evidence of HIV” (ICD10 code R75). Drug overdose deaths were those coded E850–E858 (ICD9) or X40–X44 (ICD10) under the first or second cause. During the course of the study both the State of New York and the Commonwealth of Puerto Rico required that all deaths suspected of drug intoxication be autopsied. The remaining causes were classified according to the specific system or organ failure as indicated on the death certificate's first cause. The systems found to have at least three cases were pulmonary, cardiovascular, and gastrointestinal. Finally, a separate category was created for deaths occurring due to sepsis. The remaining deaths were grouped into an ‘other’ category.
Analyses
The baseline characteristics of the two cohorts and the distributions of causes of death were compared using chi-square, Student t, and Wilcoxon–Mann–Whitney test. Relevant baseline characteristics were selected based on the mortality literature and from our previous studies with these two cohorts.35 Annual mortality rates were calculated as the total number of deaths divided by the number of person-years in each cohort. Confidence limits for the annual mortality rates were calculated by assuming a Poisson distribution. Annual survival probabilities were computed for each cohort and tested with the Kaplan Meier Log Rank test. Standardized mortality ratios were also calculated. For the NY cohort, the projected Hispanic population of New York City in 2001 was used as the standard population. The projected population of the island of Puerto Rico in 2001 was used as the standard population for the PR cohort. General population projections and number of deaths were obtained from the New York City Department of Health and Mental Hygiene and from the Puerto Rico Health Department.36,37 The standardized mortality ratio for each cohort was calculated as the number of observed deaths divided by the number of expected deaths based on the age and gender specific death rates of the respective general populations.38
To calculate adjusted relative risks of death of the PR cohort compared to the NY cohort, time to death data was modeled using Cox's proportional hazards regression.39
Results
Table 1 compares the baseline characteristics of the two cohorts. On average, the NY cohort was five years older than the PR cohort (mean ages 38.6 vs. 33.2, p < 0.001). The NY cohort had a higher proportion of females than the PR cohort (22.0 vs. 14.1%, p = 0.003), and NY participants were more likely to be married than PR participants (26.2 vs. 18.5%, p = 0.008). History of victimization, sexual abuse, and social isolation were all more likely to be reported by the NY cohort than by the PR cohort (victimization: 81.2 vs. 70.8%, p < 0.001; sexual abuse: 13.0 vs. 7.2%, p = 0.007; social isolation: 30.6 vs. 21.3%, p = 0.002). Compared to the NY cohort, the PR cohort was more likely to have injected drugs during the previous 30 days (87.0 vs. 96.9%, p < 0.001) and among those currently injecting, to inject much more frequently (mean number of injections in the last 30 days 77.5 vs. 182.0, p < 0.001). NY participants were more likely than PR participants to have used alcohol to intoxication (6.4 vs. 2.2%, p = 0.005) and to have smoked crack (50.7 vs. 33.9%, p < 0.001) but were less likely to have injected speedballs (49.3 vs. 87.8%, p < 0.001). NY participants were also more likely to report prior episodes of drug overdoses than PR participants (41.4 vs. 29.5%, p < 0.001). NY participants were more likely than their counterparts in PR to have received syringes from a needle exchange program (46.6 vs. 33.9%, p < 0.001), to be in drug treatment (56.8 vs. 9.7%, p < 0.001), and to be covered by health insurance (67.2 vs. 38.6%, p < 0.001). HIV seroprevalence was slightly higher in the NY cohort than in the PR cohort (28.9 vs. 22.9%, p = 0.048), and among HIV-positives, NY participants were more likely to be taking antiretroviral therapy (37.0 vs. 9.6%, p < 0.001).
Table 1.
