Abstract
BACKGOUND
The HEALTHY primary prevention trial developed an integrated multi-component intervention program to moderate risk factors for type 2 diabetes in middle schools. The nutrition component aimed to improve the quality of foods and beverages served to students. Changes in the School Breakfast Program (SBP), National School Lunch Program (NSLP), and a la carte venues are compared to the experience of control schools.
METHODS
The intervention was implemented in 21 middle schools from winter 2007 through spring 2009 (following a cohort of students from sixth through eighth grades); 21 schools acted as observed controls. The nutrition component targeted school food service environmental change. Data identifying foods and nutrients served (selected by students for consumption) were collected over a 20-day period at baseline and end of study. Analysis compared end of study values for intervention versus control schools.
RESULTS
Intervention schools more successfully limited dessert and snack food portion size in NSLP and a la carte and lowered fat content of foods served. Servings of high fiber grain-based foods and/or legumes were improved in SBP but not NSLP. Intervention and control schools eliminated >1% fat milk and sugar added beverages in SBP, but intervention schools were more successful in NSLP and a la carte.
CONCLUSION
The HEALTHY program demonstrated significant changes in the nutritional quality of foods and beverages served in the SBP, NSLP, and a la carte venues, as part of an effort to decrease childhood obesity and support beneficial effects in some secondary HEALTHY study outcomes.
Keywords: School Food Services, Nutrition and Diet, Child and Adolescent Health
Access to foods and beverages in schools influences dietary behaviors associated with the increasing early prevalence of chronic health conditions in youth, including overweight, obesity, and type 2 diabetes.1 Health professionals and policymakers have recommended population-based approaches to reduce risk of obesity and diabetes by improving children’s diets, including changing access to foods and beverages in schools.2
Children consume approximately 35% to 47% of their daily dietary intake in school food environments.3 The United States Department of Agriculture (USDA) provides the nutritional standards and requirements for the federally subsidized National School Lunch Program (NSLP) and the School Breakfast Program (SBP), based on the 1995 School Meals Initiative for Healthy Children and the Dietary Guidelines for Americans 2005.4 However, no federal guidelines are provided for foods labeled as “competitive” which are offered in a la carte, vending, school stores, and other venues. Many state and local school governing bodies provide nutritional guidelines, but final selection of items is also influenced by financial, community, industrial, and political pressures.
The most recent School Nutrition Dietary Assessment Study (SNDA-III), reflecting data from the second half of the 2004–2005 school year, reported that the majority of schools surveyed provided meals that met required standards, but that meals selected or purchased by students did not meet those same standards.5 Most school meals failed to meet standards for fat content, and a la carte venues were a common source of “competitive” foods.5 A systematic review of published and unpublished school-based interventions in the US and Europe concluded that the impact on regulating food and beverage availability in schools was limited by a focus on single foods, such as sweetened beverages or snack chips, rather than considering all foods and beverages available.6
Changes to the foods and beverages available in schools were implemented within the HEALTHY study, a 3-year, randomized, multi-center, school-based primary prevention trial designed to moderate risk factors, including adiposity, for type 2 diabetes.7 The nutrition component of the HEALTHY intervention program, one of four integrated intervention components, established a set of clearly defined goals to improve the foods and beverages available in the total school food environment (TSFE). We hypothesized that improvements in foods and beverages offered in the TSFE would improve those selected and served to students in intervention schools participating in the HEALTHY study. Although others have reported changes in the availability of foods and beverages offered in the TSFE, to our knowledge none have reported what was selected or served to students.8,9 Here we report the specific research objective of the nutrition intervention component to achieve goals to serve foods and beverages of higher nutrient quality and appropriate quantities. The nutrition intervention component goals, listed in Table 1, targeted all areas of the TSFE, including the federal meal programs, a la carte venues such as snack bars and school stores, vending machines, fundraisers, and classroom parties and celebrations.10 This paper reports the impact of the intervention on foods and beverages served in the three most prevalent school food service venues (NSLP, SBP, and a la carte) in intervention compared to control schools. Data reported refer to items served, by which we mean selected by students from among items available; data confirming consumption were not collected.
Table 1.
End of study percent nutrition goal attainment in control (C) and intervention (I) schools
| HEALTHY Nutrition Goal | School Breakfast Program | National School Lunch Program | A La Cartea | |||
|---|---|---|---|---|---|---|
| C | I | C | I | C | I | |
| Lower the average fat content of food served in schools. | 67% | 95% | 57% | 71% | 71% | 88% |
| Serve at least 2 servings of fruit and/or vegetables per student on NSLP and at least 1 serving per student on SBP each day.b | 5% | 5% | 9% | 19% | n/a | n/a |
| Serve all dessert and snack foods with ≤200 kcal per single size serving and/or package. | n/a | n/a | 14% | 43% | 41% | 88% |
| Eliminate milk >1% fat, all other added sugar beverages, and 100% fruit juice (100% fruit juice may only be served as ≤6 ounces as part of SBP). | 86% | 86% | 57% | 90% | 6% | 94% |
| Serve at least 2 servings of high fiber (≥2 grams of fiber per serving) grain-based foods and/or legumes per student on NSLP and at least 1 serving per student on SBP each day.c | 5% | 14% | 0% | 0% | n/a | n/a |
A la carte service includes food and beverage items that are sold in addition to federally approved meals. Data represent 34 of the 42 schools with a la carte service at both baseline and end of study.
