Abstract
Anesthesia has developed to the point where long term outcomes are important endpoints. Elderly patients are becoming an increasingly large part of most surgical practices, consistent with demographic shifts. Long term outcomes are particularly important for this group. In this review, we discuss functional outcomes in the elderly. We describe the areas of cognitive change and frailty, both of which are specific to the elderly. We also discuss prevention of surgical infections and emerging evidence around hemodynamic alterations in the operating room and their impact on long term outcomes.
Keywords: Geriatrics, Long term outcomes, Delirium, Postoperative Cognitive Dysfunction, Surgical Site Infection
The immediate risk of anesthesia used to be considered to be quite high. Intraoperative mortality was a significant issue that required substantial effort to address. Avoiding intraoperative catastrophe was the primary mission of the anesthesiologist. Fortunately, through the efforts of our national organizations dedicated to patient safety and quality improvement, the incidence of intraoperative mortality has decreased significantly.1
One could argue as to whether this is due to improved monitoring, better drugs, improved delivery devices or professional aptitude. Whatever the cause, immediate perioperative mortality is reported to have been reduced to 1 death per 10,000 over about 50 years. Beyond the obvious benefit to the patient, this state has provided an opportunity for anesthesiologists to examine outcomes over a longer period of time. While the Joint Commission for the Accreditation of Health Care Organizations continues to require documented follow-up of anesthetized patients up to 48 hours following a procedure, outcomes researchers have reached far beyond this time frame to search for perioperative outcomes months to years following a procedure. Elderly patients have higher risk of morbidity and mortality in the perioperative period and therefore are in the position to benefit the most from improvements in perioperative care.
Even healthy elderly patients continue to have a relatively higher incidence of mortality and morbidity.2 The reason for this phenomenon has not been elucidated and is the subject of significant scientific and social interest. In particular, long term outcomes represent an area of interest to the geriatric anesthesiologist. In the middle of the previous century, advanced age (over 55) was considered a contraindication to surgery and anesthesia.3 Today, operations are routinely performed on centenarians. In this report, we briefly review the physiology of aging that contributes to alterations in outcomes as well as the information available regarding these outcomes and how perioperative management may offer an opportunity to improve them.
AGING
Normal aging should be differentiated from disease processes that have a higher incidence in older patients.
Normal aging is those changes related directly to the aging process and not to a defined disease. For example, there is some arterial stiffening, particularly of the large vessels with resultant concentric ventricular hypertrophy in even well conditioned elderly patients with no cardiac disease. There are manyage related diseases such as the dementias and arthritis associated with poor mobility that are common, but should be distinguished from aging per se. When the burden of age-associated illness is low, this may lead to successful aging.4
These individuals are vibrant and active into late age, with limited impairment. However, muscle mass decreases even in the well conditioned, exercising elderly person. In order to distinguish aging from disease, researchers have had to carefully screen patients for disease processes. In doing so, many long held beliefs concerning aging have changed. One might therefore question how to define age in research context. In practice, defining age by any other than chronological age is difficult. Many studies of aging have included patients of age 60 or more commonly 65 and above. A recent trend has been to set the lower limit at 70 years of age and to make serious attempts to include patients in their late eighties and nineties in study designs. Cohorts of centenarians have also been studied fairly extensively.
Due to significant inter-individual variability, the assessment of each patient becomes critical. Despite its association with increased perioperative morbidity and mortality, chronological age is not a good gauge of aging physiology. All organs in a single body do not age synchronously. Described in the context of the ability to maintain homeostasis, homeostenosis represents the decreasing reserve capacity needed to achieve an increased level of function in response to stress.5 Conceptually, this limited ability to adequately compensate for the stress of surgery and anesthesia may be related to long term outcomes from surgery.
SURGICAL OUTCOMES PRIMARILY RELATED TO AGING
One of the major tasks that face researchers in the field of geriatrics is the determination of appropriate outcomes measures for elderly patients. There is a desire for some type of universal metric that would incorporate functional outcomes including quality of life and pathological outcomes (i.e. state of the disease). The concern is that typical pathology outcomes, e.g. troponin release defining a myocardial infarction or even post MI myocardial function ignores how the patient perceives their health. Return to normal function is the primary concern, so a significant pathology that does result in diminished function, for example a myocardial infarction with limited myocardial damage is less concerning than cognitive impairment (from either stroke or dementia) which would limit independence and may require admission to a skilled nursing facility. So, unlike younger patients, in whom recovery is to be expected, the spectrum of outcomes are varied and morbidity may be persistent. Functional outcomes measures are a vital aspect for understanding the impact of care in elderly.
A universal outcome (even a generally agreed upon such measure) does not exist as of yet. The recent interest in comparative effectiveness research has heightened an interest in this approach as researchers and policy makers try to decide how to judge what courses of treatment are effective in the elderly. There are general functional outcomes such as activities of daily living (ADLs) and independent activities of daily living (IADLs) for elderly patients. There are also a series of specific postsurgical pathology which are primarily problems of the elderly. For example, patients have been concerned about deterioration of cognitive function after surgery. There are two fairly well documented approaches to assessing cognitive change which we will discuss. Finally, there are many broader outcomes such as postoperative infection for which old age per se is not a major factor to which elderly patients may be more susceptible. In some of these areas, there is an indication that choices made in the perioperative period, e.g choice of anesthetic or care patterns, have an impact on long term outcomes.
Functional Outcomes
Traditional outcomes from surgery are defined within a period following a surgical procedure, frequently 30 days and tend to focus on morbidity and mortality. Hamel reported on 26,648 patients aged ≥80 (median age 82) and 568,263 patients < 80 (median age 62) from the Veterans Administrations National Surgical Quality Improvement Program (NSQIP) database.6
Thirty day mortality varied by procedure but were higher for patients >80. Despite this, for many common procedures, mortality is still relatively low (<2%). The incidence of complications increases with age, but probably more important is the impact of complications on mortality and functional recovery increases with age. Twenty precent of patients >80 years old had one or more complications and the presence of a complication increased mortality from 4% to 26%. Respiratory and urinary tract complications were the most common.
