Abstract
Objectives of study
To test recent claims that cancer inequities are bound to increase as population health improves.
Methods
We analyzed 1960–2006 age-standardized US county cancer mortality data, total and site-specific (lung, prostate, colorectal, breast, cervix, stomach), stratified by county income quintile for the US total, black, and white populations.
Results
Between 1960 and 2006, US socioeconomic inequities in cancer mortality variously shrunk, widened, reversed, and stagnated, depending on time period and cancer site. For all cancers combined and most, but not all, sites, absolute, but not relative, socioeconomic gaps were greater for the black compared to white population. Compared to the yearly age-specific mortality rates among whites in the most affluent counties, the percent of excess cancer deaths among whites in the lower four county income quintiles first rose above 0 in 1990 and in 2006 equaled 5.4% (95% CI 4.8, 6.0); among blacks, it rose from 6.0% (95% CI 4.5, 7.4) in 1960 to 24.7% (95% CI 23.9, 25.5) in 1990 and remained at this level through 2006.
Conclusions
The hypothesis that cancer mortality inequities are bound to increase is refuted by long-term data on total and site-specific cancer mortality stratified by socioeconomic position and race/ethnicity.
Keywords: Black, Cancer mortality, Secular trends, Socioeconomic inequalities, Race/ethnicity
Introduction
Must socioeconomic inequities in cancer mortality inevitably increase, a consequence of more affluent persons having increasingly better access to healthy living and working conditions and also to appropriate health care when ill? This hypothesis, proposed two decades ago [1], increasingly features in research on social inequalities for both cancer and other health outcomes [2, 3]—albeit with most studies having typically examined data only spanning up to two decades, often starting only in the 1980s.
Yet, challenging claims about socioeconomic cancer inequities inevitably increasing as population health improves are findings from the six extant cancer mortality studies that have examined long-term trends spanning at least four decades and/or extending back to 1960 or earlier: three US [4–6] (two nationally representative (1950–1998) [4, 5], one comparing two predominantly white and relatively affluent cohorts (1959–1972 and 1982–1996) [6], and none stratified by race/ethnicity) and three European (Norway (1960–2000) [7]; the Netherlands (1950–1984) [1]; and England and Wales (1851–1971) [8]). In all six studies, relative and absolute socioeconomic inequities in cancer mortality variously shrank, widened, and reversed over time, with patterns varying both within and across cancer sites.
Accordingly, to update and strengthen tests of the hypothesis that socioeconomic inequities in cancer mortality are bound to increase, we have conducted a repeat cross-sectional analysis of 1960–2006 age-standardized US county mortality rates stratified by county income quintile for the total, white, and black population. Our a priori hypothesis—framed by the ecosocial theory of disease distribution and its approach to analyzing how we literally embody, biologically, our societal and ecological context, thereby creating population patterns of health and health inequities [9]—was that trends in the patterning of socioeconomic inequities in cancer mortality would vary by time period, race/ethnicity, and cancer site.
Methods and materials
Mortality data
We obtained US county-level mortality data for 1960–1967 from the US National Center for Health Statistics (NCHS) [10], for which we then manually located and identified the correct county codes for each of the 3,073 counties[11]; we extracted the corresponding 1968–2006 data from the NCHS US Compressed Mortality files [12]. Underlying cause of death was coded according to the International Classification of Diseases (ICD), with codes matched to the year in which the deaths occurred: ICD-7 (1960–1967), ICD-8 (1968–1978), ICD-9 (1979–1998), and ICD-10 (1999–2006) (see eTable 1) [13]. We analyzed mortality data for all cancers (20.6 million cancer deaths; Table 1) and also for breast (women only), cervix, colorectal, lung, prostate, and stomach cancer, selected because they rank among the leading causes of both US cancer mortality and socioeconomic inequalities in US cancer mortality [3–6]. The study was approved as exempt by the Harvard School of Public Health Human Subjects Committee (HSC Protocol #P15744-101).
Table 1.
Number of deaths (n) and person-years (PY) at risk for cancer mortality (all sites and site-specific) for the total population, white population, and black population: United States, 1960–2006
| Cancer site | Total population |
White population |
Black population |
|||
|---|---|---|---|---|---|---|
| PY | n | PY | n | PY | n | |
| All cancers | 11,077,768,226 | 20,577,377 | 9,384,715,232 | 18,100,542 | 1,340,337,459 | 2,221,738 |
| Breast | 5,666,140,764 | 1,695,774 | 4,783,072,922 | 1,501,313 | 703,058,019 | 177,897 |
| Colorectal | 11,077,768,226 | 2,419,268 | 9,384,715,232 | 2,159,487 | 1,340,337,459 | 233,4 |
| Cervical | 5,666,140,764 | 254,806 | 4,783,072,922 | 196,450 | 703,058,019 | 54,009 |
| Lung | 11,077,768,226 | 5,102,902 | 9,384,715,232 | 4,520,608 | 1,340,337,459 | 525,801 |
| Prostate | 5,411,627,462 | 1,156,377 | 4,601,642,310 | 964,728 | 637,279,440 | 182,420 |
| Stomach | 11,077,768,226 | 692,764 | 9,384,715,232 | 570,211 | 1,340,337,459 | 104,014 |
Denominator data
We obtained county-level denominator data from the 1960–2000 US decennial counts, US Census Bureau intercensal population estimates, and NCHS estimates for 1968–1969 (interpolated) and 2001–2006 (extrapolated) [12]. We estimated the 1961–1967 denominators using linear interpolation, based on the 1960 and 1968 population data [11], and followed NCHS guidelines for merging and unmerging the small number of counties over time which were eliminated, established, or had boundaries redrawn [12]. Because Alaska used nonidentical county boundaries in their pre-1989 population and mortality data, Alaska analyses before 1989 were for the entire state only (equaling 0.01–0.02% of the US population). Overall, the study included 11.1 billion person-years of observation (Table 1).
County income quintiles and racial/ethnic classification
We employed US census decennial 1960–2000 county-level data on median family income [11, 14, 15], which we adjusted for inflation and regional cost of living [11, 16]. Analyses by county education level yielded similar results and are not shown. We used linear interpolation for intercensal years and extrapolated for 2001–2006 based on the slope for 1990–2000 [11]. We then assigned counties to quintiles (Q5: highest income; Q1: lowest income; cut-points in eTable 2), which we weighted by county population size, given its enormous variation [11]—e.g., ranging in 1960 from 47 in Yellowstone National Park, MT to 6,038,771 in Los Angeles County, CA, and in 2006 from 67 in Loving County, TX to 9,519,338 in Los Angeles County, CA. Missingness due to counties lacking income data was minimal (<1%) for both denominators and numerators.
We conducted all analyses for the US total, black, and white populations. Given well-known limitations of and changes in US mortality and census racial/ethnic classifications [17], including lack of long-term data on racial/ethnic groups other than white or black [10, 12, 17, 18], we followed standard practice and reclassified the “non-white” population as “black” for the period 1960–1967, when data were available only for the “white” and “non-white” population [18]. Suggesting this approach is reasonable, in 1960, 92% of the US “non-white” population was black, and mortality rates of these two populations were almost identical [18]. New Jersey death certificates did not identify race/ethnicity in 1962 and 1963, precluding the use of these two years' data (<3% of the US population).
Statistical analysis
For each calendar year, we aggregated the county mortality and population data in each county income quintile and calculated each quintile's age-standardized mortality rates, standardized to the year 2000 standard million [11]. We used SAS 9.1 to conduct all of our analyses [19], unless otherwise indicated.
For each outcome, we compared rates in the lower to highest county income quintiles to calculate each year's age-standardized mortality rate ratio (MRR), a measure of relative disparity, and also the mortality rate difference (MRD), a measure of absolute difference [11, 20]. We also calculated the total and proportion of deaths that would not have occurred each year if residents of the four lowest county income quintiles experienced the same yearly age-specific death rates as persons in the highest county income quintile: a related set of calculations for the black and white population set as referent group the mortality rate of white persons in the highest county income quintile. This metric—mathematically equivalent to the population attributable fraction (PAF) [21]—can meaningfully be interpreted as a measure of preventable excess mortality, quantifying the gap between the empirically observed and then achievable death rates across county income quintiles [11, 18, 21].
To explore changes in the slope of the decline in mortality rates, the MRR, and the MRD, we used joinpoint regression techniques [22, 23]. In these models, line segments are joined at “joinpoints,” which denote statistically significant changes (p < 0.05) in the time trend [22, 23]. The slope of these line segments, when fit on the log scale, is interpretable as the log annual percent change (APC) in the rate [22, 23].
Role of funder
The study funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Results
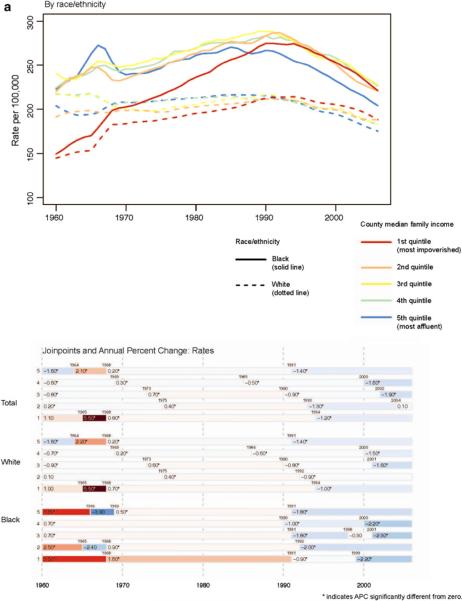
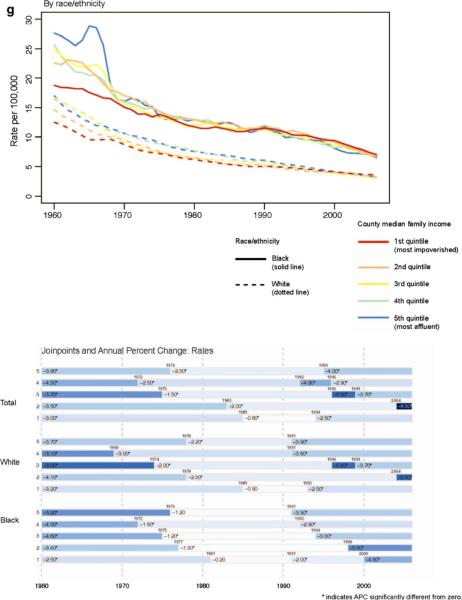
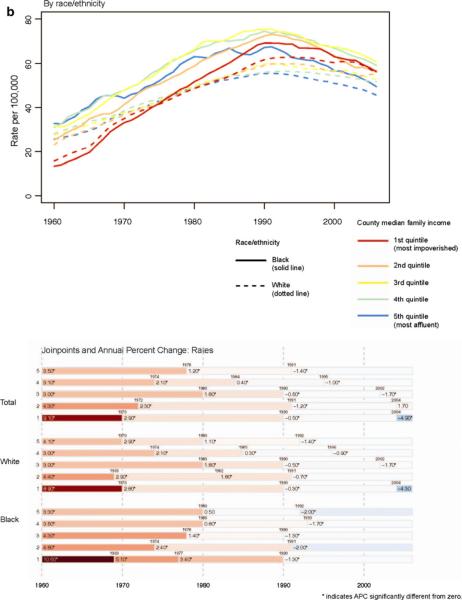
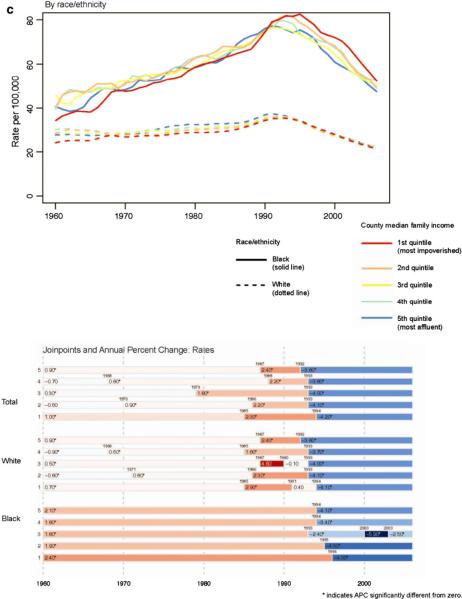
As shown in Fig. 1, trends in US cancer mortality rates, total and site-specific, have displayed considerably heterogeneity by county income quintile, thereby yielding a mix of widening, shrinking, reversing, and stagnating socioeconomic inequities. Figure 2a–g and Table 2a–g further stratify results by race/ethnicity.
