Abstract
JNK signaling has been implicated in the developmental morphogenesis of epithelial organs. In this study we employed a compound deletion of the murine Jnk1 and Jnk2 genes in the mammary gland to evaluate the requirement for these ubiquitously expressed genes in breast development and tumorigenesis. JNK1/2 was not required for breast epithelial cell proliferation or motility. However, JNK1/2 deficiency caused increased branching morphogenesis and defects in the clearance of lumenal epithelial cells. In the setting of breast cancer development, JNK1/2 deficiency significantly increased tumor formation. Together, these findings established that JNK signaling is required for normal mammary gland development and that it has a suppressive role in mammary tumorigenesis.
Introduction
The formation of epithelial organs requires the co-ordinated growth and movement of epithelial cell sheets. These developmental processes are critically regulated by many mechanisms, including cytokine and endocrine signal transduction pathways. One signaling pathway that has been implicated in epithelial organ morphogenesis is the cJun NH2-terminal kinase (JNK) signaling pathway (1, 2). Thus, genetic analysis of Drosophila demonstrates that JNK is essential for the morphogenetic epithelial cell movements that occur during dorsal closure (3), thoracic closure (4), imaginal disc development (5), and formation of the egg dorsal appendages and micropyle (6). Studies of mammalian development demonstrate that JNK is required for closure of the optic fissure (7), eyelid closure (8, 9), and neural tube closure (10). Key molecular mechanisms that may underly these processes include a requirement of JNK for paxillin phosphorylation and epithelial cell motility (11) and a requirement of JNK for actin polymerization-dependent cell protrusions at the leading edge of the epithelial cell sheet (12). An understanding of the role of JNK in these developmental processes is important because the mechanisms may be relevant to both normal physiology and to disease states (1, 2).
The purpose of this study was to test whether JNK is required for mammary gland development (13). Indeed, JNK may play a critical role in morphogenesis of the breast epithelium (14, 15). These authors report that the drug SP600125 inhibits both JNK activity and lumenal clearance of mammary epithelial cells (14, 15). However, SP600125 exhibits poor selectivity for JNK (16). It is therefore unclear whether JNK inhibition mediates the effects of SP600125 on morphogenesis of the breast epithelium. Moreover, detailed studies of breast epithelium development (17) indicate that this morphogenetic process differs substantially from other epithelial morphogenetic movements that are known to be JNK-dependent (1, 2). Thus, JNK is required for shape changes in the cells that form the leading edge of the epithelial cell sheet prior to co-ordinated cell movements (12). In contrast, elongating mammary epithelial cell ducts form a multi-layer epithelium that moves co-ordinately without extension of leading edge cells (17). Whether JNK contributes to this process during mammary gland development is unclear.
The JNK protein kinase in mammals is encoded by two ubiquitously expressed genes (Jnk1 and Jnk2) and by a third gene (Jnk3) that is selectively expressed in the brain (1). We have not detected developmental defects in mammary gland development in Jnk1−/− mice or Jnk2−/− mice (18). Since JNK1 and JNK2 display partially redundant functions (19, 20), we examined the effect of compound deficiency of JNK1 plus JNK2. Compound Jnk1−/− Jnk2−/− mice die during embryonic development (10). We therefore employed a conditional gene ablation strategy. This experimental approach enabled examination of the role of JNK in primary cultures of mammary epithelial cells and mammary gland organoids in vitro. Furthermore, transplantation assays allowed analysis of the role of JNK in mammary gland development in vivo. We report that JNK is not required for mammary epithelial cell motility or formation of mammary epithelial cell ducts. However, JNK contributes to branching morphogenesis of the mammary epithelium and is required for normal lumenal clearance of epithelial cells. Moreover, studies of mammary carcinogenesis demonstrate that JNK-deficiency causes significantly increased breast cancer. Together, these observations indicate that JNK may play an important role in both mammary gland development and mammary carcinoma formation.
Materials and Methods
Mice
We have described Jnk2−/− mice (21) and mice with conditional expression of Jnk1 (22). Nude mice (strain NU/J (Stock # 002019)), mice with conditional expression of KRasG12D (23) (strain B6.129S4-Krastm4Tyj/J (Stock # 008179)), mice with conditional expression of Trp53 (24) (strain B6.129P2-Trp53tm1Brn/J (Stock # 008462)), mice expressing 4-hydroxy-tamoxifen-stimulated Cre (25) (strain B6;129-Gt(ROSA)26Sortm1(cre/ERT)Nat/J (Stock # 004847)), and Villin-Cre mice (26) (strain B6.SJL-Tg(Vil-cre)997Gum/J (Stock # 004586)) were obtained from the Jackson Laboratory. The mice used in this study were backcrossed to the C57BL/6 strain (Jackson Laboratories) and were housed in a facility accredited by the American Association for Laboratory Animal Care. The Institutional Animal Care and Use Committee of the University of Massachusetts approved all studies using animals.
Genotype analysis
Genotype analysis was performed by PCR using genomic DNA as the template. The Jnk1+ (1.5 kb), Jnk1LoxP (1.1kb) and Jnk1Δ (0.4kb) alleles were identified using the amplimers 5’-CCTCAGGAAGAAAGGGCTTATTTC-3’ and 5’-GAACCACTGTTCCAATTTCCATCC-3’. The wild-type Jnk2 (400 bp) and knockout Jnk2 (270 bp) alleles were identified using the amplimers 5’-GGAGCCCGATAGTATCGAGTTACC-3’, 5’-GTTAGACAATCCCAGAGGTTGTGTG-3’, and 5’-CCAGCTCATTCCTCCACTCATG-3’. The wild-type Trp53 (288 bp) and Trp53LoxP (370 bp) alleles were identified using the amplimers 5’-AGCACATAGGAGGCAGAGAC-3’ and 5’-CACAAAAACAGGTTAAACCCAG-3’. The Trp53Δ (612 bp) allele was identified using the amplimers 5’-CACAAAAACAGGTTAAACCCAG-3’ and 5’-GAAGACAGAAAAGGGGAGGG-3’. The wild-type KRas (285 bp), KRasG12D (315 bp), and LoxP-Stop-LoxP-KRasG12D (600 bp) alleles were identified using the amplimers 5’-GGGTAGGTGTTGGGATAGCTG-3’ and 5’-TCCGAATTCAGTGACTACAGATGTACAGAG-3’. The Rosa26 (600 bp) and Rosa26-CreERT (300 bp) alleles were identified using the amplimers 5’-GCGAAGAGTTTGTCCTCAACC-3’, 5’-GGAGCGGGAGAAATGGATATG-3’, and 5’-AAAGTCGCTCTGAGTTGTTAT-3’. The Villin-Cre allele (450 bp) was detected using the amplimers 5’-TTACTGACCGTACACCAAATTTGCCTGC-3’ and 5’-CCTGGCAGCGATCGCTATTTTCCATGAGTG-3’.
Cre-mediated recombination
Mice were treated with tamoxifen (Sigma, T5648) to activate Cre-mediated recombination in animals with an inducible Cre recombinase (strain B6;129-Gt(ROSA)26Sortm1(cre/ERT)Nat/J). The tamoxifen was dissolved in sunflower seed oil (10 mg/mL). Mice were treated by intraperitoneal injection with 1 mg tamoxifen each day for three consecutive days.
Mammary gland transplantation assays
Transplantation assays were performed using procedures described previously (27). Donor mice were euthanized and 1mm3 fragments of the fourth inguinal mammary glands were removed aseptically and stored in DMEM on ice. Host mice (3 – 4 week old female nude mice) were anesthetized. The fourth inguinal mammary gland on one side was excised, a small pocket was formed in the cleared fat pad proximal to the inguinal lymph node, and a fragment of donor mammary tissue was placed in the pocket. The same procedure was performed on the contralateral side. Each host mouse was transplanted with both Control and JNK-deficient mammary tissue.
