Abstract
Research on behavioral HIV risk reduction interventions for injection drug users (IDUs) has focused on primary outcomes (e.g., reduced injection drug use, increased condom use) but has not fully examined the respective roles played by intervention components on these primary outcomes. In this paper, we present a structural equation modeling (SEM) approach in which we specify the causal pathways leading from theory-based intervention components to risk reduction outcomes among a sample of primarily IDUs (n = 226) participating in an inner-city community-based methadone maintenance program. Similar pathways were found leading to both drug- and sexual-related risk reduction outcomes. Findings suggest the importance of targeting participants' risk reduction motivation and behavioral skills versus employing more passive informational strategies. Findings also indicate that our intervention may be optimized by focusing more on participants' risk reduction motivation within the sexual-related content and placing equivalent emphasis on participants' risk reduction knowledge, motivation, and behavioral skills within the drug-related content. By quantifying the specific linkage between intervention components and risk reduction outcomes, our SEM findings offer empirical guidance for optimizing this intervention. This strategy may also serve as a useful theory- and data-driven means to inform the refinement of other behavioral interventions.
Keywords: Behavioral intervention, HIV risk reduction, Injection drug use, Structural equation modeling
Introduction
In the U.S. alone, 950,000 people live with HIV infection, and 450,000 people have died due to AIDS thus far.1,2 Injection drug users (IDUs) remain a target population as they continue to represent a critical vector for the transmission of new HIV infections,3,4 which occurs primarily through drug- and sexual-related risk behaviors that are highly preventable. As there is currently no vaccine to prevent new HIV infections, behavioral interventions are our primary intervention tools.5 A small number of behavioral interventions have now demonstrated evidence of effectiveness within target populations including IDUs (http://www.effectiveinterventions.org). However, research to date has yielded little evidence about what specific intervention strategies are most crucial to the outcome of different risk behaviors among IDUs or, in effect, how to optimize these types of interventions.
The research literature devoted to HIV prevention for IDUs has greatly expanded; however, much of it is either relatively imprecise, qualitative in nature,5–7 or is only partially applicable to IDUs as a distinct risk group. For instance, studies characterized as relevant to IDUs may only include a minority of participants who report a positive history of injecting drugs8–12 while other studies may sample solely from active IDUs.13,14 In addition, research that reports both sexual- and drug-related HIV risk outcomes among IDUs tends to be inconsistent. Compared with drug-related HIV risk outcomes, sexual-related outcomes among IDUs are either infrequently reported or equivocal when examining individual studies. Thus, it has not been possible to identify strategies that are most crucial to reducing sexual- vs. drug-related HIV risk behaviors. In turn, we have been unable to develop empirically guided interventions that optimally address the full range of HIV risk behaviors that often characterize people who inject drugs.
In an effort to fill this void, we recently conducted a meta-analysis in which a range of drug- and sexual-related HIV risk outcomes were examined across randomized controlled trials (RCTs) evaluating behavioral HIV risk reduction interventions targeting IDUs.15 Of particular relevance to the present study, findings point to the importance of addressing both drug- and sexual-related HIV risk behaviors and doing so in a balanced manner. Although there is accumulating evidence that more effective risk reduction interventions for IDUs tend to incorporate an equivalent focus on drug- and sexual-related risks,3,4 research to date has not been designed to specify the role played by particular components that comprise such interventions. Therefore, our objective in the present study was to implement a structural equation modeling (SEM) approach to specify the pathways leading from our intervention components to the risk reduction outcomes that we observed. In the following section, we outline the theoretical basis for our analytical approach.
