Abstract
Central Appalachian residents suffer disproportionate health disparities, including an all-cancer mortality rate 17% higher than the general population. During 10 focus groups and 19 key informant interviews, 91 Appalachian residents identified cancer screening challenges and strategies. Challenges included: (1) inadequate awareness of screening need; (2) insufficient access to screening; and (3) lack of privacy. Strategies included (1) witnessing/storytelling; (2) capitalizing on family history; (3) improving publicity about screening resources; (4) relying on lay health advisors; and (5) bundling preventive services. These insights shaped our CBPR intervention and offer strategies to others working in Appalachia, rural locales, and other traditionally underserved communities.
Keywords: Cancer screening, Community-based participatory research, Rural health, qualitative research
Introduction
Residents of central Appalachia (typically considered to be comprised of West Virginia, eastern Tennessee, and eastern Kentucky) suffer some of the nation's worst health profiles. As highlighted in Table 1, the cervical and colorectal cancer incidence rates for Appalachian Kentucky are 11.1 and 59.8 per 100,000 compared with the national rates of 8.1 and 48.8 per 100,000. These cancer incidence rates are 37% and 22% higher, respectively, than national rates reported through the Surveillance Epidemiology and End Results (SEER) survey.1,2 Although breast cancer incidence rates are lower among Appalachian Kentuckians compared to women both in non-Appalachian Kentucky and in the general U.S. population, breast cancer mortality rates are slightly higher among Appalachian Kentuckians than state and national samples. Furthermore, Appalachian Kentucky's all-cancer mortality rate is 17% higher than the nation as a whole.3 These elevated rates of cancer and cancer-related mortality motivated the National Cancer Institute to recognize Appalachians as a special population with severe cancer disparities.4 In order to reduce these disparities, researchers must pinpoint, from the community's perspective, challenges to and strategies for cancer prevention. Therefore, the purpose of this study was to identify such community perspectives.
Table 1.
| Cancer incidence rates | ||||||||
|---|---|---|---|---|---|---|---|---|
| All Cancers | Colorectal | |||||||
| Total | Male | Female | Total | Male | Female | Cervix | Breast | |
| US | 464.5 | 543.6 | 409.0 | 48.8 | 57.0 | 42.4 | 8.1 | 120.6 |
| Kentucky | 508.9 | 600.8 | 447.0 | 57.0 | 67.6 | 48.9 | 9.2 | 120.1 |
| Appalachian KY | 517.5 | 613.8 | 451.5 | 59.8 | 69.7 | 52.3 | 11.1 | 112.2 |
| Cancer mortality rates | ||||||||
|---|---|---|---|---|---|---|---|---|
| All Cancers | Colorectal | |||||||
| Total | Male | Female | Total | Male | Female | Cervix | Breast | |
| US | 183.8 | 225.4 | 155.4 | 17.6 | 21.2 | 14.9 | 2.4 | 24.0 |
| Kentucky | 216.5 | 275.0 | 177.6 | 20.8 | 25.2 | 17.6 | 2.9 | 24.2 |
| Appalachian KY | 235.0 | 300.5 | 189.3 | 22.2 | 26.5 | 19.0 | 3.1 | 26.4 |
Rates are per 100,000 population and age-adjusted to the 2000 US standard population.
Various approaches have been used to prevent or address cancer inequities, the most promising of which is increasing early detection through screening.5 Unfortunately, many Appalachian residents do not obtain cancer screening as recommended. For example, as shown in Table 2, Behavioral Risk Factor Surveillance System data indicate that approximately 36% of respondents in Appalachian Kentucky reported screening for colorectal cancer (CRC) in accordance with the guidelines of the U.S. Preventive Services Task Force, compared to 44% in Kentucky and 53% nationwide.6 Although rural Appalachian women have made progress in receiving preventive screenings over the past five decades, they still lag behind their urban and non-Appalachian counterparts. For example, both breast and cervical cancer screening rates among Appalachian women fell well below the Healthy People 2010 goals.
Table 2.