Results
Isolation of JNK-deficient mammary epithelial cells
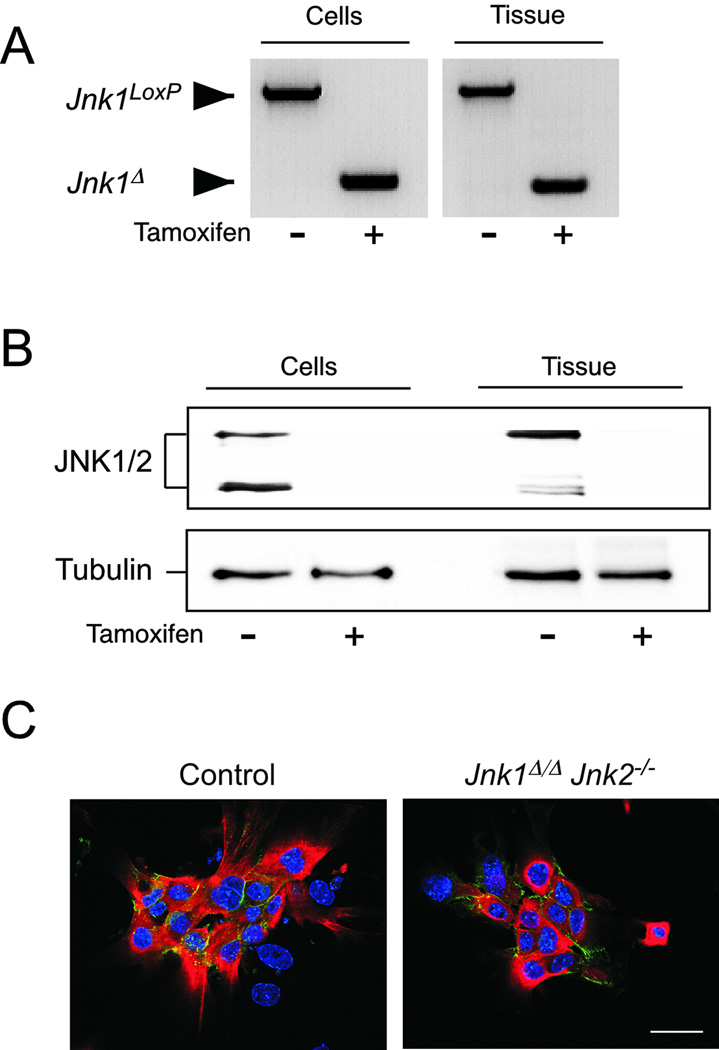
The Jnk1 and Jnk2 genes are expressed in mammary epithelial cells. We employed a conditional gene ablation strategy to create mice with deficiency of JNK1 plus JNK2. We found that Jnk1LoxP/LoxP Jnk2−/− CreERT mice were viable. These mice express a 4-hydroxy-tamoxifen-stimulated Cre recombinase. We treated the Jnk1LoxP/LoxP Jnk2−/− CreERT mice with tamoxifen, isolated mammary tissue, and prepared primary mammary epithelial cell cultures (Figure S1). Genotype analysis of genomic DNA prepared from mammary tissue and cultured epithelial cells demonstrated that tamoxifen caused ablation of the conditional Jnk1 gene (Figure 1A). Immunoblot analysis confirmed that JNK protein was not detected in mammary tissues or epithelial cells of Jnk1Δ/Δ Jnk2−/− mice (Figure 1B).
Figure 1. JNK-deficient mammary epithelial cells.
A,B) Jnk1LoxP/LoxP Jnk2−/− CreERT mice treated without or with tamoxifen in vivo were used to prepare mammary gland extracts and primary mammary gland epithelial cells. Genomic DNA was examined by PCR to detect Jnk1LoxP and Jnk1Δ alleles (A). The expression of JNK and α-Tubulin was examined by immunoblot analysis (B).
C) Primary cultures of CreERT (Control) and Jnk1Δ/Δ Jnk2−/− CreERT mammary epithelial cells prepared from tamoxifen-treated mice were examined by immunofluorescence analysis by probing with antibodies to pan-cytokeratin (red) and E-cadherin (green). DNA was stained with DAPI (blue). Representative images are shown.
To examine the effect of JNK-deficiency on primary mammary epithelial cells, we compared cultures of cells prepared from Control mice (CreERT) and Jnk1LoxP/LoxP Jnk2−/− CreERT mice following treatment with tamoxifen. The epithelial cells were identified by immunofluorescence analysis by staining with antibodies to pan-cytokeratin and E-cadherin. We did not detect an effect of JNK-deficiency on the morphology of primary mammary epithelial cells (Figure 1C).
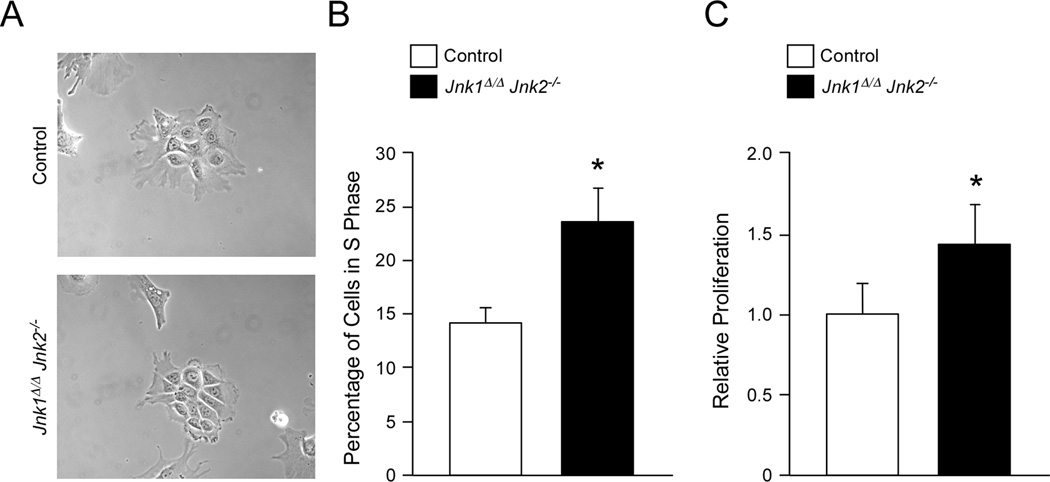
Role of JNK in mammary epithelial cell proliferation
It is established that compound JNK-deficiency in primary mouse embryonic fibroblasts (MEF) causes p53-dependent senescence (20, 22). Growth of Jnk1−/− Jnk2−/− MEF requires loss-of-function of the p53 pathway (22). We therefore anticipated that Jnk1Δ/Δ Jnk2−/− primary mammary epithelial cells would also exhibit reduced growth and senescence. However, the morphology of JNK-deficient epithelial cells was not typical of senescent cells (Figure 2A). Moreover, cell cycle analysis by flow cytometry did not demonstrate a requirement of JNK for proliferation (Figure 2B). Indeed, Jnk1Δ/Δ Jnk2−/− primary mammary epithelial cells incorporated significantly more BrdU than Control cells, indicating that JNK-deficiency may increase epithelial cell proliferation (Figure 2B). This conclusion was confirmed by measurement of cell proliferation (Figure 2C). Together, these data demonstrate that the effect of JNK-deficiency on the proliferation of MEF markedly differs from mammary epithelial cells. Thus, JNK is required for MEF proliferation, but is not required for proliferation of mammary epithelial cells.
Figure 2. Effect of JNK-deficiency on mammary epithelial cell proliferation.
A) Primary cultures of CreERT (Control) and Jnk1Δ/Δ Jnk2−/− CreERT mammary epithelial cells prepared from tamoxifen-treated mice were examined by phase contrast microscopy. Representative images are shown.
B) The cells were pulse-labeled with BrdU and examined by flow cytometry. The number of BrdU positive cells (%) is presented (mean ± SD; n = 5). Significant differences between Control cells and JNK-deficient cells are indicated with an asterisk (p < 0.05).
C) Relative cell proliferation was measured using the WST-1 assay (mean ± SD; n = 3). Significant differences between Control cells and JNK-deficient cells are indicated with an asterisk (p < 0.05).