Cohort profiles as measured upon recruitment
| NY cohort (n = 637) | PR cohort (n = 319) | ||||||
|---|---|---|---|---|---|---|---|
| n | % | Mean(SD) | n | % | Mean(SD) | p | |
| Age | 38.6(7.6) | 33.2(8.3) | <0.001 | ||||
| Female gender | 141 | 22.1 | 45 | 14.1 | 0.003 | ||
| High school education or more | 257 | 40.3 | 144 | 45.1 | 0.157 | ||
| Homeless | 145 | 22.8 | 71 | 22.3 | 0.860 | ||
| Married | 167 | 26.2 | 59 | 18.5 | 0.008 | ||
| Depression | 354 | 55.7 | 198 | 62.1 | 0.059 | ||
| History of victimization | 517 | 81.2 | 226 | 70.8 | <0.001 | ||
| History of sexual abuse | 83 | 13.0 | 23 | 7.2 | 0.007 | ||
| Social isolation | 195 | 30.6 | 68 | 21.3 | 0.002 | ||
| Engaged in income- generating illicit activities | 326 | 51.2 | 174 | 54.5 | 0.326 | ||
| Currently injecting drugs1 | 554 | 87.0 | 309 | 96.9 | <0.001 | ||
| Number of injections in the last 30 days2 | 77.5(95.7) | 182.0(147.2) | <0.001 | ||||
| Intoxicated with alcohol1 | 41 | 6.4 | 7 | 2.2 | 0.005 | ||
| Used crack1 | 323 | 50.7 | 108 | 33.9 | <0.001 | ||
| Used speedballs1 | 314 | 49.3 | 280 | 87.8 | <0.001 | ||
| History of ODs | 264 | 41.4 | 94 | 29.5 | <0.001 | ||
| Received syringes from NEP | 297 | 46.6 | 108 | 33.9 | <0.001 | ||
| In drug treatment1 | 362 | 56.8 | 31 | 9.7 | <0.001 | ||
| Covered by health insurance | 428 | 67.2 | 123 | 38.6 | <0.001 | ||
| HIV positive test results | 184 | 28.9 | 73 | 22.9 | 0.048 | ||
| Taking antiretrovirals3 | 68 | 37.0 | 7 | 9.6 | <0.001 | ||
SD Standard deviation, ODs drug overdoses, NEP Needle exchange program, last 30 days.
1During the 30-day period prior to the baseline interview.
2Among those injecting drugs during the 30-day period prior to the baseline interview.
3Among HIV-positive participants at time of recruitment, includes 20 cases reporting receiving HAART.
During the course of the study the NY cohort recorded 2,615 person years and 33 deaths, an annual mortality rate of 1.3 per 100 person years (95% CI 0.8–1.7). The PR cohort recorded 1,196 person years and 56 deaths, an annual mortality rate of 4.8 (95% CI 3.5–6.0). The risk of mortality of the PR cohort was 312 times higher than that of the NY cohort. The mortality rates were also estimated after stratifying the cohorts by HIV serostatus at recruitment. The estimates are shown in Table 2. In both cohorts the mortality rates of HIV-positives were about five times the mortality rates of HIV-negatives (NY: 3.2 vs. 0.5; PR: 12.7 vs. 2.9). Relative risks of mortality of the PR cohort compared to the NY cohort did not differ noticeably between HIV-negatives and HIV-positives (incidence rate ratios of 5.4 and 4.0, respectively).
Table 2.
Mortality rates stratified by HIV-serostatus at time of recruitment
| NY cohort | ||||||
|---|---|---|---|---|---|---|
| Person years | Deceased | Rate1 | 95% CI2 | IRR | 95% CI2 | |
| All | 2,615 | 33 | 1.3 | 0.8–1.7 | ||
| HIV-negative | 1,894 | 10 | 0.5 | 0.2–0.9 | ||
| HIV-positive | 721 | 23 | 3.2 | 1.9–4.5 | ||
| PR cohort | ||||||
| All | 1,169 | 56 | 4.8 | 3.5–6.0 | 3.8 | 2.5–5.8 |
| HIV-negative | 941 | 27 | 2.9 | 1.8–4.0 | 5.4 | 2.8–11.8 |
| HIV-positive | 228 | 29 | 12.7 | 8.1–17.3 | 4.0 | 2.3–6.9 |
IRR Incidence rate ratio.
1Rates per 100 person years.
295% confidence intervals.
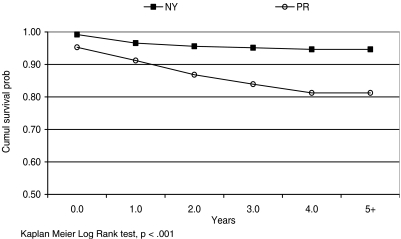
Figure 1 shows the plots of the annual cumulative survival probabilities of the two cohorts. The cumulative survival probability of the PR cohort descended at a much faster rate than that of the NY cohort, and the difference was statistically significant (p < 0.001).
Figure 1.
Cumulative survival probability of each study cohort. Kaplan Meier Log Rank test, p < 0.001
The mortality rates of the NY and PR cohorts were compared to those of their respective general populations by calculating standardized mortality ratios (SMRs, data not shown). The mortality rate of the general population of Puerto Rico was about 35% higher than that of the general population of Hispanics in New York City (321 vs. 240 per 100,000 population). The mortality rate of the NY cohort was four times higher than the rate expected based on the mortality experience of the Hispanic population of New York City (SMR = 4.4, 95% CI 3.5–5.4). The SMR of the PR cohort was 312 times higher, 16.2 (95% CI 15.7–16.6). In both cohorts, the SMRs of the females were several times higher than that of the males (NY SMRs: females = 10.6, males = 3.6; PR SMRs: females = 85.7, males = 12.9).