Serving = ½ cup canned or cut fruit or ½ cup cooked vegetable or 1 cup raw vegetables or 1 piece of fresh fruit.
Serving = 1 slice of bread or equivalent or ½ cup cooked cereal, rice, noodle, pasta, legumes, or grains or ¾ cup dry cereal.
METHODS
The HEALTHY Study
The HEALTHY study was conducted in 10 school districts located at 7 sites (see listing in Appendix) across the country. Each site recruited 6 middle schools serving largely minority and lower income populations that were randomized to control (N=21) or intervention (N= 21). A cohort of 4603 students was followed from sixth through eighth grades, beginning in fall 2006 and ending in spring 2009. The HEALTHY intervention program consisted of four integrated components: (1) nutrition,10 (2) physical activity,11 (3) behavioral knowledge and skills,12 and (4) communications and social marketing.13 Changes to the TSFE and physical education classes were enhanced by educational outreach, behavior change activities, and promotional messaging. Students provided parental informed consent and minor child assent to participate in data collection.
The HEALTHY trial tested whether the percent of students with BMI ≥85th percentile (cutoff for overweight or obese) was lower in intervention versus control schools. At end of study, both intervention and control schools had dropped by 4–5% from baseline.14 Because the four HEALTHY intervention program components were effectively integrated and inter-linked, it is not possible to address the impact of each separate component on the outcome.
The HEALTHY Nutrition Intervention Component Procedures
The 5 goals from the nutrition intervention component are listed in Table 1. A research dietitian at each site provided training and guidance to each intervention school’s food service manager and staff and coordinated achievement of study goals at the school district and individual school levels. For each goal, multiple strategies were developed. For example, strategies related to the goal to lower the average fat content of foods were to replace the highest fat entrees with lower fat options, or to offer only reduced fat and/or baked items. More details about strategies and intervention school activities have been reported.10 The nutrition intervention component also included educational events held during lunchtime in and around the cafeteria, and conducted ‘taste tests’ of new products (eg, wheat crusted chicken nuggets), unfamiliar foods (eg, kiwi fruit), or comparison of available items (eg, bottled versus tap water). The study gave each intervention school food service department $3000 per year to defray expenses and potential lost income.
Control schools followed existing school district standards and guidelines. All 42 HEALTHY study schools participated in the USDA federal school meals program. However, only 34 schools (17 intervention and 17 control) offered an a la carte program at both baseline and end of study. A la carte data include snack bars and school stores (present in 6 schools). These a la carte venues were located adjacent to NSLP service areas and provided access to competitive food alternatives during meal service.
Instruments and Data Collection
Data were collected at baseline and end of study by trained study staff not involved in implementing the intervention. Data collection started on a day with a typical volume and delivery of food services (eg, not related to holiday celebrations or breaks when food inventories were usually limited) and continued for the next 19 days that met these criteria. Nutrition data collection consisted of gathering data on all foods and beverages (names, descriptions, amounts, and nutrient content) throughout the TSFE. Nutrition data were extracted from food service management source documents maintained by school food service personnel, including work production sheets, food/beverage product specification sheets and/or labels, recipes, and menus. Numbers of standardized, typical food service servings of foods and beverages served (“taken off the line,” selected by or sold) to students in each venue were recorded.
Data Analysis
Nutrient analysis of the foods and beverages was performed using the Nutrition Data System for Research (NDSR) version 2009 (Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN). NDSR applies a database of foods and beverages to output a complete breakdown of nutrients and food components for the item entered. Data from the USDA Nutrient Data Laboratory are the primary source of information used by NDSR, supplemented with marketplace data and with site-specific food and beverage nutrient information. Trained nutrition professionals not involved in the intervention entered each food and beverage item, including serving size, food group code, and quantity. The nutrition professionals either found an identical match in the NDSR nutrient database or made a match with the closest item that was within 25 kilocalories (kcal), 2 grams of fat, and 0.5 grams of fiber of the original entry. If an identical or close match could not be identified, the food/beverage was added as a new item/recipe in the NDSR database.
For purposes of tracking and evaluating implementation of the goals of the nutrition intervention component, items were either assigned a code or grouped to indicate the food/beverage category type. For example, foods offered at NSLP were coded as entrees if they were made from school entree recipes, were listed as entrees on the school menu, provided significant protein and carbohydrate, and contained approximately 400 kcal. Items offered at SBP were considered high fat foods if they contained >30% kcal from fat, excluding beverages and fat-based spreads. Items were considered high fiber foods if they were grain-based foods or legumes providing ≥2 g of dietary fiber per serving. Other food/beverage groupings were made such as fruit, vegetable, 100% juice, or sugar-added beverages. A la carte, snack bar, and school store items were grouped in more specific categories, such as cookies, pizzas, and ice cream.
The NDSR nutrient values for each food and beverage item (expressed as kcal, ounces, grams, servings, etc.) were multiplied by quantity served to give a weighted amount. Weighted amounts were combined across codes (e.g., entrees, grain-based foods/legumes, fruit, vegetable) served within a single day for each school, and means per school per day were computed. To express values per student, we divided by the number of children participating in the meal program each day. For SBP and NSLP, student participation in the meal program was readily available from the work production sheets. For a la carte computations, the number of students participating was estimated as the total school enrollment minus the number of children participating in NSLP. Summary statistics (mean, standard deviation) were produced by averaging across number of days of data collection and across schools. In addition, the proportion of all a la carte food and beverage items served within each specific coded category was computed.