The primary concern of both elderly patients and the policy makers in charge of Medicare is disability. Symptoms and disability are the principal outcomes of most disease processes for the mid to late life patient. Verbrugge and Jett conceptualized disability in a way which helps to clarify concetpts that are important in this debate.7 Disability may begin with a disease or pathology. However, many people have no impairments of note from their disease. At a next level, impairments occur at the organ system level and are dysfunctional and structural abnormalities in specific body systems, such as cardiovascular or neurological. Anesthesiologists consider these are ASA Physical Status 2 patients. Functional limitations, actual restrictions in basic physical and mental abilities such as ambulation, reaching, bending, and communicating intelligibly consistute the next level (ASA PS3). Finally, disability itself evolves in a context and occurs when there is an insurmountable gap between an individual and environmental demands such that their expected social role is compromised. The World Health Organization makes the point that disability is a complex phenomenon reflecting an interaction between an individual’ a body and features of the society. (http://www.who.int/topics/disabilities/en/)
A desire to avoid disability and preserve or improve functional status represents the goal of therapy for a geriatric patient. Activities of daily living (ADL) and instrumental activities of daily living (IADL) are the most common measures of functional status.8 ADLs and IADLs are subjective reported measures evaluating basic activities and essential measures of independence, respectively. (See tables 1 and 2)
Table 1. Activities of Daily Living.
In each category, circle the item that most closely describes the person’s highest level of functioning and record the score assigned to that level (either 1 or 0) in the blank at the beginning of the category.
| A. Toilet | _____ | |
| 1. | Care for self at toilet completely; no incontinence | 1 |
| 2. | Needs to be reminded, or needs help in cleaning self, or has rare (weekly at most) accidents | 0 |
| 3. | Soiling or wetting while asleep more than once a week | 0 |
| 4. | Soiling or wetting while awake more than once a week | 0 |
| 5. | No control of bowels or bladder | 0 |
| B. Feeding | _____ | |
| 1. | Eats without assistance | 1 |
| 2. | Eats with minor assistance at meal times and/or with special preparation of food, or help in cleaning up after meals | 0 |
| 3. | Feeds self with moderate assistance and is untidy | 0 |
| 4. | Requires extensive assistance for all meals | 0 |
| 5. | Does not feed self at all and resists efforts of others to feed him or her | 0 |
| C. Dressing | _____ | |
| 1. | Dresses, undresses, and selects clothes from own wardrobe | 1 |
| 2. | Dresses and undresses self with minor assistance | 0 |
| 3. | Needs moderate assistance in dressing and selection of clothes | 0 |
| 4. | Needs major assistance in dressing but cooperates with efforts of others to help | 0 |
| 5. | Completely unable to dress self and resists efforts of others to help | 0 |
| D. Grooming (neatness, hair, nails, hands, face, clothing) | _____ | |
| 1. | Always neatly dressed and well-groomed without assistance | 1 |
| 2. | Grooms self adequately with occasional minor assistance, eg, with shaving | 0 |
| 3. | Needs moderate and regular assistance or supervision with grooming | 0 |
| 4. | Needs total grooming care but can remain well-groomed after help from others | 0 |
| 5. | Actively negates all efforts of others to maintain grooming | 0 |
| E. Physical Ambulation | _____ | |
| 1. | Goes about grounds or city | 1 |
| 2. | Ambulates within residence on or about one block distant | 0 |
| 3. | Ambulates with assistance of (check one) a ( ) another person, b ( ) railing, c ( ) cane, d ( ) walker, e ( ) wheelchair 1.__Gets in and out without help. 2.__Needs help getting in and out |
0 |
| 4. | Sits unsupported in chair or wheelchair but cannot propel self without help | 0 |
| 5. | Bedridden more than half the time | 0 |
| F. Bathing | _____ | |
| 1. | Bathes self (tub, shower, sponge bath) without help | 1 |
| 2. | Bathes self with help getting in and out of tub | 0 |
| 3. | Washes face and hands only but cannot bathe rest of body | 0 |
| 4. | Does not wash self but is cooperative with those who bathe him or her | 0 |
| 5. | Does not try to wash self and resists efforts to keep him or her clean | 0 |
Scoring Interpretation: For ADLs, the total score ranges from 0 to 6. In some categories, only the highest level of function receives a 1; in others, two or more levels have scores of 1 because each describes competence at some minimal level of function. These screens are useful for indicating specifically how a person is performing at the present time. When they are also used over time, they serve as documentation of a person’s functional improvement or deterioration.
Source: Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9:179–186. Copyright by the Gerontological Society of America.
Table 2. Instrument (Independent) Activities of Daily Living.
In each category, circle the item that most closely describes the person’s highest level of functioning and record the score assigned to that level (either 1 or 0) in the blank at the beginning of the category.