It is unclear whether the failure of JNK-deficient mammary epithelial cells to senesce reflects a specific role of JNK in mammary epithelial cells or whether this reflects a general role of JNK in other epithelial cells. To address this question, we examined the effect of JNK-deficiency in intestinal epithelial cells using conditional gene ablation in vivo with Villin-Cre (Figure S2). Compound JNK-deficiency caused no detected defects in the proliferation of intestinal epithelial cells (Figure S2A) or colon tumor cells (Figure S2C,D). JNK-deficiency causes increased expression of p53 by MEF (20), but no increase in p53 expression was detected in JNK-deficient intestinal epithelial cells (Figure S2B). Moreover, ionizing radiation caused a similar increase in p53 expression by Control and JNK-deficient intestinal epithelial cells. Together, these data indicate that the p53-dependent senescence of JNK-deficient MEF (20, 22) reflects a particular role of JNK in MEF, but not other cell types (e.g. mammary and intestinal epithelial cells).
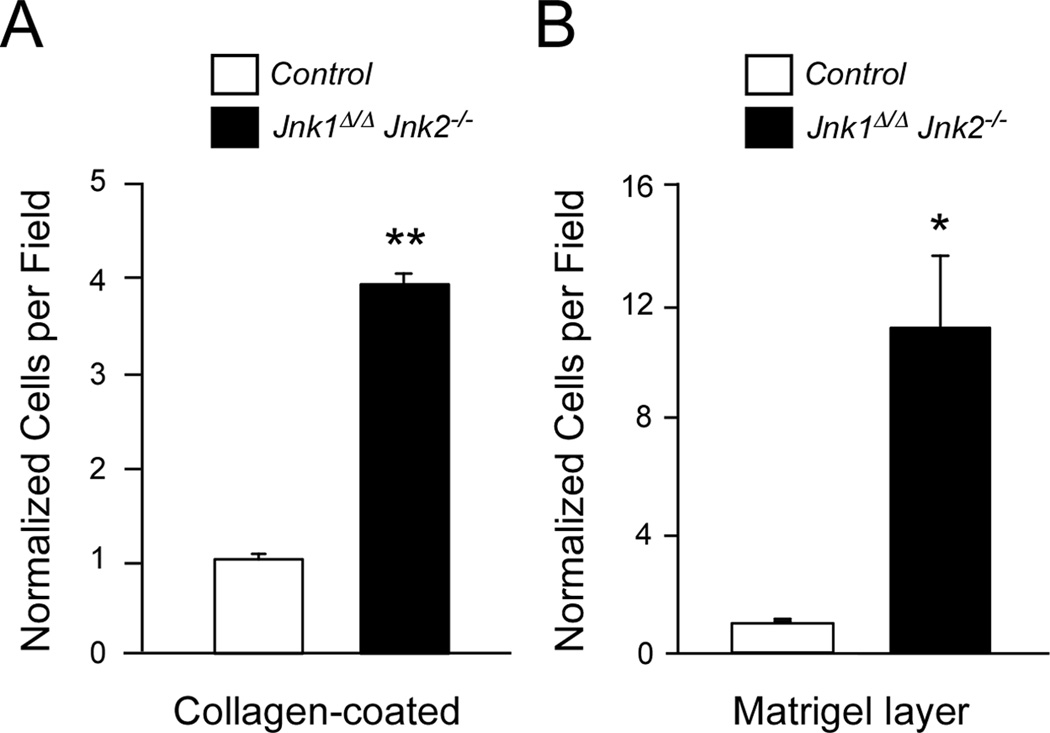
Role of JNK in mammary epithelial cell motility
It is has been reported that JNK is required for actin polymerization-dependent cell protrusions at the leading edge of epithelial cell sheets during morphogenetic movements (12). It has also been reported that paxillin phosphorylation by JNK is essential for epithelial cell movement (11). Together, these data indicate that JNK is a critical cellular component that is required for cell motility. To test this hypothesis, we prepared cultures of mammary epithelial cells from Control mice (CreERT) and Jnk1Δ/Δ Jnk2−/− CreERT mice. Comparison of Control and JNK-deficient primary mammary epithelial cells indicated that JNK is not required for cell motility. Indeed, studies using Boyden chambers coated with collagen showed that JNK-deficiency increased mammary epithelial cell motility (Figure 3A). Moreover, assays using Boyden chambers with a Matrigel layer demonstrated that JNK-deficiency increased mammary epithelial cell invasion (Figure 3B). Together, these data do not support a critical role for JNK as a positive regulator of primary mammary epithelial cell motility. This finding contrasts with previous reports that JNK plays a key role in epithelial cell motility (2, 11). We therefore examined mice with JNK-deficiency in the intestinal epithelium (Figure S2). Epithelial cells formed in intestinal crypts migrate on the surface of the villus to create the intestinal epithelium. Intestinal epithelium morphology was not disrupted by JNK-deficiency (Figure S2), consistent with a non-essential function of JNK in intestinal epithelial cell motility. Together, these data indicate that JNK is not essential for epithelial cell motility.
Figure 3. Effect of JNK-deficiency on mammary epithelial cell motility and invasion.
A,B) Primary cultures of CreERT (Control) and Jnk1Δ/Δ Jnk2−/− CreERT mammary epithelial cells prepared from tamoxifen-treated mice were examined using Boyden chambers coated with Collagen I (A) or with a Matrigel layer (B). The relative number of cells that moved from the upper chamber to the lower chamber is presented (mean ± SD; n = 5). Significant differences between Control cells and JNK-deficient cells are indicated with an asterisk (*, p < 0.05; **, p < 0.001).
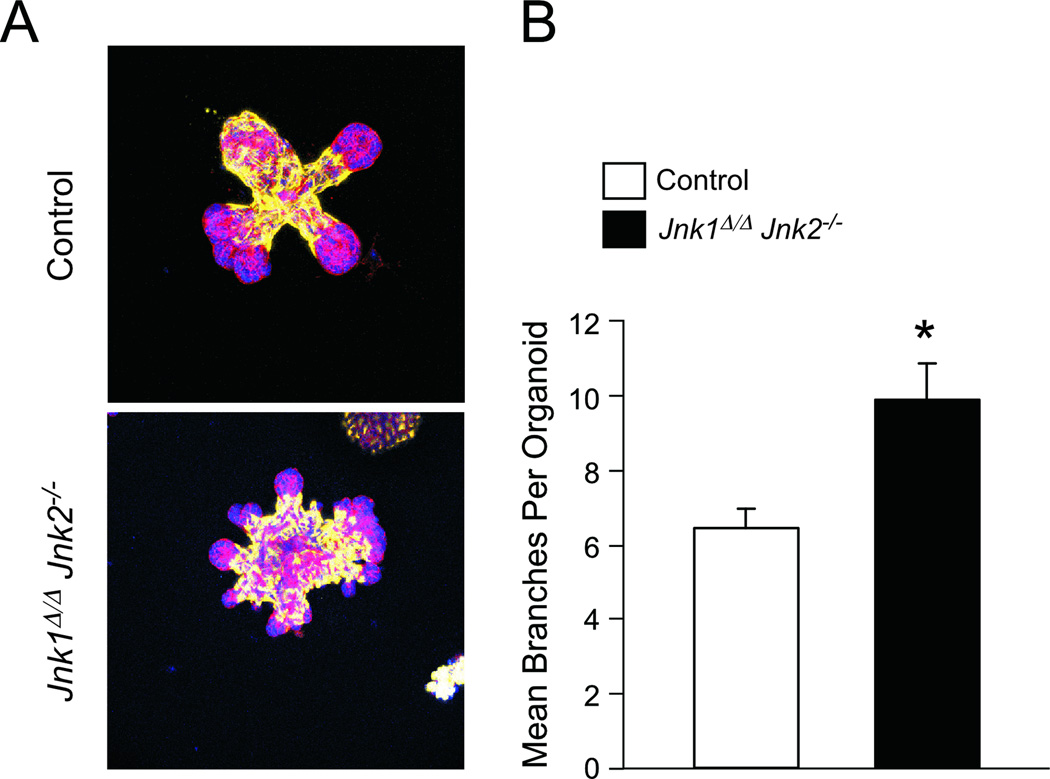
Role of JNK in mammary branching morphogenesis
Branching morphogenesis is an important aspect of mammary gland development (28, 29). This process can be studied in vitro using mammary organoid cultures in the presence of FGF2 (17). We prepared cultures of mammary organoids from Control mice (CreERT) and Jnk1Δ/Δ Jnk2−/− CreERT mice. The organoids are formed by bilayer structures with lumenal mammary epithelial cells and basal myoepithelial cells that express smooth muscle actin (30, 31). Branching morphogenesis is regulated by hormones/growth factors and by the interaction of the lumenal epithelial cells with basal myoepithelial cells and the extracellular matrix (29). Branching morphogenesis was detected in cultures of Control and Jnk1Δ/ΔJnk2−/− mammary organoids (Figure 4A). This observation indicated that JNK is not required for branching morphogenesis. However, quantitation of the branching indicated that JNK-deficient organoids exhibited significantly greater branching morphogenesis than Control organoids (Figure 4B). Together, these data demonstrate that JNK can influence mammary branching morphogenesis.
