Abstract
Study Design
Retrospective cohort study.
Objective
To determine the influence of age, comorbidities, and treatment type on mortality in elderly patients with acute Type II odontoid fractures.
Summary of Background Data
Prior studies have documented increased morbidity and mortality among geriatric patients sustaining odontoid fractures. However, there is limited data regarding the effect of patient age, medical comorbidities, and treatment selection on mortality after Type II odontoid (C2) fractures in the elderly.
Methods
An institutional registry was used to identify all Type II odontoid fractures sustained by patients aged 65 and older from 1991 to 2006. Demographic information, date of injury, associated injuries, treatment type, and comorbidities were abstracted from medical records. Mortality was ascertained using the National Death Index. Risks of mortality and their associated 95% confidence intervals (CIs) were calculated at 3 months, 1 year, 2 years, and 3 years. Multivariable Cox proportional hazard regression was used to evaluate independent factors affecting mortality stratified by age (65–74 years, 75–84 years, ≥85 years) and treatment type (operative or nonoperative treatment, and halo or collar immobilization).
Results
Of 156 patients identified with Type II odontoid fracture, the average age was 82 years (SD = 7.8; Range: 65–101). One hundred and twelve patients (72%) were treated nonoperatively. At 3 years postinjury, there was a 39% (95% CI: 32–47) mortality rate for the entire cohort. Mortality for the operative group was 11% (95% CI: 2–21) at 3 months and 21% (95% CI: 9–32) at 1 year compared with 25% (95% CI: 17–33) at 3 months and 36% (95% CI: 27–45) at 1 year in the nonoperative group. The Cox regression model showed that the protective effect of surgery was seen in patients aged 65 to 74 years, in whom the hazard ratio associated with surgery for mortality after odontoid fracture was 0.4 (95% CI: 0.1–1.5). Those aged 75 to 84 years had a hazard ratio of 0.8 (95% CI: 0.3–2.3), and patients 85 years or older had a hazard ratio of 1.9 (95% CI: 0.6–6.1; P value for interaction between age and treatment = 0.09) with operative treatment having a protective effect in patients aged 65 to 74 years.
Conclusion
In a cohort of elderly patients, Type II odontoid fractures were associated with a high rate of mortality, regardless of intervention.
Keywords: odontoid fracture, elderly, mortality, cervical spine trauma, outcomes
Management of odontoid fractures has been recognized as a challenge, since these injuries were first described in the early 20th century.1 Despite significant advances in diagnostic and treatment methods, such fractures remain problematic, particularly in the geriatric population.1–8 Odontoid fractures are the most common cervical spine fracture in the elderly.1,8 Because of their age associated comorbidities and the ubiquitous presence of degenerative changes in the aging cervical spine,6 such individuals are at a higher risk for complications and poorer outcomes than younger patients sustaining similar injuries.1–4,6,7,9–11 Furthermore, as the number of elderly patients continues to rise in the United States, the prevalence of such fractures can be expected to increase in the future.
Several prior studies have documented increased morbidity and mortality among geriatric patients sustaining odontoid fractures.1–7,9,10,12,13 The nonunion rate in this population has been reported to be as high as 85% (range, 20%–85%),3–7,9,10,12–14 whereas the mortality rate has approached 60% (range, 10%–57.1%).2–7,9,10,12,13 Moreover, the choice of management (operative vs. nonoperative, halo-vest immobilization vs. cervical orthosis) has been postulated to influence mortality. The halo vest, in particular, has been associated with an increased risk of complications and death in elderly patients.1,3,4,7,9,12,15 One study reported high complication rates of pneumonia (34%), cardiac arrest (26%), and mortality (42%) in elderly patients treated with a halo vest.7
Most information on mortality in patients with odontoid fracture is derived from reviews of small cohorts comprising less than 50 patients.3,4,5,7,9,11,13 Furthermore, only one study specifically examined treatment-based outcomes,7 while none have analyzed mortality in relation to age, or medical comorbidities.
Given the paucity of data, this investigation sought to define the influence of age, treatment, and comorbidities on mortality in a cohort (n = 156) of elderly patients sustaining Anderson and D’Alonzo16 Type II fractures of the odontoid in the cervical spine. The hypothesis was that patients treated surgically would have lower mortality than those treated nonoperatively with either a halo vest or cervical orthosis. It was also anticipated that patients with fewer medical comorbidities would have lower mortality regardless of treatment method.