Fig. 1.
Cancer mortality rates (age-standardized to the year 2000 standard million), total and site-specific, for the total population by county income quintile: United States, 1960–2006
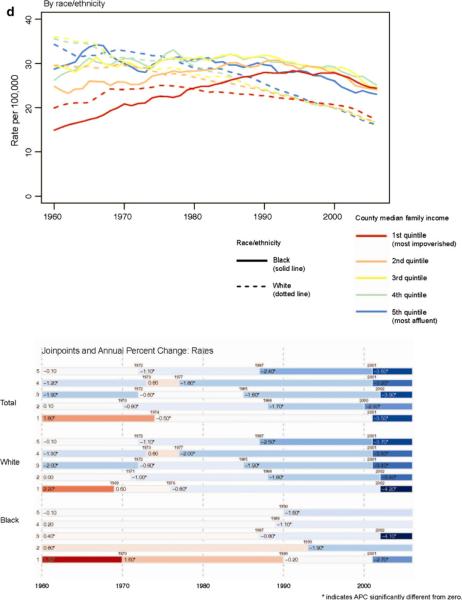
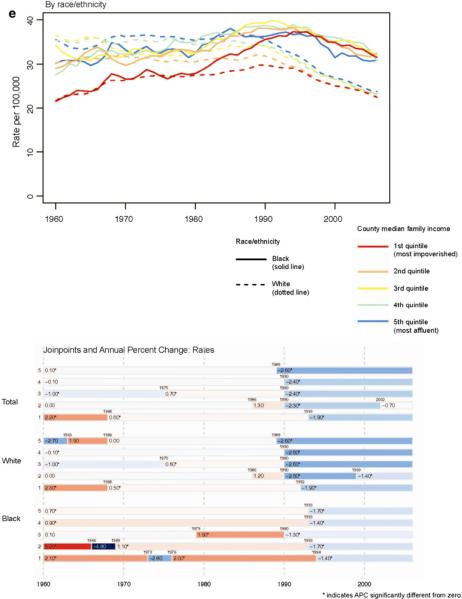
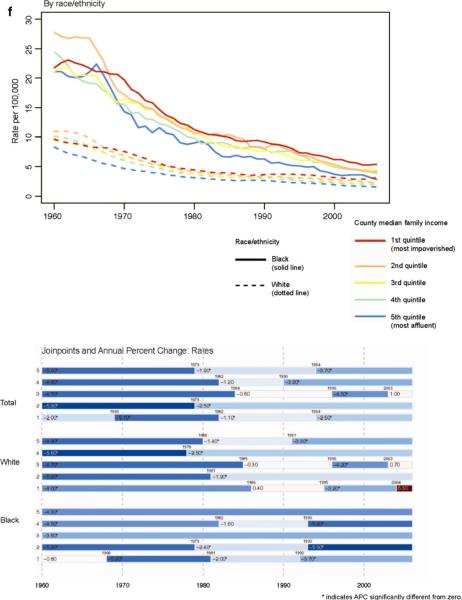
Fig. 2.
Cancer mortality rate (age-standardized to the year 2000 standard million) by county income quintile for the white and black population, and the corresponding joinpoints, and annual percent change (APC) (95% CI) between joinpoints: a total cancer, b lung, c prostate, d colorectal, e breast (women), f cervical, and g stomach: United States, 1960–2006
Fig. 2g.
stomach cancer mortality
Table 2.
Mortality rate ratio (MRR) and mortality rate difference (MRD) by county income quintile, and population attributable fraction (PAF), for the total, white, and black population: United States, 1960, 1970, 1980, 1990, 2000, and 2006
| Population | County income quintile | Year |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1960 |
1970 |
1980 |
1990 |
2000 |
2006 |
||||||||
| MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | ||
| (a) Cancer mortality rate (all sites) | |||||||||||||
| Total | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 1.06 | (1.05, 1.07) | 1.01 | (1.00, 1.03) | 1.02 | (1.01, 1.03) | 1.00 | (0.99, 1.01) | 1.05 | (1.04, 1.05) | 1.06 | (1.05, 1.07) | |
| 3 | 1.07 | (1.06, 1.09) | 0.98 | (0.97, 0.99) | 0.98 | (0.97, 0.99) | 1.04 | (1.03, 1.05) | 1.06 | (1.05, 1.07) | 1.07 | (1.06, 1.08) | |
| 2 | 0.95 | (0.94, 0.96) | 0.97 | (0.96, 0.99) | 0.98 | (0.97, 0.99) | 1.02 | (1.01, 1.02) | 1.04 | (1.03, 1.05) | 1.09 | (1.08, 1.10) | |
| 1 (lowest) | 0.71 | (0.70, 0.72) | 0.89 | (0.88, 0.91) | 0.94 | (0.93, 0.95) | 1.02 | (1.01, 1.03) | 1.09 | (1.08, 1.10) | 1.09 | (1.09, 1.10) | |
| White | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 1.06 | (1.05, 1.08) | 1.00 | (0.99, 1.01) | 1.00 | (0.99, 1.01) | 0.99 | (0.98, 1.00) | 1.02 | (1.02, 1.03) | 1.05 | (1.04, 1.06) | |
| 3 | 1.07 | (1.06, 1.08) | 0.97 | (0.96, 0.98) | 0.97 | (0.96, 0.98) | 1.01 | (1.00, 1.02) | 1.03 | (1.02, 1.04) | 1.04 | (1.03, 1.05) | |
| 2 | 0.94 | (0.93, 0.95) | 0.96 | (0.95, 0.97) | 0.95 | (0.94, 0.96) | 0.99 | (0.98, 1.00) | 1.03 | (1.02, 1.03) | 1.07 | (1.06, 1.08) | |
| 1 (lowest) | 0.71 | (0.70, 0.72) | 0.89 | (0.88, 0.90) | 0.92 | (0.91, 0.93) | 0.99 | (0.98, 1.00) | 1.06 | (1.05, 1.07) | 1.07 | (1.06, 1.08) | |
| Black | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 1.01 | (0.95, 1.06) | 1.02 | (0.97, 1.07) | 1.03 | (0.99, 1.07) | 1.06 | (1.03, 1.10) | 1.11 | (1.08, 1.15) | 1.11 | (1.08, 1.15) | |
| 3 | 1.08 | (1.03, 1.13) | 1.03 | (0.98, 1.09) | 1.04 | (1.00, 1.08) | 1.10 | (1.06, 1.13) | 1.08 | (1.05, 1.12) | 1.12 | (1.08, 1.15) | |
| 2 | 0.99 | (0.94, 1.04) | 0.98 | (0.93, 1.03) | 1.02 | (0.99, 1.06) | 1.07 | (1.04, 1.11) | 1.06 | (1.03, 1.09) | 1.08 | (1.05, 1.11) | |
| 1 (lowest) | 0.67 | (0.64, 0.70) | 0.84 | (0.80, 0.88) | 0.91 | (0.88, 0.94) | 1.05 | (1.01, 1.08) | 1.06 | (1.03, 1.10) | 1.08 | (1.05, 1.11) | |
| MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | 12.4 | (9.7, 15.1) | 2.9 | (0.5, 5.4) | 3.4 | (1.2, 5.6) | 0.5 | (−1.5, 2.4) | 8.9 | (7.1, 10.6) | 11.1 | (9.5, 12.7) | |
| 3 | 15.2 | (12.5, 17.8) | −3.9 | (−6.3, −1.4) | −3.5 | (−5.7, −1.4) | 8.8 | (6.9, 10.8) | 11.5 | (9.8, 13.2) | 12.5 | (11.0, 14.1) | |
| 2 | −10.8 | (−13.4, −8.2) | −5.5 | (−7.9, −3.1) | −3.9 | (−6.0, −1.7) | 3.3 | (1.4, 5.2) | 7.8 | (6.1, 9.5) | 16.1 | (14.6, 17.7) | |
| 1 (lowest) | −59.8 | (−62.2, −57.4) | −22.0 | (−24.3, −19.6) | −13.2 | (−15.3, −11.2) | 4.5 | (2.5, 6.4) | 16.9 | (15.2, 18.6) | 16.4 | (14.9, 17.9) | |
| White | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | 12.9 | (10.1, 15.7) | 0.1 | (−2.4, 2.7) | 0.2 | (−2.0, 2.5) | −3.1 | (−5.2, −1.0) | 4.9 | (3.0, 6.7) | 8.1 | (6.5, 9.8) | |
| 3 | 14.1 | (11.3, 16.8) | −6.5 | (−9.0, −4.0) | −6.0 | (−8.2, −3.8) | 1.6 | (−0.5, 3.7) | 6.4 | (4.6, 8.2) | 7.7 | (6.1, 9.4) | |
| 2 | −12.6 | (−15.3, −9.9) | −8.7 | (−11.3, −6.2) | −9.8 | (−12.0, −7.6) | −3.0 | (−5.0, −1.0) | 4.9 | (3.1, 6.7) | 13.0 | (11.4, 14.6) | |
| 1 (lowest) | −59.4 | (−61.9, −56.8) | −23.7 | (−26.1, −21.2) | −17.8 | (−19.9, −15.6) | −1.9 | (−3.9, 0.1) | 11.0 | (9.2, 12.8) | 13.0 | (11.3, 14.7) | |
| Black | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | 1.5 | (−10.5, 13.6) | 4.2 | (−8.6, 17.0) | 7.3 | (−2.8, 17.5) | 16.2 | (6.9, 25.5) | 26.5 | (18.6, 34.3) | 22.4 | (15.8, 29.1) | |
| 3 | 17.6 | (6.5, 28.8) | 7.1 | (−6.0, 20.2) | 9.6 | (−1.3, 20.4) | 25.4 | (16.4, 34.4) | 19.8 | (12.6, 27.0) | 23.7 | (17.5, 29.8) | |
| 2 | −2.8 | (−13.5, 7.9) | −6.0 | (−18.5, 6.5) | 6.4 | (−3.4, 16.1) | 19.6 | (10.6, 28.6) | 13.7 | (6.1, 21.2) | 16.7 | (10.4, 22.9) | |
| 1 (lowest) | −73.5 | (−83.0, −63.9) | −38.9 | (−50.9, −27.0) | −24.0 | (−33.4, −14.7) | 12.8 | (4.1, 21.5) | 15.1 | (8.2, 22.0) | 17.1 | (11.2, 22.9) |
| Referent | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Total, Q5 | −4.0% | (−4.8%, −3.2%) | −2.6% | (−3.4%, −1.8%) | −1.2% | (−1.9%, −0.6%) | 1.8% | (1.2%, 2.4%) | 4.9% | (4.4%, 5.5%) | 7.1% | (6.5%, 7.6%) |
| White | White, Q5 | −4.1% | (−4.9%, −3.2%) | −3.6% | (−4.5%, −2.8%) | −2.8% | (−3.5%, −2.1%) | −0.4% | (−1.1%, 0.2%) | 3.0% | (2.4%, 3.6%) | 5.4% | (4.8%, 6.0%) |
| Black | White, Q5 | 6.0% | (4.5%, 7.4%) | 13.5% | (12.3%, 14.7%) | 19.6% | (18.7%, 20.6%) | 24.7% | (23.9%, 25.5%) | 23.8% | (23.1%, 24.6%) | 23.0% | (22.3%, 23.8%) |
| Population | County income quintile | Year |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1960 |
1970 |
1980 |
1990 |
2000 |
2006 |
||||||||
| MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | ||
| (b) Lung cancer mortality rate | |||||||||||||
| Total | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 1.09 | (1.05, 1.12) | 1.07 | (1.04, 1.10) | 1.02 | (1.00, 1.04) | 1.02 | (1.01, 1.04) | 1.08 | (1.07, 1.10) | 1.15 | (1.13, 1.17) | |
| 3 | 1.07 | (1.04, 1.11) | 1.03 | (1.01, 1.06) | 1.03 | (1.01, 1.06) | 1.10 | (1.08, 1.12) | 1.13 | (1.11, 1.15) | 1.19 | (1.17, 1.21) | |
| 2 | 0.90 | (0.87, 0.93) | 0.99 | (0.97, 1.02) | 1.01 | (0.99, 1.03) | 1.08 | (1.07, 1.10) | 1.12 | (1.10, 1.13) | 1.23 | (1.21, 1.25) | |
| 1 (lowest) | 0.59 | (0.57, 0.62) | 0.95 | (0.92, 0.97) | 0.99 | (0.97, 1.01) | 1.13 | (1.11, 1.15) | 1.20 | (1.18, 1.22) | 1.22 | (1.20, 1.24) | |
| White | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 1.10 | (1.06, 1.13) | 1.04 | (1.02, 1.07) | 1.00 | (0.98, 1.02) | 1.01 | (0.99, 1.03) | 1.06 | (1.04, 1.08) | 1.13 | (1.11, 1.15) | |
| 3 | 1.07 | (1.04, 1.11) | 1.02 | (0.99, 1.05) | 1.02 | (1.00, 1.05) | 1.06 | (1.05, 1.08) | 1.10 | (1.08, 1.12) | 1.16 | (1.14, 1.18) | |
| 2 | 0.90 | (0.87, 0.94) | 0.98 | (0.96, 1.01) | 1.00 | (0.97, 1.02) | 1.06 | (1.04, 1.08) | 1.10 | (1.08, 1.12) | 1.22 | (1.19, 1.24) | |
| 1 (lowest) | 0.61 | (0.59, 0.64) | 0.96 | (0.93, 0.99) | 0.99 | (0.97, 1.01) | 1.11 | (1.09, 1.13) | 1.18 | (1.16, 1.20) | 1.22 | (1.20, 1.24) | |