CRC, cervical cancer, and breast cancer screening, BRFSS, 1999–2000.6
| FOBT,FS, or colonoscopy as recommended | Ever Had Pap | Never/+> 3 yr | Mammogram/CBE as recommended | |||
|---|---|---|---|---|---|---|
| Ever had Pap | Pap in last 3 yr | Pap >3 yrs | ||||
| US | 53.1% | 94.8% | 87.4% | 11.4% | 16.6% | 71.2% |
| Kentucky | 43.5% | 92.6% | 87.3% | 11.8% | 19.2% | 70.2% |
| Appalachian KY | 36.3% | 90.8% | 84.5% | 14.8% | 24.0% | 59.4–62.7% |
There are many reasons for low cancer screening rates in Appalachian Kentucky. Lack of access to health care, limited financial resources, and modest educational levels are barriers to obtaining cancer screening and contribute to the dramatic cancer inequities in the region.7 To address the suboptimal rates of cancer screening among traditionally underserved populations, researchers have employed cancer screening interventions and programs targeting individuals, providers, or the health care systems.8,9 Various theoretical perspectives have informed these interventions, including the health belief and stages-of-change models, social learning, reasoned action, and socioecological theories. However, scant research exists on Appalachian residents' perspectives on strategies to address these inequities.10 As community-based participatory research (CBPR) principles suggest, soliciting such perspectives is critical for the development of culturally appropriate and acceptable interventions.11
Health researchers have recommended CBPR to identify and address health concerns in rural Appalachia,12 a region long considered medically underserved due to financial, geographic, and health system challenges.13 Recent CBPR studies in Appalachia have demonstrated the benefits of relying on local perspectives, ideas, and talents to develop and administer programming. Programs include policy-level interventions,14 community education,15 access-enhancing strategies,16 and media campaigns.17 For example, recognizing the role of social networks, a faith-based CBPR program was created to increase Pap screening in Appalachian Kentucky by targeting individuals through their church.15 Community members assisted in the development and implementation of educational programming and lay health advisor (LHA) counseling. Other CBPR approaches have targeted tobacco use, poor diet/overweight, and lack of physical activity.18 CBPR approaches also have been used to increase CRC screening through a media campaign in Appalachian Ohio.17 In other CBPR projects, mammography screening of low-income women increased by approximately 21% in Pennsylvania, use of smokeless tobacco among men decreased, and human papillomavirus-related knowledge and screening intent increased.19,20
Because addressing health disparities through CBPR has shown promise in Appalachian communities, our research agenda and orientation was set by the community, as our developmental work highlighted Appalachian residents' concern about the disproportionate rates of cancer incidence and mortality in their region.18 We conducted focus groups and key informant interviews to identify strategies to address these cancer disparities in Appalachian Kentucky.
Setting
The Appalachian region, comprised of 410 counties in 13 states, with 22 million people, or 8% of the total U.S. population, defies easy characterization.21 However, the images evoked by Appalachia are most consistent with the central portion of this region. These images include beautiful and rugged mountain terrain, strong kinship traditions, close community ties, and challenges to health and well-being due to resource scarcity. In 2000, the poverty rate in Appalachian Kentucky was 28% higher than that of the nation22 and in 2007, per capita personal income in Central Appalachia was only 71% of the U.S. average.23 In the five counties in Appalachian Kentucky in which the current study took place, the average per capita income ranged from 55% to 67% of U.S. income, and the average percent of adults age 25 and over who had graduated from high school was 58%, compared to 80% in the nation.24
Methods
All procedures and protocols were approved by the Institutional Review Board at the University of Kentucky. Prior to initiating the focus group or key informant interview, all potential participants were read the IRB approved informed consent documents describing their rights and responsibilities. If they agreed with the conduct, participants signed the form, keeping one copy for their records, while research staff retained the other copy. The focus group or interview then began. Although considered low risk research, several steps to taken to prevent a breach of confidentiality including assigning participant identification numbers and de-identifying any data collected; using password protection for computerized files; and storing all data in a secured file cabinet. All interviewers successfully completed their certification in human research protocols (CITI).
Sample recruitment
We recruited focus group (FG) participants through churches, a prime venue for capturing diverse perspectives due to widespread attendance in the region. Although 97% of the population in the participating counties is White,25 our partnership with several African American churches helped us to obtain a more inclusive sample, particularly of a group with suboptimal health profiles.26 Additionally, our previous and future work involves faith-based partnerships, an approach heavily endorsed by a broad cross-section of the community.18
Once a church agreed to partner with us, our local staff arranged a convenient time and location for a FG. Church leaders assisted with recruitment by informing their congregants about the purpose of the discussions and requesting that any interested individuals attend the gathering on a specified date. We did not select participants or exclude anyone meeting our inclusion criteria of being 18 and older and being willing and able to participate in a FG. We did not specify that potential participants had to be church members, as many church attendees lack formal membership. Based on previous practices and participant preferences, we merged discussions of cervical and breast cancer prevention into a single topical group and CRC into another group. All participants in the former FGs were female, while both males and females participated in CRC FGs. Theoretical saturation principles guided our sample size,27 and a total of eight FGs were conducted before reaching saturation. Because we had already scheduled two additional FGs, these sessions served as a confirmation for our findings.
In addition to gauging perceptions of the general population via FGs, we also conducted 19 key informant (KI) interviews with diverse community members, including church ministers or designees, and social services and healthcare providers. In addition to inclusion criteria for the FG participants (i.e., 18 and older and willing to participate) KIs were required to possess specialized knowledge in a salient area, such as religious life, community programs, or cancer prevention. KIs were selected through snowball sampling, with theoretical saturation again guiding our sample size. In snowball sampling, participants who have special areas of expertise or insight are asked to recommend others who have a particular skill set or knowledge base,28 which was, in our case, a grounded understanding of determinants and perspectives on cancer screening in rural Appalachia and potentially appropriate programming. Once we had identified several individuals, we selected additional KIs to ensure a broad representation of perspectives and controlled the process by not recruiting redundant or irrelevant participants. No one refused participation in either the FG or the KI interviews.
