Abstract
Handoff communication is a point of vulnerability when valuable patient information can be inaccurate or omitted. In 2005 we implemented a protocol to improve the handoff process for children from the operating room to the intensive care unit after cardiac surgery. We performed a cross-sectional study of the present process to understand how users adapt a communication intervention over time. 29 handoff events were observed. Individuals required for the handoff were present at 97% of events. Content items averaged a 53% reporting rate. Some clinical information not specified in the protocol demonstrated a higher reporting rate, such as echocardiogram results (68%) and vascular access (79%). A mean of 2.3 environmental distractions per minute of communication were noted. Participant-directed adjustments in content reporting suggest that a facilitator in process improvement is user-centered innovation. Future handoff communication interventions should reduce nonessential distractions and incorporate a discussion of the anticipated patient course.
Keywords: handoff, safety, communication, pediatric intensive care units, congenital heart defects, postoperative care
BACKGROUND
Handoffs are contemporaneous, interactive processes of passing patient-specific information from one caregiver to another for the purpose of ensuring the continuity and safety of patient care.1 Handoff communication is a point of vulnerability where valuable patient information can be distorted or omitted.2-5 Due to the association of communication errors with adverse events,6 the Joint Commission has proposed implementing a standardized approach to handoff communication as a national patient safety goal.7
The handoff process for critically ill children admitted from the operating room (OR) to the pediatric intensive care unit (PICU) may be prone to error. Potential causes include: 1) the handoff often takes place in a busy, distraction-rich environment; 2) it involves the near simultaneous transfer of equipment and knowledge; 3) staff may have no prior knowledge of the patient’s medical history and thus depend on this process for critical information; 4) patients are often clinically unstable during the immediate admission period, which limits time for reviewing the medical record. In a recent study of pediatric surgical handoffs, communication errors occurred in 100% of events, with an average of 6.6 errors per handoff.3
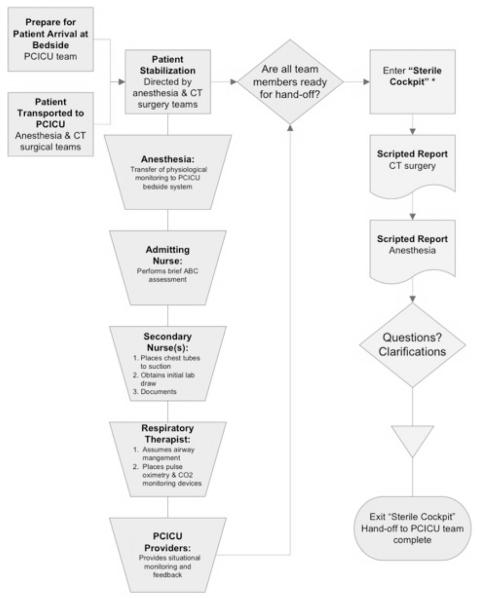
In 2005, faculty and staff in the Duke Pediatric Cardiac Intensive Care Unit (PCICU) suggested that handoff communication from the operating room team to the intensive care unit team following surgery for pediatric heart disease occurred despite the absence of members of key disciplines, included a non-standard format of information reporting, and took place in a setting fraught with avoidable distractions. In response, users designed a formal protocol to address communication gaps for children after undergoing cardiac surgery (Figure 1). Opinions were solicited from frontline providers in pediatric intensive care, cardiology, cardiac surgery, and anesthesiology. Interview and survey results were used to design the policy guideline. The resulting protocol specified 1) attendance at the handoff 2) fourteen content items to be verbally communicated and 3) a “sterile cockpit” environment, in which personnel refrain from non-essential activities in order to minimize distractions during important tasks. The sterile cockpit was to be announced by the patient’s primary bedside nurse before starting communication. To prepare for implementation, participants in the process underwent a team-training program focused on standardization of communication and the application of critical language. Additional team-training sessions were held every two to three months.
Figure 1.
Process flow map for the post-operative cardiac surgery handoff protocol.
Following implementation of the protocol, the following short-term clinical metrics improved: reduction of transition time from the OR team to the PCICU team (15.3 to 9.6 min); reduction of time to obtain critical laboratory studies (13.0 to 2.4 min); and an increase in chest radiographs completed (60% vs. 94%) and percent of patients placed on bedside cardio-respiratory monitoring within unit standards (86% vs. 99%).8 Although unit leaders encouraged compliance with the protocol, no communication metrics have been evaluated since implementation.