Mixed models were used to compare the end of the study values for intervention versus control schools, with the covariance structure adjusting for variability both between schools and between days within the same school. Probability values less than .05 were considered statistically significant. There was no adjustment for multiple comparisons. Statistical analyses were performed using SAS (version 9.2, 2008, Research Triangle Institute, Research Triangle Park, NC).
RESULTS
Table 1 shows end of study nutrition intervention goal achievement for intervention versus control schools across SBP, NSLP, and a la carte venues. (At baseline, the percent of schools meeting the nutrition intervention goals was similar in both control and intervention schools; data not shown). More intervention than control schools met all of the nutrition intervention goals within the NSLP except for the fiber and fruit and vegetable goals. For a la carte, more intervention than control schools met all applicable nutrition intervention goals. Intervention schools were more successful at attaining the goal to lower fat content of items served at SBP. High percents of both intervention and control schools served no more than six ounces of 100% fruit juice and mainly low fat milk at SBP.
Table 2 shows that intervention and control schools were equivalent at baseline in participation in SBP and NSLP and distribution across payment type. There was little change during the study. Reflecting school eligibility criteria, most students received free meals. More students participated in NSLP than in SBP.
Table 2.
Participation in the federal school meals programs in control and intervention schools at baseline and end of study.
| Baseline | End of Study | |||
|---|---|---|---|---|
| Control | Intervention | Control | Intervention | |
| National School Breakfast Program | ||||
|
| ||||
| Mean number of students/day/school | 240 | 240 | 221 | 229 |
|
| ||||
| Participation by payment typea | ||||
| Free | 84% | 89% | 81% | 83% |
| Reduced Price | 7% | 6% | 10% | 9% |
| Full Price | 9% | 5% | 9% | 8% |
|
| ||||
| National School Lunch Program | ||||
|
| ||||
| Mean n students/day/school | 587 | 643 | 564 | 611 |
|
| ||||
| Participation by payment typea | ||||
| Free | 75% | 82% | 73% | 78% |
| Reduced Price | 9% | 7% | 11% | 11% |
| Full Price | 17% | 10% | 16% | 11% |
Free: children from families with incomes below 130% of the poverty level are eligible for free meals;
Reduced Price: children from families with incomes between 130–185% of the poverty level are eligible for reduced meal cost not to exceed $0.40/meal.
SBP data are presented in Table 3 as average food group servings and nutrient amounts served per day per school. At end of study, in those items coded as high fat foods, intervention schools served significantly less energy (kcal/d) and total grams of fat. Intervention schools also served significantly more grams of fiber from grain-based foods and/or legumes than control schools. There was no difference in servings per student of high fiber (≥2 g of fiber per serving) grain-based foods and/or legumes, in servings per student of fruits with or without 100% fruit juice, or in ounces per student of any beverages related to the intervention goals.
Table 3.
Food group servings and nutrient amounts (mean ± SD served per day per school) in the School Breakfast Program at baseline and end of study in control versus intervention schools
| Baseline | End of Study | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Control | Intervention | Control (C) | Intervention (I) | p-value | |||||
| Mean n items served | Mean ± SD | Mean n items served | Mean ± SD | Mean n items served | Mean ± SD | Mean n items served | Mean ± SD | (C vs I) | |
| High Fat Foods a | |||||||||
| Energy (kcal/d) | 213 | 177 ± 37 | 223 | 181 ± 34 | 189 | 176 ± 58 | 134 | 124 ± 63 | 0.0060 |
| Total fat (g) | 213 | 9.3 ± 2.4 | 223 | 9.7 ± 2.0 | 189 | 8.8 ± 3.0 | 134 | 6.2 ± 3.2 | 0.0061 |
|
| |||||||||
| Grain-Based Foods and Legumesb | |||||||||
| Fiber (g) | 291 | 1.3 ± 0.4 | 296 | 1.4 ± 0.4 | 272 | 1.7 ± 0.5 | 290 | 2.2 ± 0.5 | 0.0042 |
| Fiber ≥ 2 g (servings/student) | 18 | 0.1 ± 0.2 | 27 | 0.1 ± 0.2 | 55 | 0.4 ± 0.4 | 91 | 0.6 ± 0.4 | 0.5195 |
|
| |||||||||
| Fruitsc (servings/student) | |||||||||
| Including 100% juice | 225 | 0.9 ± 0.3 | 201 | 0.9 ± 0.3 | 239 | 1.0 ± 0.4 | 228 | 1.0 ± 0.4 | 0.9725 |
| Excluding 100% juice | 42 | 0.1 ± 0.2 | 36 | 0.1 ± 0.2 | 58 | 0.2 ± 0.3 | 60 | 0.3 ± 0.3 | 0.2815 |
|
| |||||||||
| Beverages (oz/student) | |||||||||
| Nonfat or 1% fat milk | 154 | 5.4 ± 2.5 | 157 | 5.6 ± 2.5 | 128 | 5.1 ± 2.6 | 143 | 5.5 ± 2.2 | 0.4223 |
| > 1% milk | 17 | 1.3 ± 2.4 | 20 | 0.8 ± 1.4 | 7 | 0.8 ± 2.1 | 0 | 0.0 ± 0.0 | n/a |
| 100% fruit juice | 184 | 1.5 ± 0.8 | 165 | 3.1 ± 1.1 | 181 | 3.7 ± 0.7 | 168 | 3.1 ± 1.0 | 0.5814 |
Serving of food with >30% kcal from fat, excluding fat-based spreads and beverages.