| A. Ability to Use Telephone | _____ |
| 1. Operates telephone on own initiative; looks up and dials numbers | 1 |
| 2. Dials a few well-known numbers | 1 |
| 3. Answers telephone but does not dial | 1 |
| 4. Does not use telephone at all | 0 |
| B. Shopping | _____ |
| 1. Takes care of all shopping needs independently | 1 |
| 2. Shops independently for small purchases | 0 |
| 3. Needs to be accompanied on any shopping trip | 0 |
| 4. Completely unable to shop | 0 |
| C. Food Preparation | _____ |
| 1. Plans, prepares, and serves adequate meals independently | 1 |
| 2. Prepares adequate meals if supplied with ingredients | 0 |
| 3. Heats and serves prepared meals or prepares meals but does not maintain adequate diet | 0 |
| 4. Needs to have meals prepared and served | 0 |
| D. Housekeeping | _____ |
| 1. Maintains house alone or with occasional assistance (eg, domestic help for heavywork) | 1 |
| 2. Performs light daily tasks such as dishwashing, bedmaking | 1 |
| 3. Performs light daily tasks but cannot maintain acceptable level of cleanliness | 1 |
| 4. Needs help with all home maintenance tasks | 1 |
| 5. Does not participate in any housekeeping tasks | 0 |
| E. Laundry | _____ |
| 1. Does personal laundry completely | 1 |
| 2. Launders small items; rinses socks, stockings, etc | 1 |
| 3. All laundry must be done by others | 0 |
| F. Mode of Transportation | _____ |
| 1. Travels independently on public transportation or drives own car | 1 |
| 2. Arranges own travel via taxi but does not otherwise use public transportation | 1 |
| 3. Travels on public transportation when assisted or accompanied by another | 1 |
| 4. Travel limited to taxi or automobile with assistance of another | 0 |
| 5. Does not travel at all | 0 |
| G. Responsibility for Own Medications | _____ |
| 1. Is responsible for taking medication in correct dosages at correct time | 1 |
| 2. Takes responsibility if medication is prepared in advance in separate dosages | 0 |
| 3. Is not capable of dispensing own medication | 0 |
| H. Ability to Handle Finances | _____ |
| 1. Manages financial matters independently (budgets, writes checks, pays rent and bills, goes to bank); collects and keeps track of income | 1 |
| 2. Manages day-to-day purchases but needs help with banking, major purchases, etc | 1 |
| 3. Incapable of handling money | 0 |
Scoring Interpretation: For IADLs, from 0 to 8. In some categories, only the highest level of function receives a 1; in others, two or more levels have scores of 1 because each describes competence at some minimal level of function. These screens are useful for indicating specifically how a person is performing at the present time. When they are also used over time, they serve as documentation of a person’s functional improvement or deterioration.
Source: Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9:179–186. Copyright by the Gerontological Society of America.
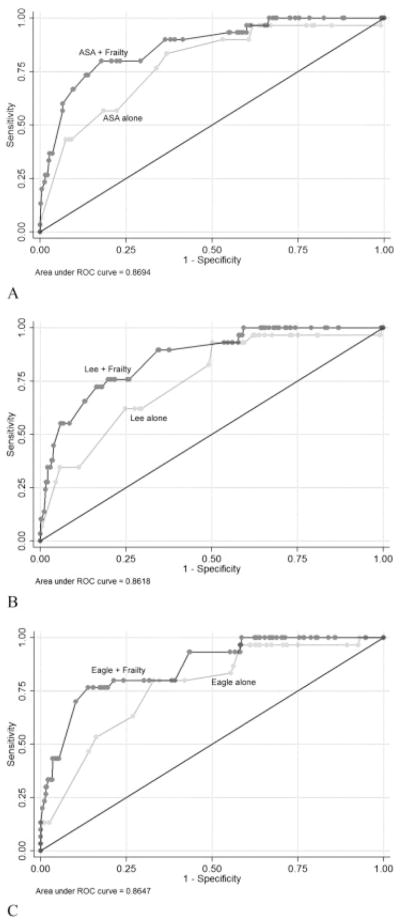
Lawrence et al. described the impact of surgery on functional outcomes in 372 elderly patients undergoing abdominal surgery.9 The participants were assessed preoperatively and postoperatively at 1, 3, and 6 weeks, 3 and 6 months, using self-report, including ADL and IADL, and performance-based measures including the timed walk, functional reach, and hand grip strength. The mean recovery times were: timed walk, 6 weeks; ADL and functional reach, 3 months; and IADL, 6 months. Remarkably, mean grip strength did not return to preoperative status by 6 months. (see Fig 1) Thus functional recovery for patients over 60 takes 3 to 6 months or longer.
Figure 1.
Rates of dependency in individual Activities of Daily Living (ADL) and Instrumental Activities of Daily Living (IADL) activities. (used with permission from : Journal of the American College of Surgeons, 2004; 199, : 762–772).
Frailty
Frail relates to being easily broken or destroyed, and frailty is the quality or state of being frail. Frailty, is primarily a geriatric syndrome which has received much attention in the past few years. Clinicians are familiar with the frail patient in a general sense, patients with decreased muscle mass who move slowly and seen to be, well, frail. However, a coherent universally accepted definition of frailty has not been developed. The first major attempt to define this sydrome was undertaken by Fried who focussed primarily on sarcopenia. Sarcopenia is the loss of muscle mass and is considered by many to be an inherent component of frailty models. This model included a cycle of frailty, in which sarcopenia created decreased activity which resulted in even more decrease in muscle mass. More recently in the perioperative arena, investigators have defined frailty by a combination of parameters. Although not standardized, these measures tend to include some functional component, such as a timed 15m walk and some historical factors, such as a history of weight loss or depedency in 1 or more ADL.
Frailty is an interesting concept when considering long term outcomes in the elderly. Recall the long duration for recovery of ADLs and IADLs described above. Many scales would suggest that many elderly patients become frail or more frail in the immediate postoperative period, but that they eventually regain the robustness.10 This suggests that frailty can be reversible and a potential target for improved outcomes. To date, this approach has not been studied.