Figure 4. Effect of JNK-deficiency on mammary branching morphogenesis.
A) Primary organoid CreERT (Control) and Jnk1Δ/Δ Jnk2−/− CreERT cultures prepared from tamoxifen-treated mice were examined by immunofluorescence microscopy by staining with an antibody to smooth muscle actin (SMA, green) and with phalloidin to stain F-actin (red). DNA was stained with DAPI (blue). Branching morphogenesis was initiated by treatment of the cultures with FGF2. The organoids were examined using a Leica TCS SP2 confocal microscope by acquiring 10 optical sections that were collapsed to a single image. Representative images are shown.
B) The number of branches per organoid was measured (mean ± SD, n = 20). Significant differences between Control cells and JNK-deficient cells are indicated with an asterisk (*, p < 0.01).
Effect of JNK-deficiency on mammary epithelial cell gene expression
It is established that the JNK signal transduction pathway can regulate gene expression (1). JNK-regulated gene expression may therefore account for the effect of JNK-deficiency on epithelial cell motility and invasion (Figure 3) and branching morphogenesis (Figure 4). We therefore examined the effect of JNK-deficiency on the expression of candidate genes that may influence these processes (Figure S3).
Matrix metalloproteases (MMPs) play key roles in mammary gland development (28). Thus, ADAM17 induces shedding of the EGF receptor ligand amphiregulin that can induce expression of MMP2 (32). MMP2 (and its activator MMP14) can promote ductal elongation (33), and both MMP3 and MMP9 promote branching morphogenesis (33, 34). We found that JNK-deficiency caused significantly decreased expression of Mmp2, Mmp9, and Mmp14 mRNA (Figure S3A). These changes do not account for the increased branching morphogenesis caused by JNK-deficiency. MMPs and ADAM17 are negatively regulated by Tissue Inhibitors of Metalloproteases (TIMPs). Down-regulated expression of TIMP1/2/3 could therefore increase MMP and/or ADAM17 activity and therefore influence branching morphogenesis (29). Indeed, a significant reduction in Timp1, Timp2, and Timp3 mRNA expression was caused by JNK-deficiency (Figure S3B). In contrast, the expression of two other genes that are implicated in branching morphogenesis (Tgfβ1 and Sprouty2) was unaffected by JNK-deficiency (Figure S3B). Together, these data suggest that decreased TIMP expression may contribute to increased branching morphogenesis caused by JNK-deficiency.
The increased motility and invasion activity of JNK-deficient mammary epithelial cells detected in Boyden chamber assays may reflect altered integrin expression. We found decreased expression of α1, α5, α6, and β1 integrins and also decreased expression of the collagen receptor DDR1 in JNK-deficient mammary epithelial cells (Figure S3C). The decreased expression of integrin α5 protein was confirmed by immunofluorescence analysis (Figure S4). Previous studies have implicated integrin α2, integrin β1, and DDR1 in mammary gland development (29), but decreased expression of these proteins is not predicted to cause the increased motility, invasion, and branching morphogenesis caused by JNK-deficiency (Figures 3 & 4). The mechanism that accounts for increased motility and invasion by JNK-deficient mammary epithelial cells is therefore unclear.
Effect of JNK-deficiency on mammary gland development
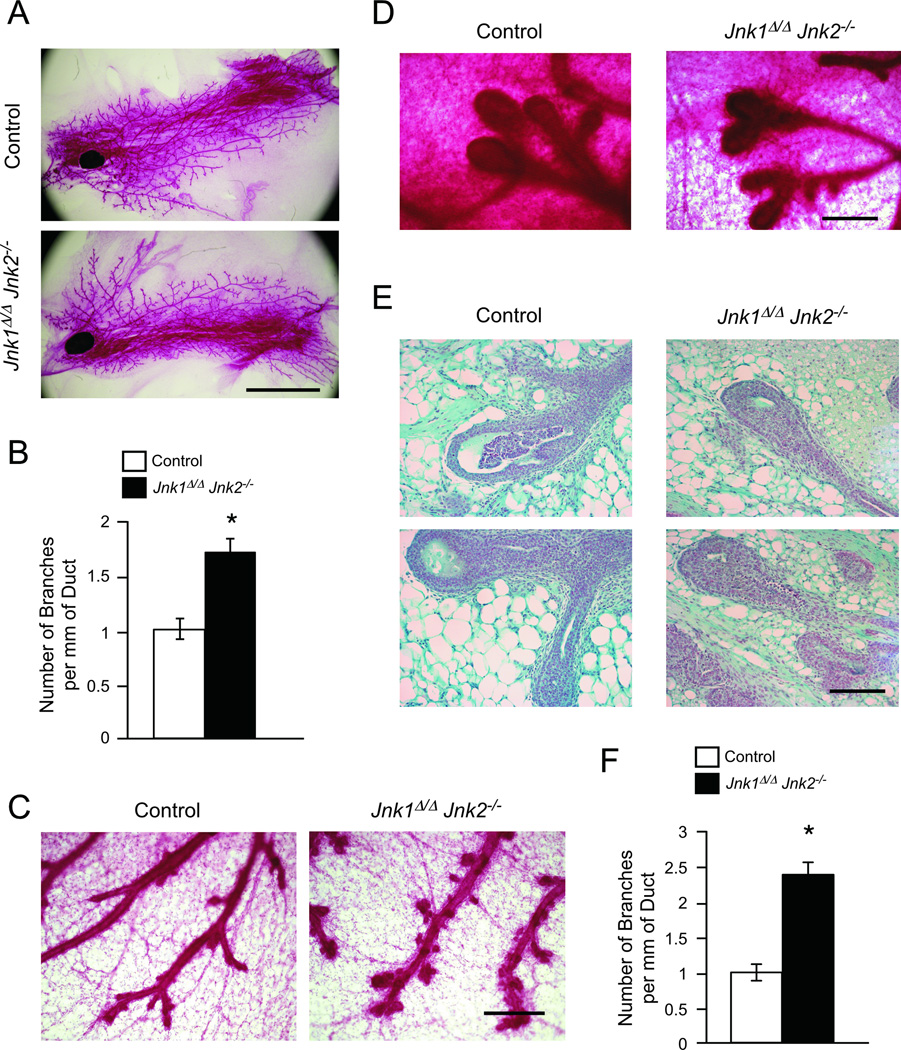
We employed transplantation assays to test the role of JNK in mammary gland development using the fourth inguinal gland pair. Control (CreERT) tissue was transplanted in one cleared mammary gland of a female nude mouse and Jnk1Δ/Δ Jnk2−/− CreERT tissue was transplanted in the contralateral gland of the same recipient mouse. Analysis of mammary gland development at 8 weeks following transplantation demonstrated that JNK-deficiency did not prevent the elaboration of mammary epithelial ducts (Figure 5A). However, JNK-deficiency caused an increase in the number of branches (Figure 5B,C). These data indicate that JNK can influence mammary branching morphogenesis in vivo.
Figure 5. Effect of JNK-deficiency on mammary gland development.
Transplantation assays were performed using mammary tissue from tamoxifen-treated female donor mice and female recipient nude mice. Control (CreERT) tissue was transplanted in one cleared mammary gland and Jnk1Δ/Δ Jnk2−/− CreERT tissue was transplanted in the contralateral gland of the same recipient mouse.
A–C) Whole mount mammary glands stained with carmine alum at 8 weeks following transplantation are shown (A,C). The number of branches per unit length (mm) of duct is presented as the mean ± SD; n = 3 (B). Statistically significant differences are indicated with an asterisk (*, p < 0.05). Scale bars: 5 mm (A); 200 µm (C).