Fiber within all grain-based foods and legumes and grain based recipes that may include insignificant percentages of fruit or vegetable as an ingredient. Serving = 1 slice of bread or equivalent or ½ cup cooked cereal, rice, noodle, pasta, legumes, or grains or ¾ cup dry cereal.
Serving = ½ cup canned/cut fruit or 1 piece of fresh fruit or 4 ounces 100% juice (when included).
In NSLP at end of study (Table 4), intervention compared to control schools served significantly less energy, less total fat, and less total percent energy from fat in entrée foods. Intervention schools had more grams of fiber in grain-based foods and/or legumes and served fewer ounces of 100% fruit juice per student (intervention schools almost completely eliminated this item). Intervention and control schools did not differ significantly in servings per student of high fiber grain-based foods and/or legumes (≥2 grams of fiber per serving), fruits with and without 100% fruit juice, vegetables whether fried or not, or in ounces per student of nonfat or 1% fat milk. Milk with >1% fat was completely eliminated in the intervention schools at NSLP.
Table 4.
Food group servings and nutrient amounts (mean ± SD served per day per school) in the National School Lunch Program at baseline and end of study in control versus intervention schools
| Baseline | End of Study | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Control | Intervention | Control (C) | Intervention (I) | p-value | |||||
| Mean n items served | Mean ± SD | Mean n items served | Mean ± SD | Mean n items served | Mean ± SD | Mean n items served | Mean ± SD | (C vs I) | |
| Entrees a | |||||||||
| Energy (kcal) | 622 | 346 ± 45 | 668 | 340 ± 46 | 595 | 343 ± 46 | 656 | 305 ± 60 | 0.0234 |
| Total fat (g) | 622 | 15.4 ± 1.6 | 668 | 15.3 ± 1.7 | 595 | 14.9 ± 2.0 | 656 | 12.2 ± 3.4 | 0.0017 |
| Fat (% of energy) | 622 | 40.1 ± 3.2 | 668 | 40.7 ± 3.3 | 595 | 39.2 ± 3.7 | 656 | 34.7 ± 4.1 | 0.0002 |
|
| |||||||||
| Grain-Based Foods and Legumesb | |||||||||
| Fiber (g) | 762 | 2.0 ± 0.6 | 824 | 2.1 ± 0.6 | 773 | 2.2 ± 0.6 | 783 | 3.0 ± 0.8 | 0.0003 |
| Fiber ≥ 2 g (servings/student) | 29 | 0.1 ± 0.1 | 41 | 0.2 ± 0.1 | 52 | 0.1 ± 0.1 | 88 | 0.2 ± 0.2 | 0.3799 |
|
| |||||||||
| Fruitsc (servings/student) | |||||||||
| Including 100% juice | 395 | 0.6 ± 0.3 | 411 | 0.6 ± 0.3 | 440 | 0.7 ± 0.3 | 436 | 0.7 ± 0.2 | 0.2427 |
| Excluding 100% juice | 296 | 0.5 ± 0.2 | 297 | 0.5 ± 0.2 | 356 | 0.6 ± 0.2 | 419 | 0.7 ± 0.2 | 0.6926 |
|
| |||||||||
| Vegetablesd (servings/student) | |||||||||
| Non fried | 584 | 0.7 ± 0.4 | 627 | 0.7 ± 0.3 | 640 | 0.8 ± 0.3 | 631 | 0.8 ± 0.3 | 0.5599 |
| Fried | 173 | 0.4 ± 0.3 | 169 | 0.4 ± 0.2 | 94 | 0.2 ± 0.2 | 40 | 0.1 ± 0.1 | 0.7326 |
|
| |||||||||
| Beverages (oz/student) | |||||||||
| Nonfat or 1% fat milk | 486 | 7.3 ± 1.4 | 487 | 6.6 ± 1.7 | 479 | 7.2 ± 1.7 | 557 | 8.0 ± 0.8 | 0.8191 |
| > 1% milk | 11 | 0.2 ± 0.4 | 14 | 0.2 ± 0.4 | 10 | 0.3 ± 1.1 | 0 | 0.0 ± 0.0 | n/a |
| 100% fruit juice | 100 | 0.7 ± 1.5 | 117 | 0.7 ± 1.5 | 84 | 0.7 ± 1.4 | 1 | 0.0 ± 0.0 | <.0001 |
Entrees include items representing school entree recipes or entrees listed on the school menu that provide significant protein and carbohydrate and ~400 kcal/serving.
Fiber within all grain-based foods and legumes and grain based recipes that may include insignificant percentages of fruit or vegetable as an ingredient. Serving = 1 slice of bread or equivalent or ½ cup cooked cereal, rice, noodle, pasta, legumes, or grains or ¾ cup dry cereal.
Serving = ½ cup canned/cut fruit or 1 piece of fresh fruit or 4 ounces 100% juice (when included).
Serving = ½ cooked vegetables or 1 cup raw vegetables.