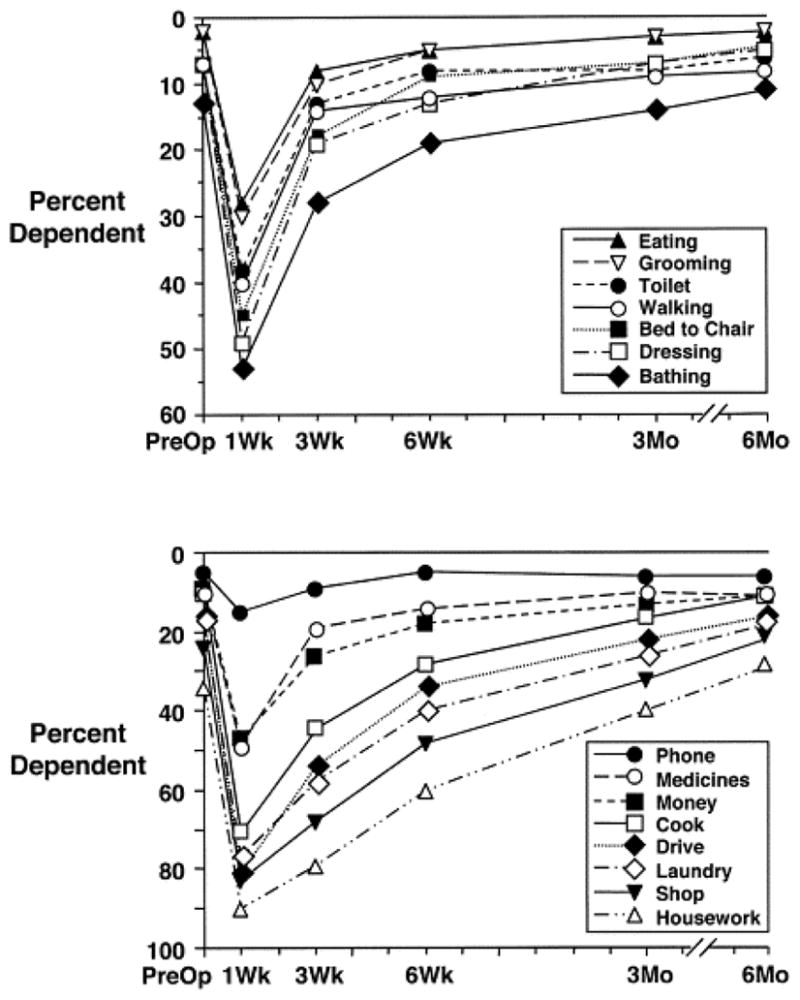
Frailty has been commonly perceived as a risk factor for poor outcomes in the elderly. Most recently, Robinson et al reported on a cohort of 223 elderly patients in which the investigators characterized a model of frailty consisting of 6 domains: burden of comorbidity, function, nutrition, cognition/mental, geriatric syndromes, and extrinsic frailty. They did not devise a single frailty number however many of the tests included in the frailty battery predicted institutionalization following surgery.11 MaKary et al defined a frailty score including weight loss, grip strength, exhaustion, physical activity and walking speed.12 Using this model, frailty was an independent predictor of discharge to a supported facility, the number of complications and length of stay. They were specifically able to show an advantage to adding their frailty index to either the ASA physical status or either the Lee or Eagle comorbidity scores. (see figure 2). In 1993, McEwen and Stellar, described allostatic load as consequences of chronic exposure to fluctuating or heightened stress.13 In essence, repeated stress on the body results in damage. This idea is related to the concept of homeostenosis described above. It is not clear frailty could be considered the phenotype of a high allostatic load.14 Frailty is an evolving area that will have a major impact on our conception of elderly assessment over the next few years.
Figure 2.
(A) American Society of Anesthesiologists (ASA), (B) Lee, and (C) Eagle risk indices. Each panel shows the area under the receiver operator characteristics (ROC) curve to demonstrate the ability of the specific risk index to predict surgical complications and discharge to an assisted or skilled nursing facility. Frailty was added to the risk index scoring to demonstrate the combined ability of these indices to predict discharge disposition. (used with permission from Journal of the American College of Surgeons, 2010; 210: 901–908)
Cognitive Outcomes
In the 1950’s, anesthesiologists began to document significant change in cognitive abilities of patients following surgery and anesthesia. A number of different pathologic states have been defined. These include inadequate emergence and emergence delirium, postoperative delirium (24–72 hours after surgery), and postoperative cognitive dysfunction (POCD), Delirium is a behavioral phenomenon which can be defined by observation and which is defined in the psychiatry literature. POCD is a research finding of deterioration in neurocognitive testing that requires a pre-operative and post operative test(s) to define.
There also appear to be some cases in which significant if not catastrophic cognitive deterioration occurs. These patients are not included in studies and if they were would probably drop out. We know of these cases through public forums such as the Alzheimer Disease Online Community (see for example: http://alzheimers.infopop.cc/eve/forums/a/tpc/f/214102241/m/3011075861/p/1) There are essentially no data on these cases, which are either anecdotes or medico-legal cases although there are some popular publications addressing this subject.15 Some retrospective reviews of patients in dementia surveillance programs have suggested that Alzheimer’s disease (AD) is more common after coronary artery bypass surgery versus percutaneous cardiac interventions16,17 while others do not support the idea that general surgery and anesthesia cause a change in the trajectory of dementia.18 However, the idea that anesthetic agents may be involved has been proposed based on laboratory observations that various anesthetics play a moderating role in the pathways leading to hyperphosphorylated Tau and neurofibrillatory tangles including caspase activation, apoptosis and the metabolism of beta-amyloid.19,,20 This is an extremely active area in which multiple different laboratory observations focus on the biochemical consequences of anesthetic exposure on AD pathogenic pathways.21 However, the link between these laboratory observations and clinical dementia has not been established, as has been described in the summary reports of recent conferences convened to discuss these issues. 22
Postoperative delirium (POD) has been identified by a large number of national surveys of the top research issues as an important issue that cuts across surgical specialties and has a significantly higher incidence in older patients. It has been associated, as noted below, with prolonged length of hospital stay and other long term consequences. The level of functional impact of POCD is less established. There are some data that cognitive change has an impact on functional outcomes such as ADLs and IADLs or the ability to work or collect support payments.23
Delirium is sudden severe confusion and is associated with rapid changes in brain function that may occur with physical or mental illness. Delirium involves an oscillation between mental states (for example, from lethargy to agitation and back to lethargy). Symptoms include alterations in: alertness, feeling (sensation) and perception, level of consciousness or awareness, movement (for example, may be slow moving or hyperactive), and sleep patterns, including drowsiness. There is also frequently confusion (disorientation) about time or place, a decrease in short-term memory and recall, disrupted or wandering attention, an inability to think or behave with purpose and problems concentrating, disorganized thinking, emotional or personality changes, and movements triggered by changes in the nervous system (psychomotor restlessness).