Causes of deaths are shown in Table 3. The causes of death of the two cohorts differed significantly (p = 0.016). The four principal causes of death of the NY cohort were HIV/AIDS (50.0%), drug overdoses (13.3%), cardiovascular conditions (13.3%), and pulmonary conditions (10.0%). The four principal causes of the PR cohort were HIV/AIDS (37.0%), drug overdoses (24.1%), sepsis (13.0%), and homicide (11.1%). Table 3 also compares the causes of death across gender groups. The distributions were not statistically significant (p = 0.762), but there were some notable differences. Compared to males, a greater proportion of females died due to pulmonary conditions (4.7 vs. 15.0%), and none died of sepsis (6.3 vs. 0.0%).
Table 3.
Causes of death by study site and gender
| Cause of death1 | NY cohort (n = 33) | PR cohort (n = 56) | p | Males (n = 67) | Females (n = 22) | p | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |||
| HIV | 15 | 50.0 | 20 | 37.0 | 26 | 40.6 | 9 | 45.0 | ||
| Drug overdose | 4 | 13.3 | 13 | 24.1 | 13 | 20.3 | 4 | 20.0 | ||
| Homicide | 0 | 0.0 | 6 | 11.1 | 5 | 7.8 | 1 | 5.0 | ||
| Pulmonary | 3 | 10.0 | 3 | 5.6 | 0.016 | 3 | 4.7 | 3 | 15.0 | 0.762 |
| Cardiovascular | 4 | 13.3 | 0 | 0.0 | 6 | 9.4 | 1 | 5.0 | ||
| Gastrointestinal | 2 | 6.7 | 2 | 3.7 | 3 | 4.7 | 1 | 5.0 | ||
| Sepsis | 0 | 0.0 | 7 | 13.0 | 4 | 6.3 | 0 | 0.0 | ||
| Other | 2 | 6.7 | 3 | 5.6 | 4 | 6.3 | 1 | 5.0 | ||
1Missing cause of death on five cases: three from the NY cohort and two from the PR cohort; three males and two females.
Table 4 shows the results from modeling time to death with Cox proportional hazards regression analysis. The table shows the hazards ratios estimated after entering each covariate separately (without adjusting for the other variables) and the hazards ratios estimated after adjusting for all other covariates. The relative risk of mortality of the PR cohort as compared to the NY cohort increased from 3.7 prior to entering other covariates in the model to 9.2 after adjusting for other covariates. The other covariates found to be significantly associated with time to death were age (35-44 years old—HR = 5.1, p = 0.028; 45 years or older—HR = 6.6, p = 0.014), female gender (HR = 1.7, p = 0.048), education, (HR=0.6, p = 0.049), social isolation (HR = 2.4, p < 0.001), use of alcohol to intoxication (HR = 1.8, p = 0.041), and HIV seropositivity at recruitment (HIV-positive not receiving antiretrovirals—HR = 2.7, p < 0.001; HIV-positive receiving antiretrovirals—HR=5.6, p < 0.001). Interaction effects between study site and all the other covariates were tested, and none were found to have a statistically significant effect over the risk of mortality (tests not shown).
Table 4.
Results of regressing time to death with Cox’s proportional hazards regression
| Covariates | Unadjusted hazards ratio | Adjusted hazards ratio | 95.0% CI | p |
|---|---|---|---|---|
| PR cohort1 | 3.7 | 9.2 | 4.8–17.8 | <0.001 |
| 25–34 years old2 | 1.9 | 2.1 | 0.5–9.4 | 0.312 |
| 35–44 years old2 | 3.9 | 5.1 | 1.2–21.8 | 0.028 |
| 45 years or more2 | 4.0 | 6.6 | 1.5–29.8 | 0.014 |
| Female gender | 1.4 | 1.7 | 1.0–2.9 | 0.048 |
| High school education or more | 0.6 | 0.6 | 0.4–1.0 | 0.049 |
| Homeless | 0.8 | 0.7 | 0.4–1.2 | 0.196 |
| Married | 0.7 | 0.9 | 0.5–1.7 | 0.818 |
| Depression | 1.5 | 1.3 | 0.8–2.1 | 0.214 |
| History of victimization | 0.8 | 1.2 | 0.7–2.0 | 0.567 |
| History of sexual abuse | 1.4 | 1.2 | 0.6–2.4 | 0.675 |
| Social isolation | 1.7 | 2.4 | 1.5–4.0 | <0.001 |
| Engaged in income-generating illicit activities3 | 0.7 | 0.7 | 0.5–1.2 | 0.185 |
| Currently injecting drugs2 | 1.2 | 1.3 | 0.4–4.2 | 0.648 |
| Intoxicated with alcohol3 | 2.4 | 1.8 | 1.0–3.1 | 0.041 |
| Used crack2 | 0.7 | 0.7 | 0.4–1.2 | 0.197 |
| Used speedballs2 | 1.8 | 1.0 | 0.6–1.7 | 0.994 |
| History of ODs | 0.8 | 0.7 | 0.4–1.1 | 0.157 |
| Received syringes from NEP | 1.5 | 1.6 | 0.9–2.8 | 0.139 |
| In drug treatment2 | 0.7 | 1.2 | 0.6–2.1 | 0.628 |
| Covered by health insurance | 0.8 | 1.1 | 0.6–1.8 | 0.837 |
| HIV-positive not receiving antiretrovirals4 | 4.0 | 2.7 | 1.7–4.5 | <0.001 |
| HIV positive receiving antiretrovirals4 | 4.3 | 5.6 | 2.9–10.9 | <0.001 |
1Reference category = NY cohort.