Although studies have examined deficiencies in handoffs2-5 and implementation of handoff protocols,9-11 little research exists on how communication strategies evolve over time. The aim of this study was to understand how users adapt a handoff process by evaluating the present practice.
METHODS
Study Design / Location
We performed an observational, cross-sectional study of handoff communication events occurring in the PCICU between the cardiothoracic surgery / anesthesiology team and the pediatric critical care team following cardiac surgery. Handoff events were identified through convenience sampling and evaluated by the principal investigator (JGC). Data were collected from January 2008 to August 2008. At the time of this study, the PCICU shared the same physical location as the multidisciplinary PICU, but PCICU patients were managed by a core nursing group with specialized cardiac training. The institution admits approximately 350 pediatric cardiac surgery cases postoperatively to the PCICU each year. Approval for the study was obtained from the Duke University Institutional Review Board.
Subjects
Study subjects comprised individuals involved in the handoff process, including faculty and trainee physicians from the disciplines of cardiothroacic surgery, cardiac anesthesiology, and intensive care, and staff from nursing and respiratory therapy. In a typical handoff, the cardiothoracic surgery and anesthesiology teams accompany the patient from the OR and transition care to the pediatric critical care team in the PCICU.
Outcomes
The primary outcome was the reliability of attendance. Reliability was defined as the frequency that a member of a particular discipline was present at the observed handoffs. For cardiothoracic surgery, anesthesia, and intensive care, a discipline member could be an attending, fellow, or nurse practitioner. A discipline was noted as absent if a member was not present at the start of the handoff.
A secondary outcome was the reliability of content reporting. Reliability was defined as the frequency that an item was reported at the observed handoffs. The original protocol specified 14 required content items. In addition, during the design of the study frontline providers suggested 29 additional content items that were not listed in the protocol, but may have been relevant to the care of the patient. Some of these users had also participated in the development of the original process. An omission was defined as an item that was not mentioned during the handoff. Anesthesia records were reviewed to see if the items were relevant to the patient before counting them as omissions. For example, if the patient did not have pacing wires and it was not reported, an omission was not noted.
Another secondary outcome was the number of distractions during the duration of communication for each handoff. A distraction was defined as an event in the room that had the potential to engage the attention of a process participant. Distractions were divided into ones that were nonessential to patient care (extraneous staff leaving or entering the room, unrelated side conversations, and television or music playing); and ones that were essential to patient care (phones ringing, overhead pages, pagers beeping, monitors alarming, and equipment failures). If a process participant looked towards the distraction, the distraction was characterized as one that engaged the attention of a process participant.
Patient age and the primary surgical procedure were recorded. Complexity of the surgical procedure was assessed with the Risk Adjustment for Congenital Heart Surgery (RACHS) score. The score ranges from 1 to 6; lower scores designate surgeries of low complexity (e.g. patent ductus arteriosus ligation - RACHS 1), and higher scores refer to surgeries with high complexity (e.g. Stage 1 palliation for single ventricle physiology - RACHS 6).12 The duration of handoff communication was also recorded.
Statistical Analysis
We estimated that observing approximately 30 handoffs would provide a representative sample of patients and surgical procedures seen in our PCICU. Descriptive statistics were used to summarize attendance, content, and distraction data. The t-test was used to compare means for parametric distribution, and the Mann-Whitney test was used to compare medians for nonparametric distributions. STATA version 10 (College Station, TX) was used for analysis.
RESULTS
From January 2008 to August 2008, 135 children were admitted to the Duke PCICU following surgery for pediatric heart disease. 29 (22%) of these handoff events were observed. In the sample, 38% of patients were newborns less than 30 days old. Ten patients (34%) had RACHS 1-2, 13 (45%) had RACHS 3-4, and 6 (21%) had RACHS 5-6. Table 1 compares age and complexity of diagnosis in the sample to all the post-surgical patients admitted during the observation period. The mean duration of handoff communication was 4:01 minutes (standard deviation (SD) 1:15 minutes).
Table 1.
Sample cases versus all cardiac surgery cases during the study period.
| Sample Cases | Other Cardiac Surgery Cases |
p-value | |
|---|---|---|---|
| N | 29 | 113 | |
| Age – median (interquartile range) |
175d (7d to 1083d) | 134d (36d to 792d) | 0.86* |
| RACHS – mean (standard deviation) |
3.21 (1.66) | 2.56 (1.34) | 0.03** |
Mann-Whitney non-parametric test.
Independent samples parametric t-test.