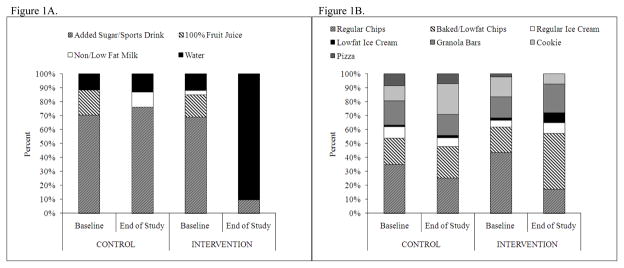
As shown in Figure 1A, at baseline for both intervention and control schools, more than 50% of the beverages served a la carte were sports drinks and other added sugar beverages. By the end of the study, intervention schools had replaced sport drinks, 100% fruit juice, and a proportion of added sugar beverages with bottled water. Although control schools also eliminated 100% fruit juice, added non/low fat milk, and continued to serve bottled water, more than 50% of the beverages served were sport drinks and beverages with added sugar. Figure 1B shows the distribution of five categories of the most popular food items served a la carte: chips, granola bars, cookies, ice cream, and pizza. Control schools made some progress in serving more baked or low fat chips, but intervention school changes were more dramatic, with half of the ice cream served low fat and baked or low fat chips making meaningful inroads into regular chip sales.
Figure 1.
Proportion (%) of types of beverages (1A) and snacks/desserts (1B) served A la Carte at baseline and end of study in Intervention and Control Schools.
* Footnote: Not all categories of A la Carte snacks/desserts are shown. A few other types of items were served (including donuts, nuts, yogurts, etc.) but were not well represented across all schools or were served in very limited quantities.
DISCUSSION
The HEALTHY study nutrition intervention component implemented changes designed to reduce fat content and dessert/snack food serving size, eliminate higher fat milk and added sugar beverages, and increase fruits, vegetables, and high fiber grain-based foods and legumes in the TSFE.10 Changes were not just in one component of the HEALTHY intervention program that also incorporated physical education class activities and management, educational and promotional events and messages, and behavior change and goal setting opportunities. Given the integrated nature of the intervention program, we are not able to single out how changes in the TSFE due to the nutrition component affected student risk factors for type 2 diabetes. However, these changes in foods served that were accomplished by the nutrition intervention may have contributed to the beneficial effects seen as a result of the overall HEALTHY Study intervention; these beneficial changes included greater reductions in the intervention schools in the secondary outcomes of BMI z score, percentages of students with waist circumference at or above the 90th percentile, fasting insulin levels and the prevalence of students with BMI ≥ 95 percentile.14 We report on the significance of changes made in the TSFE on foods and beverages selected by students in intervention versus control schools for the SBP, NSLP, and a la carte venue.
The reduction in high fat foods, dessert/snack food portion size, added sugar beverages, and higher fat milk was successful for NSLP in intervention schools compared to control schools at end of study. Although students in intervention schools were served more grain-based foods and legumes compared to students in control schools, schools were unable to consistently meet fiber goals each day at NSLP. NHANES and SDNA-III data indicate children and adolescents do not consume the amount of whole grains, grain-based foods, and legumes recommended for the prevention of type 2 diabetes.15–17 Research dietitians in the HEALTHY study met with food industry representatives to request greater availability of appealing high fiber products. Taste tests introduced high fiber grain-based foods, and food service personnel were instructed in the preparation of high fiber foods. The higher cost of fiber-rich foods compared to other foods available from USDA influenced school food service personnel to purchase fiber-rich foods in limited quantities.
Food sources of fiber offered at intervention schools at SBP were also limited. One challenge was the competition from more popular, less nutrient rich cereal products and other pre-packaged frozen breakfast foods approved for USDA reimbursement. By law, schools access entitlement foods that are provided to states by USDA for a price, based on the total number of meals served. These specific entitlement foods are determined by USDA, made available to schools at their request, and can be more cost effective than some of the market-based foods that may be more nutrient rich.18 Schools can also request “bonus” foods as they become available from surplus agricultural stock.18 The availability and price of foods coupled with unanticipated menu changes in school meals made it difficult to consistently meet the fiber goal.
Attempts to lower the fat content of foods and entrees in intervention schools were successful in SBP, NSLP, and a la carte venues. Several school-based interventions in middle schools have reported similar outcomes in changing nutrition policies and modifying school menus to offer foods and beverages lower in fat and energy.8.9 Other studies have analyzed school menus, conducted plate waste analysis, or assessed self-reported dietary intake of students at school to examine changes in the fat content of foods offered.19 Our findings suggest that lower fat foods are acceptable to children in the school environment and may impact energy intake over time.
Servings of fruits and vegetables selected by students were similar in intervention and control schools at end of study in NSLP and SBP. Study research dietitians developed school recipes to use fresh, frozen, and canned fruits or vegetables and created appealing fruit and vegetable displays. Data from 2003–2004 NHANES indicate that adolescents report consuming more fruit juice than whole fruit on a daily basis.20 In the HEALTHY study in SBP only, 100% fruit juice was limited to six ounces or less and was not available at NSLP in any of the intervention schools. Barriers to increasing the number of fruits and vegetables served included food service decisions controlled at the district rather than school level, the cost and availability of fruit and vegetables at a given time, and lack of student familiarity with a variety of fruit and vegetables.21–23
At end of study in intervention and control schools, milk with greater than 1% fat was removed at both SBP and NSLP. Cooperation of the beverage vendors and the development of school district Nutrition Wellness Policies by governing bodies supported the changes.24
Changes in a la carte items offered in intervention schools included removal of pizza and replacement of high fat, sugary cookies with portion control lower fat, lower sugar products. The additional shift from fried snack chips and regular ice cream to baked snack chips and low fat ice cream further improved student choices in this venue. A la carte and school stores are the primary source of “competitive” foods, but the HEALTHY nutrition intervention component showed that strategies to remove and replace can be successful.
