Abstract
Introduction:
Uganda has limited health resources. It is important to measure the need for imaging in order to set policy and plan for imaging services.
Objectives:
The first specific objective was to develop and apply four imaging needs indices on a case study basis, in five selected Ugandan hospitals. The indices were: Imaging Load (IL), Imaging Burden (IB), Type Specific Imaging Burden (TSIB), and Disease Specific Imaging Burden (DSIB). The second objective was to explore the perceptions of the patient, referring clinician, and radiologist regarding the values, meaning, and objective of imaging in patient care.
Materials and Methods:
This was a cross-sectional survey employing triangulation methodology, conducted in 5 Ugandan hospitals over a period of 3 years during 2005 - 2008. The subjects were divided into four clusters: Obstetrics and gynecology (obs/gynae), surgery, internal medicine, and pediatrics. For the quantitative component of the study, data from case notes was used to calculate the indices. The qualitative component explored the non-measurable aspects of imaging needs from the clinician's, radiologist's, and patient's perspective.
Results:
A total of 1961 patient case notes were studied. The IB was 460 per 1000 hospital patients per year. The highest TSIB was for ultrasound at 232 per 1000 hospital patients per year, followed by 191 patients for general X-ray. The majority of the patients interviewed had special desires, expectations, and misconceptions.
Conclusions:
There is a high IB of 460 per thousand patient populations per year, mainly due to ultrasound. The majority of the patients have perceptions, misconceptions, beliefs, and values which influence the need for imaging. There is a need to address the medical and non-tangible imaging needs of the patient and to counteract imaging-related misconceptions and over-expectations. Public awareness of the value, capabilities, limitations, and adverse effects of various imaging modalities need to be addressed to ensure that the patients make informed imaging choices and readily avail themselves of interventions in situations when imaging is crucial, for example in suspected high-risk pregnancy.
Keywords: Assessing, Imaging-Needs, Uganda
INTRODUCTION

Background
Uganda with a population of 28 million has 102 public hospitals ranging from tertiary to general hospitals.[1,2]
The National Health Equipment Policy and imaging services
The 2005/2006-2009/2010 Health Sector Strategic Plan [3] sets targets to procure equipment for all health levels with sophistication based on the hierarchical level.[4] The planning and acquisition of equipment is based on a non-evidence-based utilization levels of 20% and 5% for inpatients and outpatients, respectively.
Definition of indices and their calculation
Imaging load (IL)
This is a projected total yearly number of patients in a given hospital who will benefit from imaging. It was projected using the total recorded hospital throughput for the year and the proportion of patients for that particular hospital who would benefit from imaging. The proportion of patients who would benefit from imaging was obtained by sampling for three months. This may have introduced a bias, since it assumed no seasonal variations, but it was the only cost-effective method.
Imaging burden
The imaging burden (IB) is a rate index, indicating the number per thousand hospital patients per year, for whom imaging would be beneficial. It was calculated using the formula below:
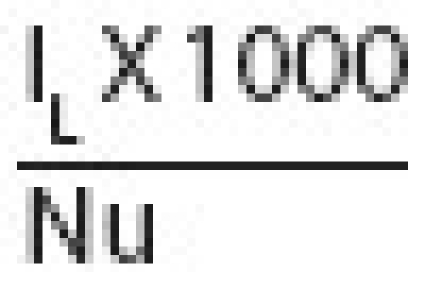
where IL is the imaging load per year and NU is total number of patients seen in the hospital/health unit per year.
Type specific imaging burden and disease specific imaging burden (DSIB)
These are rate indices. Type specific imaging burden (TSIB) is the IB concerning a specified type of investigation, e.g., the number of patients per thousand hospital patients per year, for whom ultrasound would be beneficial, is the TSIB for ultrasound. The disease specific imaging burden (DSIB) is the IB specific to that particular disease category e.g., the number per thousand tuberculosis (TB) patients per year for whom X-ray would be beneficial. TSIB and DSIB were also calculated similar to the way the IB was calculated.
OBJECTIVES
The first specific objective was to develop and apply four imaging needs indices on a case study basis, in five selected Ugandan hospitals. These indices are: IL, IB, TSIB and DSIB. The second objective was to explore the patient's, referring clinician's, and radiologist's perceptions regarding the values, meaning, and objective of imaging in patient care.
MATERIALS AND METHODS
Study design
This was a cross-sectional survey with triangulation. For the quantitative part of the study, cluster sampling was applied. The clusters were obstetrics and gynecology (Ob/Gyn), surgery, internal medicine, and pediatrics. The qualitative employed purposive sampling.