The IMB Model of HIV Preventative Behavior
The Information–Motivation–Behavioral (IMB) skills model of health behavior change,16 which served as the framework for our SEM approach, asserts that HIV risk reduction information, motivation, and behavioral skills are the key determinants of HIV risk reduction behavior. First, HIV prevention information that is directly relevant to HIV preventive behavior is a prerequisite for risk reduction behavior. Such information can include specific facts about HIV transmission (e.g., “A used syringe that appears clean can still transmit HIV”) and HIV prevention (e.g., “Oral sex is safer than vaginal or anal sex”). The information component of the model also includes critical HIV prevention heuristics—simple decision rules that permit individuals to make relatively automatic and cognitively effortless (but often incorrect) decisions about a partner's HIV status and, thus, about whether or not to engage in HIV preventive behavior. Endorsement of such heuristics has a strong negative association with subsequent HIV risk reduction practices.17–20 In addition, individuals often operate on the basis of implicit theories of HIV risk that, for instance, may hold that it is possible to detect and avoid HIV transmission risk based on assessing a person's characteristics such as dress, demeanor, personality, or social acquaintances. When a person is deemed unlikely to be HIV-infected, for example, based on implicit personality theories, HIV risk reduction behaviors are less likely to follow.18
Second, an individual's motivation to reduce HIV risk is another critical determinant of risk reduction behavior and influences whether the individual will be inclined to act on their knowledge regarding HIV risk and risk reduction. Among the many sources of motivation, HIV risk reduction motivation includes personal motivation specific to practicing risk reduction (e.g., attitudes about personally enacting specific HIV risk reduction behaviors)21 and social motivation to engage in HIV risk reduction (e.g., perception of social norms for performing such acts).21 Thus, an individual is expected to vary in terms of personal motivation to practice prevention (e.g., attitudes about never sharing needles or always using condoms) and in terms of social motivation to reduce HIV risk behavior (e.g., expectations for social acceptance or rejection for sharing needles or using condoms).
Third, a person's behavioral skills for performing HIV risk reduction acts are a final prerequisite for risk reduction behavior according to the model, and these determine the extent to which even a well-informed and -motivated person will be competent at reducing HIV risk behavior. The behavioral skills component of the IMB model is composed of an individual's objective ability and perceived self-efficacy concerning performance of the sequence of HIV-preventive behaviors that is involved in effective risk reduction practice.16,22–24 Behavioral skills involved in HIV prevention for IDUs, for instance, can include objective and perceived skills needed to obtain new needles or condoms, to negotiate and maintain abstinence from intercourse, and to engage in consistent condom use or safer needle use behaviors.
The IMB model specifies that HIV risk reduction information and motivation work primarily through HIV risk reduction behavioral skills to influence HIV preventive behavior. In essence, effects of HIV prevention information and motivation are expressed mainly as a result of using HIV risk reduction behavioral skills that are applied in the initiation and maintenance of HIV risk reduction behavior. The model also specifies that HIV risk reduction information and motivation may have direct effects on risk reduction behavior, particularly when complex or novel behavioral skills are not necessary to influence HIV risk reduction outcomes. For example, while in drug treatment, an individual may be relatively motivated to avoid becoming HIV-infected and withdraw from relationships that, in the past, have led to risk behavior until he/she has learned the risk reduction skills needed to be in such situations more safely. Importantly, information and motivation are regarded as generally independent constructs in the model. Thus, well-informed individuals are not necessarily highly motivated to practice risk reduction, and highly motivated individuals are not always well informed about HIV risk reduction.16,25
The IMB model's information, motivation, and behavioral skills constructs are regarded as highly generalizeable determinants of HIV preventive behavior across risk populations and across HIV-risk reduction behaviors.16 However, it is assumed that specific interventions based on this theoretical model will contain content that is sufficiently tailored to meet the particular risk reduction needs of specific target populations and their respective risk behaviors. Following this logic, particular model constructs, and particular causal pathways among them, will emerge as more or less powerful determinants of HIV risk reduction practices for different risk populations and their risk reduction behaviors.16,17 The model indicates the need to tailor intervention content within each of the IMB constructs in order to optimize their impact on different target populations. Our SEM approach was designed to establish how the IMB constructs were related to our observed risk reduction outcomes and, on this basis, to inform our efforts to optimize the potency of these intervention components.
Materials and Methods
We analyzed data that were obtained following the deployment of a brief group level HIV risk reduction intervention within a total of 37 ongoing treatment groups at methadone maintenance facilities owned by the APT Foundation, Inc., in New Haven, Connecticut. The APT Foundation clinics serve approximately 1,385 patients, 39% of whom are female and 65% of whom can be classified as economically disadvantaged (i.e., receiving some type of entitlement such as Title 19, SAGA, or SSI/DI). Overall, these clinics serve 28% HIV-positive, 15% status unknown, and 57% HIV-negative individuals. The intervention from which our study data were obtained was the Community-friendly Health Recovery Program (CHRP),26 which is an adapted, substantially abbreviated, form of the comprehensive evidence-based Holistic Health Recovery Program (HHRP).3,4,27 The CHRP intervention consisted of four weekly group meetings led by two bachelor's level facilitators, each of which lasted approximately 50-min. The significant effects associated with the intervention have been reported elsewhere26 and, thus, were not the focus of this report. Rather, our focus was on establishing the causal pathways (e.g., the relative importance of various intervention components) that led to the observed risk reduction outcomes, as this information could be used to optimize the CHRP intervention.