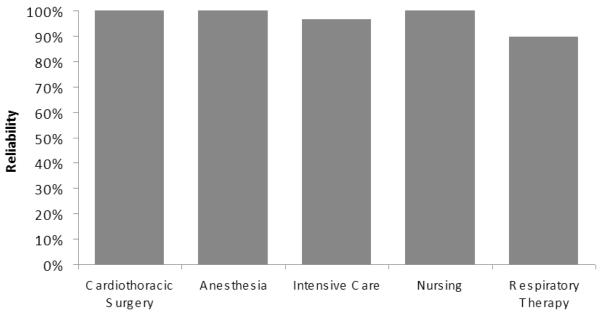
Protocol-required disciplines averaged a 97% (95% CI: 93% to 100%) attendance rate per handoff event (Figure 2). Representatives from cardiothoracic surgery, cardiac anesthesia, and critical care nursing were present for all handoffs; intensive care physicians and/or nurse practitioners were present for all but one handoff (97%); and respiratory therapy was present for all but 3 handoffs (90%).
Figure 2.
Reliability of attendance. Reliability was defined as the frequency that a member of a particular discipline was present at the observed handoffs.
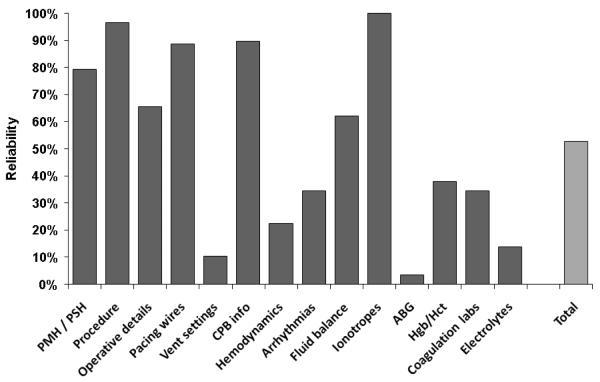
Protocol-required content items averaged a 53% (95% CI: 35% to 71%) reporting rate per handoff event (Figure 3). Some items, such as the procedure (97%) demonstrated a high reporting rate; others, such as hemodynamics (22%), did not. Table 2 depicts the percentage of the time content items not specified in the protocol were reported. Some of these items were reported often, such as the presence of chest tubes (86%), results of the post-operative echocardiogram (68%), and vascular access (79%).
Figure 3.
Reliability of the 14 content items required by the protocol. Reliability was defined as the frequency that an item was reported at the observed handoffs. PMH / PSH = past medical history / past surgical history; vent = ventilator; CPB = cardiopulmonary bypass; ABG = arterial blood gas; Hgb/Hct = hemoglobin/hematocrit.
Table 2.
Reporting rate of 29 content items not specified by the protocol.
| Frequency of reporting | |
|---|---|
| Patient information | |
| Name | 83% |
| Age | 72% |
| Weight | 28% |
| Allergies | 21% |
| Home medications | 7% |
| Cardiac surgery information | |
| Chest Tubes | 86% |
| Atrial lines | 79% |
| Post-op echocardiogram | 68% |
| Surgeon / Assistant | 14% |
| Pre-op echocardiogram | 9% |
| Open Chest? | 0% |
| Anesthesia information | |
| Vascular access | 79% |
| ETT details | 76% |
| Antibiotics | 59% |
| Blood products available | 50% |
| Milrinone load | 44% |
| Pain meds / reversal | 41% |
| Induction medications | 34% |
| Grade / visualization of airway | 28% |
| Cerebral oximeter | 23% |
| Blood loss / fluid loss | 17% |
| Lactate | 17% |
| Inotropes during case | 10% |
| O2sat | 3% |
| MvO2 | 3% |
| Anesthesiologist / Assistant | 0% |
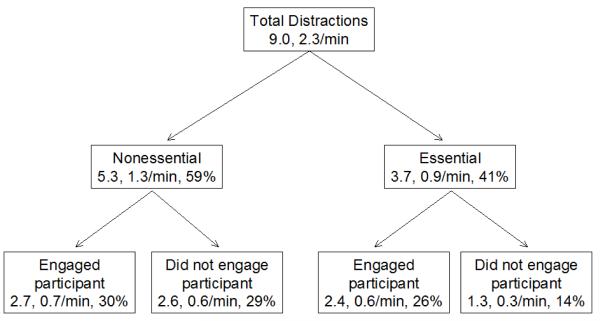
The primary bedside nurse announced the sterile cockpit and initiated communication in 6 of the handoffs (21%). There was a mean of 9.0 (SD 2.8) distractions per event; this was equivalent to 2.3 distractions per minute of communication. 5.3 distractions (1.3 per minute) were nonessential to patient care; 2.7 distractions (0.7 per minute) were nonessential and engaged the attention of a process participant (Figure 4).