POCD is more difficult to define. Broadly it refers to deterioration in cognition temporally associated with surgery. The determination of POCD requires preoperative neuropsychological testing baseline and a determination that defines how much of a decline is called cognitive dysfunction. The domains that were most sensitive include: verbal learning and working memory, episodic memory, processing speed, and set shifting. The impact on verbal abilities, perception, attention, and abstract thinking is less clear. Valid pre and postoperative testing is essential to the diagnosis of POCD as self reporting of cognitive symptoms has been demonstrated to be inaccurate.24
Unfortunately, there has not been a standard methodology used in the multiple studies within the POCD literature.25 Investigators have used different tests, different timing and different standards for the amount of deterioration that is used to definte POCD. Although there was an attempt at a consensus conference in 1996,26 these suggestions were significantly different than those that were already in use by the International Study of Postoperative Cognitive Dysfunction (ISPOCD).27 Both this group and associated investigators were actively using the ISPOCD defintions at the time and the consensus group did not include any of these investigators. Other investigators have subsequently used a variety of different definitions. Thus, a consensus has failed to emerge. Therefore, it is difficult to define the presence and therefore incidence of POCD or to clearly understand the relationship between POCD and other dementing illnesses.
The incidence of POD for non-cardiac general surgery ranges between studies 5–15%.28 Certain groups such as hip fracture patients the range is 16–62% with an average of 35%.6 The true incidence of POCD may be masked by attrition of the worst cases. No study has accounted for the aforementioned attrition. POCD may resolve with time. Currently it seems the incidence of initial deterioration in older patients is high (25% at 2–10 days) with gradual resolution (10% at 3 months, 5% at 6 months, 1% at 1 year).29
At 1 year, the cognitive decline is indistinguishable from matched controls.
The etiologies of delirium and POCD remain unknown. There is some evidence to suggest that highly organized perioperative care can decrease the incidence of delirium. There is early evidence that the amount of sedation given in the operating room can influence the incidence of delirium.30 In this study, patients who had suffered a hip fracture and were to undergo repair under subarachnoid anesthesia were randomized to one of two sedation regimens. Sedation depth was titrated using the bispectral index (BIS), and patients were randomized to receive either deep (BIS, approximately 50) or light (BIS, >or=80) sedation. The prevalence of postoperative delirium was significantly lower in the light sedation group (11/57 [19%] vs 23/57 [40%] in the deep sedation group; P=.02). The author calculated that 1 incident of delirium will be prevented for every 4.7 patients treated with light sedation. A larger study is currently evaluating this approach, but it does provide the first direct evidence of the ability to significantly impact the incidence of delirium with intraoperative alternatives.
GENERAL LONG TERM OUTCOMES
Surgical Site Infections
There are a number of other areas in which anesthesiologists have developed an interest in interventions that are associated with an impact at some distance from the anesthetic itself. Surgical site infections (SSIs) lead to adverse patient outcomes, including prolonged hospitalization and death. SSIs are common, occurring in 2% to 5% of patients undergoing surgery in the United States. 31 The Society for Healthcare Epidemiology of America/Infectious Disease Society of America Compendium of Strategies to Prevent HAI in Acute Care Hospitals summarized methods used to prevent SSI.32 Anesthesiologists are involved in this area at three essential points, the administration of antibiotics, the use of supplemental oxygen and the maintanence of normothermia.
Antimicrobial prophylaxis
Perioperative antimicrobial prophylaxis is a proven intervention that reduces the risk of SSI in elective procedures.33, 34 The goal of prophylaxis is to reduce the concentration of potential pathogens at or in close proximity to the surgical incision. The two major components of an appropriate perioperative antimicrobial prophylaxis program are giving the agent at the appropriate time and using the appropriate agent at the appropriate dose. In one retrospective study of approximately 3000 patients, the lowest rates of SSI occurred in the group of patients who received antimicrobial prophylaxis within 1 hour before incision. 34
The Surgical Quality Improvement Project (and the Center for Medicare and Medicaid Services (CMS)) process measures state that starting infusion of antimicrobial prophylaxis within 1 hour before incision maximizes benefit (2 hours before incision for vancomycin and fluoroquinolones).35 If prophylaxis is started as soon as 1 minute before incision, the OR team is still in compliance from a regulatory perspective. Although this practice may follow the strict definition of the criteria, it certainly does not follow our understanding of the science and therefore the spirit of the criteria. For most agents, antimicrobial prophylaxis is most effective if infusion is started between 30 and 60 minutes before surgery. Antimicrobial prophylaxis given 0 to 29 minutes before surgery was less effective than comparable therapy administered between 30 to 59 minutes before surgery in one prospective observational study of 3836 surgical patients. 36
Supplemental Oxygen
Anesthesiologists are primarily responsible for the oxygen concentration used in the operating room and the amount of supplementation used following surgery. To date, there are six randomized controlled trials that have evaluated the utility of high inspired oxygen fraction in the perioperative period.37,38–42 A reduction in the rate of SSI after administration of 80% FiO2 during and after surgery was demonstrated in four studies. 37,38,39,41 One study reported no difference.40 One report concluded that administration of 80% FiO2 led to higher rates of SSI.42 A recent meta-analysis that included 5 of the earlier-mentioned trials (including the negative study) concluded that high inspired oxygen decreased the risk of SSI. They also noted significant methodological differences between the studies43 On balance, supplemental oxygen seems to reduce the risk for SSI in certain surgeries such as colorectal and abdominal surgeries with a limited risk profile.