Information, motivation, and behavioral skills have been well established as critical intervention components for reducing HIV risk behavior.17,18 Yet, the pathways leading from all three of those constructs to HIV risk reduction outcomes have rarely, if ever, been examined with regard to IDUs. Therefore, the relative importance of conveying risk reduction information versus focusing intervention content on participants' motivation or risk reduction behavioral skills, for example, is unclear. We sought to clarify this question through our models.
Participants
Participants were 226 patients who were enrolled in a methadone maintenance program at the APT Foundation, Inc., in New Haven, Connecticut. The characteristics of the sample of participants were as follows: recent injection drug users (72.6%), male (51.1%), never married (50.7%), unemployed (56.0%), English speaking (89.8%), and age ranging from 19 to 58 years (mean age was 38.6 years). Participants were predominantly Caucasian (68.4%), followed by Blacks (17.8%), Hispanics (12.9%), and American Indians (0.9%). The intervention study protocol was approved by the Investigational Review Board (IRB) at the University of Connecticut and by a research review board at the APT Foundation, Inc., and all participants provided signed informed consent prior to their participation.
Measures
Several items from the Risk Assessment Battery28 (RAB) were used to assess participants' sexual- and drug-related HIV risk behavior. The scale required participants to categorize and quantify their drug use and sexual activity during the prior week. Drug use related items included how they used drugs, whether they used new syringes or cleaned syringes and, if so, how they cleaned them, and whether they shared syringes, rinse water, cooker, or cotton. Sexual activity related items assessed whether they used a condom and, if not, whether it was due to their abstinence from sexual activity.
Based on the Information–Motivation–Behavior skills16 model of health behavior change, a brief assessment that covered the following domains was measured: drug- and sexual-related HIV-risk reduction knowledge (Information component), personal and social motivation to reduce drug and sexual-related HIV risk behavior (Motivation component), and self-efficacy about reducing drug- and sexual-related HIV risk behavior (Behavioral skills component). Four items were used to assess knowledge about safer sex and safer injection drug use (e.g., “If an HIV+ person only has sex with another HIV+ person, they don't need to use condom”; “If an HIV+ person shared needles with another HIV+ person, they don't need to clean the needles.”). Six items examined participants' motivation to use condoms and clean needles, intentions to engage in safer sexual activity and safer injection drug use practices, and perception of significant others' beliefs about the importance of using condoms and using clean needles. Four items assessed participants' behavioral skills in the form of their self-efficacy about abstaining from sexual activity and using a condom and about abstaining from injecting drugs and using clean needles. This brief assessment instrument has been used in a randomized trial of what is now recognized as an evidence-based intervention (OPTIONS).29 The measure has been used to expeditiously inform clinicians about HIV-related information, motivation, and behavioral skills deficits among intervention participants.
Based on the brief IMB-based assessment and two quantitative items from the RAB, confirmatory factor analyses based on AMOS 5.0 were used to test the IMB model on drug- and sexual-related risk reduction outcome measures. The model indices for sexual-related outcomes were acceptable, χ2(11) = 7.02, p = 0.54, CFI = 1.00, RMSEA = 0.00, as were those for drug-related outcomes, χ2(11) = 12.13, p = 0.44, CFI = 1.00, RMSEA = 0.00.