Figure 4.
Distractions per handoff, broken down into those nonessential for patient care (extraneous staff leaving or entering the room, unrelated side conversations, and television or music playing); and those essential to patient care (phones ringing, overhead pages, pagers beeping, monitors alarming, and equipment failures); and those that engaged the attention of a process participant and those that did not. The total number of distractions in each handoff, distractions per minute of communication, and the percentage of the total number of distractions are noted.
Cardiothoracic surgeons and anesthesiologists discussed the anticipated post-operative course in 14% and 17% of handoffs, respectively. Time was allotted for questions in 67% of handoff events.
DISCUSSION
Three years after implementation, this handoff process demonstrated high and consistent reliability in attendance, variable reliability in required content reporting, and numerous nonessential distractions. Given the chaotic nature of the intensive care unit and unpredictability of patient acuity it may be unrealistic to expect perfect conformity to such a complex process.
Attendance was reliable for a number of possible reasons. Tradition at our institution dictated that a surgeon and anesthesiologist accompany the patient from the OR to the intensive care unit for all complex operative cases. A paging system notified the unit charge nurse and intensive care unit team immediately before and upon arrival of the patient. Participants may have believed that attendance was the first and most essential step when transitioning sick patients utilizing a complex handoff process. Indeed, other studies have suggested that face-to-face communication is preferable to indirect handoffs through a medium such as the telephone.4, 13 The minor deficiencies in attendance by intensive care unit physicians and respiratory therapists may be due to competing demands in a busy critical care environment. There was certainly a gap between conformity to attendance and deficiencies in following the rest of the protocol. Unlike attendance, there was no tradition of relaying standardized content, there was no reminder system for verbal communication, and participants may not have appreciated the importance of standardized reporting and minimal distractions during transitions in patient care.
Knowledge of some of the items not required by the protocol, such as patient weight, allergies, and vascular access, may be essential to postoperative care in the PICU. While designing the protocol it was believed that these items could easily be obtained from the electronic medical record or anesthesia record, and therefore were not necessary for the formal handoff. However, verbal communication of these data may facilitate timely care of critically ill patients by team members immediately after the transition. Accordingly, surgeons and anesthesiologists frequently reported some items not required by the protocol.
These participant-directed adjustments over time suggest that a key facilitator in process improvement is user-centered innovation. In a traditional model, administrators identify needs of users and fill them by designing products. User-centered innovation, or the exercise of participants developing and applying their own processes and services, demonstrates advantages over this model. Compared to administrators, users have a more accurate and detailed model of their deficiencies, develop what they require for their own specific circumstances, benefit directly from their innovations and thus have motivation to pursue improvements, and often freely reveal their products to other parties for modification. Moreover, user-centered innovation will only increase in frequency with improved access to computing tools and information networks.14 A standardized system that continuously incorporates feedback from process participants may benefit process performance. This idea has also been proposed in a multicenter qualitative survey of intensive care unit providers.15
Handoffs ideally should occur is a private, quiet setting with minimal interruptions.7, 13 The protocol specified that information transfer occur in a ‘sterile cockpit’ with limited distractions, where participants can focus their attention solely on the dissemination of information. However, observed handoffs demonstrated numerous distractions, with more than half being nonessential, and more than half of nonessential distractions actually engaging process participants. Studies have noted intrusive distractions in busy environments such as primary care offices,16 emergency departments,17, 18 and operating rooms.19-21 Reducing nonessential distractions represents an area for improvement.
A goal of handoff communication is to create a cognitive picture of the patient that will translate into effective decision-making.7 Surveys of housestaff suggest that discussing anticipated problems during a handoff is essential for patient care.4 In this study, discussing the anticipated patient course occurred infrequently and represents another area for improvement. There was an opportunity to ask questions after the majority of events, which reflects a key Joint Commission recommendation for an ideal handoff.7
In the future, we can enhance compliance for this and other communication processes by defining facilitators and barriers to sustainability. In research on clinician adherence to practice guidelines, major barriers occur at the individual, team, and hospital or health center level,22 and may include lack of awareness and familiarity with the protocol, disagreement with the process, belief that the protocol may not change outcomes due to sparse data, and lack of resources for implementation.23 A qualitative survey of intensive care unit leaders has suggested that maintaining effective process leadership, retaining experienced providers, and re-education improve adherence to clinical guidelines;15 such endeavors may enhance sustainability for communication initiatives as well. While this study did not demonstrate overwhelmingly positive results, the reliability of attendance and enthusiasm of faculty and staff during the project indicate that there is strong interest in improving handoff communication during transitions in care at our institution. The next step involves addressing other ways to improve sustainability. At present there is no ownership of the communication process due to turnover among leadership, and therefore no data has been collected since this study. Ways to sustain compliance and continually improve this protocol at our institution may include identifying strong leaders, collecting and publicizing future data, and mandating education sessions at regular intervals.