Challenges and Limitations
Our experience reflects the nature of the TSFE infrastructure. Due to the annual food bidding process, many items, particularly entrees, were selected a year in advance and, as a result, more costly items reformulated to be lower in fat or higher in fiber and/or those new to the marketplace were difficult to obtain. Avoiding waste was a high priority and the amounts and types of foods acquired and prepared needed to closely match student purchasing projections; this was particularly true of more perishable items such as milk, fruits, and vegetables. Many schools used profits from the sale of a la carte items to finance school activities and therefore resisted offering more nutritious items that might be less popular or changing the price of items to affect purchasing patterns.
A limitation to implementing changes uniformly was the variability in management, organization, and governance across school districts and individual schools. Additionally, availability of foods and beverages differed from school to school based on proximity to markets and capacity of storage and food preparation facilities.
Conclusions
The intention of the HEALTHY nutrition intervention component was that environmental changes in foods and beverages served would in part lead to changes in choices and behaviors that would reduce overall energy consumption in dietary intake and improve health.25 The fact that significant changes were made to the TSFE but did not translate to overall improvement in overweight and obesity status is a reminder of the multifaceted issues associated with the problem of childhood obesity. For this reason the HEALTHY intervention was developed as a multi-faceted program uniting changes in the school nutrition environment with changes in the physical education environment, education, behavior change, promotion, and marketing. Despite this effort, both intervention and control schools achieved similar decreases in the percent of students in the overweight or obese category.
IMPLICATIONS FOR SCHOOL HEALTH
Institutional, federal, and state regulations exert control over what foods, beverages, and dietary patterns are available in school meal programs, but ultimately students decide what to select and consume.26 Lessons learned in the HEALTHY study can add to the body of knowledge that guides school food service and nutrition policies and can be integrated into the design, structure, and promotion of school meals programs. Reductions in high fat foods, dessert/snack food portion size, added sugar beverages, and higher fat milk is acceptable among middle school students. Necessary emphasis on fruits, vegetables, and dietary fiber rich foods present challenges demanding strategic approaches to encourage students’ school meals choices. School superintendents, principals and teachers can advocate for school food service environmental changes linked to nutrition curriculum that promote healthy dietary choices associated with decreased risk for type 2 diabetes. Solutions to stem childhood obesity requires continuing study and researchers can build upon lesson learned in this study to enhance future initiatives. Passage of the Healthy Hungry Free-Kids Act in December, 2010 by the US Congress will provide opportunity for continuing improvement in future school nutrition programs.27 This Act supports reform in US school meals programs by upgrading nutritional standards and increasing access to quality food choices.
Human Subjects Approval Statement
This study was approved by Institutional Review Boards at each of the participating sites in the HEALTHY Study.
Acknowledgments
Source of Grant Support
This work was completed with funding from NIDDK/NIH grant numbers U01-DK61230, U01-DK61249, U01-DK61231, and U01-DK61223 to the STOPP-T2D collaborative group.
The following individuals and institutions constitute the HEALTHY Study Group (* indicates principal investigator or director): STOPP-T2D Study Chair Childrens Hospital Los Angeles: F.R. Kaufman Field Centers Baylor College of Medicine: T. Baranowski*, L. Adams, J. Baranowski, A. Canada, K.T. Carter, K.W. Cullen, M.H. Dobbins, R. Jago, A. Oceguera, A.X. Rodriguez, C. Speich, L.T. Tatum, D. Thompson, M.A. White, C.G. Williams Oregon Health & Science University: L. Goldberg*, D. Cusimano, L. DeBar, D. Elliot, H.M. Grund, S. McCormick, E. Moe, J.B. Roullet, D. Stadler Temple University: G. Foster* (Steering Committee Chair), J. Brown, B. Creighton, M. Faith, E.G. Ford, H. Glick, S. Kumanyika, J. Nachmani, L. Rosen, S. Sherman, S. Solomon, A. Virus, S. Volpe, S. Willi University of California at Irvine: D. Cooper*, S. Bassin, S. Bruecker, D. Ford, P. Galassetti, S. Greenfield, J. Hartstein, M. Krause, N. Opgrand, Y. Rodriguez, M. Schneider University of North Carolina at Chapel Hill: J. Harrell*, A. Anderson, T. Blackshear, J. Buse, J. Caveness, A. Gerstel, C. Giles, A. Hackney, A. Jessup, P. Kennel, R. McMurray, D. Rubin, A-M. Siega-Riz, M. Smith, A. Steckler, A. Zeveloff University of Pittsburgh: M.D. Marcus*, M. Carter, S. Clayton, B. Gillis, K. Hindes, J. Jakicic, R. Meehan, R. Noll, J. Vanucci, E. Venditti University of Texas Health Science Center at San Antonio: R. Treviño*, A. Garcia, D. Hale, A. Hernandez, I. Hernandez, C. Mobley, T. Murray, J. Stavinoha, K. Surapiboonchai, Z. Yin Coordinating Center George Washington University: K. Hirst*, K. Drews, S. Edelstein, L. El ghormli, S. Firrell, M. Huang, P. Kolinjivadi, S. Mazzuto, T. Pham, A. Wheeler Project Office National Institute of Diabetes and Digestive and Kidney Diseases: B. Linder*, C. Hunter, M. Staten Central Blood Laboratory University of Washington Northwest Lipid Metabolism and Diabetes Research Laboratories: S.M. Marcovina* HEALTHY intervention materials are available for download at http://www.healthystudy.org/
We wish to recognize Dr. Anna Maria Siega-Riz, R.D. and Ms. Amy Virus, R.D. as authors on this paper.. We thank the administration, faculty, staff, students, and their families at the middle schools and school districts; particularly the school food service administration and staff that participated in the HEALTHY study.