Results
In order to provide a proper context for our present study, we should briefly summarize the relevant results from our outcome analyses, which have been reported elsewhere.26 A repeated measures analysis of variance was performed with Intervention (pre- vs. post-intervention) as a within-subjects variable and with HIV Risk Group (high, moderate, and low—based on composite HIV risk scores at pre-test) as between-subjects variables on all variables pertaining to sexual- and drug-related outcomes. Analyses of sexual- and drug-related risk reduction outcomes were performed separately so that we could compare outcomes across these HIV risk domains. A positive main effect was found for Intervention on drug-related risk reduction, F(1, 223) = 9.81, p < 0.01, as well as for HIV Risk Group, F(10, 424) = 10.76, p < 0.001. Similarly, a positive main effect was found for Intervention on sexual-related risk reduction, F(5, 211) = 10.60, p < 0.001, as well as for HIV Risk Group, F(10, 424) = 21.17, p < 0.001. Of particular interest, these main effects were superseded by significant Intervention × HIV Risk Group interactions, F(10, 424) = 9.05, p < 0.001 for drug-related risk reduction and F(10, 424) = 9.40, p < 0.001 for sexual-related risk reduction, primarily indicating that participants at higher risk for HIV tended to show greater improvement. Thus, in the present study, we sought to examine the pathways leading to improvement.
Our data analytic approach involved testing separate structural equation models for drug- vs. sexual-related HIV risk behavior outcomes based on AMOS 5.0 (Table 1 displays a description of variables). This approach was selected in order to capture possible differences between the pathways leading to drug- vs. sexual-related risk reduction, respectively, as implied by recent research.15 Using the IMB framework,16 pathways were examined among HIV-related knowledge, personal and social motivation, self-efficacy, and HIV risk behavior (Figures 1 and 2). We expected to find positive paths leading from HIV knowledge and social motivation to personal motivation, respectively. In turn, we expected greater personal motivation to be linked with greater self-efficacy regarding HIV risk reduction behavioral skills. Finally, we expected higher levels of self-efficacy to be associated with enhanced risk reduction outcomes (e.g., reduced frequency of injecting behavior, increased frequency of condom use).
Table 1.
Correlation matrix, means, and standard deviations in structural equation models
| Information | Social motivation | Personal motivation | Behavioral skills | Behavior | |
|---|---|---|---|---|---|
| Drug-risk reduction modela | |||||
| Sample size | 226 | 226 | 226 | 226 | 225 |
| Correlation matrix | |||||
| Information (knowledge) | −0.01 | 0.17* | 0.15* | 0.01 | |
| Social motivation | 0.02 | 0.39*** | 0.04 | −0.04 | |
| Personal motivation | 0.05 | 0.62*** | 0.16* | −0.07 | |
| Behavioral skills | 0.07 | 0.08 | 0.07 | 0.16* | |
| Behavior | −0.07 | −0.03 | −0.06 | 0.10 | |
| Means (pre) | 83.85% | 4.56 | 4.67 | 4.28 | 5.91 |
| Standard deviations (pre) | 28.17% | 0.95 | 0.60 | 0.88 | 0.39 |
| Means (post) | 91.15% | 4.61 | 4.83 | 4.35 | 5.93 |
| Standard deviations (post) | 21.80% | 0.97 | 0.46 | 0.87 | 0.32 |
| Sexual-risk reduction modela | |||||
| Sample size | 226 | 226 | 226 | 226 | 221 |
| Correlation matrix | |||||
| Information (knowledge) | 0.04 | −0.06 | −0.10 | −0.19*** | |
| Social motivation | −0.07 | 0.44*** | 0.17* | 0.13 | |
| Personal motivation | −0.13* | 0.36*** | 0.33*** | 0.40*** | |
| Behavioral skills | −0.06 | 0.19** | 0.36*** | 0.30*** | |
| Behavior | −0.10 | 0.11 | 0.31*** | 0.24*** | |
| Means (pre) | 72.57% | 4.49 | 4.26 | 3.44 | 4.43 |
| Standard deviations (pre) | 31.97% | 1.03 | 0.93 | 1.30 | 1.92 |
| Means (post) | 81.42% | 4.76 | 4.53 | 3.50 | 4.64 |
| Standard deviations (post) | 25.99% | 0.68 | 0.76 | 1.22 | 1.86 |
*p < 0.05.
**p < 0.01.
***p < 0.001.
aNumbers in upper diagonal indicate correlations in pre-test scores, whereas numbers in lower diagonal indicate correlations in post-test scores.
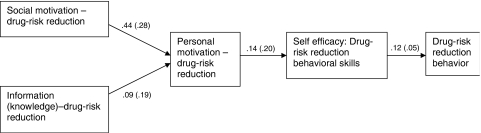
Figure 1.
Pathways to drug-risk reduction behavior: a fitting model, χ216 = 14.82, p = 0.54. CFI = 1.00, RMSEA = 0.000 (0.000–0.041)1.