Study areas
Five health units were selected for inclusion:
-
(i)
One government tertiary level hospital - Mulago hospital.
-
(ii)
Two government Regional Referral (secondary level) hospitals - Kabale and Mbale hospitals.
-
(iii)
Two government General (primary level) hospitals - Rakai and Masindi hospitals.
The selection of these hospitals was to allow hierarchical and geographical representation, thereby improving both internal validity and generalizability.
Sample size and sampling procedure for the quantitative component of the study
The sample size was estimated using the formula by Kish and Leslie. Cluster sampling was employed and a design effect E applied, with E = 1 and sample size of 384, for primary level hospitals, and E = 2 and a sample size of 786 for regional and tertiary hospitals.[5]
A systematic sampling procedure was applied. The period of data collection was fixed at 3 months due to logistical limitations.
Methods of data collection for the quantitative component of the study
The data pertaining to imaging was extracted from the patients' case notes. This information was recorded on pre-coded data sheets and used for rating appropriateness and subsequently for calculating the performance indices.
Rating for appropriateness
A group of three peer raters excluding the principal investigator (PI) rated each patient's case details, as to whether imaging would have benefited or not. Each case note was initially rated by two raters as to whether the patient would benefit from imaging or not. Rating was independent and each rater was blind to the score assigned by the other raters. The rating was based on a set of previously agreed on set of imaging criteria designed by the raters together with the PI for purposes of this study. If the two raters agreed that the patient would have benefited from imaging, then imaging was deemed appropriate for that patient. If the two raters disagreed, a third rater who was not the PI was brought in as a tie breaker. This information was used to calculate the four needs indices.
Data collection for the qualitative component of the study
Twenty two in-depth interviews (IDI), 4 focus group discussions (FGDs), and 42 self-administered questionnaires (SAQ) were employed to explore the value, role, and meaning clinicians and radiologists attached to imaging. Patients were interviewed for their perception on imaging and its role in patient care.
Sources of bias in the calculation of efficiency indices
The possible causes of bias in this study were two namely: Inability to accurately define the outcome variable namely (appropriate and non-appropriate requisitions) and inability to get a gold test or gold standard for appropriateness. As a solution, a criterion for appropriateness was developed and applied. Using two raters to agree on appropriateness helped to overcome subjectivity by just one observer and where the two disagreed, a third rater was brought in as a tie-breaker.
Ethical clearance
Ethical clearance was obtained from the Uganda National Council for Science and Technology.
RESULTS
Study population characteristics
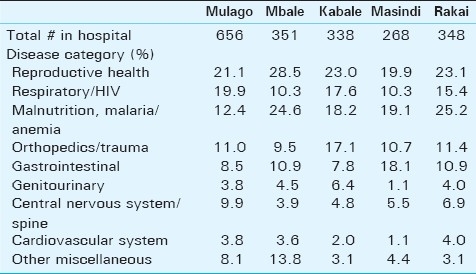
The total sample size was 1961 patients, 46% outpatients and 54% inpatients. The distribution among clusters was: Ob/Gyn 24.5%, surgery 22.5%, internal medicine 25.9%, and pediatrics 27.1%. The male to female ratio was 0.6:1. Age ranged from 1 to 90 years, with a mean age of 22.9 years and standard deviation of 19.7. The clinical diagnoses for the patients in the sample were summarized into nine broad disease categories [Table 1].
Table 1.
Percentage of disease categories within the hospitals
Imaging load (IL)
At Mulago tertiary hospital, the projected yearly imaging load (IL) was 182,874 patients (based on an annual output workload of 481,249 patients and a calculated appropriate proportion of 38%), for Mbale regional hospital it was 52,111 patients (based on an annual output workload of 106,350 patients and a calculated appropriate proportion of 49%), for Kabale regional hospital, it was 28,743 patients (based on an annual output workload of 56,358 patients and a calculated appropriate proportion of 51%), for Masindi district hospital it was 1270 patients (based on an annual output workload of 2,702 patients and a calculated appropriate proportion of 47%), and for Rakai district hospital it was 4571 patients (based on an annual workload of 8,791 patients and a calculated proportion of 52%).
Imaging burden
The average IB for all the hospitals was 460 per 1000 hospital patients per year distributed as: Mulago hospital 380 per 1000 per year, Mbale hospital 490 per 1000 per year, Kabale hospital 510 per 1per year, Masindi hospital 470, and Rakai 520 per 1000 patients per year.