Footnotes
Disclaimer: The authors have indicated they have no financial relationships relevant to this article, nor conflicts of interest to disclose
Contributor Information
Connie C. Mobley, Email: connie.mobley@unlv.edu, Associate Dean of Research and Professor of Nutrition, University of Nevada Las Vegas, 1001 Shadow Lane MS 7425, Las Vegas, NV 89106, Phone: 702-774-2643, FAX: 7027742647.
Diane D. Stadler, Email: stadlerd@ohsu.edu, Assistant Professor, Division of Health Promotion & Sports Medicine, Director of Graduate Programs in Human Nutrition, Oregon Health & Science University, 3181 SW Sam Jackson Park Rd, CR110, Portland, Oregon 97239, Phone: 503-494-0168, FAX: 503-494-1310.
Myrlene A Staten, Email: statenm@niddk.nih.gov, Senior Advisor, Diabetes Translational Research, National Institutes of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, 6707 Democracy Blvd, Rm 6107, Bethesda, MD 20892, Phone: 301-402-7886, FAX: 301-480-3503.
Laure El ghormli, Email: Elghorml@biostat.bsc.gwu.edu, Senior Research Associate, Biostatistics Center, George Washington University, 6110 Executive Blvd, Suite 750, Rockville, MD 20852, Phone: 301-231-6804, Fax: 301-881-3767.
Bonnie Gillis, Email: gillisbp@upmc.edu, Senior Manager, Scientific Content Development, Health Promotion Department, University of Pittsburgh Medical Center Health Plan, Two Chatham Center, 112 Washington Place, Pittsburgh, PA 15219, Phone: 412-454-5658, FAX: 412-454-2942.
Jill Hartstein, Email: hartstej@uci.edu, Nutritionist, University of California, Irvine, 620 University Tower, 4199 Campus Drive, Irvine, CA 92697, Phone: 949-285-4626, Fax: 949-824-8849.
Anna Maria Siega-Riz, Email: am_siegariz@unc.edu, Professor of Epidemiology and Nutrition, Associate Chair of Epidemiology, 2105-A McGavran Greenberg Bld, Gillings School of Global Public Health, The University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, Phone: 919-962-8410.
Amy Virus, Email: amyvir@temple.edu, Center for Obesity Research & Education, Temple University, 3223 North Broad Street, Suite 175, Philadelphia PA 19140, Phone: 215-707-8669, FAX: 215-707-6475.
References
- 1.Van Cleave J, Gortmaker SL, Perrin M. Dynamics of obesity and chronic health conditions among children and youth. JAMA. 2010;303(7):623–630. doi: 10.1001/jama.2010.104. [DOI] [PubMed] [Google Scholar]
- 2.Finkelstein DM, Hill EL, Whitaker RC. School food environments and policies in US public schools. Pediatrics. 2010;122(1):e251–e259. doi: 10.1542/peds.2007-2814. [DOI] [PubMed] [Google Scholar]
- 3.Briefell RR, Crepinsek MK, Cabili C, et al. School food environments and practices affect dietary behaviors of US public school children. J Am Diet Assoc. 2009;109(suppl 2):S91–S107. doi: 10.1016/j.jada.2008.10.059. [DOI] [PubMed] [Google Scholar]
- 4.Crepinsek MK, Gordon AM, MCKinney PM, et al. Meals offered and served in US public schools: do they meet nutrient standards? J Am Diet Assoc. 2009;109:S31–S43. doi: 10.1016/j.jada.2008.10.061. [DOI] [PubMed] [Google Scholar]
- 5.Gordon AR, Crepinsek MK, Nogales R, et al. Report No. CN-07-SNDA-III. US Department of Agriculture, Food; 2007. [Accessed April 28, 2010]. School Nutrition Dietary Assessment Study-III: Volume I: School Food Service, School Food Environment, and Meals Offered and Served. [Online]. Available at: http://www.fns.usda.gov/oane/MENU/Published/CNP/FILES/SNDAIII-Vol1.pdf. [Google Scholar]
- 6.Jamie PC, Lock K. Do school based food and nutrition policies improve diet and reduce obesity? Prev Med. 2009;48:45–53. doi: 10.1016/j.ypmed.2008.10.018. [DOI] [PubMed] [Google Scholar]
- 7.The HEALTHY Study Group. HEALTHY study rationale, design and methods: moderating risk of type 2 diabetes in multi-ethnic middle school students. Int J Obes. 2009;33(suppl 4):S4–S20. doi: 10.1038/ijo.2009.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Osganian SK, Ebzery MK, Montgomery DH, et al. Changes in the nutrient content of school lunches: results from the CATCH eat smart food service intervention. Prev Med. 1996;25(4):400–412. doi: 10.1006/pmed.1996.0072. [DOI] [PubMed] [Google Scholar]
- 9.Sallis JF, McKenzie TL, Conway TL, et al. Environmental interventions for eating and physical activity. A randomized controlled trial in middle schools. Am J Prev Ed. 2003;24(3):209–217. doi: 10.1016/s0749-3797(02)00646-3. [DOI] [PubMed] [Google Scholar]