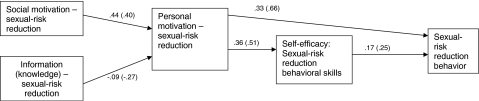
Figure 2.
Pathways to sexual-risk reduction behavior: a good fitting model, χ215 = 13.89, p = 0.53. CFI = 1.00, RMSEA = 0.000 (0.000–0.042).
A Model of Drug-Related HIV Risk Reduction
The model specifying the pathways that led to drug-related HIV risk reduction behavior is a good-fitting model, χ2 = 14.82, p = 0.54, GFI =1.00, RMSEA = 0.00, and was found to be stable when considering data from pre- and post-test measurement points (Figure 1). As expected, positive paths were found from drug-related HIV risk reduction knowledge (Beta = 0.09) and social motivation regarding drug-related HIV risk reduction (Beta = 0.44) to personal motivation regarding drug-related HIV risk reduction. This pattern suggests that increased knowledge and social motivation (perceived norms) specific to drug-related HIV risk reduction significantly increases one's personal motivation to reduce drug-related HIV risk behavior.
Also, as expected, personal motivation (Beta = 0.14) was found to be positively linked with HIV risk reduction self-efficacy. Thus, greater personal motivation to reduce drug-related HIV risk was associated with greater self-efficacy in practicing drug-related HIV risk reduction. Greater self-efficacy (Beta = 0.12), in turn, was found to be significantly linked with safer injection drug use outcome behavior.
A Model of Sexual-Related HIV Risk Reduction
Similarly, we tested a model specifying the pathways that led to sexual-related HIV risk reduction behavior (Figure 2). We expected to see positive paths leading from sexual-related HIV risk reduction knowledge and social motivation (perceived norms) about sexual-related risk reduction to personal motivation regarding sexual-related risk reduction. In addition, we predicted that greater personal motivation would be linked with greater self-efficacy to reduce sexual-related HIV risk that, in turn, would be positively linked with reduced sexual-related HIV risk behavior.
After adding one path from personal motivation to sexual-related HIV risk behavior (i.e., condom use behavior), we were able to specify a good fitting model, χ2 = 13.89, p = 0.53, GFI = 1.00, RMSEA = 0.00, which was found to be stable when considering data from pre- and post-test measurement points. As expected, social motivation was positively linked with personal motivation to reduce sexual-related HIV risk (Beta = 0.44). Greater personal motivation was associated with greater self-efficacy for practicing safer sexual behavior (Beta = 0.36). Moreover, both greater personal motivation to practice safer sex and greater self-efficacy for practicing safer sex were associated with a higher frequency of condom use (Beta = 0.33 for personal motivation; Beta = 0.17 for self-efficacy). Unexpectedly, greater sexual-related HIV risk reduction knowledge was somewhat negatively related to participants' personal motivation to practice safer sex (Beta = −0.09).
Discussion
The research literature on risk reduction for IDUs has greatly expanded. Studies to date, however, have not been designed to specify how intervention components individually or collectively lead to HIV risk behavior change. The present study contributes to the literature by taking a structural equation modeling (SEM) approach to quantifying the interrelated roles of theory-based intervention components in drug- and sexual-related risk reduction outcomes.
On a general level, similar causal pathways were found leading to drug- and sexual-related outcomes. Across both risk domains, increased social motivation (perceived norms) to reduce HIV risk was linked with greater personal motivation to reduce risk behavior. Greater personal motivation to reduce risk was associated with higher levels of self-efficacy in practicing HIV risk reduction which, in turn, was related to enhanced risk reduction outcome behavior. In addition, both models suggest the importance of enhancing participants' level of motivation (social and personal) to reduce risk and sharpening risk reduction behavioral skills as opposed to simply providing information about HIV risks. Thus, our findings are consistent with recent reviews15,30 that argue against the exclusive implementation of passive informational strategies (e.g., HIV/AIDS education) and point to the benefit of using active behavioral strategies (e.g., enhancing motivation, teaching risk reduction skills). Our findings are also consistent with recent reviews that indicate the increased potency of interventions that focus equivalently on drug- and sexual-related risk reduction behaviors15 and the advantages inherent in delivering such interventions concurrently with drug treatment.31 A drug treatment environment may produce a synergistic effect on risk reduction outcomes when interventions are integrated into that context. Future research could examine the precise mechanism(s) through which drug treatment influences risk reduction outcomes.