Discussion Guide
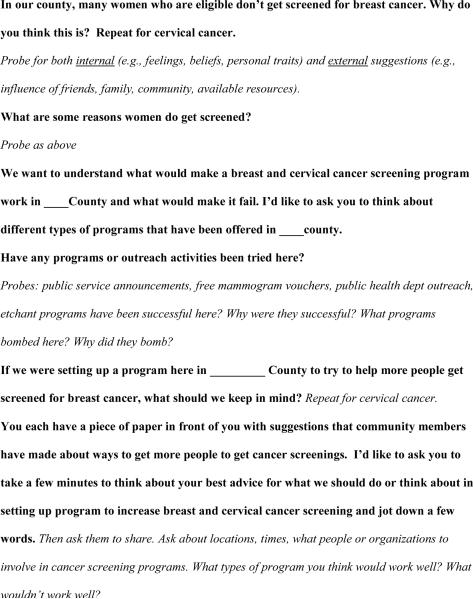
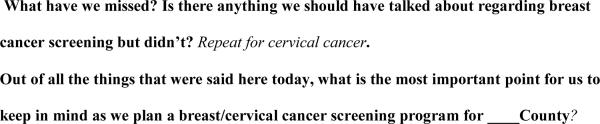
Our discussion guide (Figure 1) was developed by project staff, which included both academic researchers and community members. The guide, modified for the specific cancer site, focused on perceived barriers to and facilitators of screening, types and characteristics of programming desirable for the community, and past successes and failures.
Figure 1.
Example of Focus Group Interview Guide
Procedures
Our community staff, including two trained primary moderators (NF and GW) and two additional experienced assistants, conducted the sessions over a five-month period. The assistants gathered paperwork, took field notes, and wrote memos. We took the following steps to ensure consistency across the 10 FGs: the same moderators and assistants were present at all sessions; one discussion guide was used; transcripts were reviewed immediately to detect deviation from or incompleteness of the discussion guide; and, periodically, outside investigators attended the sessions.29 Most sessions lasted 90–120 minutes.
After describing the purpose of the FG, the moderator asked the open-ended questions and probes from the discussion guide, and sessions concluded with the participants completing a sociodemographic form. The process was repeated for the KI interviews with the exception that transcripts included non-identifying statements attributable to those with specific expertise (e.g., cancer coalition member, health department worker), while no descriptors were used for FG participants. All participants received $25 for their time, travel, and effort.
Analysis
With the permission of participants, all sessions were tape recorded. Tapes were then transcribed by local, trained transcriptionists and reviewed for accuracy by the community staff. The transcripts were then imported into NVivo (QSR, Melbourne, Australia) for coding, organization, and analysis. One member of the research staff engaged in line-by-line coding of the transcripts, affixing codes to each text segment, and then worked with another researcher to refine and define the codes. They developed a preliminary codebook, which allowed standardization of the content analysis and served as a record for definitions and operationalization of codes. The codebook was refined six times.30 To ensure rigor, several steps were taken, including conducting the FG and KI interviews in a uniform manner using the same interviewers, employing member-checking protocols at the end of the interview sessions, and developing, revising, and using a codebook to standardize data analysis.31
Findings
Sample
Table 3 provides a summary of selected sociodemographic characteristics of the combined FG participants. Given that half of the FGs centered on breast and cervical cancer (and thus were comprised exclusively of women), most participants were female. Furthermore, given their greater health vulnerability, we oversampled African Americans relative to their presence in the population. Otherwise, our sample approximated Central Appalachia, with a modest level of education, lower income, and moderate health. Most (16 of 19) KIs were female. Their ages ranged from 25–64, and all were from the five counties in which the study took place. Three participants were physicians who perform cancer screening, four KIs worked as Cooperative Extension agents, seven were local health department employees, two were cancer survivors, and the remaining three were ministers or involved in cancer coalitions.
Table 3.
Combined Focus Group and Key Informant Participants' Characteristics (N=91)
| Characteristic | Frequency | Percent |
|---|---|---|
| Sex | ||
|
| ||
| Male | 22 | 24 |
| Female | 69 | 76 |
|
| ||
| Age | ||
|
| ||
| 18–30 | 12 | 13 |
| 31–40 | 10 | 11 |
| 41–50 | 14 | 15 |
| 51–60 | 21 | 23 |
| 61–70 | 24 | 26 |
| 71+ | 10 | 11 |
|
| ||
| Race | ||
|
| ||
| White | 82 | 90 |
| African-American | 7 | 8 |
| Other | 2 | 2 |
|
| ||
| Education | ||
|
| ||
| Ninth grade or less | 7 | 8 |
| Some High school | 10 | 11 |
| High school graduate | 37 | 41 |
| More than High school | 37 | 41 |
|
| ||
| Marital Status | ||
|
| ||
| Married | 56 | 62 |
| Separated/Divorced/Never married | 22 | 24 |
| Widowed | 13 | 14 |
|
| ||
| Perceived Income Adequacy | ||
|
| ||
| Struggle to get by | 19 | 21 |
| Enough to get by | 44 | 48 |
| More than I need | 24 | 26 |
| Unable/unwilling to say | 4 | 4 |
|
| ||
| Actual income | ||
|
| ||
| Under $10,000 | 15 | 17 |
| $10,0001 – 20,000 | 9 | 10 |
| $20,001–30,000 | 21 | 23 |
| $30,001–40,000 | 9 | 10 |
| Over $40,001 | 26 | 29 |
| Unable/unwilling to say | 11 | 12 |
|
| ||
| Perceived Health Status | ||
|
| ||
| Excellent | 5 | 6 |
| Very good | 23 | 25 |
| Good | 40 | 44 |
| Fair | 19 32 | 21 |
| Poor | 4 | 4 |
Themes
Participants identified three key challenges to residents' obtaining cancer screenings in their Appalachian communities, including (1) inadequate awareness of the need to screen, (2) insufficient access to screening services, and (3) concerns over lack of privacy. Numerous programmatic recommendations accompanied these perceived challenges, including using (1) witnessing or storytelling from those who have been screened or who have experienced cancer, (2) family history to increase the salience of screenings, (3) improved publicity about sliding scale screening opportunities and other community resources, (4) lay health advisors and provider counseling, and (5) preventive services bundling to make any one procedure less onerous. Each programmatic suggestion was accompanied by recommendations on what characteristics should be in place for the program to succeed.