IB and level of the hospital
The IB for Tertiary referral hospital was 380 per 1000 patients per year, for the Regional hospital level, it was 510, and for General 490 per 1000 patients per year.
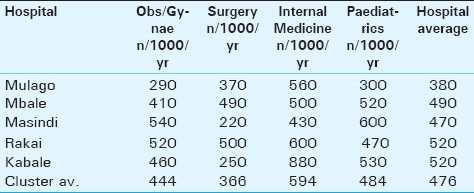
IB and cluster
The IB for the Obs/Gynae cluster, considering all hospitals, was 420 per 1000 per year, for surgery 380 per 1000 per year, for internal medicine 580, and for pediatrics 460 per 1000 per year. The IB within the various clusters for the five hospitals was highest for internal medicine in three hospitals, followed by pediatrics in two hospitals [Table 2].
Table 2.
Imaging burden within clusters for the five hospitals
Relationship between IB and age
Patients were divided into seven age groups and IB was calculated for each age group. The highest IB was for the age group 51-50 years, (520 per 1000 patients per year) followed by the age group 41-50 years (500 per 1000 patients per year). For the rest of the age brackets, IB ranged from 420 to 460.
Relationship between IB and gender
Females formed 60% of the total sample size. The IB was 460 per 1000 patients per year in females and 470 per 1000 per year in males.
Relationship between IB and disease category (Disease Specific Imaging Burden)
There was a variation of the DSIB with disease category. DSIB was highest in the cardiovascular (530 per 1000 patients per year) followed by malnutrition, anemia and malaria (520 per 1000 patients per year), GIT (510), respiratory and HIV (500), genitourinary (470), central nervous system (430), Obstetrics and gynecology (410), and orthopedics and trauma (390).
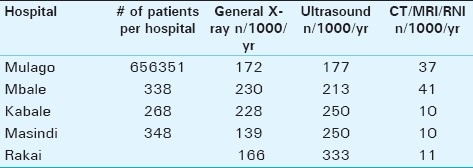
Type specific imaging burden
The highest type specific imaging burden (TSIB) was for ultrasound 232 per 1000 patients per year, followed by conventional radiography with 191 per 1000 patients per year). CT and MRI had TSIB of 25 per 1000 patients per year. For four out of the five hospitals, ultrasound had the highest TSIB [Table 3].
Table 3.
Type specific imaging burden for examinations in the hospitals
How patients' perceptions, influence the need for imaging
A total of 72 patients were interviewed, concerning their perceptions, objectives, values, and the meaning they attached to imaging. The patients were categorized into two groups based on their level of education. Group 1, which had 36 patients, was composed of those with no formal education or with primary level education. Group 2, which had 36 patients, was composed of those with secondary, and with or without additional tertiary education.
It was noted that one-third of the patients from group one knew nothing at all as to the role imaging results would play in their management, compared to a tenth of those from group two. Most of the patients thought that the results were to play a major role, helping in finding out the disease and its severity. One patient from group one said: “The doctor will know the cause and gravity of my illness, and will use that as a basis to treat me”. One patient from Group 1 thought imaging was also curative.
The value of imaging to patients
Most patients from both groups attached high value to imaging, with regard to their particular illness. One-third of the patients from Group 2 compared to almost one-half from Group 1 felt that all patients with serious diseases regardless of the type of disease should receive imaging. They felt that the doctor would not make an accurate diagnosis without imaging. In response to how one would feel if the doctor had not asked for imaging, one patient from Group 2 said: “the diagnosis the doctor would have made is not right, because I believe the X-ray helps in diagnosis”.
In response to whether one would have asked for the imaging himself or herself if the doctor had not, almost one-third of the patients from both groups replied they would. They had a great desire to know what was happening inside their bodies, which to them only imaging could reveal. One said: “I don't know what is happening inside my body, causing my illness, yet I want to know.”
Meaning of imaging to patients
Imaging meant much to the majority of the patients regardless of education status. A large majority of those from both groups thought that imaging meant good health care and was necessary for their illness to be cured. One patient from Group 2 said: “I would not have been satisfied with the way I am being managed by my doctor if he had not asked for imaging”.
Patient's desires and wishes
About half of the patients had had an explanation from the referring doctor as to why they should be imaged. The majority of the patients from both groups were anxious to know from their referring doctor, the role the imaging results were to play in their management. Some wished to know from the referring doctor what would happen to them subsequent to being imaged.