On a more specific level, differences in the causal pathways within the sexual- vs. the drug-related domains may inform future interventions by showing the relative importance of intervention components as applied within each risk domains. For example, HIV knowledge had a differential influence on sexual- vs. drug-related risk reduction (Figures 1 and 2). This may stem from the fact that successful sexual-related risk reduction (e.g., initiating/increasing condom use) may demand substantial cooperation between partners whereas drug-related risk reduction (e.g., reducing injection behavior, not sharing needles/equipment) may not. Future studies could examine whether the failure to translate sexual-related risk reduction knowledge to risk reduction motivation and behavior is impacted by resistance from one's sexual partner.
Finally, the present study may serve as an exemplar of applying an SEM approach as an empirical basis for optimizing the potency of an intervention. For example, one may conclude that the potency of the CHRP intervention would be enhanced by (1) placing equivalent emphasis on all three IMB elements within the drug-related content (Figure 1) and placing increased emphasis on personal and social motivation and decreased emphasis on providing information within the sexual-related content (Figure 2).
The limitations of this study should also be acknowledged. First, our data were obtained from a community-based clinical intervention study that implemented a within-subjects design—with participants serving as their own controls—rather than a more stringent between-subjects randomized design. There are limitations with the use of a within-subjects design, such as experimental artifacts. However, as noted elsewhere,26 among our primary outcomes are objective improvements (e.g., significant gains in participants' knowledge pertaining to both drug- and sexual-related risks) that cannot readily be explained as due to experimental artifacts such as demand characteristics. Moreover, the pattern of results does not indicate biases due to self-reporting. If self-reporting bias were operating, we would expect to find strong effects stemming from personal motivation and relatively weak effects stemming from social motivation since there is no self-serving reason for participants to systematically misrepresent their perceptions of others' motivation to reduce HIV risk. It is also unlikely that external influences led to changes we detected in what are well established as difficult-to-change behaviors.32 In addition, because of the community-based clinical context in which the present study was conducted, we were obliged to use a brief assessment battery29 that covered a relatively short time frame3 and did not capture long-term behavioral patterns. Related to this, we should emphasize that our objective was to optimize the CHRP intervention within community-based treatment programs where significant rates of continued drug- and sex-related HIV risk behavior have been well documented3,4,26,33 and where intervention integration appears promising26; our findings are not intended to generalize to “out-of-treatment” IDUs who may tend to possess different characteristics (e.g., pre-contemplation stage of health behavior change34) that may be more effectively addressed using a different intervention approach.
Notwithstanding the above limitations, this study provides a fresh look at how theory-based components of a community-friendly intervention led to the desired HIV risk reduction outcomes. The findings we have gleaned will inform our efforts to optimize the CHRP intervention for future use. Given the struggle to reduce HIV risk among IDUs,35 and because behavioral interventions remain our primary means for doing so,5 there is a pressing need to optimize the interventions that we deploy. The SEM strategy that we employed in the present study could serve as a useful theory-and data-driven tool to guide the refinement of such interventions.
Acknowledgement
Funding to support this study was provided by the Connecticut Department of Public Health—AIDS Division (DPH Log #2004-154) to Michael M. Copenhaver. Funding to support data analyses and preparation of this manuscript was provided by the National Institute on Drug Abuse, grant K23-DA017015 to Michael M. Copenhaver.
Footnotes
Standardized correlation coefficients (with unstandardized correlation coefficients in parentheses).
Copenhaver and Lee are with the Department of Psychology, Center for Health/HIV Intervention & Prevention (CHIP), University of Connecticut, 2006 Hillside Drive, Unit 1248, Storrs, CT 06269, USA.
References
- 1.Centers for Disease Control and Prevention 2004. Special! Data Request. Available at: http://www.statehealthfacts.kff.org. Accessed August 18, 2004.
- 2.Joint United Nations Programme on HIV/AIDS. Q&A II: basic facts about the AIDS epidemic and its impact, UNAIDS questions and answers. UNAIDS; 2004. Available at: http://www.unaids.org. Accessed August 19, 2004.