MATERIALS AND METHODS
After the investigational review board approval, the institution’s research patient data registry was used to identify all cervical spine fractures that occurred in patients aged 65 years and older from 1991 to 2006. The research patient data registry is a data registry that has been maintained for all patients treated at two participating Level-I trauma centers since 1979. For the purposes of this study, only those patients determined by the treating physician to have sustained an Anderson and D’Alonzo16 Type II fracture of the odontoid process were reviewed. Additional inclusion criteria included age 65 years or older at the time of injury and radiographic evidence of an acute fracture documented in the electronic medical record.
Data obtained for each patient included age, race, sex, date of injury, fracture classification, associated injuries, presence of neurologic injury, treatment type, presence or absence of 13 medical comorbidities (Charlson index17), and mortality. The research patient data registry was cross-linked with the National Death Index, allowing accurate assessment of patient mortality. Any inconsistencies in the electronic medical record were resolved via a manual review of the patient’s hard copy medical record.
Definitive treatment for the patients’ odontoid fractures was determined by treating physicians at the time of injury. On review, treatments were divided into operative or nonoperative methods. The nonoperative treatment was further stratified into halo vest immobilization or hard cervical orthosis. Patients who received surgery as the Definitive intervention in the acute period (first 3 weeks) after injury were included in the operative group. Patients treated with a halo vest for the majority of their clinical care (i.e., 8 of 12 weeks) were included in the halo vest group. Within each treatment group, patients were stratified by three age strata (65–74 years, 75–84 years, and ≥85 years). The Charlson index was divided into three categories; “0” (no comorbidities), “1 or more” (at least one comorbidity), and “missing.” We created the category of “missing” because 18% of the participants did not have comorbidity data and we wanted to avoid excluding participants from the multivariable analysis.
Risks of mortality for 3-month and 1-, 2-, and 3-year intervals, along with 95% confidence intervals (CIs), were calculated for the entire cohort. The risk of mortality was calculated from the date of injury only. Since we hypothesized that the effect of treatment on the risk of mortality would vary by age, we also calculated mortality risks stratified by age and treatment.
The χ2 test of independence was used to compare mortality between groups, while the Breslow-Day test was performed to test for the interaction between age and treatment. Kaplan-Meier survival curves were also derived to compare treatments for each age group. A propensity score model was constructed that predicted the probability of receiving surgery. Factors in the propensity score model included age, race, sex, preoperative ambulatory status, preoperative living situation, discharge destination, smoking status, trauma type, and neurologic involvement. The propensity score was categorized into quintiles and was controlled for in a multivariable Cox proportional hazard regression analysis that evaluated risk factors for mortality. Propensity scores are a useful way to control for multiple confounding variables when treatment choice is not randomized. This methodology also aids in diminishing bias due to selection processes of treatment choice.18 All statistical analyses were performed using SAS statistical software version 9.1 (SAS Institute Inc, Cary, NC).
RESULTS
Study Sample
Between 1991 and 2006, 640 patients aged 65 years and older presented with cervical spine fractures to the authors’ institutions. Of these individuals, 261 (41%) had fractures involving the second cervical vertebra, of which 242 (93%) involved the odontoid process. The majority (64%) of these odontoid process fractures (n = 156) were found to be Anderson and D’Alonzo Type II fractures as classified by the attending orthopedic surgeon. This cohort represented 24% of all patients aged 65 years and older presenting with cervical spine fractures.
The average age of the 156 patients in our cohort was 82 years (SD: 7.8; range: 65–101). Of these 156 patients, 71 (46%) were male and 21 (13%) were of nonwhite race. Fifty-six patients (36%) sustained odontoid fractures in conjunction with polytrauma and three (2%) cases were associated with neurologic injury. Forty-four (28%) patients received surgery as the Definitive treatment for their fracture, whereas 112 (72%) were managed nonoperatively. Of the 112 patients treated nonoperatively, 28 (25%) were managed with halo-vest immobilization and 84 (75%) were treated with a hard cervical orthosis. Additional demographic data on the investigational cohort stratified by treatment can be found in Table 1.
TABLE 1.