This study represents the first evaluation of a post-operative handoff process beyond the immediate implementation period. While other studies have examined content omissions3, 10 during post-operative handoff communication, this is the first study to assess content reporting outside the protocol and thus detect provider efforts to improve the practice. Quantitatively measuring attendance and distractions is a novel addition to the study of handoff communication.
Limitations include the fact that no communication metrics were recorded immediately after implementation. We thus do not know if reliability has changed since implementation, but recent dissatisfaction among participants suggests that the process has indeed worsened over time. There may be a Hawthorne effect in this study, in which process participants may have behaved differently under observation. However, this effect would be expected to bias the handoff towards improved content and distraction outcomes, and this study demonstrated subpar performance in these portions of the process. Convenience sampling was used due to the unpredictable timing of surgery cases. Sample cases demonstrated higher surgical complexity, but it is unclear how this would affect results. Higher patient acuity may have encouraged participants to pass along more information, but also may have hindered transfer during the communication period. There was only a single observer, which may limit the reliability of the data. Finally, this single-center study took place an intensive care unit with a moderate surgical volume and numerous opportunities to practice the process, possibly limiting the generalizability of the results.
Future directions include addressing the process deficiencies uncovered in this study, eliciting facilitators to sustainability for this and other communication processes, and exploring modalities for communication education such as simulation that could recreate a realistic handoff environment and assess comprehension in handoff recipients.
CONCLUSION
Initiatives to improve this handoff communication process include reducing non-essential distractions and incorporating a discussion of the anticipated patient course. Participant-directed adjustments over time suggest that user-centered innovation is a modality for process improvement in health care. Ways to sustain compliance may include identifying strong leaders, collecting and publicizing future data, and mandating education sessions at regular intervals. Interventions to improve post-operative handoff communication should ensure attendance by key personnel and include an opportunity for questions.
Acknowledgments
This project was supported with divisional funds from the Division of Pediatric Critical Care, Department of Pediatrics, Duke University Medical Center.
Footnotes
This study was presented in abstract form at the Society of Critical Care Medicine 38th Annual Congress as: Chen JG, Wright MC, Mistry KP. Sustaining the Success of Quality Improvement Initiatives: Evaluating a Post-Operative Cardiac Surgery Handoff Process.
CONFLICTS OF INTEREST AND FINANCIAL DISCLOSURES
The authors have no conflicts of interest nor financial disclosures to report.
REFERENCES
- 1.Joint Commission . Compliance Strategies for the Universal Protocol. 1st edition Vol. 63. Joint Commission Resources; 2007. [Google Scholar]
- 2.Carter AJ, David KA, Evans LV, Cone DC. Information loss in emergency medical services handover of trauma patients. Prehosp Emerg Care. 2009;13(3):280–5. doi: 10.1080/10903120802706260. [DOI] [PubMed] [Google Scholar]
- 3.Mistry KP, Landrigan CP, Goldman DA, Bates DW. Communication During Post-Operative Patient Handoff in the Pediatric Intensive Care Unit. Abstract, Society of Critical Care Medicine 35th Critical Care Congress. Crit Care Med. 2005;33(12):A12. [Google Scholar]
- 4.Arora V, Johnson J, Lovinger D, Humphrey HJ, Meltzer DO. Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care. 2005;14:401–7. doi: 10.1136/qshc.2005.015107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bomba DT, Prakash R. A description of handover processes in an Australian public hospital. Aust Health Rev. 2005;29:68–79. doi: 10.1071/ah050068. [DOI] [PubMed] [Google Scholar]
- 6.Joint Commission The Joint Commission’s Annual Report on Quality and Safety 2007. Sentinel Event Root Cause and Trend Data. :45–46. [Google Scholar]
- 7.Joint Commission [accessed 23 Sept 2009];2009 National Patient Safety Goals. 2008 November; http://www.jointcommission.org/NR/rdonlyres/31666E86-E7F4-423E-9BE8-F05BD1CB0AA8/0/HAP_NPSG.pdf.