- 3.Avants SK, Margolin A, Usubiaga MH, Doebrick C. Targeting HIV-related outcomes with intravenous drug users maintained on methadone: a randomized clinical trial of a harm reduction group therapy. J Subst Abuse Treat. 2004;26:67–78. doi: 10.1016/S0740-5472(03)00159-4. [DOI] [PubMed] [Google Scholar]
- 4.Margolin A, Avants SK, Warburton LA, Hawkins KA, Shi J. A randomized clinical trial of a manual-guided risk reduction intervention for HIV-positive injection drug users. Health Psychol. 1997;22:223–228. doi: 10.1037/0278-6133.22.2.223. [DOI] [PubMed] [Google Scholar]
- 5.Semaan S, Jarlais DC, Sogolow E, Johnson WD, Hedges LV, Ramirez G, Flores SA, Norman L, Sweat MD, Needle R. A meta-analysis of the effect of HIV prevention interventions on the sex behaviors of drug users in the United States. JAIDS. 2002;30:S73–S93. [PubMed] [Google Scholar]
- 6.Strathdee SA, Hogg RS, Martindale SL, Cornelisse PGA, Craib KJP, Montaner JSG, et al. Determinants of sexual risk-taking among young HIV-negative gay men. JAIDS. 1998;19:61–66. doi: 10.1097/00042560-199809010-00010. [DOI] [PubMed] [Google Scholar]
- 7.Vlahov D, Junge B, Brookmeyer R, Cohn S, Riley E, Armenian H, Beilenson P. Reductions in high-risk drug use behaviors among participants in the Baltimore needle exchange program. JAIDS. 1997;16:400–406. doi: 10.1097/00042560-199712150-00014. [DOI] [PubMed] [Google Scholar]
- 8.Coyle SL, Needle RH, Normand J. Outreach-based HIV prevention for injecting drug users: a review of published outcome data. Pub Health Rep. 1998;113(Suppl. 1):19–30. [PMC free article] [PubMed] [Google Scholar]
- 9.Himmelgreen DA, Singer M. HIV, AIDS, and other health risks: findings from a multisite study—an introduction. Am J Drug Alcohol Abuse. 1998;24:187–197. doi: 10.3109/00952999809001708. [DOI] [PubMed] [Google Scholar]
- 10.Kotranski L, Semaan S, Collier K, Lauby J, Halbert J, Feighan K. Effectiveness of an HIV risk reduction counseling intervention for out-of-treatment drug users. AIDS Educ Prev. 1988;10:19–33. [PubMed] [Google Scholar]
- 11.Reikowski DJ. A Behavioral and Cognitive Intervention for AIDS Prevention [dissertation]. Stanford, CA: Stanford University; 1994.
- 12.Malow RM, West JA, Corrigan SA, Pena JM, Cunningham SC. Outcome of psychoeducation for HIV risk reduction. AIDS Educ Prev. 1994;6:113–125. [PubMed] [Google Scholar]
- 13.Baker A, Heather N, Wodak A, Dixon J, Holt P. Evaluation of a cognitive–behavioural intervention for HIV prevention among injecting drug users. AIDS. 1993;7:247–256. doi: 10.1097/00002030-199302000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Calsyn DA, Saxon AJ, Freeman G, Jr., Whittaker S. Ineffectiveness of AIDS education and HIV antibody testing in reducing high-risk behaviors among injection drug users. Am J Publ Health. 1992;82:573–575. doi: 10.2105/AJPH.82.4.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Copenhaver M, Johnson BT, Lee IC, Harman J, Carey M. HIV risk reduction among people who inject drugs: meta-analytic evidence of efficacy. J Subst Abuse Treat. In press 2006. [DOI] [PMC free article] [PubMed]
- 16.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111:455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- 17.Fisher WA, Fisher JD, Harman J. The information–motivation–behavioral skills model: a general social psychological approach to understanding and promoting health behavior. In: Suls J, Wallston KA, editors. Social Psychological Foundations of Health and Illness. Malden, MA: Blackwell; 2003. pp. 82–106. [Google Scholar]
- 18.Fisher JD, Fisher WA. The information–motivation–behavioral skills model. In: DiClemente R, Crosby R, Kegler M, editors. Emerging Theories in Health Promotion Practice and Research. San Francisco, CA: Jossey-Bass; 2002. pp. 40–70. [Google Scholar]