Normothermia
A case has been made for the importance of normothermia (usually requiring active warming) during and following an operation as a means of avoiding infection. Kurz demonstrated a significant decrease in both SSI (19% vs 6%) and length of stay for patients who have been kept normothermic.44 This and other reports have led to a recommendation in the Surgical Quality Improvement Project to maintain normothermia for colorecral surgery. There has been some recent concern regarding the utility of this standard.45 There are other reasons apart from SSI to achieve normothermia, including a decrease in transfusion requirements.46
Triple Low: Mean Arterial Pressure, Minimun Alveolar Concentration, Bispectral Index
Perhaps the most intriguing of areas in which long term outcomes are the focus of intense research was put into play by the Outcomes Research Group headed by Dr. D. Sessler at the Cleveland Clinic. They have identified a combination state, referred to as a triple low, which is an excellent predictor of 30 and 90day mortality, at least in preliminary evaluations. There are currently at least two major studies of this concept underway. The triple low condition consisting of Bispectral Index (BIS) <45, mean arterial pressure (MAP) <75 mmHg, and end-tidal volatile anesthetic concentrations in minimum alveolar concentration (MAC) equivalents <0.7. This ominous combination may identify patients who are especially sensitive to anesthesia and, possibly, at risk of brain hypoperfusion. Preliminary results indicate that 90-day mortality is similar at ≈2.0% in patients who never experience a Triple Low and in those given vasopressors in ≤5 min, but significantly greater at 2.97% in those given vasopressors later or not at all. Although this information has not been age adjusted to date, the interest to gerontologists is clear. The blood pressure limit of 75 mmHg is usually considered a well tolerated blood pressure, so this paradigm raises the bar of what is called hypotension in the perioperative period.47 Just having a blood pressure below this cutoff is not the primary concern, but rather finding this condition in the presence of either a low MAC and/or a low BIS reading. A low MAC would indicate that the low pressure is ocurring in a patient with relatively low level of general anesthetic agent, i.e. a patient who is very sensitive to anesthetics. This is most commonly either a patient who is very ill or an elderly patient. The low BIS score would indicate that the patient’s brain is deeply anesthetized. In the presence of a low MAC, this would have to be explained by increased sensitivity, again either due to concurrent illness or age. Low BIS for a prolonged period of time has been associated with increased mortality in and of itself, although no prospective studies have confirmed this result. In the triple low concept, the combination of all three creates a state that, if not corrected rapidly, is associated with a marked increase in short term mortality. An interesting aspect of this finding is that it suggests an approach to correcting it. By paying attention to this combination of signs and reacting rapidly, alterations in mortality appear to be prevented. This is an area that will generate much work in the next few years. It is particularly interesting as anesthesiologists have been relatively sanguine about mean blood pressures down to about 60 mmHg. Triple low may identify patients who are frail and vulnerable to complications in the perioperative period. However, one of the major problems with this study was that MAC was not adjusted for age.
INTERVENTIONS TO IMPROVE GERIATRIC OUTCOMES
For many years, investigators have evaluated the role of geriatric focussed care most commonly under the moniker of comperhensive geriatric assessment (CGA). In his Joseph Freeman lecture, Rubenstein outlined the history and general efficacy of this approach as well as the limitations imposed by the current systems of reimbursement for medical care.48 (Rubenstein) Many of these programs have been directed as orthopedic services and have shown promising results.49 Marcantonio et al has shown that a similar approach decreases the incidence of delirium in patients with hip fractures.50 (See Table 3)One case of delirium was prevented for every 5.6 patients in the geriatrics consultation group. The Hospital Elder Life Program (HELP) is a form of this approach specifically directed at the prevention of delirium which has been successfully employed in both academic medical centers and community hospitals.51 These programs do not offer anything unusual or innovative, rather they apply standard geriatric principles to the care of perioperative patients. It would seem that these approaches would benefit most elderly patients.
Table 3. Module with Recommendations from Marcantonio’s Active Geriatric Consultation.
|
Modified from E. R. Marcantonio, J. M. Flacker, R. J. Wright, and N. M. Resnick. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr.Soc. 49 (5):516–522, 2001.
CONCLUSION
Perioperative care of the elderly is still a developing field. While the number of patients is significant, the amount of specifically perioperative research remains limited. The practitioner must extrapolate from a variety of reports to develop a coherent anesthetic and perioperative plan. Long term outcomes are particularly important and an evolving area of anesthetic practice, but there is increasing evidence that the care provided in and around the operating room will have impacts significantly beyond the immediate perioperative period.
Acknowledgments
Grant support: Dr. Deiner is supported by Grant 1 R03 AG040624-01 from the National Institutes on Aging and additional support from the American Geriatrics Society and the Foundation for Anesthesia Education and Research. Dr. Silverstein is supported by Grant 1 R01 AG029656-01A1 from the National Institutes on Aging.