D–F) Terminal end buds in whole mount mammary glands stained with carmine alum at 2 weeks following transplantation are shown (D). Stained sections of the end buds in whole mount mammary glands are presented (E). The number of branches per unit length (mm) of duct is presented as the mean ± SD; n = 3 (F). Statistically significant differences are indicated with an asterisk (*, p < 0.05). Scale bars: 200 µm (D); 100 µm (E).
To test whether JNK may alter the early time course of mammary gland development, we examined mice at 2 weeks following transplantation. This analysis demonstrated the presence of terminal end buds (TEBs) in glands formed by Control and JNK-deficient tissue (Figure 5D). No differences in proliferating cells (PCNA-positive) or dying cells (TUNEL-positive) were detected between Control and JNK-deficient mammary glands (Figure S5). Sections of TEBs formed by transplantation of Control tissue demonstrated the presence of a lumenal space (Figure 5E). In contrast, this TEB lumenal space was partially filled with cells in glands formed by transplantation of JNK-deficient tissue (Figure 5E). These data indicate that JNK-deficiency disrupts TEB morphology during mammary gland development. Moreover, JNK-deficiency increased the number of branches detected at 2 weeks following transplantation (Figure 5F).
Effect of JNK-deficiency on mammary tumorigenesis
JNK-deficiency influences the proliferation, motility, invasion activity, and branching morphogenesis in vitro (Figures 2 – 4) and mammary gland development in vivo (Figure 5). These changes indicate that JNK may influence mammary tumor development. To test this hypothesis, we examined the effect of mutational activation of the endogenous KRas gene in vivo. Transplantation assays were performed using donor tissue from Control mice (KRasLSL-G12D/+ CreERT) and mice with conditional expression of JNK (KRasLSL-G12D/+ Jnk1LoxP/LoxP Jnk2−/− CreERT). The recipient nude mice were transplanted with both Control tissue and JNK-deficient tissue in the fourth inguinal gland pair. The transplanted mice were treated with tamoxifen at two weeks post-surgery to induce expression of activated Ras (KRasG12D) and to ablate the conditional Jnk1 gene. No tumors were detected in these mice within 6 months of transplantation.
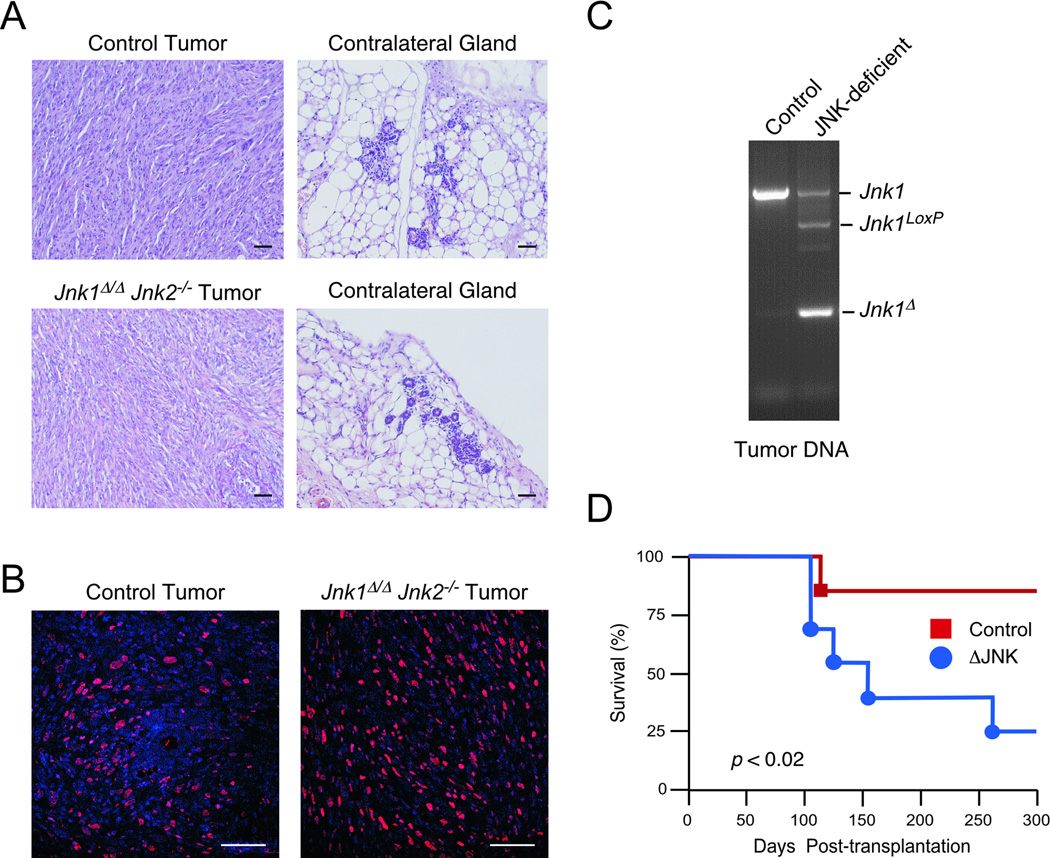
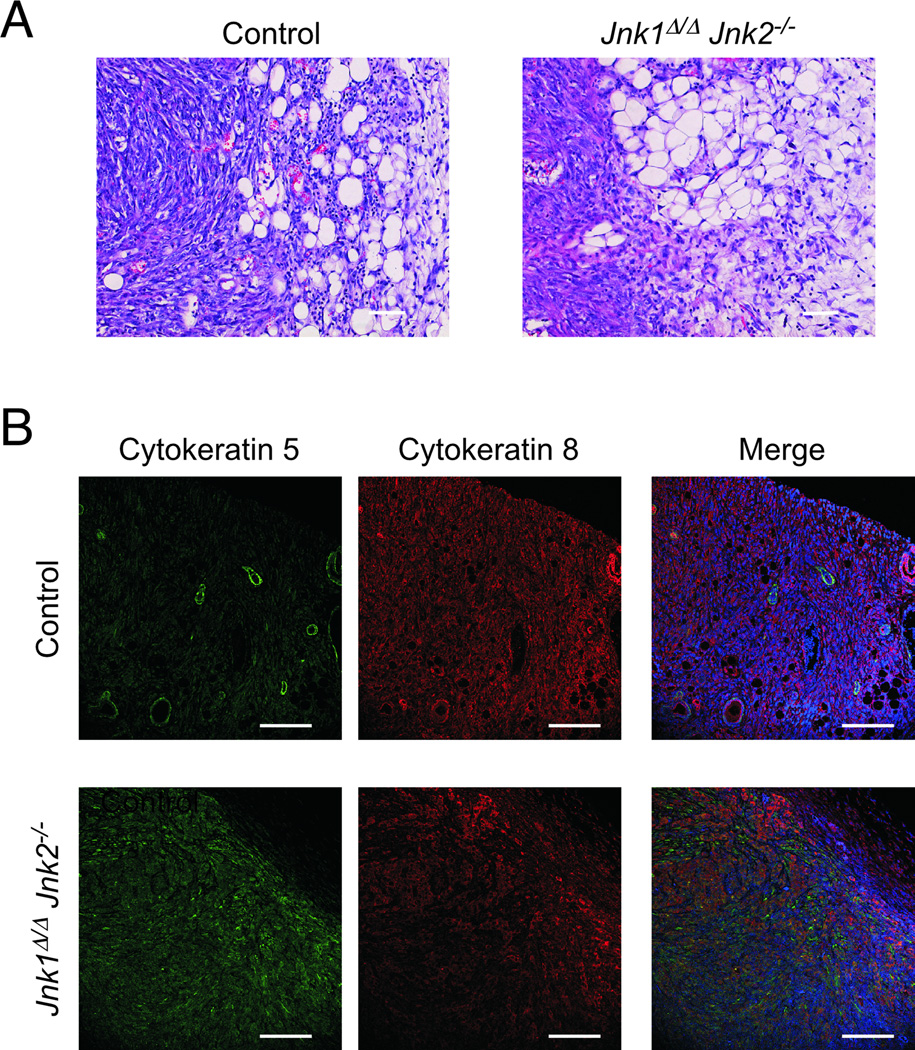
The KRasG12D oncogene may require a co-operating mutation to efficiently induce breast cancer (35). We therefore examined the effect of p53 loss-of-function on KRasG12D -induced breast cancer. Transplantation assays were performed using donor tissue from Control mice (KRasLSL-G12D/+ Trp53LoxP/LoxP CreERT) and mice with conditional expression of JNK (KRasLSL-G12D/+ Jnk1LoxP/LoxP Jnk2−/− Trp53LoxP/LoxP CreERT). These transplanted mice developed mammary carcinoma (Figure 6). Analysis of tissue sections demonstrated that both Control and JNK-deficient tumors were composed primarily of spindle-like cells (Figure 6A) that stained with an antibody to the proliferation marker PCNA (Figure 6B). Genotype analysis confirmed Jnk1 gene disruption in tumors obtained from mammary glands transplanted with JNK-deficient tissue (Figure 6C). Kaplan-Meier analysis demonstrated that compound JNK-deficiency caused a significant increase in the number of mice with breast cancer (Figure 6D). The mean tumor volume at necropsy was 0.62 cm3 ± 0.19 (mean ± SD; n = 7) and no significant difference between Control and JNK-deficient tumor volume was observed. The Control and JNK-deficient tumors were locally invasive (Figure 7A), but no metastasis was detected. Tumor sections stained for markers of basal-like (cytokeratin 5) and non-basal-like (cytokeratin 8) breast cancer demonstrated that the tumors obtained represented mixed origins (basal and non-basal). However, the JNK-defcient tumors stained more efficiently for cytokeratin 5 than Control tumors, indicating that JNK-deficiency may promote basal-like tumors in this KRas/Trp53 model of murine breast cancer.