| Black | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 0.94 | (0.83, 1.08) | 1.12 | (1.00, 1.26) | 1.04 | (0.97, 1.12) | 1.10 | (1.03, 1.18) | 1.16 | (1.09, 1.24) | 1.20 | (1.13, 1.27) | |
| 3 | 0.97 | (0.86, 1.09) | 1.06 | (0.94, 1.19) | 1.04 | (0.96, 1.13) | 1.15 | (1.08, 1.22) | 1.16 | (1.09, 1.23) | 1.23 | (1.16, 1.30) | |
| 2 | 0.77 | (0.68, 0.88) | 0.91 | (0.81, 1.02) | 0.93 | (0.87, 1.00) | 1.07 | (1.00, 1.14) | 1.10 | (1.03, 1.17) | 1.15 | (1.08, 1.22) | |
| 1 (lowest) | 0.41 | (0.36, 0.46) | 0.74 | (0.66, 0.83) | 0.79 | (0.73, 0.85) | 1.06 | (1.00, 1.13) | 1.08 | (1.02, 1.14) | 1.14 | (1.08, 1.20) | |
| MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | 2.3 | (1.4, 3.2) | 2.5 | (1.5, 3.5) | 1.2 | (0.1, 2.2) | 1.3 | (0.3, 2.3) | 4.3 | (3.4, 5.2) | 6.8 | (6.0, 7.6) | |
| 3 | 1.8 | (1.0, 2.7) | 1.2 | (0.2, 2.2) | 1.7 | (0.7, 2.8) | 5.6 | (4.6, 6.6) | 6.6 | (5.7, 7.5) | 8.3 | (7.5, 9.1) | |
| 2 | −2.6 | (−3.5, −1.8) | −0.2 | (−1.2, 0.8) | 0.6 | (−0.4, 1.6) | 4.7 | (3.7, 5.7) | 5.9 | (5.0, 6.8) | 10.2 | (9.4, 11.0) | |
| 1 (lowest) | −10.6 | (−11.4, −9.8) | −2.0 | (−2.9, −1.0) | −0.7 | (−1.6, 0.3) | 7.2 | (6.3, 8.2) | 10.0 | (9.1, 10.9) | 9.9 | (9.1, 10.7) | |
| White | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | 2.5 | (1.5, 3.4) | 1.6 | (0.6, 2.7) | 0.1 | (−0.9, 1.2) | 0.3 | (−0.7, 1.4) | 3.2 | (2.2, 4.1) | 6.1 | (5.2, 7.0) | |
| 3 | 1.8 | (0.9, 2.7) | 0.7 | (−0.3, 1.7) | 1.2 | (0.2, 2.3) | 3.6 | (2.6, 4.7) | 5.3 | (4.3, 6.2) | 7.2 | (6.4, 8.1) | |
| 2 | −2.5 | (−3.3, −1.6) | −0.6 | (−1.6, 0.5) | −0.2 | (−1.3, 0.8) | 3.4 | (2.3, 4.4) | 5.4 | (4.4, 6.3) | 9.8 | (8.9, 10.7) | |
| 1 (lowest) | −9.9 | (−10.7, −9.1) | −1.5 | (−2.5, −0.5) | −0.5 | (−1.6, 0.5) | 6.2 | (5.2, 7.3) | 9.2 | (8.3, 10.2) | 10.0 | (9.1, 10.9) | |
| Black | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | −1.8 | (−6.1, 2.5) | 5.5 | (0.2, 10.8) | 2.7 | (−2.1, 7.6) | 6.9 | (2.4, 11.5) | 9.5 | (5.6, 13.3) | 9.7 | (6.4, 13.0) | |
| 3 | −1.0 | (−4.9, 2.9) | 2.6 | (−2.7, 8.0) | 2.7 | (−2.5, 7.9) | 9.8 | (5.4, 14.2) | 9.0 | (5.5, 12.6) | 11.3 | (8.2, 14.4) | |
| 2 | −7.5 | (−11.2, −3.7) | −4.0 | (−9.0, 1.1) | −4.3 | (−8.9, 0.4) | 4.5 | (0.1, 8.9) | 5.6 | (1.9, 9.4) | 7.5 | (4.4, 10.6) | |
| 1 (lowest) | −19.4 | (−22.8, −16.1) | −11.4 | (−16.3, −6.6) | −13.7 | (−18.1, −9.3) | 4.2 | (0.0, 8.5) | 4.6 | (1.1, 8.0) | 6.8 | (3.9, 9.7) |
| Referent | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Total, Q5 | −7.0% | (−9.2%, −4.8%) | 2.0% | (0.2%, 3.7%) | 1.7% | (0.4%, 3.0%) | 7.1% | (6.0%, 8.1%) | 10.4% | (9.4%, 11.4%) | 15.0% | (14.0%, 16.0%) |
| White | White, Q5 | −5.7% | (−8.0%, −3.5%) | 1.3% | (−0.5%, 3.1%) | 0.9% | (−0.5%, 2.3%) | 5.3% | (4.2%, 6.5%) | 8.9% | (7.8%, 9.9%) | 14.0% | (13.0%, 15.1%) |
| Black | White, Q5 | −3.1% | (−7.4%, 1.3%) | 14.6% | (11.9%, 17.4%) | 19.5% | (17.6%, 21.5%) | 24.2% | (22.6%, 25.8%) | 21.6% | (20.0%, 23.1%) | 23.4% | (21.8%, 24.9%) |
| Population | County income quintile | Year |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1960 |
1970 |
1980 |
1990 |
2000 |
2006 |
||||||||
| MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | ||
| (c) Prostate cancer mortality rate | |||||||||||||
| Total | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 1.07 | (1.01, 1.14) | 1.05 | (0.99, 1.11) | 0.99 | (0.94, 1.04) | 0.97 | (0.93, 1.01) | 1.04 | (1.00, 1.09) | 1.05 | (1.01, 1.10) | |
| 3 | 1.04 | (0.98, 1.10) | 1.05 | (0.99, 1.11) | 0.95 | (0.91, 1.00) | 1.05 | (1.01, 1.09) | 1.05 | (1.01, 1.09) | 1.04 | (1.00, 1.08) | |
| 2 | 1.03 | (0.97, 1.10) | 1.02 | (0.96, 1.08) | 1.00 | (0.96, 1.05) | 1.01 | (0.97, 1.05) | 1.04 | (1.00, 1.08) | 1.04 | (1.00, 1.08) | |
| 1 (lowest) | 0.90 | (0.84, 0.95) | 1.02 | (0.96, 1.07) | 0.97 | (0.93, 1.02) | 1.02 | (0.98, 1.06) | 1.13 | (1.09, 1.17) | 1.08 | (1.04, 1.12) | |
| White | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 1.08 | (1.01, 1.16) | 0.99 | (0.93, 1.05) | 0.94 | (0.89, 0.99) | 0.93 | (0.89, 0.97) | 1.00 | (0.96, 1.04) | 1.02 | (0.98, 1.06) | |
| 3 | 1.02 | (0.96, 1.09) | 1.00 | (0.94, 1.06) | 0.92 | (0.88, 0.97) | 0.98 | (0.94, 1.03) | 0.97 | (0.93, 1.01) | 0.97 | (0.93, 1.01) | |
| 2 | 1.02 | (0.96, 1.09) | 0.97 | (0.91, 1.03) | 0.92 | (0.88, 0.97) | 0.95 | (0.91, 0.99) | 1.00 | (0.96, 1.04) | 0.99 | (0.95, 1.03) | |
| 1 (lowest) | 0.87 | (0.82, 0.93) | 0.94 | (0.89, 1.00) | 0.88 | (0.84, 0.93) | 0.94 | (0.90, 0.97) | 1.01 | (0.97, 1.05) | 0.98 | (0.94, 1.02) | |
| Black | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 0.97 | (0.78, 1.21) | 1.22 | (0.98, 1.51) | 1.10 | (0.94, 1.28) | 0.98 | (0.87, 1.11) | 1.14 | (1.01, 1.28) | 1.11 | (0.98, 1.25) | |
| 3 | 1.13 | (0.93, 1.37) | 1.20 | (0.96, 1.49) | 1.03 | (0.88, 1.20) | 1.01 | (0.90, 1.13) | 1.09 | (0.97, 1.21) | 1.06 | (0.95, 1.18) | |
| 2 | 0.99 | (0.82, 1.20) | 1.04 | (0.84, 1.28) | 1.13 | (0.98, 1.30) | 1.02 | (0.91, 1.15) | 1.11 | (0.99, 1.25) | 1.03 | (0.92, 1.16) | |
| 1 (lowest) | 0.84 | (0.71, 1.01) | 1.06 | (0.86, 1.29) | 1.06 | (0.92, 1.21) | 1.01 | (0.91, 1.13) | 1.19 | (1.07, 1.32) | 1.10 | (0.99, 1.23) | |
| MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | 2.1 | (0.3, 4.0) | 1.5 | (−0.2, 3.2) | −0.4 | (−1.9, 1.2) | −1.3 | (−2.7, 0.2) | 1.3 | (0.1, 2.4) | 1.2 | (0.3, 2.2) | |
| 3 | 1.1 | (−0.7, 2.9) | 1.3 | (−0.4, 3.0) | −1.6 | (−3.1, −0.1) | 2.0 | (0.5, 3.5) | 1.5 | (0.4, 2.6) | 0.9 | (0.0, 1.8) | |
| 2 | 1.0 | (−0.8, 2.7) | 0.5 | (−1.2, 2.1) | 0.0 | (−1.5, 1.5) | 0.4 | (−1.1, 1.8) | 1.2 | (0.1, 2.3) | 0.9 | (0.0, 1.8) | |
| 1 (lowest) | −3.0 | (−4.6, −1.3) | 0.5 | (−1.1, 2.1) | −0.8 | (−2.3, 0.6) | 0.7 | (−0.7, 2.1) | 3.7 | (2.6, 4.8) | 1.7 | (0.8, 2.6) | |
| White | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | 2.3 | (0.4, 4.2) | −0.2 | (−2.0, 1.5) | −2.0 | (−3.6, −0.4) | −2.5 | (−4.0, −1.0) | −0.1 | (−1.2, 1.1) | 0.4 | (−0.5, 1.4) | |
| 3 | 0.6 | (−1.2, 2.4) | 0.0 | (−1.7, 1.8) | −2.5 | (−4.1, −1.0) | −0.6 | (−2.1, 0.9) | −0.8 | (−2.0, 0.3) | −0.7 | (−1.6, 0.2) | |
| 2 | 0.7 | (−1.1, 2.5) | −0.9 | (−2.6, 0.8) | −2.6 | (−4.2, −1.1) | −1.9 | (−3.4, −0.5) | −0.1 | (−1.3, 1.0) | −0.2 | (−1.1, 0.7) | |
| 1 (lowest) | −3.6 | (−5.3, −1.9) | −1.6 | (−3.2, 0.0) | −3.9 | (−5.4, −2.4) | −2.3 | (−3.8, −0.9) | 0.2 | (−0.9, 1.3) | −0.5 | (−1.5, 0.4) | |
| Black | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | −1.1 | (−9.8, 7.7) | 9.8 | (−0.4, 20.1) | 5.5 | (−3.3, 14.3) | −1.6 | (−10.9, 7.7) | 8.4 | (0.8, 15.9) | 5.2 | (−0.7, 11.0) | |
| 3 | 5.2 | (−3.1, 13.4) | 8.8 | (−1.5, 19.2) | 1.6 | (−7.6, 10.7) | 0.4 | (−8.5, 9.3) | 5.3 | (−1.6, 12.1) | 2.8 | (−2.6, 8.1) | |
| 2 | −0.2 | (−7.9, 7.5) | 1.7 | (−8.0, 11.4) | 7.4 | (−1.0, 15.9) | 1.6 | (−7.3, 10.5) | 6.8 | (−0.4, 14.0) | 1.5 | (−3.9, 7.0) | |
| 1 (lowest) | −6.3 | (−13.3, 0.6) | 2.5 | (−6.8, 11.8) | 3.2 | (−4.8, 11.2) | 1.1 | (−7.5, 9.6) | 11.3 | (4.6, 18.0) | 4.9 | (−0.3, 10.0) |
| Referent | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Total, Q5 | 1.2% | (−2.4%, 4.9%) | 4.7% | (1.1%, 8.3%) | −0.5% | (−3.5%, 2.5%) | 1.5% | (−0.9%, 3.9%) | 6.5% | (4.1%, 8.8%) | 5.3% | (2.8%, 7.8%) |