Demographic Characteristics of Patients with Type II Odontoid Fractures
| Operative Treatment, N (%) | Non-Operative Treatment, N (%) | |||
|---|---|---|---|---|
| (N = 44) | All (N = 112) | Halo (N = 28) | Collar (N = 84) | |
| Age | ||||
| 65–74 | 13 (30) | 21 (19) | 10 (36) | 11 (13) |
| 75–84 | 21 (48) | 42 (38) | 8 (29) | 34 (40) |
| ≥85 | 10 (23) | 49 (44) | 10 (36) | 39 (46) |
| Sex | ||||
| Male | 19 (43) | 52 (46) | 16 (57) | 36 (43) |
| Female | 25 (57) | 60 (54) | 12 (43) | 48 (57) |
| Poly-trauma* | ||||
| Yes | 16 (36) | 40 (36) | 10 (36) | 30 (36) |
| No | 28 (64) | 72 (64) | 18 (64) | 54 (64) |
| Charlson comorbidity score | ||||
| 0 | 13 (30) | 32 (29) | 8 (29) | 24 (29) |
| ≥1 | 25 (57) | 58 (52) | 15 (54) | 43 (51) |
| Missing | 6 (14) | 22 (20) | 5 (18) | 17 (20) |
| Neurologic involvement | ||||
| Yes | 2 (5) | 1 (1) | 0 (0) | 1 (1) |
| No | 42 (95) | 111 (99) | 28 (100) | 83 (99) |
The occurrence of injuries to more than one body system or region (i.e., subdural hematoma, pneumothorax, and odontoid fracture).
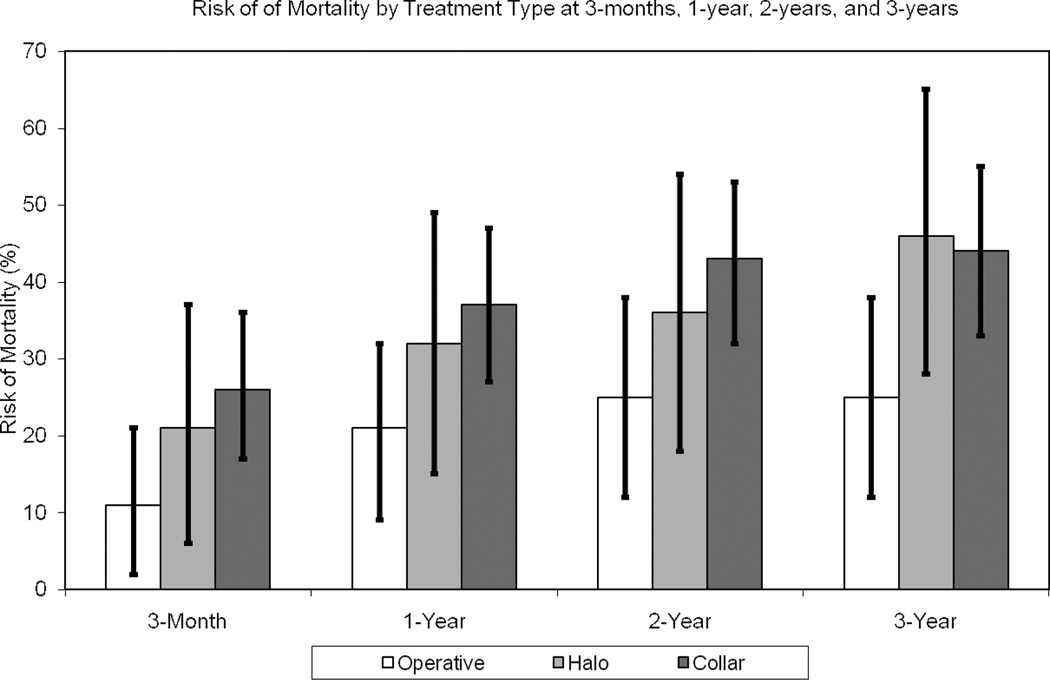
Three-Month Mortality
The mortality rate at 3 months after the date of injury was 21% (33 patients; 95% CI: 15–28). Sixteen patients died during the initial hospital admission, for an in-hospital mortality of 10%. This included one of the 44 patients (2%) who received surgery and 15 of the 112 individuals (13%) managed nonoperatively (P = 0.04). Age was statistically significantly associated with mortality at 3 months (P < 0.01). There was a 6% mortality for patients aged 65 to 74 years, while age groups 75 to 84 years and 85 years or older had 18% and 34% mortalities respectively (Table 2). When comparing nonoperative versus operative groups (Figure 1), the risk of mortality was higher in the nonoperatively treated patients (25% nonoperative vs. 11% operative), but the difference did not reach statistical significance (P = 0.06). The estimated 3-month mortality among patients treated with halo immobilization was 21% (95% CI: 6–37), which was similar to mortality in patients treated with cervical orthosis alone (26%, 95% CI: 17–36) (Figure 1). The Breslow-Day test for interaction did not reveal a statistically significant interaction between age and treatment on the 3-month mortality rate (P = 0.13).
TABLE 2.