2Reference category = 18 to 24 years old.
3During the 30-day period prior to the baseline interview.
4Reference category = HIV-negative at time of recruitment.
Conclusions
In this study we found the annual mortality rate of IDUs in Puerto Rico to be 312 times higher that that of Puerto Rican IDUs in New York City. Such a large difference is rather surprising given that the cohort in New York City was older, had a higher rate of HIV seroprevalence, was more likely to report histories of victimization and sexual abuse, and was more likely to be socially isolated. The relative risks of mortality of IDUs in Puerto Rico compared to their counterparts in New York City did not differ noticeably among HIV-negatives and HIV-positives. This suggests that the cross-site difference in the risk of mortality was not due to differences in the rates of progression to AIDS or HIV prognosis but that mortality was substantially higher regardless of HIV serostatus. However, the magnitude of the difference in the death rates among HIV-positives should not be overlooked: Of those who were HIV positive at baseline, 13% died in the New York cohort compared to 40% in the Puerto Rico cohort. We also compared the mortality rates of the two cohorts to that of their respective general populations and found that the SMR of the Puerto Rico cohort was still 312 higher than that of the New York cohort. Thus, differences in mortality rates in the general populations could not account for the large cross-site difference.
The causes of death of the two cohorts also differed notably. Compared to the New York City cohort, larger proportions of the deceased in Puerto Rico died of drug overdoses (13 vs. 24%), homicide (none vs. 11%), and sepsis (none vs. 13%). We had previously examined drug-overdose deaths at the population level and found that while per-capita rates in the U.S., as well as in New York State, doubled during the period from 1990 to 2000 (from 1.8 to 4.5 per 100,000 population, and from 1.9 to 3.5, respectively), the rate in Puerto Rico increased threefold from an already high rate of 3.3 in 1990 to 11.1 in the year 2000.40 From our data, we cannot discern the extent to which differences in drug-overdose deaths could be accounted by differences in purity of the drugs available to each cohort. However, according to the information available at the Drug Enforcement Administration, both the purity and price of street heroin in East Harlem and Bayamon during the recruitment period were quite similar (average purity 53.1 ± 4.3% in the Bayamon area and 53.9 ± 2.8% in the East Harlem area; Michael Chapman, personal communication).
The difference in homicide deaths is also congruent with population-level statistics. In 2001 the metropolitan area of San Juan had the highest murder rate among 275 metropolitan areas reporting uniform crime statistics to the U.S. Department of Justice.41 The per capita murder rate for San Juan was 25.8, while that of New York City was 7.2.
Deaths caused by sepsis could be suggestive of an overall lower quality of life among IDUs in Puerto Rico compared to New York City, with a preponderance of deaths due to acute causes as opposed to chronic conditions.42 Specifically, soft skin infections left untreated could lead to death by sepsis. In our study, outreach workers and interviewers conducting cross-site visits commented on the unusually high rate of infected skin lesions observed among the IDUs in Puerto Rico. Unfortunately, we failed to collect measures of skin lesions and infections.
The large difference in the mortality rates of the two cohorts was not reduced after adjusting for other predictors of mortality. The relative risk of the PR cohort compared to the NY cohort increased more than twofold from 3.7 to 9.2 after adjustment. This increase in relative risk of mortality was probably the result of the PR cohort being younger and less likely to be socially isolated and HIV infected than the NY cohort, yet having a substantially higher mortality rate.