| White | White, Q5 | 0.4% | (−3.4%, 4.3%) | −0.1% | (−4.0%, 3.8%) | −6.8% | (−10.1%, −3.5%) | −4.0% | (−6.7%, −1.3%) | 0.1% | (−2.6%, 2.8%) | 0.0% | (−2.9%, 2.8%) |
| Black | White, Q5 | 39.4% | (35.6%, 43.2%) | 50.2% | (47.3%, 53.0%) | 50.1% | (47.7%, 52.4%) | 53.7% | (51.8%, 55.5%) | 61.1% | (59.6%, 62.7%) | 58.5% | (56.7%, 60.2%) |
| Population | County income quintile | Year |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1960 |
1970 |
1980 |
1990 |
2000 |
2006 |
||||||||
| MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | ||
| (d) Colorectal cancer mortality rate | |||||||||||||
| Total | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 1.03 | (1.00, 1.07) | 0.97 | (0.94, 1.00) | 1.03 | (1.00, 1.06) | 0.97 | (0.95, 1.00) | 1.05 | (1.02, 1.08) | 1.06 | (1.03, 1.09) | |
| 3 | 1.05 | (1.01, 1.08) | 0.94 | (0.91, 0.97) | 0.98 | (0.96, 1.01) | 1.00 | (0.97, 1.02) | 1.06 | (1.03, 1.09) | 1.06 | (1.03, 1.09) | |
| 2 | 0.86 | (0.83, 0.89) | 0.90 | (0.88, 0.93) | 0.93 | (0.91, 0.96) | 0.97 | (0.94, 0.99) | 1.04 | (1.01, 1.07) | 1.07 | (1.04, 1.10) | |
| 1 (lowest) | 0.57 | (0.55, 0.59) | 0.72 | (0.70, 0.74) | 0.85 | (0.82, 0.87) | 0.92 | (0.89, 0.94) | 1.08 | (1.05, 1.11) | 1.12 | (1.08, 1.15) | |
| White | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 1.04 | (1.00, 1.07) | 0.96 | (0.93, 1.00) | 1.02 | (0.99, 1.05) | 0.96 | (0.93, 0.99) | 1.02 | (0.99, 1.05) | 1.04 | (1.01, 1.07) | |
| 3 | 1.05 | (1.01, 1.08) | 0.94 | (0.91, 0.97) | 0.97 | (0.94, 1.00) | 0.97 | (0.94, 0.99) | 1.02 | (0.99, 1.05) | 1.03 | (1.00, 1.06) | |
| 2 | 0.86 | (0.83, 0.89) | 0.90 | (0.88, 0.93) | 0.92 | (0.90, 0.95) | 0.94 | (0.92, 0.97) | 1.03 | (1.00, 1.05) | 1.05 | (1.02, 1.08) | |
| 1 (lowest) | 0.58 | (0.56, 0.60) | 0.73 | (0.71, 0.76) | 0.84 | (0.81, 0.86) | 0.90 | (0.87, 0.92) | 1.05 | (1.02, 1.08) | 1.08 | (1.04, 1.11) | |
| Black | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 0.91 | (0.78, 1.07) | 0.98 | (0.84, 1.15) | 1.04 | (0.92, 1.17) | 1.01 | (0.91, 1.12) | 1.13 | (1.02, 1.24) | 1.09 | (0.99, 1.20) | |
| 3 | 1.02 | (0.89, 1.18) | 1.01 | (0.86, 1.18) | 1.14 | (1.01, 1.29) | 1.05 | (0.95, 1.17) | 1.11 | (1.02, 1.22) | 1.07 | (0.98, 1.17) | |
| 2 | 0.87 | (0.75, 1.00) | 0.87 | (0.75, 1.02) | 0.96 | (0.85, 1.07) | 1.00 | (0.90, 1.10) | 1.04 | (0.94, 1.14) | 1.04 | (0.95, 1.14) | |
| 1 (lowest) | 0.52 | (0.45, 0.60) | 0.65 | (0.56, 0.76) | 0.88 | (0.78, 0.99) | 0.90 | (0.81, 0.99) | 1.03 | (0.95, 1.13) | 1.06 | (0.97, 1.15) | |
| MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | 1.1 | (0.0, 2.3) | −1.0 | (−2.0, 0.0) | 0.8 | (0.0, 1.6) | −0.7 | (−1.4, 0.0) | 0.9 | (0.4, 1.5) | 1.0 | (0.5, 1.5) | |
| 3 | 1.6 | (0.4, 2.7) | −1.9 | (−2.9, −0.9) | −0.5 | (−1.3, 0.3) | −0.1 | (−0.8, 0.6) | 1.1 | (0.6, 1.7) | 1.0 | (0.5, 1.5) | |
| 2 | −4.8 | (−5.9, −3.8) | −3.1 | (−4.1, −2.1) | −1.9 | (−2.7, −1.1) | −0.8 | (−1.5, −0.1) | 0.8 | (0.3, 1.4) | 1.2 | (0.7, 1.6) | |
| 1 (lowest) | −14.8 | (−15.8, −13.8) | −9.1 | (−10.0, −8.2) | −4.4 | (−5.1, −3.6) | −2.1 | (−2.8, −1.5) | 1.6 | (1.1,2.1) | 1.9 | (1.4, 2.3) | |
| White | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | 1.3 | (0.1, 2.5) | −1.2 | (−2.2, −0.1) | 0.7 | (−0.2, 1.5) | −1.0 | (−1.8, −0.3) | 0.5 | (−0.1, 1.1) | 0.6 | (0.1, 1.1) | |
| 3 | 1.7 | (0.5, 2.9) | −2.1 | (−3.2, −1.1) | −1.0 | (−1.8, −0.1) | −0.9 | (−1.6, −0.2) | 0.4 | (−0.2, 1.0) | 0.4 | (0.0, 0.9) | |
| 2 | −4.8 | (−5.9, −3.7) | −3.1 | (−4.2, −2.1) | −2.2 | (−3.0, −1.4) | −1.4 | (−2.1, −0.7) | 0.5 | (−0.1, 1.1) | 0.7 | (0.2, 1.2) | |
| 1 (lowest) | −14.4 | (−15.4, −13.3) | −8.9 | (−9.8, −7.9) | −4.7 | (−5.5, −3.9) | −2.6 | (−3.3, −1.9) | 0.9 | (0.4, 1.5) | 1.2 | (0.7, 1.7) | |
| Black | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | −2.5 | (−7.0, 1.9) | −0.6 | (−5.4, 4.3) | 1.1 | (−2.4, 4.6) | 0.3 | (−2.9, 3.6) | 3.4 | (0.7, 6.1) | 2.1 | (−0.2, 4.3) | |
| 3 | 0.7 | (−3.4, 4.8) | 0.3 | (−4.6, 5.3) | 4.1 | (0.2, 7.9) | 1.7 | (−1.5, 4.9) | 3.0 | (0.5, 5.4) | 1.6 | (−0.5, 3.7) | |
| 2 | −3.9 | (−7.8, 0.1) | −4.0 | (−8.6, 0.7) | −1.3 | (−4.7, 2.1) | −0.1 | (−3.3, 3.0) | 1.0 | (−1.6, 3.5) | 1.0 | (−1.1,3.1) | |
| 1 (lowest) | −13.9 | (−17.4, −10.3) | −10.9 | (−15.4, −6.5) | −3.5 | (−6.7, −0.3) | −3.1 | (−6.1, −0.1) | 0.9 | (−1.5, 3.2) | 1.4 | (−0.6, 3.4) |
| Referent | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Total, Q5 | −11.9% | (−14.1%, −9.7%) | −11.2% | (−13.4%, −8.9%) | −4.8% | (−6.8%, −2.9%) | −3.3% | (−5.1%, −1.5%) | 4.8% | (3.0%, 6.5%) | 6.8% | (5.0%, 8.5%) |
| White | White, Q5 | −10.8% | (−13.0%, −8.6%) | −11.0% | (−13.3%, −8.7%) | −5.7% | (−7.7%, −3.7%) | −5.3% | (−7.2%, −3.4%) | 2.6% | (0.7%, 4.4%) | 4.3% | (2.4%, 6.3%) |
| Black | White, Q5 | −34.9% | (−40.8%, −28.9%) | −15.8% | (−20.4%, −11.1%) | 0.4% | (−3.1%, 3.9%) | 18.4% | (15.7%, 21.0%) | 31.4% | (29.2%, 33.6%) | 35.1% | (33.0%, 37.2%) |
| Population | County income quintile | Year |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1960 |
1970 |
1980 |
1990 |
2000 |
2006 |
||||||||
| MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | ||
| (e) Breast cancer mortality rate | |||||||||||||
| Total | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 0.99 | (0.95, 1.03) | 0.96 | (0.92, 0.99) | 0.98 | (0.95, 1.01) | 0.98 | (0.95, 1.01) | 1.02 | (0.99, 1.05) | 1.00 | (0.97, 1.03) | |
| 3 | 1.04 | (1.00, 1.08) | 0.92 | (0.88, 0.95) | 0.93 | (0.90, 0.96) | 1.00 | (0.97, 1.03) | 1.01 | (0.98, 1.05) | 0.99 | (0.96, 1.02) | |
| 2 | 0.86 | (0.82, 0.90) | 0.87 | (0.84, 0.91) | 0.87 | (0.84, 0.90) | 0.95 | (0.92, 0.98) | 0.96 | (0.93, 0.99) | 1.02 | (0.99, 1.05) | |
| 1 (lowest) | 0.62 | (0.59, 0.64) | 0.72 | (0.70, 0.75) | 0.78 | (0.75, 0.80) | 0.88 | (0.85, 0.91) | 0.98 | (0.95, 1.01) | 0.99 | (0.96, 1.02) | |
| White | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 0.99 | (0.95, 1.04) | 0.96 | (0.92, 0.99) | 0.96 | (0.93, 1.00) | 0.96 | (0.93, 0.99) | 0.98 | (0.95, 1.01) | 0.98 | (0.94, 1.01) | |
| 3 | 1.03 | (0.99, 1.07) | 0.91 | (0.88, 0.95) | 0.92 | (0.89, 0.95) | 0.97 | (0.94, 1.01) | 0.98 | (0.95, 1.01) | 0.95 | (0.92, 0.98) | |
| 2 | 0.85 | (0.81, 0.89) | 0.87 | (0.83, 0.90) | 0.85 | (0.82, 0.88) | 0.91 | (0.88, 0.94) | 0.93 | (0.90, 0.96) | 0.98 | (0.94, 1.01) | |
| 1 (lowest) | 0.61 | (0.58, 0.64) | 0.72 | (0.69, 0.75) | 0.76 | (0.74, 0.79) | 0.85 | (0.82, 0.87) | 0.92 | (0.89, 0.95) | 0.95 | (0.91, 0.98) | |
| Black | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 0.91 | (0.75, 1.11) | 0.99 | (0.82, 1.19) | 1.12 | (0.98, 1.29) | 1.16 | (1.03, 1.30) | 1.12 | (1.01, 1.24) | 1.00 | (0.90, 1.10) | |
| 3 | 1.14 | (0.96, 1.35) | 1.02 | (0.85, 1.23) | 1.01 | (0.87, 1.17) | 1.11 | (0.99, 1.24) | 1.01 | (0.92, 1.11) | 1.04 | (0.95, 1.14) | |
| 2 | 0.96 | (0.81, 1.14) | 0.95 | (0.79, 1.13) | 1.06 | (0.93, 1.21) | 1.13 | (1.01, 1.27) | 1.01 | (0.91, 1.12) | 1.05 | (0.96, 1.16) | |
| 1 (lowest) | 0.71 | (0.60, 0.84) | 0.82 | (0.68, 0.97) | 0.85 | (0.75, 0.97) | 1.00 | (0.90, 1.12) | 1.01 | (0.92, 1.11) | 1.02 | (0.93, 1.12) | |
| MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | −0.3 | (−1.7, 1.1) | −1.5 | (−2.8, −0.2) | −0.7 | (−1.9, 0.4) | −0.7 | (−1.8, 0.3) | 0.4 | (−0.4, 1.3) | 0.0 | (−0.7, 0.8) | |
| 3 | 1.3 | (−0.2, 2.7) | −3.0 | (−4.3, −1.7) | −2.4 | (−3.5, −1.3) | 0.1 | (−1.0, 1.1) | 0.4 | (−0.4, 1.2) | −0.2 | (−0.9, 0.5) | |
| 2 | −5.0 | (−6.4, −3.6) | −4.6 | (−5.9, −3.3) | −4.4 | (−5.6, −3.3) | −1.8 | (−2.8, −0.7) | −1.0 | (−1.9, −0.2) | 0.4 | (−0.3, 1.2) | |
| 1 (lowest) | −13.6 | (−14.9, −12.3) | −10.0 | (−11.3, −8.8) | −7.8 | (−8.9, −6.7) | −4.2 | (−5.2, −3.2) | −0.6 | (−1.4, 0.2) | −0.2 | (−0.9, 0.5) | |
| White | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | −0.2 | (−1.7, 1.3) | −1.6 | (−2.9, −0.2) | −1.3 | (−2.5, −0.1) | −1.4 | (−2.5, −0.3) | −0.6 | (−1.5, 0.4) | −0.5 | (−1.3, 0.3) | |
| 3 | 1.1 | (−0.4, 2.6) | −3.3 | (−4.6, −1.9) | −2.8 | (−4.0, −1.6) | −0.9 | (−2.0, 0.2) | −0.5 | (−1.4, 0.3) | −1.2 | (−2.0, −0.4) | |
| 2 | −5.3 | (−6.7, −3.9) | −4.9 | (−6.2, −3.5) | −5.5 | (−6.6, −4.3) | −3.1 | (−4.2, −2.1) | −1.9 | (−2.8, −1.0) | −0.6 | (−1.3, 0.2) | |
| 1 (lowest) | −13.9 | (−15.3, −12.6) | −10.4 | (−11.7, −9.2) | −8.4 | (−9.6, −7.3) | −5.4 | (−6.5, −4.4) | −2.1 | (−3.0, −1.2) | −1.3 | (−2.1, −0.5) | |
| Black | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | −2.6 | (−8.3, 3.0) | −0.4 | (−6.1, 5.4) | 3.9 | (−0.5, 8.4) | 5.5 | (1.2, 9.7) | 4.1 | (0.4, 7.7) | −0.2 | (−3.3, 2.9) | |
| 3 | 4.1 | (−1.3, 9.5) | 0.7 | (−5.1, 6.6) | 0.2 | (−4.6, 4.9) | 3.8 | (−0.3, 7.8) | 0.3 | (−3.0, 3.6) | 1.3 | (−1.6, 4.2) | |
| 2 | −1.2 | (−6.3, 4.0) | −1.6 | (−7.2, 4.0) | 1.8 | (−2.5, 6.2) | 4.7 | (0.6, 8.8) | 0.4 | (−3.1, 3.9) | 1.7 | (−1.3, 4.7) | |
| 1 (lowest) | −8.7 | (−13.3, −4.0) | −5.8 | (−11.2, −0.4) | −4.7 | (−8.7, −0.6) | 0.2 | (−3.8, 4.1) | 0.3 | (−2.9, 3.5) | 0.7 | (−2.1, 3.5) |
| Referent | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Total, Q5 | −10.3% | (−13.0%, −7.6%) | −12.8% | (−15.6%, −10.1%) | −10.1% | (−12.4%, −7.8%) | −4.8% | (−6.9%, −2.8%) | −0.7% | (−2.7%, 1.3%) | −0.2% | (−2.3%, 1.8%) |
| White | White, Q5 | −10.4% | (−13.2%, −7.7%) | −13.0% | (−15.8%, −10.2%) | −11.3% | (−13.7%, −8.9%) | −7.3% | (−9.5%, −5.2%) | −3.9% | (−6.0%, −1.7%) | −3.4% | (−5.6%, −1.1%) |
| Black | White, Q5 | −21.3% | (−27.7%, −14.8%) | −24.9% | (−31.0%, −18.8%) | −12.7% | (−17.4%, −7.9%) | 6.9% | (3.5%, 10.2%) | 21.9% | (19.2%, 24.7%) | 26.1% | (23.5%, 28.8%) |
| Population | County income quintile | Year |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1960 |
1970 |
1980 |
1990 |
2000 |
2006 |
||||||||
| MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | ||
| (f) Cervical cancer mortality rate | |||||||||||||
| Total | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 1.21 | (1.12, 1.30) | 1.35 | (1.23, 1.47) | 1.26 | (1.14, 1.39) | 1.30 | (1.18, 1.44) | 1.33 | (1.19, 1.49) | 1.32 | (1.18, 1.48) | |
| 3 | 1.20 | (1.12, 1.29) | 1.33 | (1.21, 1.45) | 1.26 | (1.14, 1.40) | 1.33 | (1.20, 1.47) | 1.49 | (1.34, 1.66) | 1.50 | (1.34, 1.68) | |
| 2 | 1.38 | (1.28, 1.48) | 1.54 | (1.41, 1.68) | 1.53 | (1.39, 1.69) | 1.38 | (1.25, 1.53) | 1.52 | (1.36, 1.69) | 1.58 | (1.42, 1.77) | |
| 1 (lowest) | 1.25 | (1.16, 1.35) | 1.77 | (1.62, 1.93) | 1.61 | (1.47, 1.78) | 1.57 | (1.42, 1.73) | 1.92 | (1.74, ,2.13) | 2.08 | (1.88, 2.32) | |
| White | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 1.22 | (1.13, 1.33) | 1.34 | (1.21, 1.48) | 1.20 | (1.07, 1.35) | 1.26 | (1.12, 1.41) | 1.28 | (1.13, 1.45) | 1.34 | (1.18, 1.53) | |
| 3 | 1.19 | (1.10, 1.29) | 1.32 | (1.19, 1.46) | 1.23 | (1.10, 1.38) | 1.22 | (1.09, 1.37) | 1.43 | (1.26, 1.61) | 1.44 | (1.27, 1.64) | |
| 2 | 1.32 | (1.22, 1.43) | 1.48 | (1.34, 1.63) | 1.41 | (1.27, 1.58) | 1.25 | (1.12, 1.39) | 1.50 | (1.33, 1.69) | 1.61 | (1.42, 1.82) | |
| 1 (lowest) | 1.16 | (1.07, 1.26) | 1.60 | (1.46, 1.77) | 1.45 | (1.30, 1.62) | 1.42 | (1.28, 1.59) | 1.82 | (1.62, 2.05) | 2.08 | (1.85, 2.35) | |
| Black | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 1.16 | (0.94, 1.43) | 0.86 | (0.67, 1.11) | 1.05 | (0.81, 1.35) | 1.28 | (0.96, 1.70) | 1.27 | (0.95, 1.70) | 1.37 | (1.01, 1.87) | |
| 3 | 1.00 | (0.83, 1.21) | 0.93 | (0.72, 1.20) | 1.23 | (0.94, 1.60) | 1.38 | (1.05, 1.81) | 1.43 | (1.09, 1.88) | 1.58 | (1.19, 2.10) | |
| 2 | 1.31 | (1.09, 1.58) | 1.02 | (0.80, 1.30) | 1.28 | (1.01, 1.63) | 1.60 | (1.22, 2.10) | 1.45 | (1.09, 1.93) | 1.48 | (1.10, 1.98) | |
| 1 (lowest) | 1.03 | (0.86, 1.23) | 1.18 | (0.94, 1.49) | 1.28 | (1.01, 1.62) | 1.64 | (1.25, 2.14) | 1.76 | (1.36, 2.29) | 1.93 | (1.47, 2.54) | |
| MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | 1.9 | (1.2, 2.6) | 1.8 | (1.2, 2.3) | 0.9 | (0.5, 1.2) | 0.8 | (0.5, 1.2) | 0.6 | (0.4, 0.9) | 0.5 | (0.3, 0.7) | |
| 3 | 1.8 | (1.1, 2.5) | 1.7 | (1.1, 2.2) | 0.9 | (0.5, 1.3) | 0.9 | (0.6, 1.2) | 0.9 | (0.7, 1.2) | 0.8 | (0.6, 1.0) | |
| 2 | 3.4 | (2.7, 4.2) | 2.7 | (2.2, 3.3) | 1.8 | (1.4, 2.2) | 1.1 | (0.7, 1.4) | 1.0 | (0.7, 1.2) | 0.9 | (0.7, 1.2) | |
| 1 (lowest) | 2.3 | (1.6, 3.0) | 3.9 | (3.3, 4.5) | 2.0 | (1.6, 2.4) | 1.6 | (1.2, 1.9) | 1.8 | (1.5, 2.0) | 1.8 | (1.5, 2.0) | |
| White | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | 1.9 | (1.1, 2.6) | 1.6 | (1.0, 2.1) | 0.6 | (0.2, 1.0) | 0.7 | (0.3, 1.0) | 0.5 | (0.2, 0.7) | 0.5 | (0.3, 0.7) | |
| 3 | 1.6 | (0.9, 2.3) | 1.5 | (0.9, 2.0) | 0.7 | (0.3, 1.1) | 0.6 | (0.3, 0.9) | 0.8 | (0.5, 1.0) | 0.7 | (0.4, 0.9) | |
| 2 | 2.7 | (1.9, 3.4) | 2.2 | (1.6, 2.7) | 1.2 | (0.9, 1.6) | 0.6 | (0.3, 1.0) | 0.9 | (0.6, 1.1) | 0.9 | (0.7, 1.1) | |
| 1 (lowest) | 1.3 | (0.6, 2.1) | 2.8 | (2.2, 3.3) | 1.4 | (1.0, 1.7) | 1.1 | (0.8, 1.4) | 1.5 | (1.2, 1.7) | 1.6 | (1.3, 1.9) | |
| Black | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | 3.3 | (−1.5, 8.1) | −2.3 | (−6.3, 1.7) | 0.4 | (−1.9, 2.8) | 1.5 | (−0.2, 3.2) | 1.0 | (−0.2, 2.2) | 1.0 | (0.0, 2.0) | |
| 3 | 0.0 | (−4.0, 4.0) | −1.2 | (−5.3, 2.9) | 2.0 | (−0.6, 4.6) | 2.1 | (0.4, 3.7) | 1.6 | (0.5, 2.8) | 1.6 | (0.7, 2.5) | |
| 2 | 6.6 | (2.3, 10.9) | 0.4 | (−3.6, 4.4) | 2.6 | (0.2, 4.9) | 3.3 | (1.6, 5.0) | 1.7 | (0.5, 2.9) | 1.3 | (0.4, 2.3) | |
| 1 (lowest) | 0.6 | (−3.1, 4.4) | 3.0 | (−0.9, 7.0) | 2.5 | (0.3, 4.8) | 3.5 | (1.8, 5.2) | 2.9 | (1.7, 4.0) | 2.6 | (1.7, 3.5) |
| Referent | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Total, Q5 | 17.1% | (13.1%, 21.1%) | 28.4% | (23.7%, 33.1%) | 25.1% | (19.9%, 30.4%) | 24.6% | (19.3%, 29.8%) | 31.4% | (26.2%, 36.7%) | 33.5% | (28.2%, 38.8%) |
| White | White, Q5 | 15.0% | (10.6%, 19.5%) | 25.9% | (20.6%, 31.2%) | 20.1% | (14.0%, 26.2%) | 18.7% | (12.5%, 24.8%) | 28.4% | (22.2%, 34.5%) | 32.0% | (25.8%, 38.1%) |
| Black | White, Q5 | 65.4% | (62.9%, 68.0%) | 72.6% | (70.1%, 75.2%) | 71.7% | (68.8%, 74.6%) | 66.1% | (62.6%, 69.6%) | 66.9% | (63.1%, 70.6%) | 64.4% | (60.2%, 68.7%) |
| Population | County income quintile | Year |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1960 |
1970 |
1980 |
1990 |
2000 |
2006 |
||||||||
| MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | MRR | (95% CI) | ||