Figure 6. Effect of JNK-deficiency on mammary tumor development.
Transplantation assays were performed using mammary tissue from female donor mice and female recipient nude mice. Control (KRasLSL-G12D/+ Trp53LoxP/LoxP CreERT) tissue was transplanted in one cleared mammary gland and KRasLSL-G12D/+ Trp53LoxP/LoxP Jnk1LoxP̃/LoxP Jnk2−/− CreERT tissue was transplanted in the contralateral gland of the same recipient mouse. The transplanted mice were treated with tamoxifen at two weeks post-surgery.
A) Sections of transplanted breast mammary glands were stained with H&E. Scale bar = 50 µm.
B) Sections of breast tumors were stained with an antibody to PCNA (red). DNA was stained with DAPI. Scale bar = 75 µm.
C) Genomic DNA isolated from Control and JNK-deficient breast tumors was examined by PCR using amplimers to detect the wild-type Jnk1 allele (1.5 kb), the Jnk1LoxP allele (1.1 kb), and the ablated allele ΔJnk1 (0.4kb).
D) Kaplan-Meier analysis of tumor-free survival of transplanted mice (n = 8). The development of JNK-deficient tumors was significantly more rapid than Control tumors (p < 0.02; Log-rank test).
Figure 7. JNK-deficiency causes increased basal-like mammary carcinogenesis.
Transplantation assays were performed using Control and JNK-deficient tissue (Figure 6).
A) Sections showing the periphery of Control and JNK-deficient mammary tumors were stained with H&E. Scale bar = 150 µm.
B) Sections of Control and JNK-deficient mammary tumors were stained with an antibody to cytokeratin 5 (green) and cytokeratin 8 (red). DNA was stained with DAPI. Scale bar = 150 µm.
Discussion
Mice with defects in JNK expression have provided insight into the biological function of the JNK signaling pathway (1, 36). However, the ubiquitously expressed Jnk1 and Jnk2 genes have partially redundant functions (19, 20) and compound mutant Jnk1−/− Jnk2−/− mice die during mid-embryogenesis (10). Studies of the effect of compound JNK-deficiency have therefore largely focused on an analysis of MEF (20). However, MEF are not representative of many differentiated cell types. Progress has been made towards the creation of mice with conditional and chemical genetic Jnk alleles (19, 22) that enable the analysis of cell types that are relevant to specific physiological processes (37). The focus of this study was to employ conditional gene targeting to examine the role of JNK in mammary epithelial cells. We report that JNK contributes to mammary gland development. Importantly, the functions of JNK in mammary epithelial cells differ from those previously identified in MEF.
JNK is not essential for mammary epithelial cell proliferation or motility
Compound JNK-deficiency in MEF causes increased p53 expression and senescence (20, 22). In contrast, JNK-deficient mammary epithelial cells did not exhibit a defect in proliferation in vitro (Figure 2). Moreover, transplantation assays demonstrated that JNK-deficient cells retained sufficient proliferative capacity to form a mammary gland in vivo (Figure 5). These data demonstrate that JNK is not essential for proliferation of mammary epithelial cells. This conclusion may apply to other epithelial cells because studies of intestinal epithelial cells also demonstrated that JNK is not required for proliferation (Figure S2). Thus, the effect of JNK-deficiency to engage the p53-mediated senescence pathway may represent a specialized response of MEF to loss of JNK signaling.
JNK signaling has been implicated in the regulation of cell motility (2). The role of JNK may be mediated by JNK-dependent paxillin phosphorylation (11) and/or a requirement of JNK for actin polymerization-dependent cell protrusions (12). Nevertheless, we did not detect defects in mammary epithelial cell motility caused by JNK-deficiency. Indeed, JNK-deficiency caused an increase in mammary epithelial cell motility in Boyden chamber assays (Figure 3A). Similarly, JNK-deficiency caused increased invasion of mammary epithelial cells through a Matrigel layer (Figure 3B). Furthermore, JNK-deficiency did not prevent the formation of mammary epithelial cell ducts or the intestinal epithelium in vivo (Figures 5 & S2). Together, these data demonstrate that JNK is not essential for epithelial cell motility. This conclusion may reflect a redundant role of JNK for paxillin phosphorylation (11). Moreover, JNK-dependent leading edge cell protrusions may not be rate limiting for motility (e.g. roles of adhesion and rear-end detachment).
JNK is required for normal mammary gland development
Transplantation assays demonstrated that JNK is not required for the formation of a mammary gland in a virgin female mouse (Figure 5). However, developmental defects were detected. Thus, examination of terminal end buds (TEBs) at 2 weeks following transplantation demonstrated that lumenal cell clearance found in Control TEBs was incomplete in JNK-deficient TEBs (Figure 5E). Previous studies have established that lumenal clearance is caused by cell death, partially mediated by apoptosis (38), that involves the BH3-only proteins Bim (15, 39) and Bmf (40). Interestingly, Bim and Bmf are targets of pro-apoptotic signaling by JNK (41, 42). Loss of JNK signaling may lead to defects in Bim/Bmf function and consequently failure of lumenal clearance (15). Nevertheless, it should be noted that the defect in TEB lumenal cell clearance caused by JNK-deficiency was partial (Figure 5E), suggesting the presence of redundant or compensatory mechanisms of lumenal cell clearance in the JNK-deficient mammary glands. This type of compensation has been noted in studies of Bim-deficient mammary glands (39).
JNK-deficiency caused altered branching morphogenesis. Transplantation assays demonstrated that JNK-deficiency caused increased branching of mammary ducts in vivo. (Figure 5B,F). This effect of JNK-deficiency to cause increased branching morphogenesis was also observed in FGF2-stimulated organoid cultures in vitro (Figure 4). The mechanism that accounts for increased branching morphogenesis is unclear, but it is established that this process is regulated by hormones/growth factors and by the interaction of the lumenal epithelial cells with basal myoepithelial cells and the extracellular matrix (28, 29). One potential role of JNK is represented by expression of TIMP isoforms that inhibit matrix metalloproteases (MMPs). JNK-deficiency caused decreased expression of Timp1/2/3 (Figure S3B). Decreased TIMP activity may lead to increased activity of MMP3 and MMP9 that function, in part, to promote branching morphogenesis (33, 34). This mechanism may contribute to the altered branching morphogenesis caused by JNK-deficiency.