The mortality rates estimated in this study are consistent with previous estimates published for drug users in Puerto Rico and New York City.43,44 Mortality among IDUs in Puerto Rico was examined in the early part of the 1990s when HAART was not widely available.30 The estimate from this previous study was equal to that of the current study (4.8). The findings of our study are also consistent with some of our previous findings from the parent ARIBBA project, indicating greater overall HIV risk and incidence and lower use of protective and health services in the PR cohort compared to the NY cohort.35,45,46 The covariates found to be significantly associated with time to death in the Cox proportional hazards regression analysis—age, education, HIV infection, social isolation—are also consistent with other studies of mortality.47–49
Even though we cannot rule out that other unmeasured individual-level factors could account for the cross-site difference, higher-level factors such as access and availability of services might also be exerting an important influence. For example, the catchment area where the NY cohort was recruited had five methadone programs with multiple clinics where HIV care was directly offered. The catchment area in PR had one methadone clinic working at full capacity and offering no other health service.46 Additionally, HIV-positive IDUs in the New York cohort were close to four times more likely to be on antiretrovirals than their counterparts in the Puerto Rico cohort (37.0 vs. 9.6%). Focus group discussions in both sites regarding experiences of mainland-island travel revealed that seeking drug treatment and other health services was often presented as a reason for traveling to the mainland but not for traveling from the mainland to the island.
Our study has a number of potential limitations that merit further discussion. As is the case with all studies conducted with samples of community-recruited drug users, the cohorts in this study cannot be considered representative of drug users in either catchment area. We attempted to reduce selection biases by mapping the street sites where drug users congregate and conducting recruitment visits at random. Another limitation of our study is the fact that, except for the mortality and HIV serostatus data, measures were derived from self-reports. We invested considerable efforts at developing a comparable interview protocol for the two cohorts, and previous studies of self-reports of street-recruited IDUs suggest that the self-reports are reasonably valid and reliable.50,51 Nevertheless, the presence of selection, recall, or social desirability biases in the data cannot be ruled out. The mortality status of both cohorts was acquired from the same source, NDI, and we had several conversations with officials of the NDI to confirm that states followed similar reporting procedures and schedules. Nevertheless, we lack hard data on differences in the accuracy and quality of state mortality reports.
Contrary to other studies,42 we found that receiving antiretroviral medications among HIV-positives increased the risks of mortality. This finding should be interpreted with caution. Our sample included a large number of HIV-negative individuals, and they comprised the reference category against which the risk of mortality of HIV-positives on antiretrovirals was assessed.
Notwithstanding these limitations, we believe the findings of this study are highly compelling. The large disparity in mortality rates found in this study suggests that the current emphasis on analyzing health disparities across different ethnic/racial groups52,53 should be expanded to include the study of the disparities that occur within single groups. The study of intra-group disparities could contribute additional information on the factors affecting disparities and help address them more effectively.
Our results also point to an urgent need to reduce excess mortality among IDUs in Puerto Rico. The findings suggest that interventions should include efforts to reduce violence and aggression against drug users, reduce fatal drug overdoses, and raise the level of health care provided to IDUs in Puerto Rico. The especially high mortality rates among females in both cohorts should also be of concern. The SMR of females in the New York cohort was three times that of males and in Puerto Rico almost seven times that of males. Moreover, after adjusting for other predictors of mortality, female IDUs were almost two times more likely to die than males. Early mortality among women is generally explained by women's health behaviors, such as reduced use of HAART despite its wide availability, lack of health care, and lack of a regular source of care.54,55 However, the high mortality rate of female IDUs in our cohorts also needs to be understood in light of the disproportional stigma the Hispanic culture holds against drug-using women.56,57 Designing supportive systems, including health and drug treatment programs, that address the specific needs of Puerto Rican drug-using women should also become a high priority public health issue.
AcknowledgEments
This study was funded by the National Institute On Drug Abuse, Grant DA10425. The authors also wish to express their appreciation to the Demographic Registry of the Puerto Rico Department of Health, the National Death Index of the National Center for Health Statistics, and the Office of Vital Statistics, New York City Department of Health, for their collaboration in obtaining the mortality data.