| (g) Stomach cancer mortality rate | |||||||||||||
| Total | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 0.96 | (0.92, 1.01) | 1.05 | (0.99, 1.10) | 1.05 | (0.99, 1.11) | 1.01 | (0.95, 1.06) | 0.99 | (0.93, 1.05) | 0.98 | (0.92, 1.04) | |
| 3 | 0.99 | (0.94, 1.03) | 0.88 | (0.83, 0.93) | 0.86 | (0.82, 0.91) | 0.95 | (0.90, 1.01) | 1.00 | (0.94, 1.05) | 0.93 | (0.87, 0.99) | |
| 2 | 0.87 | (0.83, 0.92) | 0.94 | (0.89, 0.99) | 0.90 | (0.86, 0.95) | 0.92 | (0.87, 0.97) | 1.01 | (0.96, 1.07) | 0.97 | (0.91, 1.03) | |
| 1 (lowest) | 0.76 | (0.73, 0.80) | 0.88 | (0.83, 0.92) | 0.86 | (0.82, 0.91) | 0.87 | (0.83, 0.92) | 1.09 | (1.03, 1.15) | 1.15 | (1.08, 1.22) | |
| White | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 0.96 | (0.92, 1.01) | 1.04 | (0.98, 1.10) | 1.03 | (0.97, 1.09) | 0.98 | (0.92, 1.04) | 0.97 | (0.91, 1.04) | 0.94 | (0.87, 1.00) | |
| 3 | 0.98 | (0.93, 1.03) | 0.86 | (0.81, 0.91) | 0.87 | (0.82, 0.93) | 0.91 | (0.86, 0.97) | 0.95 | (0.89, 1.01) | 0.88 | (0.82, 0.95) | |
| 2 | 0.86 | (0.82, 0.91) | 0.90 | (0.85, 0.96) | 0.87 | (0.82, 0.92) | 0.89 | (0.84, 0.94) | 0.97 | (0.91, 1.04) | 0.96 | (0.90, 1.03) | |
| 1 (lowest) | 0.73 | (0.70, 0.77) | 0.84 | (0.79, 0.89) | 0.82 | (0.77, 0.87) | 0.83 | (0.78, 0.88) | 1.03 | (0.97, 1.10) | 1.10 | (1.03, 1.17) | |
| Black | 5 (highest) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| 4 | 0.93 | (0.78, 1.10) | 0.97 | (0.79, 1.19) | 1.03 | (0.86, 1.24) | 1.03 | (0.86, 1.23) | 1.01 | (0.84, 1.21) | 1.03 | (0.86, 1.23) | |
| 3 | 0.90 | (0.77, 1.05) | 0.94 | (0.76, 1.17) | 0.84 | (0.69, 1.02) | 1.05 | (0.88, 1.24) | 1.16 | (0.98, 1.36) | 1.06 | (0.90, 1.25) | |
| 2 | 0.82 | (0.70, 0.95) | 1.02 | (0.83, 1.26) | 0.98 | (0.82, 1.17) | 1.09 | (0.92, 1.29) | 1.19 | (1.01, 1.42) | 0.96 | (0.81, 1.14) | |
| 1 (lowest) | 0.68 | (0.59, 0.78) | 0.88 | (0.72, 1.07) | 0.90 | (0.76, 1.06) | 1.01 | (0.86, 1.20) | 1.20 | (1.03, 1.41) | 1.06 | (0.90, 1.24) | |
| MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | MRD | (95% CI) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | −0.7 | (−1.5, 0.1) | 0.5 | (−0.1, 1.1) | 0.4 | (0.0, 0.8) | 0.0 | (−0.3, 0.4) | −0.1 | (−0.3, 0.2) | −0.1 | (−0.3, 0.1) | |
| 3 | −0.2 | (−1.0, 0.6) | −1.3 | (−1.9, −0.8) | −1.1 | (−1.5, −0.7) | −0.3 | (−0.6, 0.0) | 0.0 | (−0.3, 0.2) | −0.3 | (−0.5, 0.0) | |
| 2 | −2.2 | (−3.0, −1.4) | −0.7 | (−1.3, −0.1) | −0.8 | (−1.2, −0.4) | −0.5 | (−0.9, −0.2) | 0.1 | (−0.2, 0.3) | −0.1 | (−0.3, 0.1) | |
| 1 (lowest) | −4.2 | (−4.9, −3.5) | −1.3 | (−1.9, −0.8) | −1.1 | (−1.5, −0.7) | −0.8 | (−1.1, −0.5) | 0.4 | (0.1, 0.6) | 0.5 | (0.3, 0.8) | |
| White | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | −0.6 | (−1.4, 0.2) | 0.4 | (−0.2, 1.0) | 0.2 | (−0.2, 0.6) | −0.1 | (−0.5, 0.2) | −0.1 | (−0.4, 0.2) | −0.2 | (−0.4, 0.0) | |
| 3 | −0.3 | (−1.1, 0.5) | −1.5 | (−2.1, −0.9) | −0.9 | (−1.4, −0.5) | −0.5 | (−0.9, −0.2) | −0.2 | (−0.5, 0.0) | −0.4 | (−0.6, −0.2) | |
| 2 | −2.4 | (−3.1, −1.6) | −1.0 | (−1.6, −0.4) | −1.0 | (−1.4, −0.6) | −0.7 | (−1.0, −0.4) | −0.1 | (−0.4, 0.2) | −0.1 | (−0.3, 0.1) | |
| 1 (lowest) | −4.5 | (−5.3, −3.8) | −1.7 | (−2.3, −1.1) | −1.3 | (−1.7, −0.9) | −1.0 | (−1.3, −0.7) | 0.1 | (−0.1, 0.4) | 0.3 | (0.1, 0.5) | |
| Black | 5 (highest) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||||||
| 4 | −1.9 | (−6.5, 2.6) | −0.6 | (−4.1, 3.0) | 0.4 | (−1.9, 2.8) | 0.3 | (−1.7, 2.3) | 0.1 | (−1.3, 1.5) | 0.2 | (−1.0, 1.4) | |
| 3 | −2.8 | (−6.8, 1.2) | −1.0 | (−4.6, 2.6) | −2.1 | (−4.5, 0.3) | 0.5 | (−1.4, 2.4) | 1.2 | (−0.1, 2.6) | 0.4 | (−0.7, 1.5) | |
| 2 | −5.1 | (−8.9, −1.2) | 0.4 | (−3.1, 4.0) | −0.2 | (−2.5, 2.0) | 1.0 | (−0.9, 2.9) | 1.5 | (0.1, 3.0) | −0.3 | (−1.4, 0.9) | |
| 1 (lowest) | −8.8 | (−12.4, −5.2) | −2.1 | (−5.5, 1.2) | −1.3 | (−3.5, 0.8) | 0.2 | (−1.7, 2.0) | 1.6 | (0.3, 2.9) | 0.4 | (−0.7, 1.5) |
| Referent | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | PAF | (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Total, Q5 | −9.4% | (−12.4%, −6.4%) | −4.7% | (−8.4%, −1.0%) | −6.1% | (−9.8%, −2.4%) | −5.6% | (−9.2%, −1.9%) | 2.1% | (−1.6%, 5.7%) | 1.0% | (−2.9%, 4.9%) |
| White | White, Q5 | −11.0% | (−14.1%, −7.8%) | −7.3% | (−11.3%, −3.3%) | 64.4% | (−12.4%, −4.4%) | −9.1% | (−13.1%, −5.0%) | −1.5% | (−5.7%, 2.8%) | −2.6% | (−7.1%, 1.9%) |
| Black | White, Q5 | 32.4% | (29.1%, 35.8%) | 41.3% | (37.9%, 44.8%) | 41.2% | (37.7%, 44.7%) | 48.3% | (45.3%, 51.3%) | 54.9% | (52.1%, 57.7%) | 51.4% | (48.1%, 54.6%) |
Total cancer mortality (Fig. 2a, Table 2a)
From 1960 to about 1990, among both the white and black populations, the age-standardized total cancer mortality rate in the top four county income quintiles was fairly similar and rose slightly, with rates in each income quintile highest for blacks. After 1990, these rates declined, especially in the most affluent county income quintile (white 1991–2006 APC: −1.40, p < 0.05; black 1991–2006 APC: −1.80, p < 0.05). In both populations, rates in the lowest county income quintile were initially lowest, rose most quickly, and in the late 1980s crossed over and thereafter exceeded those of the highest income quintile, thereby producing a pattern (total, white, black) of shrinking, reversing, and rising inequities. Throughout, the black population experienced larger absolute, but similar relative, socioeconomic gaps in mortality, e.g., in 2006, comparing (within racial/ethnic group) the bottom four to the top county income quintiles, the absolute gaps among blacks (range: 17.1–23.7/100,000) were twice those among whites (range: 7.7–13.0/100,000), despite similar relative risks (range: 1.08–1.12 vs. 1.04–1.07). Their PAFs were also consistently higher (comparing both groups to whites in the highest income quintile): among whites, the PAF first rose above 0 in 1990 and in 2006 equaled 5.4% (95% CI 4.8, 6.0); among blacks, in 1960, it equaled 6.0% (95% CI 4.5, 7.4) and in 1990 reached 24.7% (95% CI 23.9, 25.5) and remained at this level through 2006.
Lung cancer mortality (Fig. 2b; Table 2b)
Fig. 2b.
lung cancer mortality
Lung cancer exhibited a similar pattern of shrinking, reversing, and rising inequities, reflecting its huge impact on overall cancer mortality. Among whites, the PAF thus increased from −5.7% (95% CI −8.0, −3.5) in 1960 to 14.0% (95% CI 13.0, 15.1) in 2006; among blacks, it rose from −3.1% (95% CI −7.4, 1.3) in 1960 to 19.5% (95% CI 17.6, 21.5) by 1990 and thereafter remained significantly between 20 and 25%.
Prostate cancer mortality (Fig. 2c; Table 2c)
Fig. 2c.
prostate cancer mortality
Among the white population, prostate cancer mortality rates increased across all county income quintiles from 1960 to about 1992, with rates marginally higher in the highest income county quintile and also, within income quintiles, below those of their black counterparts. Between 1992 and 1994, rates among the white population began declining in every income quintile (APC ranging from −3.7 to −4.1) and by 2006 were indistinguishable, with the PAF in 2006 equaling 0.0% (95% CI = −2.9, 2.8).