Unadjusted Risks of Mortality for Patients with Type II Odontoid Fractures
| 3-month Mortality % (95% CI) |
1-year Mortality % (95% CI) |
|
|---|---|---|
| Overall | 21 (15–28) | 31 (24–39) |
| Age | ||
| 65–74 | 6 (0–14) | 21 (7–34) |
| 75–84 | 18 (8–27) | 29 (17–40) |
| ≥85 | 34 (22–46) | 41 (28–53) |
| Sex | ||
| Male | 23 (13–32) | 32 (22–43) |
| Female | 20 (12–29) | 31 (21–40) |
| Poly-trauma | ||
| Yes | 23 (12–34) | 32 (20–44) |
| No | 20 (12–28) | 31 (22–40) |
| Charlson comorbidity score | ||
| 0 | 13 (3–23) | 18 (7–29) |
| ≥1 | 27 (17–36) | 39 (28–49) |
| Missing | 18 (4–32) | 32 (15–49) |
| Treatment | ||
| Operative | 11 (2–21) | 21 (9–32) |
| Nonoperative | 25 (17–33) | 36 (27–45) |
| Halo | 21 (6–37) | 32 (15–49) |
| Collar | 26 (17–36) | 37 (27–47) |
CI indicates confidence interval.
Figure 1.
Mortality rates for patients categorized by type of treatment.
Patients with a Charlson score of 0 had a 13% (95% CI: 3–23) risk of mortality, while those with a score of one or higher had a 27% (95% CI: 11–44) mortality rate, but due to the sample size this difference did not reach statistical significance (P = 0.20). We did not find an association between sex (P = 0.70) and the presence of polytrauma versus isolated spine trauma (P = 0.64) with 3-month mortality. The risk of mortality stratified by neurologic involvement was not definable because of the small number of patients (3 of 156) who sustained neurologic injury in conjunction with their odontoid fractures.
One-Year Time-Point
The 1-year mortality was 31% (49 patients; 95% CI: 24–39). Patients aged between 65 and 74 years had a 1-year mortality rate of 21% (95% CI: 7–34). Patients aged between 75 and 84 years had a mortality of 29% (95% CI: 17–40), and those 85 years and older had a 41% mortality rate (95% CI: 28–53). The association between patient age and mortality at the 1-year time-point did not reach statistical significance (P = 0.11). At the 1-year time-point, mortality for the operative group was 21% (95% CI: 9–32), while it was 36% (95% CI: 27–45) for the nonoperative group (P = 0.06). Patients treated with halo immobilization had a 32% (95% CI: 14–49) mortality rate, while those managed in a collar had a 37% (95% CI: 27–47) mortality rate (Figure 1), but this difference did not reach statistical significance (P = 0.16). Breslow-Day analysis did not reach a statistically significant threshold for interaction between age and treatment for mortality rates at 1 year (Breslow-Day P for interaction = 0.14).
Patients with a Charlson index of 0 had an 18% (95% CI: 7–29) risk of mortality at 1-year, while those with scores of 1 or higher had a 35% (95% CI: 17–52) risk of mortality (P = 0.05). Sex (P = 0.81) and trauma type (P = 0.88) were not found to have an impact on mortality at the 1-year time-point (Table 2).
Time-points Beyond 1-Year
Mortalities for the cohort at 2 and 3 years were 37% (57 patients; 95% CI: 29–44) and 39% (61 patients; 95% CI: 32–47), respectively. Patients between 65 and 74 years had 2- and 3-year risks of mortality of 24% (95% CI: 9–38) and 29% (95% CI: 14–45). Patients between 75 and −84 years had risks of mortality of 35% (95% CI: 23–47) at 2 and 3 years follow-up. Those 85 years and older had a 46% (95% CI: 33–59) risk of mortality at 2 years, and this increased to 49% (95% CI: 36–62) after 3 years. The association between age and mortality was not statistically significant (P = 0.09 at 2 years and P = 0.12 at 3 years).
At 2- and 3-year time points, mortality for the operative group was 25% (95% CI: 12–38; Figure 1). Patients in the nonoperative cohort had a 41% (95% CI: 32–50) mortality at 2 years and this increased to 45% (95% CI: 35–54) after 3 years. Those treated with halo immobilization had 36% (95% CI: 18–54) and 46% (95% CI: 28–65) mortalities at 2 and 3 years, respectively.