References
- 1.Vlahov D, Wang C, Galai N, et al. Mortality risk among new onset injection drug users. Addiction. 2004;99:946–954. doi: 10.1111/j.1360-0443.2004.00780.x. [DOI] [PubMed] [Google Scholar]
- 2.Goedert JJ, Fung MW, Felton S, Battjes RJ, Engels EA. Cause-specific mortality associated with HIV and HTL-VII infections among injecting drug users in the USA. AIDS. 2001;15:1295–1302. doi: 10.1097/00002030-200107060-00012. [DOI] [PubMed] [Google Scholar]
- 3.Tyndall MW, Craib KJ, Currie S, Li K, O'Shaughnessy MV, Schechter MT. Impact of HIV infection on mortality in a cohort of injection drug users. J Acquir Immune Defic Syndr. 2001;28:351–357. doi: 10.1097/00126334-200112010-00008. [DOI] [PubMed] [Google Scholar]
- 4.Hulse GK, English DR, Milne E, Holman CD. The quantification of mortality resulting from the regular use of illicit opiates. Addiction. 1999;94:221–229. doi: 10.1046/j.1360-0443.1999.9422216.x. [DOI] [PubMed] [Google Scholar]
- 5.Copeland L, Budd J, Robertson JR, Elton RA. Changing patterns in causes of death in a cohort of injecting drug users, 1980–2001. Arch Intern Med. 2004;164:1214–1220. doi: 10.1001/archinte.164.11.1214. [DOI] [PubMed] [Google Scholar]
- 6.Marzuk PM, Tardiff K, Leon AC, et al. Poverty and fatal accidental drug overdoses of cocaine and opiates in New York City: an ecological study. Am J Drug Alcohol Abuse. 1997;23:221–228. doi: 10.3109/00952999709040943. [DOI] [PubMed] [Google Scholar]
- 7.Kawachi I, Kennedy BP, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. Am J Public Health. 1997;87:1491–1498. doi: 10.2105/ajph.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whitman S, Murphy J, Cohen M, Sherer R. Marked declines in human immunodeficiency virus-related mortality in Chicago in women, African Americans, Hispanics, young adults, and injection drug users, from 1995 through 1997. Arch Intern Med. 2000;160:365–369. doi: 10.1001/archinte.160.3.365. [DOI] [PubMed] [Google Scholar]
- 9.Bargagli AM, Sperati A, Davoli M, Forastiere F, Perucci CA. Mortality among problem drug users in Rome: an 18-year follow-up study, 1980–97. Addiction. 2001;96:1455–1463. doi: 10.1046/j.1360-0443.2001.961014559.x. [DOI] [PubMed] [Google Scholar]
- 10.Wahren CA, Brandt L, Allebeck P. Has mortality in drug addicts increased? A comparison between two hospitalized cohorts in Stockholm. Int J Epidemiol. 1997;26:1219–1226. doi: 10.1093/ije/26.6.1219. [DOI] [PubMed] [Google Scholar]
- 11.Zaccarelli M, Gattari P, Rezza G, et al. Impact of HIV infection on non-AIDS mortality among Italian injecting drug users. AIDS. 1994;8:345–350. doi: 10.1097/00002030-199403000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Galli M, Musicco M. Mortality of intravenous drug users living in Milan, Italy: role of HIV-1 infection. COMCAT Study Group. AIDS. 1994;8:1457–1463. doi: 10.1097/00002030-199410000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Darke S, Zador D. Fatal heroin ‘overdose’: a review. Addiction. 1996;91:1765–1772. doi: 10.1111/j.1360-0443.1996.tb03800.x. [DOI] [PubMed] [Google Scholar]
- 14.Sperry K. An epidemic of intravenous narcoticism deaths associated with the resurgence of black tar heroin. J Forensic Sci. 1988;33:1156–1162. [PubMed] [Google Scholar]
- 15.Darke S, Hall W, Weatherburn D, Lind B. Fluctuations in heroin purity and the incidence of fatal heroin overdose. Drug Alcohol Depend. 1999;54:155–161. doi: 10.1016/S0376-8716(98)00159-8. [DOI] [PubMed] [Google Scholar]
- 16.Appel PW, Joseph H, Richman BL. Causes and rates of death among methadone maintenance patients before and after the onset of the HIV/AIDS epidemic. Mt Sinai J Med. 2000;67:444–451. [PubMed] [Google Scholar]
- 17.Galea S, Ahern J, Tardiff K, et al. Racial/ethnic disparities in overdose mortality trends in New York City, 1990–1998. J Urban Health. 2003;80:201–211. doi: 10.1093/jurban/jtg023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Delva J, Wallace JM, Jr, O'Malley PM, Bachman JG, Johnston LD, Schulenberg JE. The epidemiology of alcohol, marijuana, and cocaine use among Mexican American, Puerto Rican, Cuban American, and other Latin American eighth-grade students in the United States: 1991–2002. Am J Public Health. 2005;95:696–702. doi: 10.2105/AJPH.2003.037051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alvarez J, Olson BD, Jason LA, Davis MI, Ferrari JR. Heterogeneity among Latinas and Latinos entering substance abuse treatment: findings from a national database. J Subst Abuse Treat. 2004;26:277–284. doi: 10.1016/j.jsat.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 20.Ortega AN, Rosenheck R, Alegria M, Desai RA. Acculturation and the lifetime risk of psychiatric and substance use disorders among Hispanics. J Nerv Ment Dis. 2000;188:728–735. doi: 10.1097/00005053-200011000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Selik, R.M. Comparison of Rates of Death Due to HIV Disease among U.S. Hispanics of Different National Origins in 2000. Paper presented at the National HIV Prevention Conference, Atlanta, Georgia, July 2003.