JNK contributes to mammary tumor development
The effect of JNK-deficiency to perturb normal mammary gland development may be relevant to breast cancer. However, the contribution of JNK to breast cancer is unclear (1). Mutations in JNK pathway genes (Jnk1, Jnk2, Mkk4 and Mkk7) are detected in human cancers (43, 44), but it is unclear whether these mutations are causally related to tumorigenesis (45). Insight into the potential function of JNK has been obtained from murine studies of KRas-induced lung cancer (46), carcinogen-induced hepatocellular carcinoma (47) and colon cancer (Figure S2) with tissue-specific compound ablation of the Jnk1 and Jnk2 genes. These studies have demonstrated an essential role for JNK in KRas-induced lung cancer (46), but no required role for JNK in carcinogen-induced colon cancer (Figure S2). In contrast, JNK plays a more complex role in hepatocellular carcinoma because JNK promotes an inflammatory microenvironment to support tumor development, but acts in hepatocytes to reduce tumor development (47). Together, these data indicate that, in individual tumor types, JNK may play no role in tumor development or may contribute (positively or negatively) to tumor pathology.
Studies using single gene ablation (Jnk1 or Jnk2) indicate that JNK-deficiency can increase mammary carcinoma in the Trp53 BALB/c mouse model (18). Moreover, JNK2-deficiency shortens tumor latency and increases tumor multiplicity in a transgenic mouse model with expression of polyoma virus T antigen (48). These observations suggest that JNK may function to reduce tumor development. However, JNK1 and JNK2 exhibit partially redundant functions (20, 22). Consequently, single gene ablation (Jnk1 or Jnk2) may not provide insight into the effects of compound JNK deficiency (37, 47, 49). Here we demonstrate that compound JNK-deficiency promotes tumor development in a KRas/Trp53 mouse model of breast cancer. Further studies will be required to confirm the pro-tumorigenic effect of JNK-deficiency in a model of breast cancer that has direct relevance to human disease. Nevertheless, it is likely that pro-tumorigenic effects of JNK-deficiency reflect functional roles for JNK pathway gene (Jnk1, Jnk2, Mkk4 and Mkk7) mutations that have been detected in human cancer (43, 44) and JNK-regulated genetic instability (48).
Small molecule inhibitors of JNK have been proposed to be useful for the treatment of metabolic and inflammatory disorders in humans (50). The design of such therapies should take into account the potential pro-tumorigenic effects of JNK inhibition.
Supplementary Material
Acknowledgments
We thank Tammy Barrett for expert technical assistance, and Kathy Gemme for administrative assistance.
Grant Support
These studies were supported by a grant from the National Institutes of Health (R01-CA65861). N.G. was supported by training grant T32 CA130807. R.J.D. is an Investigator of the Howard Hughes Medical Institute and is also a member of the Diabetes and Endocrinology Research Center of the University of Massachusetts Medical School that is funded by the National Institutes of Health grant P30-DK032520.
Footnotes
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- 1.Davis RJ. Signal transduction by the JNK group of MAP kinases. Cell. 2000;103:239–252. doi: 10.1016/s0092-8674(00)00116-1. [DOI] [PubMed] [Google Scholar]
- 2.Xia Y, Karin M. The control of cell motility and epithelial morphogenesis by Jun kinases. Trends Cell Biol. 2004;14:94–101. doi: 10.1016/j.tcb.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Ip YT, Davis RJ. Signal transduction by the c-Jun N-terminal kinase (JNK)--from inflammation to development. Curr Opin Cell Biol. 1998;10:205–219. doi: 10.1016/s0955-0674(98)80143-9. [DOI] [PubMed] [Google Scholar]
- 4.Zeitlinger J, Bohmann D. Thorax closure in Drosophila: involvement of Fos and the JNK pathway. Development. 1999;126:3947–3956. doi: 10.1242/dev.126.17.3947. [DOI] [PubMed] [Google Scholar]
- 5.Agnes F, Suzanne M, Noselli S. The Drosophila JNK pathway controls the morphogenesis of imaginal discs during metamorphosis. Development. 1999;126:5453–5462. doi: 10.1242/dev.126.23.5453. [DOI] [PubMed] [Google Scholar]
- 6.Suzanne M, Perrimon N, Noselli S. The Drosophila JNK pathway controls the morphogenesis of the egg dorsal appendages and micropyle. Dev Biol. 2001;237:282–294. doi: 10.1006/dbio.2001.0384. [DOI] [PubMed] [Google Scholar]
- 7.Weston CR, Wong A, Hall JP, Goad ME, Flavell RA, Davis RJ. JNK initiates a cytokine cascade that causes Pax2 expression and closure of the optic fissure. Genes Dev. 2003;17:1271–1280. doi: 10.1101/gad.1087303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weston CR, Wong A, Hall JP, Goad ME, Flavell RA, Davis RJ. The c-Jun NH2-terminal kinase is essential for epidermal growth factor expression during epidermal morphogenesis. Proc Natl Acad Sci U S A. 2004;101:14114–14119. doi: 10.1073/pnas.0406061101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang L, Wang W, Hayashi Y, Jester JV, Birk DE, Gao M, et al. A role for MEK kinase 1 in TGF-beta/activin-induced epithelium movement and embryonic eyelid closure. EMBO J. 2003;22:4443–4454. doi: 10.1093/emboj/cdg440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuan CY, Yang DD, Samanta Roy DR, Davis RJ, Rakic P, Flavell RA. The Jnk1 and Jnk2 protein kinases are required for regional specific apoptosis during early brain development. Neuron. 1999;22:667–676. doi: 10.1016/s0896-6273(00)80727-8. [DOI] [PubMed] [Google Scholar]
- 11.Huang C, Rajfur Z, Borchers C, Schaller MD, Jacobson K. JNK phosphorylates paxillin and regulates cell migration. Nature. 2003;424:219–223. doi: 10.1038/nature01745. [DOI] [PubMed] [Google Scholar]
- 12.Homsy JG, Jasper H, Peralta XG, Wu H, Kiehart DP, Bohmann D. JNK signaling coordinates integrin and actin functions during Drosophila embryogenesis. Dev Dyn. 2006;235:427–434. doi: 10.1002/dvdy.20649. [DOI] [PubMed] [Google Scholar]
- 13.Whyte J, Bergin O, Bianchi A, McNally S, Martin F. Key signalling nodes in mammary gland development and cancer. Mitogen-activated protein kinase signalling in experimental models of breast cancer progression and in mammary gland development. Breast Cancer Res. 2009;11:209. doi: 10.1186/bcr2361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murtagh J, McArdle E, Gilligan E, Thornton L, Furlong F, Martin F. Organization of mammary epithelial cells into 3D acinar structures requires glucocorticoid and JNK signaling. J Cell Biol. 2004;166:133–143. doi: 10.1083/jcb.200403020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhan L, Rosenberg A, Bergami KC, Yu M, Xuan Z, Jaffe AB, et al. Deregulation of scribble promotes mammary tumorigenesis and reveals a role for cell polarity in carcinoma. Cell. 2008;135:865–878. doi: 10.1016/j.cell.2008.09.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bain J, McLauchlan H, Elliott M, Cohen P. The specificities of protein kinase inhibitors: an update. Biochem J. 2003;371:199–204. doi: 10.1042/BJ20021535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ewald AJ, Brenot A, Duong M, Chan BS, Werb Z. Collective epithelial migration and cell rearrangements drive mammary branching morphogenesis. Dev Cell. 2008;14:570–581. doi: 10.1016/j.devcel.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cellurale C, Weston CR, Reilly J, Garlick DS, Jerry DJ, Sluss HK, et al. Role of JNK in a Trp53-dependent mouse model of breast cancer. PLoS One. 2010;5:e12469. doi: 10.1371/journal.pone.0012469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jaeschke A, Karasarides M, Ventura JJ, Ehrhardt A, Zhang C, Flavell RA, et al. JNK2 is a positive regulator of the cJun transcription factor. Mol Cell. 2006;23:899–911. doi: 10.1016/j.molcel.2006.07.028. [DOI] [PubMed] [Google Scholar]