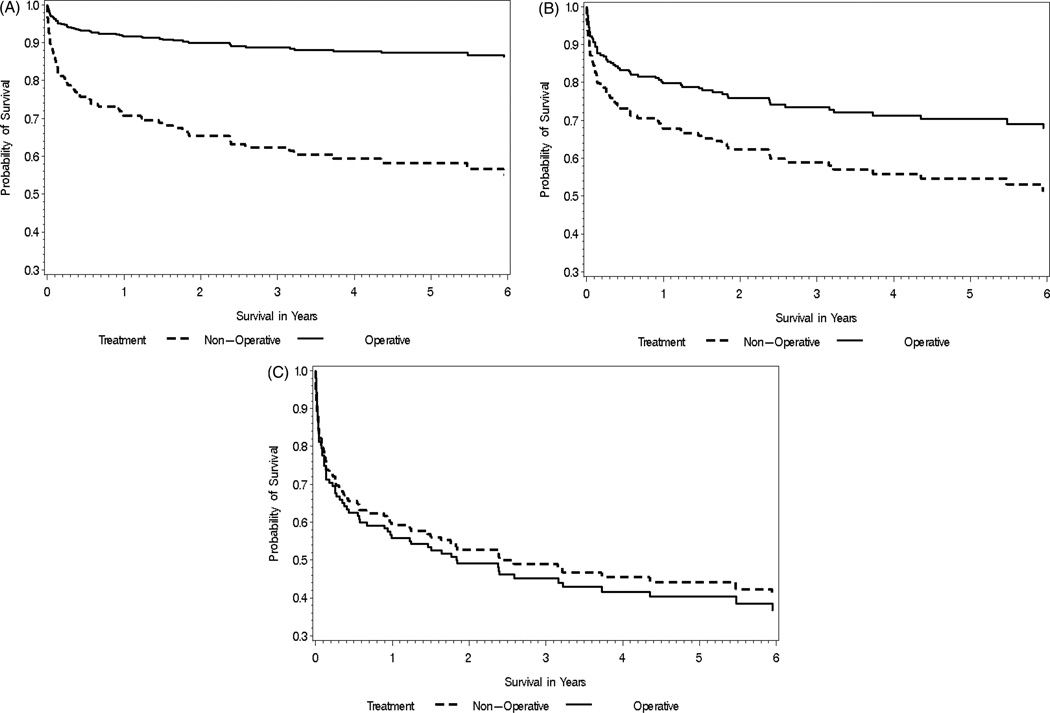
Figure 2A–C demonstrates the effect of treatment on survival for each age group. Surgical intervention appeared to be associated with reduced mortality for patients aged 65 to 74 years (Figure 2A). As patient age increased, this association diminished. Ultimately, the survival curves nearly coincided for those 85 years and older (Figure 2C).
Figure 2.
A, Kaplan-Meier curves depicting survival for patients (A) between 65 and 74 years of age stratified by treatment. B, Kaplan-Meier curves depicting survival for patients between 75 and 84 years of age stratified by treatment. C, Kaplan-Meier curves depicting survival for patients 85 years of age and over stratified by treatment.
MULTIVARIABLE ANALYSIS
For individuals aged 65 to 74 years the hazard ratio associated with surgery for mortality after odontoid fracture was 0.4 (95% CI: 0.1–1.5). Those between 75 and 84 years had a hazard ratio of 0.8 (95% CI: 0.3–2.3), and patients 85 years or older had a hazard ratio of 1.9 (95% CI: 0.6–6.1). The interaction between age and treatment did not reach statistical significance (P = 0.09). Charlson comorbidity index was not associated with mortality when adjusting for the other factors in the model (P = 0.21). The hazard ratio for having at least one comorbidity compared to having zero comorbid conditions was 1.7 (95% CI: 0.9–3.2).
DISCUSSION
Odontoid fractures are the most common cervical spine fracture in elderly patients and are known to carry a high risk of complications and mortality.2–4,6–13,15,19 Over the last 25 years, reports have documented high mortality in this population as a whole and in those patients treated with halo vests in particular.7,12 This trend may be attributed to the elderly population’s increased risk for cardiac events and airway compromise, as well as a markedly decreased functional reserve.12,19–22
In light of these observations, controversy remains regarding the management of odontoid fractures in the elderly.12,19–25 Some authors have advocated aggressive surgical stabilization in these patients, citing an increased fusion, or fracture healing, rate, and decreased morbidity and mortality.4,5,7,9,10,13,23 Other reports, however, have not shown a significant advantage for surgery versus nonoperative management.3,25 In addition, while a few authors have documented the safe and efficacious use of halo-vest immobilization in the elderly,6,24 a number of reports have demonstrated poor outcomes.4,5,7,9,12
The results of the present study suggest that surgical intervention was associated with reduced mortality for individuals aged 65 to 74 years and, to a lesser extent, those patients aged 75 to 84 years. Although this association decreased as patients aged, only 21% of those treated surgically had died at 1-year postinjury compared with 36% of the individuals managed nonoperatively.