- 19.Hammer J, Fisher JD, Fisher WA. When two heads aren't better than one: AIDS risk behavior in college couples. J Appl Soc Psychol. 1996;26:375–397. doi: 10.1111/j.1559-1816.1996.tb01855.x. [DOI] [Google Scholar]
- 20.Misovich SJ, Fisher JD, Fisher WA. The perceived AIDS-preventive utility of knowing one's partner well: a public health dictum and individuals' risky sexual behavior. Can J Hum Sex. 1996;5:83–90. [Google Scholar]
- 21.Fishbein M, Ajzen I. Belief, Attitude, Intention, and Behavior: An Introduction to Theory and Research. Reading, MA: Addison-Wesley; 1975. [Google Scholar]
- 22.Bandura A. Perceived self-efficacy in the exercise of control over AIDS infection. In: Mays VM, Albee GW, Schneider SM, editors. Primary Prevention of AIDS. Newbury Park, CA: Sage; 1989. pp. 128–141. [Google Scholar]
- 23.Bandura A. Social cognitive theory and exercise of control over HIV infection. In: DiClemente RJ, Peterson JL, editors. Preventing AIDS: Theories and Methods of Behavioral Interventions. New York, NY: Plenum Press; 1994. pp. 25–59. [Google Scholar]
- 24.Kelly J.A., St. Lawrence J.S. AIDS prevention and treatment: psychology's role in the health crisis. Clin Psychol Rev. 1988;8:255–284. doi: 10.1016/0272-7358(88)90091-8. [DOI] [Google Scholar]
- 25.Fisher JD, Fisher WA, Williams SS, Malloy TE. Empirical tests of on information–motivation–behavioral skills model of AIDS preventive behavior. Health Psychol. 1994;13:238–250. doi: 10.1037/0278-6133.13.3.238. [DOI] [PubMed] [Google Scholar]
- 26.Copenhaver M, Lee I, Margolin A. Successfully integrating an HIV risk reduction intervention into a community-based substance abuse treatment program. Am J Drug Alcohol Abuse. In press 2006. [DOI] [PubMed]
- 27.Centers for Disease Control and Prevention. Cases of HIV infection and AIDS in the United States. HIV/AIDS Surveillance Report. Atlanta, Georgia: US Department of Health and Human Services, CDC; 2003.
- 28.Metzger D, Woody GE, Navaline H, et al. The Risk Assessment Battery (RAB): validity and reliability. Presented at: The Sixth Annual Meeting of National Cooperative Vaccine Development Group for AIDS; October 30-November 4, 1993; Alexandria, Virginia.
- 29.Fisher JD, Cornman DH, Osborn CY, Amico KR, Fisher WA, Friedland GA. Clinician-initiated HIV risk reduction intervention for HIV-positive persons: formative research, acceptability, and fidelity of the OPTIONS project. JAIDS. 2004;37:S78–S87. doi: 10.1097/01.qai.0000140605.51640.5c. [DOI] [PubMed] [Google Scholar]
- 30.Albarracín D. A test of major assumptions about behavior change: a comprehensive look at HIV prevention since the beginning of the epidemic. Paper presented at: The Center for Health/HIV Intervention and Prevention (CHIP), University of Connecticut; 2004; Storrs, Connecticut.
- 31.Metzger DS, Navaline H, Woody G. Drug abuse treatment as AIDS prevention. Pub Health Rep. 1998;113:97–106. [PMC free article] [PubMed] [Google Scholar]
- 32.Pigott TD. Missing predictors in models of effect size. Eval Health Prof. 2001;24:277–307. doi: 10.1177/01632780122034920. [DOI] [PubMed] [Google Scholar]
- 33.Avants SK, Warburton LA, Hawkins KA, Margolin A. Continuation of high-risk behavior by HIV-positive drug users: treatment implications. J Subst Abuse Treat. 2001;19(1):15–22. doi: 10.1016/S0740-5472(99)00092-6. [DOI] [PubMed] [Google Scholar]
- 34.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: applications to addictive behaviors. Am Psychol. 1992;47:1102–1114. doi: 10.1037/0003-066X.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 35.Copenhaver M, Fisher JD. Experts outline ways to decrease the decade-long yearly rate of 40,000 new HIV infections in the U.S. AIDS Behav. In press DOI 10.1007/s10461-005-9034-x 2006. [DOI] [PubMed]