- 20.Tournier C, Hess P, Yang DD, Xu J, Turner TK, Nimnual A, et al. Requirement of JNK for stress-induced activation of the cytochrome c-mediated death pathway. Science. 2000;288:870–874. doi: 10.1126/science.288.5467.870. [DOI] [PubMed] [Google Scholar]
- 21.Yang DD, Conze D, Whitmarsh AJ, Barrett T, Davis RJ, Rincon M, et al. Differentiation of CD4+ T cells to Th1 cells requires MAP kinase JNK2. Immunity. 1998;9:575–585. doi: 10.1016/s1074-7613(00)80640-8. [DOI] [PubMed] [Google Scholar]
- 22.Das M, Jiang F, Sluss HK, Zhang C, Shokat KM, Flavell RA, et al. Suppression of p53-dependent senescence by the JNK signal transduction pathway. Proc Natl Acad Sci U S A. 2007;104:15759–15764. doi: 10.1073/pnas.0707782104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jackson EL, Willis N, Mercer K, Bronson RT, Crowley D, Montoya R, et al. Analysis of lung tumor initiation and progression using conditional expression of oncogenic K-ras. Genes Dev. 2001;15:3243–3248. doi: 10.1101/gad.943001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marino S, Vooijs M, van Der Gulden H, Jonkers J, Berns A. Induction of medulloblastomas in p53-null mutant mice by somatic inactivation of Rb in the external granular layer cells of the cerebellum. Genes Dev. 2000;14:994–1004. [PMC free article] [PubMed] [Google Scholar]
- 25.Badea TC, Wang Y, Nathans J. A noninvasive genetic/pharmacologic strategy for visualizing cell morphology and clonal relationships in the mouse. J Neurosci. 2003;23:2314–2322. doi: 10.1523/JNEUROSCI.23-06-02314.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Madison BB, Dunbar L, Qiao XT, Braunstein K, Braunstein E, Gumucio DL. Cis elements of the villin gene control expression in restricted domains of the vertical (crypt) and horizontal (duodenum, cecum) axes of the intestine. J Biol Chem. 2002;277:33275–33283. doi: 10.1074/jbc.M204935200. [DOI] [PubMed] [Google Scholar]
- 27.Young L. Chapter 6 The Cleared Mammary Fat Pad and the Transplantation of Mammary Gland Morphological Structures and Cells. In: Ip M, Asch B, editors. Methods in Mammary Gland Biology and Breast Cancer Research. New York: Kluwer Academic / Plenum Publishers; 2000. pp. 67–74. [Google Scholar]
- 28.Sternlicht MD. Key stages in mammary gland development: the cues that regulate ductal branching morphogenesis. Breast Cancer Res. 2006;8:201. doi: 10.1186/bcr1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fata JE, Werb Z, Bissell MJ. Regulation of mammary gland branching morphogenesis by the extracellular matrix and its remodeling enzymes. Breast Cancer Res. 2004;6:1–11. doi: 10.1186/bcr634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Deugnier MA, Teuliere J, Faraldo MM, Thiery JP, Glukhova MA. The importance of being a myoepithelial cell. Breast Cancer Res. 2002;4:224–230. doi: 10.1186/bcr459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bissell MJ, Rizki A, Mian IS. Tissue architecture: the ultimate regulator of breast epithelial function. Curr Opin Cell Biol. 2003;15:753–762. doi: 10.1016/j.ceb.2003.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sternlicht MD, Sunnarborg SW, Kouros-Mehr H, Yu Y, Lee DC, Werb Z. Mammary ductal morphogenesis requires paracrine activation of stromal EGFR via ADAM17-dependent shedding of epithelial amphiregulin. Development. 2005;132:3923–3933. doi: 10.1242/dev.01966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wiseman BS, Sternlicht MD, Lund LR, Alexander CM, Mott J, Bissell MJ, et al. Site-specific inductive and inhibitory activities of MMP-2 and MMP-3 orchestrate mammary gland branching morphogenesis. J Cell Biol. 2003;162:1123–1133. doi: 10.1083/jcb.200302090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee PP, Hwang JJ, Murphy G, Ip MM. Functional significance of MMP-9 in tumor necrosis factor-induced proliferation and branching morphogenesis of mammary epithelial cells. Endocrinology. 2000;141:3764–3773. doi: 10.1210/endo.141.10.7697. [DOI] [PubMed] [Google Scholar]
- 35.Podsypanina K, Politi K, Beverly LJ, Varmus HE. Oncogene cooperation in tumor maintenance and tumor recurrence in mouse mammary tumors induced by Myc and mutant Kras. Proc Natl Acad Sci U S A. 2008;105:5242–5247. doi: 10.1073/pnas.0801197105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weston CR, Davis RJ. The JNK signal transduction pathway. Curr Opin Cell Biol. 2007;19:142–149. doi: 10.1016/j.ceb.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 37.Das M, Sabio G, Jiang F, Rincon M, Flavell RA, Davis RJ. Induction of hepatitis by JNK-mediated expression of TNF-alpha. Cell. 2009;136:249–260. doi: 10.1016/j.cell.2008.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mailleux AA, Overholtzer M, Brugge JS. Lumen formation during mammary epithelial morphogenesis: insights from in vitro and in vivo models. Cell Cycle. 2008;7:57–62. doi: 10.4161/cc.7.1.5150. [DOI] [PubMed] [Google Scholar]
- 39.Mailleux AA, Overholtzer M, Schmelzle T, Bouillet P, Strasser A, Brugge JS. BIM regulates apoptosis during mammary ductal morphogenesis, and its absence reveals alternative cell death mechanisms. Dev Cell. 2007;12:221–234. doi: 10.1016/j.devcel.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schmelzle T, Mailleux AA, Overholtzer M, Carroll JS, Solimini NL, Lightcap ES, et al. Functional role and oncogene-regulated expression of the BH3-only factor Bmf in mammary epithelial anoikis and morphogenesis. Proc Natl Acad Sci U S A. 2007;104:3787–3792. doi: 10.1073/pnas.0700115104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hubner A, Barrett T, Flavell RA, Davis RJ. Multisite phosphorylation regulates Bim stability and apoptotic activity. Mol Cell. 2008;30:415–425. doi: 10.1016/j.molcel.2008.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hubner A, Cavanagh-Kyros J, Rincon M, Flavell RA, Davis RJ. Functional cooperation of the proapoptotic Bcl2 family proteins Bmf and Bim in vivo. Mol Cell Biol. 2010;30:98–105. doi: 10.1128/MCB.01155-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Greenman C, Stephens P, Smith R, Dalgliesh GL, Hunter C, Bignell G, et al. Patterns of somatic mutation in human cancer genomes. Nature. 2007;446:153–158. doi: 10.1038/nature05610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kan Z, Jaiswal BS, Stinson J, Janakiraman V, Bhatt D, Stern HM, et al. Diverse somatic mutation patterns and pathway alterations in human cancers. Nature. 2010;466:869–873. doi: 10.1038/nature09208. [DOI] [PubMed] [Google Scholar]
- 45.Whitmarsh AJ, Davis RJ. Role of mitogen-activated protein kinase kinase 4 in cancer. Oncogene. 2007;26:3172–3184. doi: 10.1038/sj.onc.1210410. [DOI] [PubMed] [Google Scholar]
- 46.Cellurale C, Sabio G, Kennedy NJ, Das M, Barlow M, Sandy P, et al. Requirement of c-Jun NH(2)-terminal kinase for Ras-initiated tumor formation. Mol Cell Biol. 2011;31:1565–1576. doi: 10.1128/MCB.01122-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Das M, Garlick DS, Greiner DL, Davis RJ. The role of JNK in the development of hepatocellular carcinoma. Genes Dev. 2011;25:634–645. doi: 10.1101/gad.1989311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen P, O'Neal JF, Ebelt ND, Cantrell MA, Mitra S, Nasrazadani A, et al. Jnk2 effects on tumor development, genetic instability and replicative stress in an oncogene-driven mouse mammary tumor model. PLoS One. 2010;5:e10443. doi: 10.1371/journal.pone.0010443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Xu P, Das M, Reilly J, Davis RJ. JNK regulates FoxO-dependent autophagy in neurons. Genes Dev. 2011;25:310–322. doi: 10.1101/gad.1984311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Manning AM, Davis RJ. Targeting JNK for therapeutic benefit: from junk to gold? Nat Rev Drug Discov. 2003;2:554–565. doi: 10.1038/nrd1132. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.