The findings presented here also support prior evidence of increased mortality rates among elderly patients with odontoid fractures, irrespective of the choice of treatment. For example, the in-hospital mortality rate in this study was 10%. Three papers have previously cited a greater than 25% in-hospital mortality rate in patients aged 65 years and older with similar injuries.3,7,10 Koech et al24 focused entirely on nonoperative management of such patients with odontoid fractures, reported a 14% in-hospital mortality.
In addition, the results of this study show a high mortality rate over the first 3 months postinjury that plateaus within 1 to 2 years. The mortality in this investigation may have been influenced by the presence of medical comorbidities. Cox proportional hazard regression analysis demonstrated a hazard ratio of 1.7 (95% CI: 1–3) for patients having at least one comorbidity. The presence of medical comorbidities may predispose patients to an increased risk of complications in the setting of fracture care, such as thromboembolic disease, urinary tract infections, cardiac events, and pneumonia.7,12,26 The recent work of Stelfox et al26 has documented a higher complication rate in elderly patients treated with prolonged cervical immobilization and such a factor may account for the disparate outcomes between cohorts in this investigation. Nonetheless, both Koech et al,24 and Hart and colleagues,27 documented satisfactory outcomes in elderly patients with odontoid fractures treated nonoperatively. Both of these investigations were limited by small patient cohorts.
The 3-month mortality in this investigation is comparable to figures presented by Frangen et al4 while the 2-year mortality is lower than the 47% rate reported in the work of Hanigan and colleagues.10 Comparison with national mortality data28 demonstrates a substantially increased risk of mortality for patients aged 65 years and older who sustain odontoid fractures. Between 2002 and 2004, the mortality rate for all persons aged 65 to 74 years was 2.2%, while it was 5.3% for individuals aged 75 to 84 years and 13.9% for those 85 years and older.28 Results presented here indicate a three-fold increase in mortality for patients aged 85 years and older who sustain an odontoid fracture. For those aged 65 to 74 years, the mortality risk is increased 10-fold. These findings are in keeping with recent data published by Bliuc et al.29 These authors found an increased risk of mortality for patients older than the age of 60 years who sustained both hip and vertebral fractures. In addition, the mortality risk remained elevated from 5 to 10 years after injury.29 While the data presented here cannot elucidate whether mortality was directly related to the fracture, or to complications surrounding fracture care, it does suggest that such injuries are a marker for an increased risk of mortality at 1 year.
Of note, patients in this study who were treated with halo immobilization were not found to be at increased risk for mortality when compared with patients receiving operative intervention or a cervical orthosis (Figure 1). This is in contrast to prior reports documenting a high mortality rate among patients 65 years and older treated with a halo.7,12 Majercik et al12 and Tashjian and colleagues7 each documented greater than 40% acute mortality rates for elderly patients treated with halo-vest immobilization. Mortality rates for those managed with halo vests in this study were markedly lower: 21% at 3 months and 32% at 1 year. Similarly, mortality rates for the operative and nonoperative cohorts in this investigation were lower than previously reported estimates.3,4,10
It is important to note that most other studies in the literature consist of small samples with short-term follow-up and an average patient age of 81 years.3–5,7,9,10,24 To the best of our knowledge, this series represents one of the larger studies investigating mortality in patients aged 65 years and older with Type II odontoid fractures and midrange follow-up. Therefore, the mortality estimates presented here may be more valid than those documented in studies of smaller cohorts with less than 2-year follow-up. Moreover, as the average age of patients in prior investigations was 81 years, it is possible that the higher mortality rates could be attributed to patient age alone. Unfortunately, most previous reports have not stratified patient cohorts by age.
There are several limitations to the current investigation. First, this was a retrospective study, conducted using information compiled from an institutional database. Therefore, it suffers from the limitations inherent in all retrospective reviews, including bias regarding surgical indication. It is possible that the perceived association between surgery and decreased mortality may be due to the selection of patients better able to tolerate surgical intervention. While we have attempted to adjust for selection bias using sophisticated analytic techniques, we fully acknowledge that residual confounding by indication is possible. These data must be interpreted cautiously. The most accurate answer to the question of optimal intervention could only be derived from a prospective, randomized trial that allocated elderly patients to specific arms of operative or nonoperative management, stratifying them by age.
Another limitation was that data regarding the cause of death were not recorded. Such information would have been useful to quantify the number of patients who died of complications directly related to their odontoid fracture, or from the treatment rendered. As findings in this study demonstrated higher mortality rates among patients of advanced age, as well as in those with more comorbidities, the roles of treatment, comorbidity, and age could have been more clearly elucidated had the cause of death been recorded. Also, with regard to our data collection, fracture stability and displacement were not recorded. These two variables may be related to treatment choice and thus confound the association between treatment and mortality. However, we did control for trauma type and neurologic involvement in our propensity score as markers of injury severity.