By contrast, among the black population, the socioeconomic inequities widened, then shrunk, and stagnated. Between the mid-1960s and mid-1990, rates in the four lowest income quintiles exceeded those in the highest quintile and rose most quickly in the lowest income quintile; thereafter, rates fell in all income quintiles (APC on the order of −4%), but rates in the lower income quintiles remained absolutely higher. Consequently, the absolute gap between the lowest and highest county income quintiles rose from effectively 0 for 1960–1990 (all 95% CI spanned 0) to 11.3/100,000 (95% CI 4.6, 18.0) in 2000, a gap equaling 50% of the white prostate mortality rate in 2006, a year the black PAF equaled 58.5% (95% CI 56.7, 60.2).
Colorectal cancer mortality (Fig. 2d; Table 2d)
Fig. 2d.
colorectal cancer mortality
Among both the white and black population, socioeconomic inequities in colorectal cancer mortality shrank (1960s to mid-1990s), reversed, and, after the mid-1990s, stagnated or widened. The white socioeconomic convergence in the mid-1990s, however,occurredin a context of lower—andmore steeply falling—mortality rates as compared to their black counterparts. Thus, among whites, the PAF reversed from −10.8% (95% CI −13.0, −8.6) in 1960 to 4.3% (95% CI 2.4, 6.3) in 2006; among blacks, it changed from −34.9% in 1960 (95% CI −40.8, −28.9) to 35.1% (95% CI 33.0, 37.2) in 2006.
Breast cancer mortality (women) (Fig. 2e; Table 2e)
Fig. 2e.
breast cancer mortality (women)
Among the white women, within the top four income quintiles, breast cancer mortality rates remained relatively stable until 1989–1990, with rates equally highest among the top two income quintiles; thereafter, mortality rates in all four income quintiles began to decline significantly by 2.6% per year. Among white women in the lowest income quintile, however, their initially much lower rates significantly increased by 2.3% per year until 1968, then increased more slowly but still significantly by 0.5% per year until 1992, and then declined by 1.9% per year—yielding a pattern of both stagnant and shrinking inequities. By 2006, mortality rates across income quintiles effectively converged, and the PAF rose from −10.4% (95% CI −13.2, −7.7) in 1960 to −3.4% (95% CI −5.6, −1.1) in 2006.
Among the black women, mortality rates among those in the top four income quintiles were similar and on par with the white rates until the mid-1980s, then rose above them, peaked in the early/mid-1990s, and declined thereafter. Rates among black women in the lowest county income quintile, initially lowest, rose most quickly and converged with those of black women in the higher income quintiles in the mid-1990s. The reversal in the black PAF thus exceeded that observed among the white women, shifting from −21.3% in 1960 (95% CI −27.7, −14.8) to 26.1% (95% CI 23.5, 28.8) in 2006.
Cervical cancer mortality (Fig. 2f; Table 2f)
Fig. 2f.
cervical cancer mortality
Among both white and black women, rates consistently declined in all county income quintiles and were consistently higher in the lowest quintiles. This decline slowed after the early 1980s, especially for those in the lower income quintiles, producing a pattern of stagnant and then widening socioeconomic inequities. Among white women, their PAF increased from 15.0% in 1960 (95% CI 10.6, 19.5) to 32.0% in 2006 (95% CI 25.8, 38.1%); among black women, their PAF remained high throughout the study period, on the order of 65–75%, and in 2006 equaled 64.4% (95% CI 60.2, 68.7).
Stomach cancer mortality (Fig. 2g; Table 2g)
Although stomach mortality rates were consistently higher among blacks vs whites within each income quintile, they initially were lowest, in each group, in the lowest county income quintile. In both groups, rates in every income quintile declined over time and converged, in the mid-1970s, among blacks, and in the mid-1990s among whites. The PAF in the white population thus rose from −11.0% in 1960 (95% CI −14.1, −7.8) to −2.6% in 2006 (95% CI −7.1, 1.9); in the black population, it rose from 32.4% (95% CI 29.1, 35.8) in 1960 to nearly 50% in 1990, peaking at 54.9% (95% CI 52.1, 57.7%) in 2000, and equaling 51.4% (95% CI 48.1, 54.6) in 2006.
Discussion
Our results refute the increasingly prominent hypothesis that socioeconomic inequities in cancer mortality are bound to rise [1–3], and instead extend evidence demonstrating that between 1960 and 2006, US socioeconomic inequities in cancer mortality variously shrunk, widened, reversed, and stagnated, depending on time period and cancer site. These patterns, moreover, differed by race/ethnicity. For all cancers combined and most, but not all, sites, larger absolute, but not relative, socioeconomic gaps in mortality occurred among the black compared to white population, e.g., in 2006, the absolute gaps, compared, respectively, to blacks and to whites in the most affluent county income quintile, were two time higher among blacks (range: 17.1–23.7/100,000) versus whites (range: 7.7–13.0/100,000), despite similar relative risks (range: 1.08–1.12 vs. 1.04–1.07). Consequently, had the white and black population in the lower four county income quintiles experienced the same yearly age-specific mortality rates as whites in the most affluent county income, the proportion of total cancer deaths that would not have occurred would have, respectively, equaled −4.1% (95% CI −4.9, −3.2) and 6.0% (95% CI 4.5, 7.4) in 1960 versus 5.4% (95% CI 4.8, 6.0) and 23.0% (95% CI 22.3, 23.8) in 2006. Additionally, whereas the PAF among the white population ranged in 1960 from around −10% for colorectal, breast, and stomach cancer up to 15% for cervical cancer versus in 2006 from close to 0% for breast, prostate, and stomach cancer to 32.0% for cervical cancer, among the black population it ranged, in 1960, from –34.9% for colorectal cancer to 65.4% for cervical cancer versus in 2006 from 23.4% for lung cancer to 64.4% for cervical cancer.
Study limitations
Before interpreting our results, several study limitations merit mention. At issue are (1) data quality (especially for death certificate data [11, 24], compounded by changes in coding of causes of death across IDC-7 through ICD-10 [13]) and (2) reliance on repeat cross-sectional county-level data (the only available nationally representative data for estimating US socioeconomic inequities in mortality preceding 1968 [2, 4, 11]). Their net impact, however, is likely to be small.
Of note, US death registration was 99% complete by 1960 [25], and any greater tendency to underestimate cause-specific death counts among the lower income and black populations would result in reducing, not inflating, the observed cause-specific socioeconomic inequities. Similarly, the census undercount, also disproportionately affecting lower income populations and populations of color, has declined substantially over time [26], further reducing, not inflating, the more recent estimates of cancer mortality inequities. Misclassification of “white” and “black” deaths in US mortality data has been shown to be minor [24], and the effect of having had to equate the “non-white” with black population for 1960–1967 is also likely small [18]. Moreover, suggesting our use of county-level data is not unduly biased by ecologic fallacy or population mobility, the direction and magnitude of our results are consistent with those of the one individual-level US study on long-term trends in socioeconomic inequalities in cancer mortality [6], and related research on long-term trends in socioeconomic disparities in US county-level life expectancy found that taking into account county migration data did not alter results [2].
Interpretation
As is well-recognized, cancer mortality rates—and their social inequalities—reflect the interplay of the social patterning of cancer incidence and survival rates [27]. Thus, any comprehensive interpretation, let alone analysis, of determinants of social inequities in cancer mortality would need to address, simultaneously, social inequities in both incidence and survival [9, 27]. The purpose of this study, however, was narrower, given our focus on testing hypotheses about long-term US socioeconomic trends in cancer mortality, all-site and site-specific, both overall and by race/ethnicity.
Three findings merit attention. First, our results of variously shrinking, widening, reversing, and stagnating socioeconomic inequities in cancer mortality rates are compatible with—and extend—those observed in the handful of other long-term analyses of total and site-specific cancer mortality in both the US [3–7] and other countries [1, 7, 8, 28, 29]. The chief exception concerns stomach cancer, for which mortality in both the US and Europe historically has been higher among more economically deprived groups [1, 27]. A new US study, however, has recently documented unexpectedly rising rates of stomach cancer incidence among young white adults, suggesting changes in stomach cancer incidence and mortality, including in relation to race/ethnicity and socioeconomic position, may be underway [30]. Likely, explanations for the changing trends in socioeconomic inequities in mortality observed for the other cancer sites, discussed in other literature, involve socioeconomic and racial/ethnic changes in the distribution of: smoking (relevant especially to lung cancer and also cervical and colorectal cancer) [2–6, 31–33]; age at first childbirth and use of hormone therapy (relevant to breast cancer) [34–37]; obesity, diet, and physical activity (relevant especially to breast and colorectal cancer) [2–6, 34, 35, 38, 39]; access and barriers to screening (relevant especially to prostate, breast, cervical, and colorectal cancer) [32–35, 38–41], and access and barriers to appropriate medical care and advances in treatment to reduce risk of mortality, once diagnosed (relevant especially to breast, cervical, and colorectal cancer) [32–35, 38, 39].
Second, our study newly documents long-term US racial/ethnic differences in trends in socioeconomic inequities in cancer mortality and provides novel evidence that for total cancer mortality and many, but not all, sites, larger absolute socioeconomic inequities existed among the black versus white population, despite similar relative gaps. This occurred because within each income quintile mortality rates were higher among the black compared to white populations, especially in the lower income quintiles, resulting also in larger PAFs. Of note, the findings of excess black compared to white mortality within specified socioeconomic strata is consistent with other research on the joint distribution of US socioeconomic and racial/ethnic health inequities [9, 18, 42, 43], which has documented these differentials for many, but not all, health outcomes. The two most prominent explanations are: (1) artefactual, due to residual socioeconomic confounding, and (b) substantive, due to differential adverse exposures at any given economic level [42–45]. For example, with regard to residual confounding, most studies (including ours, given data limitations) typically employ only one socioeconomic measure evaluated at one point in time, thereby incompletely capturing the many economic dimensions in which the US black population fares more poorly than the white population (e.g., lower wealth at a given income level, lower income return for education at a given educational level, and greater cumulative impoverishment across the life course and transgenerationally) [42–51]. Additional research, moreover, has documented that black compared to white Americans at any given economic level not only experience the adverse impact of institutional and interpersonal racial discrimination but also are likely to be more subject to adverse exogenous exposures (e.g., at work, in the neighborhood, at home) [42–50, 52, 53]. It accordingly should not be surprising that black/white differences persist within economic strata, even as controlling for socioeconomic position can reduce black/white health inequities [42–47].
Third, our results refute the hypothesis that, as population health improves, a widening of socioeconomic inequities in health, including for cancer mortality, is inevitable [1–3]. More broadly, our findings underscore that inferences based only on recent trends and that focus on socioeconomic position alone without also considering race/ethnicity, or address only specific sites, or examine only relative and not absolute gaps, are unlikely to provide an adequate basis for comprehending trends in overall cancer mortality, let alone the dynamics of social inequities in cancer mortality [9, 27]. Instead, as attested to by the mutability of the observed inequities, a long-term macroscopic perspective is essential—and clarifies that the currently high burdens of cancer mortality experienced especially by the US black population in low income counties, far from being inevitable, are inequities that need not, and should not, exist.
Supplementary Material
Acknowledgments
We thank Jacob Bor (doctoral student, Harvard School of Public Health) for his work, as a paid research assistant, in harmonizing the ICD codes used in these analyses (permission for this acknowledgment obtained in writing on October 5, 2010). This work was supported by the National Cancer Institute at the National Institutes of Health (grant 1R03CA137666). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. All authors had full access to all of the data in the study, and the corresponding author has final responsibility for the collective decision to submit for publication.
Abbreviations
- CDC
Centers for disease control and prevention
- CI
Confidence interval
- ICD
International classification of disease
- MRD
Mortality rate difference
- MRR
Mortality rate ratio
- NCHS
National center for health statistics
- PAF
Population attributable fraction
Footnotes
Electronic supplementary material The online version of this article (doi:10.1007/s10552-011-9879-4) contains supplementary material, which is available to authorized users.