- 22.Montoya ID, Bell DC, Richard AJ, Carlson JW, Trevino RA. Estimated HIV risk among Hispanics in a national sample of drug users. J Acquir Immune Defic Syndr. 1999;21:21–50. doi: 10.1097/00126334-199905010-00006. [DOI] [PubMed] [Google Scholar]
- 23.Ortega AN, Rosenheck R, Alegria M, Desai RA. Acculturation and the lifetime risk of psychiatric and substance use disorders among Hispanics. J Nerv Ment Dis. 2000;188:728–735. doi: 10.1097/00005053-200011000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Wallace JM, Jr, Bachman JG, O'Malley PM, Johnston LD, Schulenberg JE, Cooper SM. Tobacco, alcohol, and illicit drug use: racial and ethnic differences among U.S. high school seniors, 1976–2000. Public Health Rep. 2002;117(Suppl 1):S67–S75. [PMC free article] [PubMed] [Google Scholar]
- 25.HIV AIDS Surveill Rep, 2004. Vol. 16. Atlanta: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2005. [Google Scholar]
- 26.Pan American Health Organization. AIDS Surveillance in the Americas. Pan American Health Organization, Washington DC, June 2002.
- 27.Puerto Rico Department of Health. AIDS Surveillance Report. Puerto Rico Department of Health, San Juan, Puerto Rico, 2005.
- 28.Diaz T, Buehler JW, Castro KG, Ward JW. AIDS trends among Hispanics in the United States. Am J Public Health. 1993;83:504–509. doi: 10.2105/ajph.83.4.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Deren S, Robles RR, Andia JF, Colón HM, Kang S-Y, Perlis T. Trends in HIV seroprevalence and needle sharing among Puerto Rican drug injectors in Puerto Rico and New York: 1992–1999. J Acquir Immune Defic Syndr. 2001;26:164–169. doi: 10.1097/00042560-200102010-00009. [DOI] [PubMed] [Google Scholar]
- 30.Robles RR, Matos TD, Colon HM, et al. Mortality among Hispanic drug users in Puerto Rico. P R Health Sci J. 2003;22:369–376. [PubMed] [Google Scholar]
- 31.Deren S, Oliver-Velez D, Finlinson A, et al. Integrating qualitative and quantitative methods: comparing HIV-related risk behaviors among Puerto Rican drug users in Puerto Rico and New York. Subst Use Misuse. 2003;38:1–24. doi: 10.1081/JA-120016563. [DOI] [PubMed] [Google Scholar]
- 32.Oliver-Velez D, Finlinson HA, Deren S, et al. Mapping the air-bridge locations: the application of ethnographic mapping techniques to dual-site study of HIV risk behavior determinants in East Harlem, New York and Bayamón, Puerto Rico. Hum Organ. 2002;61:262–276. [Google Scholar]
- 33.Radloff LS. A CES-D scale: a self-report depression scale for research in the general population. J Appl Meas. 1977;1:385–401. [Google Scholar]
- 34.Vera M, Alegria M, Freeman D, Robles RR, Rios R, Rios CF. Depressive symptoms among Puerto Ricans: island poor compared with residents of the New York City area. Am J Epidemiol. 1991;134:502–510. doi: 10.1093/oxfordjournals.aje.a116122. [DOI] [PubMed] [Google Scholar]
- 35.Colon HM, Robles RR, Deren S, et al. Between-city variation in frequency of injection among Puerto Rican injection drug users: East Harlem, New York, and Bayamon, Puerto Rico. J Acquir Immune Defic Syndr. 2001;27:405–413. doi: 10.1097/00126334-200108010-00012. [DOI] [PubMed] [Google Scholar]
- 36.Bureau of Vital Statistics. Summary of Vital Statistics 2002: The City of New York. New York City Department of Health and Mental Hygiene; 2003.
- 37.Informe anual de estadísticas vitales de Puerto Rico. San Juan, Puerto Rico: Departamento de Salud; 1995. [Google Scholar]
- 38.Sahai H, Khurshid A. Statistics in Epidemiology: Methods, Techniques, and Applications. New York: CRC; 1996. [Google Scholar]
- 39.Cox DR, Oakes DO. Analysis of Survival Data. London: Chapman & Hall; 1984. [Google Scholar]
- 40.Colon HM, Reyes JC, Matos TE, Robles RR. Drug induced deaths is Puerto Rico 1990–2000: Evidence of a public health emergency. Poster presented at the 131 Annual Meeting of the American Public Health Association, November 2003.