Misconceptions and fears
The majority of the patients had misconceptions about imaging . Almost one-third of the patients from both groups wished that the referring doctor would have informed them about the dangers and risks from imaging. One patient expressed this desire saying: “I would have wanted to know from my doctor whether the X-rays enter you or not”. Another said: “I would have wanted the doctor to encourage me that there is no harm from the X-rays”.
Further questioning revealed that only a quarter of the patients from Group 1 knew that X-rays may be harmful compared to one half from Group 2. Some thought they might reduce or weaken life. One patient from Group 2 stated : “they cut short one's life” and another: “they disorganize baby's growth”. A patient from Group 1 expressed her fears saying: “I was told if pregnant women are scanned a lot, they give birth to albinos”.
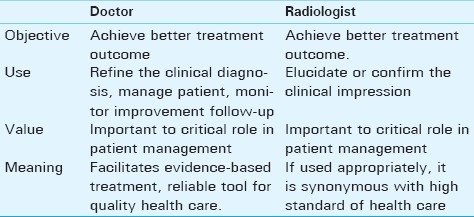
The meaning, value and objective the clinician and radiologist attached to imaging
The users pointed out the important role of imaging in patient care as shown in the matrix which summarizes the objective, value, and use of imaging to two users of the two users for imaging [Table 4].
Table 4.
A summary of the objective, value, use, and meaning the clinician and the radiologist attached to imaging
DISCUSSION
Imaging burden
IB for different hospitals
The overall IB of 460 per 1000 patients per year [Table 2], with slight variations in the different hospitals may be explained by a higher prevalence of disease categories, which have higher probability for imaging [Table 1]. The lower level health units have a higher IB possibly because of the higher proportion of diseases like respiratory/HIV, obstetrics and gynecology and malnutrition, which carry a relatively high DISB. Patients with malnutrition are usually pediatric and chest X-ray is performed in these patients to exclude coexisting pulmonary tuberculosis. The relatively low IB for Mulago hospital, a tertiary hospital, may be explained by the fact that currently the hospital functions both as tertiary and general hospital, and receives general cases in addition to more complex referrals from lower level hospitals. It, therefore, has a heterogeneous patient population.
IB within clusters
The IB was highest for the internal medicine cluster, 580 per 1000 patients per year, followed by the pediatrics cluster [Table 2]. The high burden in the internal medicine and pediatrics may be related to the high prevalence of disease categories in this cluster which have a high DSIB namely: TB and other respiratory tract infections, central nervous system, cardiovascular, GIT, and malnutrition. The need for chest radiography in HIV/AIDS patients to a large extent contributes to the imaging burden for Internal medicine. Cockshott also recorded trauma, chest infection and obstetrics as the commonest disease conditions requiring imaging in several African countries.[6]
IB within disease categories
The IB within disease categories (DSIB) varied for different diseases [Table 1]. The different DSIB for various disease categories may be related to the disease-specific clinical signs plus the potential of that disease to be diagnosed by imaging. Furthermore, imaging should have a high likelihood of influencing therapy decisions for that particular disease. For this reason, cardiac, CNS, GIT, and respiratory diseases and HIV had a high DSIB.
Type specific imaging burden
The highest TSIB was for ultrasound followed by general X-ray. The relatively higher prevalence of abdominal and pelvic pathology requiring ultrasound in all clusters may account for ultrasound being the imaging decision of choice for these two clusters. On the other hand, internal medicine and pediatric clusters have a higher proportion of chest pathology, especially bacterial and TB infections, and these lend themselves to X-ray diagnosis, hence they register a higher general X-ray TSIB.