Inadequate awareness of the need to screen
Participants indicated that many Appalachian residents still lack awareness of the need for cancer screening and maintain perspectives that thwart early detection. One FG participant indicated that “public education is the main thing…It's the bottom line—people just need to be aware,” while another noted,
I don't think that Eastern Kentucky [Appalachia] is educated about the survival rate for those that catch it early. Cancer itself it perceived as a death sentence. Why would you go looking for it? That's the last thing you want is to go looking for it if you don't think there's anything you can do about it anyways.
According to many participants, lack of knowledge is particularly pervasive for lesser known preventable cancers, including CRC. As one health department official noted,
…We cannot dispute how breast cancer awareness [has led] to the reduction of breast cancer because of the types of media campaigns they have had over the last several years. …It's time to slow down on the pink ribbons and bring out the blue ribbons and get as much media attention to colon cancer as breast cancer has had.
Another participant perceived that women's screenings focus primarily on breast and cervical cancer screenings to the exclusion of CRC. “They will tell us women that we need to get a pap or a mammogram but they always fail to mention the colonoscopy.”
In addition to public awareness campaigns and increasing physician recommendations for screening, participants mentioned several strategies to enhance knowledge about screening, including publicizing the experiences of local community members who had received the screenings. Such an approach might ease people's minds about the procedures while emphasizing the benefits of early detection. One FG participant explained about her Pap test,
…It's not as scary as everyone thinks it is. I went with my friend when she was having one, and it lasted maybe 5 minutes. Then I decided to have one after she talked to me, and having the nurse there too helped. She was patient and let me feel the equipment and told me what she was doing and went through every step.
Although there was some joking about colonoscopy, most FG participants indicated that the procedures were easier to take than generally perceived and well worth it. “The test prep seems to have gotten better. It used to be over three days and by the third day most people cheated so then they couldn't get a clear reading anyways. Now it's only a one day prep, and even though it's torture, it's better than three.” Furthermore, a KI who was a nurse noted,
I just tell people to not be afraid of the colonoscopy. I tell everyone it is the best nap you'll ever have! I mean we all want a good nap and the cleaning out process the day before is really the worst. But what you go through now is nothing compared to what I went through ten years ago.
Peer education, whether in person or on videos, was emphasized.
It's important to the normal person. It is not medical; it is in terms of everyday life. I like the idea of the guy explaining about just getting his colonoscopy, and he shows how his mashed potatoes is the colon and the peas are the polyps and you just remove those polyps off the colon. So it is easy to understand, and it is everyday people doing what should be an everyday activity.
Involving survivors who could “witness” about the benefits of early detection was viewed as a compelling strategy. As one man stated, “When I found out I had colon cancer, I realized how simple it was to treat.” This personal messaging resonated with others, who pointed out the benefits of personal survivorship stories. “If someone comes and tells you that you need to have this and that done, then I will probably hear them, but I will forget it. But if someone tells me a personal story then it is more likely to stick with me. That is what I think makes the difference.” And, “Maybe on some of the flyers that are made, if there was a person from the community that has had cancer that might help others to connect to their story and maybe influence them to get screened.”
Another strategy that emerged across the FGs was improving the salience of screening tests by ensuring that people know their family histories as described by one FG participant,
[I was motivated by] the fear of cancer. With our family, the real reason we are so concerned with getting screened is because we have had two members of the family die in the last year because of colon cancer. If you have family that die from it, and you see it happen, it puts a fear into you and makes all these little embarrassments small. I'd turn my butt up to anyone to keep from having the condition that those two men had, where you just watch them die everyday a little bit at a time. It was a hard time for their brother to go through with a colonoscopy, but he knew he had to do it.
Participants noted, however, that knowing one's family history can be a difficult, particularly in traditionally underserved communities that historically (and currently) lack access to medical services. One FG participant noted her lack of knowledge about her family, “I think that is especially true with the black community. We don't know our family's medical history. We just didn't sit down and talk about that stuff unless it was widely known that someone was sick.” Additionally, as African American FG participants noted, many family members are disinclined to discuss illness, even if they were aware of it.