- 41.Uniform Crime Report: Crime in the United Sates, 2001. Washington, DC: US Department of Justice; 2002. [Google Scholar]
- 42.Mayor AM, Gómez MA, Ríos-Olivares E, Hunter-Mellado R. Mortality trends of HIV-infected patients after introduction of highly active antiretroviral therapy: analysis of a cohort of 3,322 HIV-infected persons. Ethn Dis. 2005;15(Suppl 5):57–62. [PubMed] [Google Scholar]
- 43.Appel PW, Joseph H, Richman BL. Causes and rates of death among methadone maintenance patients before and after the onset of the HIV/AIDS epidemic. Mt Sinai J Med. 2000;67:444–451. [PubMed] [Google Scholar]
- 44.Friedman LN, Williams MT, Singh TP, Frieden TR. Tuberculosis, AIDS, and death among substance abusers on welfare in New York City. N Engl J Med. 1996;334:828–833. doi: 10.1056/NEJM199603283341304. [DOI] [PubMed] [Google Scholar]
- 45.Deren S, Kang SY, Colon HM, Andia JF, Robles RR. HIV incidence among high-risk Puerto Rican drug users: a comparison of East Harlem, New York, and Bayamon, Puerto Rico. J Acquir Immune Defic Syndr. 2004;36:1067–1074. doi: 10.1097/00126334-200408150-00010. [DOI] [PubMed] [Google Scholar]
- 46.Robles RR, Matos TD, Colon HM, et al. Determinants of health care use among Puerto Rican drug users in Puerto Rico and New York City. Clin Infect Dis. 2003;37(Suppl 5):S392–S403. doi: 10.1086/377552. [DOI] [PubMed] [Google Scholar]
- 47.Gossop M, Stewart D, Treacy S, Marsden J. A prospective study of mortality among drug misusers during a 4-year period after seeking treatment. Addiction. 2002;97:39–47. doi: 10.1046/j.1360-0443.2002.00079.x. [DOI] [PubMed] [Google Scholar]
- 48.O'Driscoll PT, McGough J, Hagan H, Thiede H, Critchlow C, Alexander ER. Predictors of accidental fatal drug overdose among a cohort of injection drug users. Am J Public Health. 2001;91:984–987. doi: 10.2105/AJPH.91.6.984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Piketty C, Castiel P, Giral P, et al. Lack of legal income is strongly associated with an increased risk of AIDS and death in HIV-infected injecting drug users. AIDS Care. 1999;11:429–436. doi: 10.1080/09540129947802. [DOI] [PubMed] [Google Scholar]
- 50.Weatherby NL, Needle R, Cesari H, Booth RE. Validity of self-reported drug use among injection drug users and crack cocaine users recruited through street outreach. Eval Program Plann. 1994;17:347–355. doi: 10.1016/0149-7189(94)90035-3. [DOI] [Google Scholar]
- 51.Dowling GS, Johnson ME, Fisher DG, Needle R. Reliability of drug users' self-reported HIV risk behaviors and validity of self-reported recent drug use. Assessment. 1994;1:383–392. [Google Scholar]
- 52.Buka SL. Disparities in health status and substance use: ethnicity and socioeconomic factors. Public Health Rep. 2002;117(Suppl 1):S118–S125. [PMC free article] [PubMed] [Google Scholar]
- 53.Zambrana RE, Carter-Pokras O. Health data issues for Hispanics: implications for public health research. J Health Care Poor Underserved. 2001;12:20–34. doi: 10.1353/hpu.2010.0547. [DOI] [PubMed] [Google Scholar]
- 54.Palacio H, Shiboski CH, Yelin EH, Hessol NA, Greenblatt RM. Access to and utilization of primary care services among HIV-infected women. J Acquir Immune Defic Syndr. 1999;21:293–300. doi: 10.1097/00126334-199908010-00006. [DOI] [PubMed] [Google Scholar]
- 55.Solomon L, Stein M, Flynn C, et al. Health services use by urban women with or at risk of HIV-1 infection: the HIV epidemiology research study (HERS) J Acquir Immune Defic Syndr Hum Retrovirol. 1998;17:253–261. doi: 10.1097/00042560-199803010-00011. [DOI] [PubMed] [Google Scholar]
- 56.Sanders-Phillips K. The ecology of urban violence: its relationship to health promotion behaviors in low-income black and Latino communities. Am J Health Promot. 1996;10:308–317. doi: 10.4278/0890-1171-10.4.308. [DOI] [PubMed] [Google Scholar]
- 57.Bauer HM, Rodriguez MA, Quiroga SS, Flores-Ortiz YG. Barriers to health care for abused Latina and Asian immigrant women. J Health Care Poor Underserved. 2000;11:33–44. doi: 10.1353/hpu.2010.0590. [DOI] [PubMed] [Google Scholar]