Further limitations include the fact that the diagnosis of Type II odontoid fracture was solely based on documentation in the medical record, as well as the 15-year span over which patients presenting with odontoid fractures were included in this study. As the presence of Type II odontoid fracture was not independently confirmed, it is possible that some patients included in this study did not have true Type II fractures. This is additionally complicated by the fact that the Anderson and D’Alonzo classification used in this study has been found to have poor inter-rater reliability.30 In addition, over the course of the 15 years in which patients included in this study presented with odontoid fractures, substantial changes occurred in the biomechanical understanding of these injuries and the surgical techniques available for treatment. This further complicates any comparison between the operative and nonoperative cohorts in this investigation.
CONCLUSIONS
The results of this investigation confirm the devastating nature of odontoid fractures in the geriatric population. This study also highlights a mortality rate that increases with patient age and the number of comorbidities. While surgery was associated with reduced mortality in patients younger than 75 years of age, the analyses of treatment effects are vulnerable to confounding by indication and, therefore, do not permit firm conclusions. Prospective research must be conducted to definitively describe the factors responsible for mortality in elderly patients with odontoid fractures. However, in light of the findings presented here, future investigations regarding outcomes in elderly patients with odontoid fractures should stratify patients by age.
Key Points.
-
□
There is a high mortality rate for elderly patients within 1 year after an acute Type II odontoid fracture regardless of intervention.
-
□
Mortality risk increases with advancing patient age and the number of comorbidities.
-
□
It is difficult to evaluate the effect of surgery on mortality because of selection bias. With this limitation in mind, the data suggest that surgery may offer a protective benefit in patients younger than 75 years of age.
Footnotes
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
References
- 1.Chutkan NB, King AG, Harris MB. Odontoid fractures: evaluation and management. J Am Acad Orthop Surg. 1997;5(4):199–204. doi: 10.5435/00124635-199707000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Spivak JM, Weiss MA, Cotler JM, et al. Cervical spine injuries in patients 65 and older. Spine. 1994;19(20):2302–2306. doi: 10.1097/00007632-199410150-00009. [DOI] [PubMed] [Google Scholar]
- 3.Muller EJ, Wick M, Russe O, et al. Management of odontoid fractures in the elderly. Eur Spine J. 1999;8(5):360–365. doi: 10.1007/s005860050188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frangen TM, Zilkens C, Muhr G, et al. Odontoid fractures in the elderly: dorsal C1/C2 fusion is superior to halo-vest immobilization. J Trauma. 2007;63(1):83–89. doi: 10.1097/TA.0b013e318060d2b9. [DOI] [PubMed] [Google Scholar]
- 5.Bednar DA, Parikh J, Hummel J. Management of type II odontoid process fractures in geriatric patients: a prospective study of sequential cohorts with attention to survivorship. J Spinal Dis. 1995;8(2):166–169. [PubMed] [Google Scholar]
- 6.Malik SA, Murphy M, Connolly P, et al. Evaluation of morbidity, mortality and outcome following cervical spine injuries in elderly patients. Eur Spine J. 2008;17(4):585–591. doi: 10.1007/s00586-008-0603-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tashjian RZ, Majercik S, Biffl WL, et al. Halo-vest immobilization increased early morbidity and mortality in elderly odontoid fractures. J Trauma. 2006;60(1):199–203. doi: 10.1097/01.ta.0000197426.72261.17. [DOI] [PubMed] [Google Scholar]
- 8.Greene KA, Dickman CA, Marciano FF, et al. Acute axis fractures: analysis of management and outcome in 340 consecutive cases. Spine. 1997;22(16):1843–1852. doi: 10.1097/00007632-199708150-00009. [DOI] [PubMed] [Google Scholar]
- 9.Pepin JW, Bourne RB, Hawkins RJ. Odontoid fractures, with special reference to the elderly patient. Clin Orthop Rel Res. 1985;193:178–183. [PubMed] [Google Scholar]