References
- 1.Braz LG, Braz DG, Cruz DS, Fernandes LA, Modolo NS, Braz JR. Mortality in anesthesia: a systematic review. Clinics (Sao Paulo) 2009;64:999–1006. doi: 10.1590/S1807-59322009001000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bentrem DJ, Cohen ME, Hynes DM, Ko CY, Bilimoria KY. Identification of specific quality improvement opportunities for the elderly undergoing gastrointestinal surgery. Arch Surg. 2009;144:1013–20. doi: 10.1001/archsurg.2009.114. [DOI] [PubMed] [Google Scholar]
- 3.Ochsner A. Is risk of operation too great in the elderly? Geriatrics. 1927;22:121. [PubMed] [Google Scholar]
- 4.Rowe JW, Kahn RL. Successful aging. Gerontologist. 1997;37:433–40. doi: 10.1093/geront/37.4.433. [DOI] [PubMed] [Google Scholar]
- 5.Silverstein JH, Rooke GA. Hazzard’s Geriatric Medicine and Gerontology. 6. New York: McGraw Hill; 2009. Anesthesia; p. 417. [Google Scholar]
- 6.Hamel MB, Henderson WG, Khuri SF, Daley J. Surgical outcomes for patients aged 80 and older: morbidity and mortality from major noncardiac surgery. J Am Geriatr Soc. 2005;53:424–9. doi: 10.1111/j.1532-5415.2005.53159.x. [DOI] [PubMed] [Google Scholar]
- 7.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 8.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–86. [PubMed] [Google Scholar]
- 9.Lawrence VA, Hazuda HP, Cornell JE, et al. Functional independence after major abdominal surgery in the elderly. J Am Coll Surg. 2004;199:762–72. doi: 10.1016/j.jamcollsurg.2004.05.280. [DOI] [PubMed] [Google Scholar]
- 10.Sarkisian CA, Gruenewald TL, John Boscardin W, Seeman TE. Preliminary evidence for subdimensions of geriatric frailty: the MacArthur study of successful aging. J Am Geriatr Soc. 2008;56:2292–7. doi: 10.1111/j.1532-5415.2008.02041.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Robinson TN, Wallace JI, Wu DS, et al. Accumulated Frailty Characteristics Predict Postoperative Discharge Institutionalization in the Geriatric Patient. J Am Coll Surg. 2011 doi: 10.1016/j.jamcollsurg.2011.01.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Makary MA, Segev DL, Pronovost PJ, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010;210:901–8. doi: 10.1016/j.jamcollsurg.2010.01.028. [DOI] [PubMed] [Google Scholar]
- 13.McEwen BS, Seeman T. Protective and damaging effects of mediators of stress. Elaborating and testing the concepts of allostasis and allostatic load. Ann N Y Acad Sci. 1999;896:30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- 14.Gruenewald TL, Seeman TE, Karlamangla AS, Sarkisian CA. Allostatic load and frailty in older adults. J Am Geriatr Soc. 2009;57:1525–31. doi: 10.1111/j.1532-5415.2009.02389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McMurtry L. Walter Benjamin at the Dairy Queen. New York: Siimon & Shuster; 1999. [Google Scholar]
- 16.Bohnen NI, Warner MA, Kokmen E, Beard CM, Kurland LT. Alzheimer’s disease and cumulative exposure to anesthesia: a case-control study. J Am Geriatr Soc. 1994;42:198–201. doi: 10.1111/j.1532-5415.1994.tb04952.x. [DOI] [PubMed] [Google Scholar]
- 17.Lee TA, Wolozin B, Weiss KB, Bednar MM. Assessment of the emergence of Alzheimer’s disease following coronary artery bypass graft surgery or percutaneous transluminal coronary angioplasty. J Alzheimers Dis. 2005;7:319–24. doi: 10.3233/jad-2005-7408. [DOI] [PubMed] [Google Scholar]
- 18.Avidan MS, Searleman AC, Storandt M, et al. Long-term cognitive decline in older subjects was not attributable to noncardiac surgery or major illness. Anesthesiology. 2009;111:964–70. doi: 10.1097/ALN.0b013e3181bc9719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bittner EA, Yue Y, Xie Z. Brief review: anesthetic neurotoxicity in the elderly, cognitive dysfunction and Alzheimer’s disease. Can J Anaesth. 2011;58:216–23. doi: 10.1007/s12630-010-9418-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhen Y, Dong Y, Wu X, et al. Nitrous oxide plus isoflurane induces apoptosis and increases beta-amyloid protein levels. Anesthesiology. 2009;111:741–52. doi: 10.1097/ALN.0b013e3181b27fd4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Papon MA, Whittington RA, El-Khoury NB, Planel E. Alzheimer’s disease and anesthesia. Front Neurosci. 2011;4:272. doi: 10.3389/fnins.2010.00272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baranov D, Bickler PE, Crosby GJ, et al. Consensus statement: First International Workshop on Anesthetics and Alzheimer’s disease. Anesth Analg. 2009;108:1627–30. doi: 10.1213/ane.0b013e318199dc72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Steinmetz J, Christensen KB, Lund T, Lohse N, Rasmussen LS ISPOCD Group. Long-term consequences of postoperative cognitive dysfunction. Anesthesiology. 2009;110:548–55. doi: 10.1097/ALN.0b013e318195b569. [DOI] [PubMed] [Google Scholar]
- 24.Jorm AF, Christensen H, Korten AE, Henderson AS, Jacomb PA, Mackinnon A. Do cognitive complaints either predict future cognitive decline or reflect past cognitive decline? A longitudinal study of an elderly community sample. Psychol Med. 1997;27:91–8. doi: 10.1017/s0033291796003923. [DOI] [PubMed] [Google Scholar]
- 25.Newman S, Stygall J, Hirani S, Shaefi S, Maze M. Postoperative cognitive dysfunction after noncardiac surgery: a systematic review. Anesthesiology. 2007;106:572–90. doi: 10.1097/00000542-200703000-00023. [DOI] [PubMed] [Google Scholar]
- 26.Mahanna EP, Blumenthal JA, White WD, et al. Defining neuropsychological dysfunction after coronary artery bypass grafting. Ann Thorac Surg. 1996;61:1342–7. doi: 10.1016/0003-4975(95)01095-5. [DOI] [PubMed] [Google Scholar]
- 27.Rasmussen LS, Larsen K, Houx P, et al. The assessment of postoperative cognitive function. Acta Anaesthesiol Scand. 2001;45:275–89. doi: 10.1034/j.1399-6576.2001.045003275.x. [DOI] [PubMed] [Google Scholar]