Insufficient access to screening services
Ensuring access to screening facilities, particularly in terms of location and hours, loomed large in participants' minds. Frequent mention was made of lack of medical facilities, particularly those accepting patients on Medicaid. Access issues went beyond simply having sufficient income or insurance coverage and involved healthcare capacity in the community, including convenient locations and flexible clinic hours.
Participants described several possibilities for enhancing access to cancer screenings, including use of mobile screening units and setting up screening in worksites and community centers such as food stamp offices, grocery stores, Wal-Mart, and locations within schools where lower income parents might spend time, for example, Family Resource Centers. Worksite promotion was viewed favorably, especially if combined with the incentive of getting the day off. In the words of one FG participant,
Wouldn't it be great if employers would just say that you have a day during the year to go and get screened and it would not count against your pay or your banked time? Just to give people the time to go and get screened…The employers would benefit just as much as the person…Also, if you took a friend or coworker to get screened then you would get a day off just for helping out.
Participants described challenges beyond simply inadequate facilities or time for screening, including efforts by skilled and knowledgeable educators and providers. As noted by one participant, it is relatively easy to hand out Fecal Occult Blood Test cards, but “(t)he problem also is that people don't know how to do it and they also have to mail it, and this is confusing.”
To decrease this confusion, some participants recommended greater publicity about screening protocols overall, including fliers, billboards, and radio advertising. Regular healthcare providers were not necessarily viewed as the best venue for such information, as one FG participant suggested, “I think it would help people a whole lot if they just had a way to answer all of their cancer screening questions without having to go to the doctor!” Instead, many participants advocated for a regular community member - a lay health advisor (LHA) - who could speak their language, reassure them of the need and benefits for such screenings, and inform them about where and when to obtain screening. Such an individual would have to know a great deal about sliding scale opportunities or special “mammogram months” or “free Pap” opportunities and be able to spread the word. As one breast cancer FG participant mentioned, “I think a lot of people can't afford to go to the [private] clinic, yet a lot of the fliers and advertising are at the clinic. So if people who can't afford to go to the clinic they won't even see those fliers.”Another participant mentioned,
That would be the best person [LHAs] to do that as long as they were educated enough to know where the programs were being offered even if they didn't know how to do them, a lot of people in our area are intimidated by professionals and all they need is to have someone talk on their level. I believe this would work better than the newspaper advertisements and everything because after doing this for 5 or 6 years. We still have people say they didn't know about it. This way it would be a guarantee that people know there is transportation, or that this clinic offers this screening on a sliding scale or whatever special program.
Concern over lack of privacy
Inadequate privacy preoccupied many participants, including one who noted, “You don't want people seeing your bottom that you can walk into Wal-Mart and see, it's just too embarrassing.” Another key informant indicated,
I know from my experience it that most people including myself would feel too embarrassed to get one. They don't want to shed their clothes off and let someone see their body. I think that is the biggest reason people don't get screened. Since I have had it done I have talked to three or four people about it and let them know that it is not that bad.
Program suggestions to address privacy concerns focused on developing trusting relations with sensitive physicians and informal navigators or LHAs. Some participants saw the merits of local physicians, mainly through enhanced access to care and developing a close personal connection. For example participants described the key role that a caring and persistent physician played in ensuring screening: “I went for other things but she [the healthcare provider] talked me into the mammogram because it was free, and I got a pap smear then, too.” Another participant indicated that “If my doctor had not been so insistent on me getting one, I would have not done it.”
Along similar lines many key informants suggested that bundling prevention activities could decrease embarrassment while getting everything done at once.
You have to tell people `hey, not just colon cancer that we want, it's all screenings: cardiac, diabetic. At this age you have to have this test done; when you're 45 you have to have your heart checked; when your diabetes needs to be checked or your cancer screened.' This is cost effective, less of an invasion of privacy, and their whole health is being taken care of while reducing cancer. That way you can put it together and get funds from everywhere so you could combine the financial fund, and it would be cheaper, too.
This bundling of preventive procedures resonated with FG participants, one of whom noted, “I think it's good to get all of these things done together. Last time, I had my blood work done, my urine tested, a pelvic exam, then I went down the hall and had a mammogram. It was like, `get her done' time.”
Discussion
Our findings corroborate some existing research on barriers to and strategies for increasing cancer screening in rural32 and, more specifically, Appalachian populations. Community members reported lack of awareness of and access to screening opportunities as well as embarrassment and concern for privacy.26,33 Notably, privacy concerns focused on the body rather than on potential abridgement of medical records or personal information. Additionally, some participants' strategies for improving screening rates are supported by existing literature. These suggestions include enhancing educational opportunities regarding the need for screening, increasing publicity for low-cost or free screening opportunities, and putting an LHA system in place.10,15 Community members also articulated perspectives and described strategies that have not received extensive attention, including drawing on local residents to “witness” or provide testimonies on the importance of cancer screening and early detection, leveraging family history to increase the salience of cancer screening, and bundling preventive services.