- 10.Hanigan WC, Powell FC, Elwood PW, et al. Odontoid fractures in elderly patients. J Neurosurg. 1993;78(1):32–35. doi: 10.3171/jns.1993.78.1.0032. [DOI] [PubMed] [Google Scholar]
- 11.Platzer P, Thalhammer G, Ostermann R, et al. Anterior screw fixation of odontoid fractures comparing younger and elderly patients. Spine. 2007;32(16):1714–1720. doi: 10.1097/BRS.0b013e3180dc9758. [DOI] [PubMed] [Google Scholar]
- 12.Majercik S, Tashjian RZ, Biffl WL, et al. Halo vest immobilization in the elderly: a death sentence? J Trauma. 2005;59(2):350–357. doi: 10.1097/01.ta.0000174671.07664.7c. [DOI] [PubMed] [Google Scholar]
- 13.Kuntz C, IV, Mirza SK, Jarell AD, et al. Type II odontoid fractures in the elderly: early failure of nonsurgical treatment. Neurosurgical Focus. 2000;8(6):e7. doi: 10.3171/foc.2000.8.6.8. [DOI] [PubMed] [Google Scholar]
- 14.Schatzker J, Rorabeck CH, Waddell JP. Fractures of the dens (odontoid process): an analysis of thirty-seven cases. J Bone Joint Surg Br. 1971;53(3):392–405. [PubMed] [Google Scholar]
- 15.Ryan MD, Taylor TK. Odontoid fractures—a rational approach to treatment. J Bone Joint Surg Br. 1982;64(4):416–421. doi: 10.1302/0301-620X.64B4.7096414. [DOI] [PubMed] [Google Scholar]
- 16.Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56(8):1663–1674. [PubMed] [Google Scholar]
- 17.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic co-morbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 18.D’Agostino RB., Jr Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17(19):2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 19.Damadi AA, Saxe AW, Fath JJ, et al. Cervical spine fractures in patients 65 years or older: a 3-year experience at a level I trauma center. J Trauma. 2008;64(3):745–748. doi: 10.1097/TA.0b013e3180341fc6. [DOI] [PubMed] [Google Scholar]
- 20.Golob JF, Claridge JA, Yowler CJ, et al. Isolated cervical spine fractures in the elderly: a deadly injury. J Trauma. 2008;64(2):311–315. doi: 10.1097/TA.0b013e3181627625. [DOI] [PubMed] [Google Scholar]
- 21.Kuhne CA, Ruchholtz S, Kaiser GM, et al. Working Group On Multiple Trauma Of The German Society Of Trauma. Mortality in severely injured elderly trauma patients–when does age become a risk factor? World J Surg. 2005;29(11):1476–1482. doi: 10.1007/s00268-005-7796-y. [DOI] [PubMed] [Google Scholar]
- 22.Smith DP, Enderson BL, Maull KI. Trauma in the elderly: determinants of outcome. South Med J. 1990;83(2):171–177. doi: 10.1097/00007611-199002000-00010. [DOI] [PubMed] [Google Scholar]
- 23.Omeis I, Duggal N, Rubano J, et al. Surgical treatment of C2 fractures in the elderly: a multicenter retrospective analysis. J Spinal Disord Tech. 2009;22(2):91–95. doi: 10.1097/BSD.0b013e3181723d1b. [DOI] [PubMed] [Google Scholar]
- 24.Koech F, Ackland HM, Varma DK, et al. Nonoperative management of type II odontoid fractures in the elderly. Spine. 2008;33(26):2881–2886. doi: 10.1097/BRS.0b013e31818d5407. [DOI] [PubMed] [Google Scholar]
- 25.Smith HE, Kerr SM, Maltenfort M, et al. Early complications of surgical versus conservative treatment of isolated type II odontoid fractures in octogenarians: a retrospective cohort study. J Spinal Disord Tech. 2008;21:535–539. doi: 10.1097/BSD.0b013e318163570b. [DOI] [PubMed] [Google Scholar]
- 26.Stelfox H, Velmahos G, Gettings E, et al. Computed tomography for early and safe discontinuation of cervical spine immobilization in obtunded multiply injured patients. J Trauma. 2007;63(3):630–636. doi: 10.1097/TA.0b013e318076b537. [DOI] [PubMed] [Google Scholar]
- 27.Hart R, Saterbak A, Rapp T, et al. Nonoperative management of dens fracture nonunion in elderly patients without myelopathy. Spine. 2000;25(11):1339–1343. doi: 10.1097/00007632-200006010-00004. [DOI] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention. Death rates by 10-year age groups: United States and each state, 1999–2007. [Accessed April 7, 2011]; http://www.cdc.gov/nchs/nvss/mortality/gmwk23r.htm.
- 29.Bliuc D, Nguyen ND, Milch VE, et al. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301(5):513–521. doi: 10.1001/jama.2009.50. [DOI] [PubMed] [Google Scholar]
- 30.Barker L, Anderson J, Chestnut R, et al. Reliability and reproducibility of dens fracture classification with use of plain radiography and reformatted computer-aided tomography. J Bone Joint Surg Am. 2006;88(1):106–112. doi: 10.2106/JBJS.D.02834. [DOI] [PubMed] [Google Scholar]