This study has clearly demonstrated that overall, in Uganda, ultrasound is emerging as the leading beneficial imaging modality, surpassing X-ray and this may support its increasing usage. This is in contrast to USA where the utilization of ultrasound appears to be declining relative to CT.[7–9] These trends in USA have been attributed to changes in perception of physicians concerning the clinical usefulness of these technologies.[8]
The influence of patients' perceptions on imaging needs
The patients in general regarded imaging as a very important process, enabling diagnosis and rational treatment. According to this study, appropriate application of imaging was taken to be synonymous with high standards of health care. This view was the same among the patients regardless of educational status. The symbolic interactionism theory,[10,11] states that people behave and interact based on how they interpret or give meaning to specific symbols in their lives. The symbol in this case is imaging and the individuals relating to this symbol are the patients. The meaning and value the patient attaches to imaging will influence his/her need for imaging. At an individual level, the need for imaging is dictated not only by the patient's illness, but also by the way he/she perceives the role of imaging in management of the illness, plus meaning and value he/she has toward the imaging phenomenon. Because of the value the patient places on imaging, he/she may demand imaging regardless of its relevance and benefit.[12] Farjado underscores the role of the patient's attitude, values, and preferences in seeking and accepting medical tests. He argues that in addition to the usefulness factors, patients' attitudes, values, and preferences should be considered.[13]
Some patients who participated in this study expressed their fears and misconceptions toward imaging. The patient's misconceptions and fears may have a negative effect on the imaging-seeking behavior. The stigma attached to radiation is at the back of most patients' minds and a referral to radiology may be a mysterious and frightening experience, a painful intrusion into their privacy. They may feel vulnerable, fragile or emotional amidst the forest of technology and barriers imposed by the technical language in the department. This may cause them to yearn for empathy and a listening ear. They will want to be treated as individuals by other individuals, rather than as items by an impersonal organization.[14]
CONCLUSIONS
There is a high IB of 460 per thousand patient populations per year, mainly due to ultrasound and general X-ray investigations. The patient has perceptions and misconceptions, which influence the need for imaging. These perceptions and misconceptions should be addressed. Public awareness interventions on the value, capabilities, limitations and adverse effects of various imaging modalities need to be undertaken to ensure that the patients make informed imaging choices and readily avail themselves in situations where imaging is crucial for example in suspected high risk pregnancy.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/53/90035
REFERENCES
- 1.Republic of Uganda. Uganda Demographic and Health Survey. The Republic of Uganda: 2006. Jan 01, [Google Scholar]
- 2.Ssennono V, Petit P, Leadbeter D. Uganda 2002 population and housing census special analysis on health workers considered by the EU DHRH Project. 2005 [Google Scholar]
- 3.Ministry of Health Uganda. Vol. 1. Kampala, Ministry of Health, Uganda: 2005. Health Sector Strategic Plan II, 2005/06 - 2009/10. [Google Scholar]
- 4.Ministry of Health Uganda. Ministry of Health, Uganda.: 2005. National Health Equipment Policy Document. [Google Scholar]
- 5.Kalsbeck WF. C sample: Analysing data from complex survey samples.Epi info version 6, users guide. 2000;157:82. [Google Scholar]
- 6.Cockshott WP. Diagnostic radiology: Geography of a high technology. AJR Am J Roentgenol. 1979;132:339–44. doi: 10.2214/ajr.132.3.339. [DOI] [PubMed] [Google Scholar]
- 7.Liebeskind ME, Arger PH, Liebeskind A, Maston K, Langlotz C. Using sonography to examine adult patients at an academic medical center: Have usage patterns changed with the expansion of managed care? AJR Am J Roentgenol. 2002;179:1395–9. doi: 10.2214/ajr.179.6.1791395. [DOI] [PubMed] [Google Scholar]
- 8.Martin TA, Quiroz FA, Rand SD, Kahn CE., Jr Applicability of American College of Radiology appropriateness criteria in a general internal medicine clinic. AJR Am J Roentgenol. 1999;173:9–11. doi: 10.2214/ajr.173.1.10397090. [DOI] [PubMed] [Google Scholar]
- 9.Khasgiwala VC, Aronson MD, Davis RB, Rosen MP. Imaging utilization in the era of the hospitalis. AJR Am J Roentgenol. 2006;187:2–7. doi: 10.2214/AJR.05.0664. [DOI] [PubMed] [Google Scholar]
- 10.Blumer H. New Jersy: Prentice-Hall. Inc; 1967. Symbolic interactionism, perspective and method. [Google Scholar]
- 11.Mead GH1. George herbert mead on social psychology. Chicago: University of Chicago Press; 1964. [Google Scholar]
- 12.Abrams HL. Sounding board: The overutilization of x-rays. New Engl J Med. 1979;300:11213–6. doi: 10.1056/NEJM197905243002110. [DOI] [PubMed] [Google Scholar]
- 13.Fajardo LL. Measuring and incorporating patient preferences and utilities in the assessment of diagnostic technology. Acad Radiol. 1999 Jan;(6 Suppl 1):S113–4. doi: 10.1016/s1076-6332(99)80104-4. [DOI] [PubMed] [Google Scholar]
- 14.Alderson OP. Noninterpretive skills for radiology residents: Customer service and satisfaction in radiology. AJR Am J Roentgenol. 2000;175:319–23. doi: 10.2214/ajr.175.2.1750319. [DOI] [PubMed] [Google Scholar]