Most individuals, particularly underserved populations that may not be accustomed to or trusting of the medical establishment, seek health advice from informal sources prior to visiting a health care professional.34 Recruiting respected laypeople who, based on their personal experiences, can witnesses to fellow community members on the necessity of cancer screening may be an effective approach to cancer prevention.35 Unlike encouragement from members of the research or health education communities, such witnessing may be particularly effective since community insiders share a common language and cultural understandings.36 Additionally, enlisting local people as witnesses to present their personal experiences with screening services or surviving cancer can be a powerful emotional motivator for behavior change.37 Rural and faith-based programs utilizing the combination of LHAs and witnessing have increasing cancer screening by 23–88%.38,39 Peer educator programs also build local capacity, which is a desired outcome in CBPR approaches.40
Participants also recommended focusing on family history to increase the salience of cancer screening. Knowing that cancer has been present in one's family can raise the specter of vulnerability and motivate screening. Even in communities with inadequate resources, including meager support for genetic testing, family history might be used to stratify disease risk and susceptibility.41 Increasingly, there are tools and techniques to facilitate the recording and use of family history, include the NIH's My Family Health Portrait, Health Heritage©, the CDC's Family Healthware, and Family HealthLink, which are electronic and often web-based tools that patients can use both to collect family health history and to determine disease risk.42 Such patient provision of family history information is important as current studies suggest that only a small minority of physicians ever discuss patient family history and that family history is rarely entered into patient records.43 Moreover, collecting family history is inexpensive, considered acceptable by patients, and encourages consideration of shared genetic and environmental factors. Recent research has shown that Appalachian residents are often willing to share family history with healthcare providers and that electronic tools can be viewed as acceptable.44 Although precise data are lacking on computer use, rates of home computer ownership, internet adoption, and access to broadband internet service by low-income families in Kentucky have grown substantially since 2004, due in part to such programs as No Child Left Offline. In Kentucky, home computer ownership has grown by 24% and broadband internet coverage has grown by 35% between 2004 and 2007, with significant increases in Appalachian Kentucky.45 Such increasing use and ownership of computers makes the prospect of electronic health histories more viable. Other research has demonstrated the potential for LHAs to enhance knowledge of family history and highlight its importance in disease prevention.46
As our participants described, however, leveraging family history has its limitations, especially among traditionally underserved populations.47 Historically, many Appalachian residents were unable to access formal medical care, leaving no record of morbidity or mortality. Low levels of education exacerbated this information void, and many patients and their families were uncertain of their diagnoses. Additionally, cancer has been viewed as a stigmatizing condition, resulting in reluctance to share diagnosis information.48 For these reasons and others, many Appalachian residents are unaware of their family health history. With greater access to medical resources, enhanced health literacy, and the de-stigmatization of a cancer diagnosis, there are now greater opportunities to take advantage of family health histories to increase the salience of screening and to employ risk stratification rubrics.
Participants in the current study also described the potential benefits of “bundling” preventive care services. Akin to the value perceived by combining service packages of telecommunications products (e.g., lower costs, one stop shopping), coordinating preventive services into one timeslot and in one location may enhance reach, acceptability, and cost-effectiveness. Given that risk behaviors tend to cluster (e.g., it is estimated that 92% of smokers exhibit at least one additional adverse behavior49), addressing such behaviors together makes intuitive sense. Additionally, the ability to improve one or more behaviors increases self-confidence and motivation,50 and, conversely, failure to change behavior may elicit a reduced sense of self-efficacy and decrease the likelihood of additional behavioral change.51 Regarding health care costs, effectively treating two adverse behaviors results in approximately $2000 of savings per year.52
Although we currently lack definitive results on the effectiveness of preventive services bundling, a growing body of research suggests that targeting multiple risk behaviors and prevention strategies may improve personal motivation and self-efficacy, enhance health status, and reduce health care costs. Like other populations, Appalachian residents' cancer screening and other preventive behaviors tend to cluster.53 That is, those who obtain mammograms are also more likely to receive regular annual checkups or other preventive services.54 In their recommendations to improve uptake of such vital health care services, participants emphasized the cultural acceptability of this bundling approach.
Conclusion, limitations, and future directions
It is common for researchers to justify their work by characterizing communities with health disparities as a collection of pathologies; however, a more constructive approach to addressing these problems requires direct and sustained partnership with communities. Local residents, including our participants, have the greatest potential to identify and address problems salient to the community and identify strategies to address these challenges.
Although this project is limited by its sampling size and orientation (purposive and convenience sampling) and its geographical orientation (five counties in Appalachian Kentucky), we suspect that many of the identified challenges and recommended strategies will apply to many traditionally underserved groups. Sharing numerous features, including lower socioeconomic status, resource deficiencies, and traditions of mutual support, strong kin reliance and religiosity, the findings in this article likely will resonate among diverse populations burdened by health inequities. To extend this work into the future requires using formative research to determine what local residents perceive as health challenges in their communities, melding scientific and community perspectives to develop strategies to address these challenges, and, ultimately, embarking on community-based interventions that must be held to high standards of evaluation.
Acknowledgements
We appreciate the assistance of Tina Kruger, Gwen Whitaker, Sherry Wright, Kaye Dollarhide, and the dozens of community members who provided these insights.