References
- 1.Kunst AE, Looman CW, Mackenbach JP. Socio-economic mortality differences in The Netherlands in 1950–1984: a regional study of cause-specific mortality. Soc Sci Med. 1990;31:141–152. doi: 10.1016/0277-9536(90)90055-w. [DOI] [PubMed] [Google Scholar]
- 2.Ezzati M, Friedman AB, Kulkarni SC, Murray CJ. The reversal of fortunes: trends in county mortality and cross-county mortality disparities in the United States. PLoS Med. 2008;5:e66. doi: 10.1371/journal.pmed.0050066. Erratum (2008) in: PLoS Med 5(5) doi:10.1371/journal. pmed.0050119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kinsey T, Jemal A, Liff J, Ward E, Thun M. Secular trends in mortality from common cancers in the United States by educational attainment, 1993–2001. J Natl Cancer Inst. 2008;100:1003–1012. doi: 10.1093/jnci/djn207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh GK, Miller BA, Hankey BG, Feuer EJ, Pickle LW. Changing area socioeconomic patterns in US cancer mortality, 1950–1998: Part I—all cancers among men. J Natl Cancer Inst. 2002;94:904–915. doi: 10.1093/jnci/94.12.904. [DOI] [PubMed] [Google Scholar]
- 5.Singh GK, Miller BA, Hankey BF. Changing area socioeconomic patterns in US cancer mortality, 1950–1998: Part II–Lung and colorectal cancers. J Natl Cancer Inst. 2002;94:916–925. doi: 10.1093/jnci/94.12.916. [DOI] [PubMed] [Google Scholar]
- 6.Steenland K, Henley J, Thun M. All-cause and cause-specific death rates by educational status for two million people in two American Cancer Society cohorts, 1959–1996. Am J Epidemiol. 2002;156:11–21. doi: 10.1093/aje/kwf001. [DOI] [PubMed] [Google Scholar]
- 7.Strand BH, Grøholt EK, Steingr9imsdøtter OA, Blakely T, Graff-Iversen S, Naess Ø . Educational inequalities in mortality over four decades in Norway: prospective study of middle aged men and women followed for cause specific mortality, 1960–2000. BMJ. 2010;304:c654. doi: 10.1136/bmj.c654. doi:10.1136/bmj.c654. Erratum in: BMJ 2010; 340:c1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Logan WPD. Cancer mortality by occupation and social class. (Studies on medical and population subjects No. 44) Her Majesty's Stationery Office; International Agency for Research on Cancer; London: Lyon: 1982. [Google Scholar]
- 9.Krieger N. Epidemiology and the people's health: theory and context. Oxford University Press; New York: 2011. [Google Scholar]
- 10.National Office of Vital Statistics. Public Health Service. US Department of Health, Education and Welfare . Documentation of the Detail Mortality Tape File (1959–1961, 1962–1967) US Department of Health, Education, and Welfare; Washington, DC: 1969. [Google Scholar]
- 11.Krieger N, Rehkopf DH, Chen JT, Waterman PD, Marcelli E, Kennedy M. The fall and rise of US inequities in premature mortality: 1960–2002. PLoS Med. 2008;5(2):e46. doi: 10.1371/journal.pmed.0050046. doi:10.1371/journal. pmed.0050046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Center for Health Statistics [Accessed May 14, 2011];Compressed Mortality Files. 2011 http://www.cdc.gov/nchs/data_access/cmf.htm.
- 13.World Health Organization (WHO) International Classification of Diseases (ICD) [Accessed May 14, 2011];2011 http://www.who.int/classifications/icd/en/.
- 14.GeoLytics Census Reference Package. GeoLytics; New Brunswick, NJ: 2011. [Accessed May 14, 2011]. http://www.geolytics.com/USCensus,Census-Research-Package,Products.asp. [Google Scholar]
- 15.US Census [Accessed May 14, 2011];Historical income tables for counties. 2011 http://www.census.gov/hhes/www/income/data/historical/county/county2. html.
- 16.US Department of Labor, Bureau of Labor Statistics [Accessed May 14, 2011];Consumer Price Indexes. 2011 http://www.bls.gov/cpi/home.htm.
- 17.Mays VM, Ponce NA, Washington DL, Cochran SD. Classification of race and ethnicity: implications for public health. Annu Rev Public Health. 2003;24:83–110. doi: 10.1146/annurev.publhealth.24.100901.140927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kitagawa EM, Hauser PM. Differential mortality in the united states: a study in socioeconomic epidemiology. Harvard University Press; Cambridge: 1973. [Google Scholar]
- 19.SAS Institute . SAS 9/1/3: language reference dictionary Fifth Edition. SAS Institute; Cary, NC: 2002–2006. [Google Scholar]
- 20.Keppel K, Pamuk E, Lynch J, Carter-Pokras O, Kim I, Mays V, Pearcy J, Schoenbach V, Weissman JS. Methodological issues in measuring health disparities. Vital Health Stat. 2005;141:1–16. [PMC free article] [PubMed] [Google Scholar]
- 21.Greenland S, Drescher K. Maximum likelihood estimation of the attributable fraction from logistic models. Biometrics. 1993;49:865–872. [PubMed] [Google Scholar]
- 22.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 23.National Cancer Institute [Accessed May 14, 2011];Joinpoint regression program. (ver 3.0). 2005 Available http://surveillance.cancer.gov/joinpoint/.
- 24.Arias E, Schauman WS, Eschbach K, Sorlie PD, Backlund E. The validity of race and Hispanic origin reporting on death certificates in the United States. Vital Health Stat 2. 2008;148:1–23. [PubMed] [Google Scholar]
- 25.Hetzel AM. History and organization of the vital statistics system. National Center for Health Statistics; Bethesda: 1997. [Google Scholar]
- 26.Clark JR, Moul DA. Census 2000 testing, experimentation, and evaluation program topic report no. 10, TR-10, coverage and improvement in census 2000 enumeration. US Census Bureau; Washington: 2004. [Google Scholar]
- 27.Koh H, editor. Toward the elimination of cancer disparities: a clinical and public health perspective. Springer; New York: 2009. [Google Scholar]
- 28.Mackenbach JP, Bos V, Andersen O, Cardano M, Costa G, Harding S, Reid A, Hemström O, Valkonen T, Kunst AE. Widening socioeconomic inequalities in mortality in six Western European countries. Int J Epidemiol. 2003;32:830–837. doi: 10.1093/ije/dyg209. [DOI] [PubMed] [Google Scholar]
- 29.Fawcett J, Blakely T. Cancer is overtaking cardiovascular disease as the main driver of socioeconomic inequalities in mortality: New Zealand (1981–99) J Epidemiol Community Health. 2007;61:59–66. doi: 10.1136/jech.2005.044016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Anderson WF, Camargo MC, Fraumeni JF, Jr, Correa P, Rosen-berg PS, Rabkin CS. Age-specific trends in incidence of noncardia gastric cancer in US adults. JAMA. 2010;303:1723–1728. doi: 10.1001/jama.2010.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Koh HK, Lequra L, Short SM. Disparities in tobacco use and lung cancer. In: Koh H, editor. Toward the elimination of cancer disparities: a clinical and public health perspective. Springer; New York: 2009. pp. 109–136. [Google Scholar]
- 32.Newmann S, Garner E. Social inequities along the cervical cancer continuum: a structured review. Cancer Causes Control. 2005;16:63–70. doi: 10.1007/s10552-004-1290-y. [DOI] [PubMed] [Google Scholar]
- 33.del Carmen M, Diaz-Montez . Disparities and cervical cancer. In: H Koh., editor. Toward the elimination of cancer disparities: a clinical and public health perspective. Springer; New York: 2009. pp. 203–226. [Google Scholar]
- 34.Bigby J, Holmes M. Disparities across the breast cancer continuum. Cancer Causes Control. 2005;16:35–44. doi: 10.1007/s10552-004-1263-1. [DOI] [PubMed] [Google Scholar]
- 35.Wallington SF, Brawley OW, Holmes MD. Socioeconomic status and breast cancer disparities. In: Koh H, editor. Toward the elimination of cancer disparities: a clinical and public health perspective. Springer; New York: 2009. pp. 137–160. [Google Scholar]
- 36.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Yin R, Coull BA. Race/ethnicity and changing US socioeconomic gradients in breast cancer incidence: California and Massachusetts, 1978–2002. Cancer Causes Control. 2006;17:217–226. doi: 10.1007/s10552-005-0408-1. [DOI] [PubMed] [Google Scholar]
- 37.Krieger N, Chen JT, Waterman PD. Decline in US breast cancer rates after the women's health initiative: socioeconomic and racial/ethnic differentials. Am J Public Health. 2010;100:S132–S139. doi: 10.2105/AJPH.2009.181628. NIHMS # 171687. Erratum (2010): Am J Public Health 100: 972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Palmer RC, Schneider EC. Social disparities across the continuum of colorectal cancer: a systematic review. Cancer Causes Control. 2005;16:55–61. doi: 10.1007/s10552-004-1253-3. [DOI] [PubMed] [Google Scholar]
- 39.Schneider EC. Disparities and colorectal cancer. In: Koh H, editor. Toward the elimination of cancer disparities: a clinical and public health perspective. Springer; New York: 2009. pp. 161–178. [Google Scholar]
- 40.Gilligan T. Social disparities and prostate cancer: mapping the gaps in our knowledge. Cancer Causes Control. 2005;16:45–53. doi: 10.1007/s10552-004-1291-x. [DOI] [PubMed] [Google Scholar]
- 41.Brawley OW, Wallington WF. Disparities in prostate cancer. In: Koh H, editor. Toward the elimination of cancer disparities: a clinical and public health perspective. Springer; New York: 2009. pp. 179–202. [Google Scholar]
- 42.Kington RS, Nickens HW. Racial and ethnic difference in health: recent trends, current patterns, future directions. In: Smelser NJ, Wilson WJ, Mitchell F, editors. America becoming: racial trends and their consequences. vol 2. National Academy Press; Washington: 2001. pp. 253–310. [Google Scholar]
- 43.Williams DR. The health of US racial and ethnic populations. J Gerontol Ser B. 2005;60B(Special Issue II):53–62. doi: 10.1093/geronb/60.special_issue_2.s53. [DOI] [PubMed] [Google Scholar]
- 44.Krieger N. Defining and investigating social disparities in cancer: critical issues. Cancer Causes Control. 2005;16:5–14. doi: 10.1007/s10552-004-1251-5. [DOI] [PubMed] [Google Scholar]
- 45.Freeman HP. Poverty, culture, and social injustice: determinants of cancer disparities. CA Cancer J Clin. 2004;54:72–77. doi: 10.3322/canjclin.54.2.72. [DOI] [PubMed] [Google Scholar]
- 46.Krieger N. Discrimination and health. In: Berkman L, Kawachi I, editors. Social epidemiology. Oxford University Press; New York: 2000. pp. 36–75. [Google Scholar]
- 47.Krieger N, Williams D, Moss N. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–378. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- 48.Lynch J, Kaplan G. Socioeconomic position. In: Berkman L, Kawachi I, editors. Social Epidemiology. Oxford University Press; New York: 2000. pp. 13–35. [Google Scholar]
- 49.Fairclough A. Better day coming: blacks and equality, 1890–2000. Viking; New York: 2001. [Google Scholar]
- 50.Smelser NJ, Wilson WJ, Mitchell F, editors. National Research Council, Commission on Behavioral and Social Sciences and Education. Volumes I and II. National Academy Press; Washington, DC: 2001. America becoming: racial trends and their consequences. [Google Scholar]
- 51.Scholz JK, Levine K. US Black-white wealth inequality. In: Neckerman KM, editor. Social inequality. Russell Sage; New York: 2004. pp. 524–544. [Google Scholar]
- 52.Krieger N, Emmons K, Williams D. Defining, investigating, and addressing cancer inequities: critical issues. In: Koh H, editor. Toward the elimination of cancer disparities: a clinical and public health perspective. Springer; New York: 2009. pp. 3–28. [Google Scholar]
- 53.Sorensen G, Sembajwe G, Harley A, Quintiliani L. Work and occupation: important indicators of socioeconomic position and life experiences influencing cancer disparities. In: Koh H, editor. Toward the elimination of cancer disparities: a clinical and public health perspective. Springer; New York: 2009. pp. 29–48. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.