- 8.Mistry KP, Norman S, Mericle J, Kern FH, Meliones JN, Lodge AJ, Jaggers J. Structured communication and team training improve handoffs of postoperative pediatric cardiovascular (CV) patients. Abstract, Society of Critical Care Medicine 36th Critical Care Congress. Crit Care Med. 2006;34(12):A60. [Google Scholar]
- 9.Wayne JD, Tyagi R, Reinhardt G, et al. Simple standardized patient handoff system that increases accuracy and completeness. J Surg Educ. 2008;65:476–85. doi: 10.1016/j.jsurg.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 10.Catchpole KR, de Leval MR, McEwan A, et al. Patient handover from surgery to intensive care: using Formula 1 pit-stop and aviation models to improve safety and quality. Paediatr Anaesth. 2007;17(5):470–8. doi: 10.1111/j.1460-9592.2006.02239.x. [DOI] [PubMed] [Google Scholar]
- 11.Petersen LA, Orav EJ, Teich JM, O’Neil AC, Brennan TA. Using a computerized sign-out program to improve continuity of inpatient care and prevent adverse events. Jt Comm J Qual Improv. 1998;24(2):77–87. doi: 10.1016/s1070-3241(16)30363-7. [DOI] [PubMed] [Google Scholar]
- 12.Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI. Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg. 2002;123(1):6–7. doi: 10.1067/mtc.2002.119064. [DOI] [PubMed] [Google Scholar]
- 13.Solet DJ, Norvell JM, Rutan GH, Frankel RM. Lost in translation: challenges and opportunities in physician-to-physician communication during patient handoffs. Acad Med. 2005;80(12):1094–1099. doi: 10.1097/00001888-200512000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Von Hippel E. Democratizing Innovation. MIT Press; Cambridge, MA: 2005. pp. 16–33. [Google Scholar]
- 15.Sinuff T, Cook D, Giacomini M, Heyland D, Dodek P. Facilitating clinician adherence to guidelines in the intensive care unit: A multicenter, qualitative study. Crit Care Med. 2007;35(9):2083–9. doi: 10.1097/01.ccm.0000281446.15342.74. [DOI] [PubMed] [Google Scholar]
- 16.Chisholm CD, Dornfeld AM, Nelson DR, Cordell WH. Work interrupted: a comparison of workplace interruptions in emergency departments and primary care offices. Ann Emerg Med. 2001;38(2):146–51. doi: 10.1067/mem.2001.115440. [DOI] [PubMed] [Google Scholar]
- 17.Laxmisan A, Hakimzada F, Sayan OR, Green RA, Zhang J, Patel VL. The multitasking clinician: decision-making and cognitive demand during and after team handoffs in emergency care. Int J Med Inform. 2007;76(11-12):801–11. doi: 10.1016/j.ijmedinf.2006.09.019. [DOI] [PubMed] [Google Scholar]
- 18.Chisholm CD, Collison EK, Nelson DR, Cordell WH. Emergency department workplace interruptions: are emergency physicians “interrupt-driven” and “multitasking”? Acad Emerg Med. 2000;7(11):1239–43. doi: 10.1111/j.1553-2712.2000.tb00469.x. [DOI] [PubMed] [Google Scholar]
- 19.Healey AN, Primus CP, Koutantji M. Quantifying distraction and interruption in urological surgery. Qual Saf Health Care. 2007;16(2):135–9. doi: 10.1136/qshc.2006.019711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sevdalis N, Healey AN, Vincent CA. Distracting communications in the operating theatre. J Eval Clin Pract. 2007;13(3):390–4. doi: 10.1111/j.1365-2753.2006.00712.x. [DOI] [PubMed] [Google Scholar]
- 21.Healey AN, Sevdalis N, Vincent CA. Measuring intra-operative interference from distraction and interruption observed in the operating theatre. Ergonomics. 2006;49(5-6):589–604. doi: 10.1080/00140130600568899. [DOI] [PubMed] [Google Scholar]
- 22.Grol H, Grimshaw J. From best evidence to best practice: effective implementation of changes in patients’ care. Lancet. 2003;362:1225–30. doi: 10.1016/S0140-6736(03)14546-1. [DOI] [PubMed] [Google Scholar]
- 23.Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PC, Rubin HR. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282(15):1458–65. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]