- 28.Deiner S, Silverstein JH. Postoperative delirium and cognitive dysfunction. Br J Anaesth. 2009;103 (Suppl 1):i41–46. doi: 10.1093/bja/aep291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abildstrom H, Rasmussen LS, Rentowl P, et al. Cognitive dysfunction 1–2 years after non-cardiac surgery in the elderly. ISPOCD group. International Study of Post-Operative Cognitive Dysfunction. Acta Anaesthesiol Scand. 2000;44:1246–51. doi: 10.1034/j.1399-6576.2000.441010.x. [DOI] [PubMed] [Google Scholar]
- 30.Sieber FE, Gottshalk A, Zakriya KJ, Mears SC, Lee H. General anesthesia occurs frequently in elderly patients during propofol-based sedation and spinal anesthesia. J Clin Anesth. 2010;22:179–83. doi: 10.1016/j.jclinane.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 31.Graves EJ. National hospital discharge survey: annual summary 1987. 1989. [PubMed] [Google Scholar]
- 32.Anderson DJ, Kaye KS, Classen D, et al. Strategies to prevent surgical site infections in acute care hospitals. Infect Control Hosp Epidemiol. 2008;29 (Suppl 1):S51–61. doi: 10.1086/591064. [DOI] [PubMed] [Google Scholar]
- 33.Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999;20(250):78. doi: 10.1086/501620. quiz 279–80. [DOI] [PubMed] [Google Scholar]
- 34.Classen DC, Evans RS, Pestotnik SL, Horn SD, Menlove RL, Burke JP. The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. N Engl J Med. 1992;326:281–6. doi: 10.1056/NEJM199201303260501. [DOI] [PubMed] [Google Scholar]
- 35.Bratzler DW, Hunt DR. The surgical infection prevention and surgical care improvement projects: national initiatives to improve outcomes for patients having surgery. Clin Infect Dis. 2006;43:322–30. doi: 10.1086/505220. [DOI] [PubMed] [Google Scholar]
- 36.Weber WP, Marti WR, Zwahlen M, et al. The timing of surgical antimicrobial prophylaxis. Ann Surg. 2008;247:918–26. doi: 10.1097/SLA.0b013e31816c3fec. [DOI] [PubMed] [Google Scholar]
- 37.Belda FJ, Aguilera L, Garcia de la Asuncion J, et al. Supplemental perioperative oxygen and the risk of surgical wound infection: a randomized controlled trial. JAMA. 2005;294:2035–42. doi: 10.1001/jama.294.16.2035. [DOI] [PubMed] [Google Scholar]
- 38.Greif R, Akca O, Horn EP, Kurz A, Sessler DI Outcomes Research Group. Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. N Engl J Med. 2000;342:161–7. doi: 10.1056/NEJM200001203420303. [DOI] [PubMed] [Google Scholar]
- 39.Mayzler O, Weksler N, Domchik S, Klein M, Mizrahi S, Gurman GM. Does supplemental perioperative oxygen administration reduce the incidence of wound infection in elective colorectal surgery? Minerva Anestesiol. 2005;71:21–5. [PubMed] [Google Scholar]
- 40.Meyhoff CS, Wetterslev J, Jorgensen LN, et al. Effect of high perioperative oxygen fraction on surgical site infection and pulmonary complications after abdominal surgery: the PROXI randomized clinical trial. JAMA. 2009;302:1543–50. doi: 10.1001/jama.2009.1452. [DOI] [PubMed] [Google Scholar]
- 41.Myles PS, Leslie K, Chan MT, et al. Avoidance of nitrous oxide for patients undergoing major surgery: a randomized controlled trial. Anesthesiology. 2007;107:221–31. doi: 10.1097/01.anes.0000270723.30772.da. [DOI] [PubMed] [Google Scholar]
- 42.Pryor KO, Fahey TJ, 3rd, Lien CA, Goldstein PA. Surgical site infection and the routine use of perioperative hyperoxia in a general surgical population: a randomized controlled trial. JAMA. 2004;291:79–87. doi: 10.1001/jama.291.1.79. [DOI] [PubMed] [Google Scholar]
- 43.Qadan M, Akca O, Mahid SS, Hornung CA, Polk HC., Jr Perioperative supplemental oxygen therapy and surgical site infection: a meta-analysis of randomized controlled trials. Arch Surg. 2009;144(359):66. doi: 10.1001/archsurg.2009.1. discussion 366–7. [DOI] [PubMed] [Google Scholar]
- 44.Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996;334:1209–15. doi: 10.1056/NEJM199605093341901. [DOI] [PubMed] [Google Scholar]
- 45.Lehtinen SJ, Onicescu G, Kuhn KM, Cole DJ, Esnaola NF. Normothermia to prevent surgical site infections after gastrointestinal surgery: holy grail or false idol? Ann Surg. 2010;252:696–704. doi: 10.1097/SLA.0b013e3181f6c2a9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rajagopalan S, Mascha E, Na J, Sessler DI. The effects of mild perioperative hypothermia on blood loss and transfusion requirement. Anesthesiology. 2008;108:71–7. doi: 10.1097/01.anes.0000296719.73450.52. [DOI] [PubMed] [Google Scholar]
- 47.Stapelfeldt WH, Greenwald SD, Manberg PJ, Chamoun N, Sessler DI. Modeling the Impact of Alert Thresholds of ‘Triple Low’ Conditions on 90-Day Postoperative Mortality. Anesthesiology. 2010:A922. [Google Scholar]
- 48.Rubenstein LZ, Joseph T. Freeman award lecture: comprehensive geriatric assessment: from miracle to reality. J Gerontol A Biol Sci Med Sci. 2004;59:473–7. doi: 10.1093/gerona/59.5.m473. [DOI] [PubMed] [Google Scholar]
- 49.Harari D, Hopper A, Dhesi J, Babic-Illman G, Lockwood L, Martin F. Proactive care of older people undergoing surgery (‘POPS’): designing, embedding, evaluating and funding a comprehensive geriatric assessment service for older elective surgical patients. Age Ageing. 2007;36:190–6. doi: 10.1093/ageing/afl163. [DOI] [PubMed] [Google Scholar]
- 50.Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001;49:516–22. doi: 10.1046/j.1532-5415.2001.49108.x. [DOI] [PubMed] [Google Scholar]
- 51.Rubin FH, Neal K, Fenlon K, Hassan S, Inouye SK. Sustainability and scalability of the hospital elder life program at a community hospital. J Am Geriatr Soc. 2011;59:359–65. doi: 10.1111/j.1532-5415.2010.03243.x. [DOI] [PMC free article] [PubMed] [Google Scholar]