Funding Disclosure: Support for this research was provided by the National Institutes of Health (NIH)/ National Center on Minority Health and Health Disparities/ National Cancer Institute through grant #1 R24MDOOZ75741 (P.I. Schoenberg).
References
- 1.NCI State cancer profiles: Dynamic views of cancer statistics for prioritizing cancer control efforts in the nation, states, and counties. 2009 http://statecancerprofiles.cancer.gov/index.html, 11-16-2010.
- 2.ACCN The Cancer Burden in Appalachia, Appalachian Community Cancer Network. 2009 http://www.accnweb.com/docs/2009/CancerBurdenAppalachia2009.pdf, 11-16-2010.
- 3.Centers for Disease Control and Prevention Cancer death rates — Appalachia, 1994–1998. MMWR Morb Mortal Wkly Rep. 2002;51(24):527–529. [PubMed] [Google Scholar]
- 4.Appalachian Regional Commission . An Analysis of the Financial Conditions of Health Care Institutions in the Appalachian Region and their Economic Impacts. 2002. [Google Scholar]
- 5.Kamangar F, Dores GM, Anderson WF. Patterns of Cancer Incidence, Mortality, and Prevalence Across Five Continents: Defining Priorities to Reduce Cancer Disparities in Different Geographic Regions of the World. Journal of Clinical Oncology. 2006 May 10;24(14):2137–2150. doi: 10.1200/JCO.2005.05.2308. 2006. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention Colorectal Cancer Test Use Among Persons Aged 50 Years. MMWR. 2003;52:193–196. [Google Scholar]
- 7.Freeman H, Wingrove B. Excess Cervical Cancer Mortality: A Marker for Low Access to Health Care in Poor Communities. National Cancer Institute, Center to Reduce Cancer Health Disparities; Rockville, MD: 2005. [Google Scholar]
- 8.Rabin B, Glasgow R, Kerner J, Klump M, Brownson R. Dissemination and Implementation Research on Community-Based Cancer Prevention: A Systematic Review. American Journal of Preventive Medicine. 2010;38(4):443–456. doi: 10.1016/j.amepre.2009.12.035. [DOI] [PubMed] [Google Scholar]
- 9.Pasick R, Hiatt R, Paskett E. Lessons learned from community-based cancer screening intervention research. Cancer. 2004;101(S5):1146–1164. doi: 10.1002/cncr.20508. [DOI] [PubMed] [Google Scholar]
- 10.Katz ML, Wewers ME, Single N, Paskett ED. Key informants' perspectives prior to beginning a cervical cancer study in Ohio Appalachia. Qualitative Health Research. 2007;17(1):131–141. doi: 10.1177/1049732306296507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Israel B, Eng E, Schulz A, Parker E. Introduction to methods in community-based participatory research for health. In: Israel B, Eng E, Schulz A, Parker E, editors. Community-based participatory research for health. Jossey-Bass; San Francisco, CA: 2005. pp. 3–30. [Google Scholar]
- 12.Denham SA, Meyer MG, Toborg MA, Mande MJ. Providing health education to Appalachia populations. Holistic Nursing Practice. 2004;18(6):293–301. doi: 10.1097/00004650-200411000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Lengerich EJ, Wyatt SW, Rubio A, et al. The Appalachia Cancer Network: Cancer Control Research Among a Rural, Medically Underserved Population. The Journal of Rural Health. 2004;20(2):181–187. doi: 10.1111/j.1748-0361.2004.tb00026.x. [DOI] [PubMed] [Google Scholar]
- 14.Schetzina KE, Dalton WT, Lowe EF, et al. A coordinated school health approach to obesity prevention among appalachian youth: The winning with wellness pilot project. Family and Community Health. 2009;32(3):271–285. doi: 10.1097/FCH.0b013e3181ab3c57. [DOI] [PubMed] [Google Scholar]
- 15.Schoenberg NE, Hatcher J, Dignan MB, Shelton B, Wright S, Dollarhide KF. Faith Moves Mountains: an Appalachian cervical cancer prevention program. American Journal of Health Behavior. 2009;33(6):627–638. doi: 10.5993/ajhb.33.6.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ward AJ, Kluhsman BC, Lengerich EJ, Piccinin AM. The impact of cancer coalitions on the dissemination of colorectal cancer materials to community organizations in rural Appalachia. Preventing Chronic Disease. 2006;3(2):1–13. [PMC free article] [PubMed] [Google Scholar]
- 17.Katz ML, Reiter P, Fickle D, et al. Community involvement in the development and feedback about a colorectal cancer screening media campaign in Ohio Appalachia. Health Promotion Practice. 2010 doi: 10.1177/1524839909353736. 1524839909353736, published online November 4, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schoenberg NE, Hatcher J, Dignan MB. Appalachian women's perceptions of their community's health threats. Journal of Rural Health. 2008;24(1):75–83. doi: 10.1111/j.1748-0361.2008.00140.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bencivenga M, DeRubus S, Leach P, Lotito L, Shoemaker C, Lengerich EJ. Community partnerships, food pantries, and an evidence-based intervention to increase mammography among rural women. Journal of Rural Health. 2008;24(1):91–95. doi: 10.1111/j.1748-0361.2008.00142.x. [DOI] [PubMed] [Google Scholar]
- 20.Lengerich E, Kluhsman BC, Bencivenga MM, et al. The Northern Appalachia Cancer Network: Changing cancer research, changing people's lives. Journal of Higher Education Outreach and Engagement. 2010;14(3):83–95. [Google Scholar]
- 21.Friedell G, Linville L, Hullet S. Cancer control in rural Appalachia. Cancer. 1998;(83):1868–1871. [Google Scholar]
- 22.Appalachian Regional Commission Poverty Rates, 2000. 2000 http://www.arc.gov/reports/custom_report.asp?REPORT_ID=11. Accessed May 3, 2010.