- 10.Gillis B, Mobley C, Stadler DD, et al. Rationale, design and methods of the HEALTHY study nutrition intervention component. Int J of Obes. 2009;33:S29–S36. doi: 10.1038/ijo.2009.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McMurray RG, Bassin S, Jago R, et al. Rational, design and methods of the HEALTHY study physical education intervention component. Int J of Obes. 2009;33:S37–S43. doi: 10.1038/ijo.2009.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Venditti EM, Elliot DL, Faith MS, et al. Rational, design and methods of the HEALTHY study behavior intervention component. Int J of Obes. 2009;33:S44–S51. doi: 10.1038/ijo.2009.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DeBar LL, Schneider M, Ford EG, et al. Social marketing-based communications to integrate and support the HEALTHY study intervention. Int J of Obes. 2009;33:S52–S59. doi: 10.1038/ijo.2009.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The HEALTHY Study Group. A school-based Intervention for diabetes risk reduction: the HEALTHY study. N Engl J Med. 2010;363:443–453. doi: 10.1056/NEJMoa1001933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Venn B, Mann J. Cereal, grains, legumes and diabetes. Eur J Clin Nutr. 2004;58:1443–1461. doi: 10.1038/sj.ejcn.1601995. [DOI] [PubMed] [Google Scholar]
- 16.Slavin JL. Position of the American Dietetic Association: health implications of dietary fiber. J Am Diet Assoc. 2008;108(10):1716–1731. doi: 10.1016/j.jada.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 17.Institute of Medicine. Proposed Approach for Recommending Revisions. Washington, DC: The National Academies Press; 2008. Nutrition Standards and Meal Requirements for National School Lunch and Breakfast Programs: Phase I. [PubMed] [Google Scholar]
- 18.National School Lunch Program Fact Sheet. US Department of Agriculture Food and Nutrition; Aug, 2009. [Accessed May 2, 2010]. Website [Online] Available at: http://www.fns.usda.gov/cnd/lunch/aboutlunch/NSLPFactSheet.pdf. [Google Scholar]
- 19.Story M, Snyder MP, Anliker J, et al. Changes in the nutrient content of school lunches: results from the Pathways study. Prev Med. 2003;37:S35–S45. doi: 10.1016/j.ypmed.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 20.Kimmons J, Gillespie C, Seymour J, Serdula M, Blanck HM. Fruit and vegetable intake among adolescents and adults in the United States: percentage meeting individualized recommendations. [Accessed April 15, 2010];Medscape J Med. 2009 11(1):26. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2654704/?tool=pubmed. [PMC free article] [PubMed]
- 21.Hoffman JA, Franko DL, Thompson DR, Power TJ, Stallings VA. Longitudinal behavioral effects of a school-based fruit and vegetable promotion program. J Pediatr Psychol. 2010;35(1):61–71. doi: 10.1093/jpepsy/jsp041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lytle LA, Kubic MY, Perry C, et al. Influencing healthful food choices in schools and home environments: results from the TEENS study. Prev Med. 2006;43(1):8–13. doi: 10.1016/j.ypmed.2006.03.020. [DOI] [PubMed] [Google Scholar]
- 23.Dezwaltowski DA, Estabrooks PA, Welk G, et al. Healthy youth places: a randomized controlled trial to determine the effectiveness of facilitating adult and youth leaders to promote physical activity and fruit and vegetable consumption in middle schools. Health Educ Behav. 2009;36:583–600. doi: 10.1177/1090198108314619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Health Policy Tracking Service. Balance: A Report on State Action to Promote Nutrition, Increase Physical Activity, and Prevent Obesity. Robert Wood Johnson Foundation; 2006. [Accessed January, 2008]. Web site [Online] Available at: http://www.rwjf.org/files/research/Balance122006.pdf. [Google Scholar]
- 25.Krebs-Smith SM, Reedy J, Bosire C. Healthfulness of the food supply. Am J Prev Med. 2010;38(5):472–477. doi: 10.1016/j.amepre.2010.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Briefel RR, Crepinsek MK, Cabili C, et al. School food environments and practices affect dietary behaviors of US public school children. J Am Diet Assoc. 2009;109:S91–S107. doi: 10.1016/j.jada.2008.10.059. [DOI] [PubMed] [Google Scholar]
- 27.USDA Office of Communication. [Accessed December 15, 2010];Release No. 0632.10. Agriculture Secretary Vilsack Statement on Passage of the Healthy Hunger-Free Kids Act. Available at: http://www.usda.gov/wps/portal/usda.