- 23.Appalachian Regional Commission Appalachian Region Income Report, 2009. 2009 http://www.arc.gov/images/appregion/AppalachianIncomeReport2009%282007Data%29.pdf. Accessed May 3, 2010.
- 24.Kentucky Institute of Medicine The Health of Kentucky: A County Assessment. 2007 http://www.kyiom.org/healthky2007a.pdf.
- 25.Appalachian Regional Commission Demographic and health information. 2006 http://www.arc.gov/index.do?nodeId=56. Accessed December 21, 2009.
- 26.Behringer B, Friedell GH, Dorgan KA, et al. Understanding the challenges of reducing cancer in Appalachia: Addressing a place-based health disparity population. Californian Journal of Health Promotion. 2007;5:40–50. [Google Scholar]
- 27.Luborsky M, Rubenstein R. Sampling in qualitative research. Research on Aging. 1995;17(91):89–113. doi: 10.1177/0164027595171005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patton MQ. Qualitative Research and Evaluation Methods. 3rd ed. Sage; Thousand Oaks, CA: 2002. [Google Scholar]
- 29.Morgan D. Focus Groups as Qualitative Research. Sage; Thousand Oaks, CA: 1997. [Google Scholar]
- 30.MacQueen KM, McLellan E, Milstein KK, Milstein B. Codebook development for team-based qualitative analysis. Cultural Anthropology Methods. 1998;10(2):6. [Google Scholar]
- 31.Morse JM, Swanson JM, Kuzel AJ, editors. The Nature of Qualitative Evidence. Sage; Thousand Oaks, CA: 2001. [Google Scholar]
- 32.Coughlin SS, Tompson TD. Colorectal cancer screening practices among men and women in rural and nonrural areas of the United States, 1999. Journal of Rural Health. 2004;20(118-124) doi: 10.1111/j.1748-0361.2004.tb00017.x. [DOI] [PubMed] [Google Scholar]
- 33.Schoenberg NE, Hopenhayn C, Christian A, Knight EA, Rubio A. An in-depth and updated perspective on determinants of cervical cancer screening among central Appalachian women. Women & Health. 2005;42(2):89. doi: 10.1300/j013v42n02_06. [DOI] [PubMed] [Google Scholar]
- 34.Ogedegbe G, Cassells AN, Robinson CM, et al. Perceptions of barriers and facilitators of cancer early detection among low-income minority women in community health centers. Journal of the National Medical Association. 2005;97:162–170. [PMC free article] [PubMed] [Google Scholar]
- 35.Moore A, Earp JAL. Healthcare services: Partnering with lay health advisors to improve health equity. In: Earp JAL, French EA, Gilkey MB, editors. Patient Advocacy for Health Care Quality: Strategies for Achieving Patient-Centered Care. Jones and Bartlett Publishers; Sudbury, MA: 2008. pp. 121–150. [Google Scholar]
- 36.Rhodes SD, Foley KL, Zometa CS, Bloom FR. Lay health advisor interventions among Hispanics/Latinos: A qualitative systematic review. American Journal of Preventive Medicine. 2007;33(5):418–427. doi: 10.1016/j.amepre.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 37.Delony L. An implementation guide for The Witness Project: A culturally sensitive, community-based cancer education program for African-American women. Arkansas Cancer Research Center; Little Rock: 1996. [Google Scholar]
- 38.Erwin DO. Cancer education takes on a spiritual focus for the African American faith community. Journal of Cancer Education. 2002;17(1):46–49. doi: 10.1080/08858190209528792. [DOI] [PubMed] [Google Scholar]
- 39.Kriger H. Outreach to multiethnic, multicultural, and multilingual women for breast cancer and cervical cancer education and screening: A model using professional and volunteer staffing. Family and Community Health. 2003;26(4):307–318. doi: 10.1097/00003727-200310000-00007. [DOI] [PubMed] [Google Scholar]
- 40.Wandersman A, Florin P. Community interventions and effective prevention. American Psychologist. 2003;58(6/7):441–448. doi: 10.1037/0003-066x.58.6-7.441. [DOI] [PubMed] [Google Scholar]
- 41.Yoon PW, Scheuner MT, Peterson-Oehlke KL, Gwinn M, Faucett A, Khoury MJ. Can family history be used as a tool for public health and preventive medicine? Genetics in Medicine. 2002;4(4):304–310. doi: 10.1097/00125817-200207000-00009. [DOI] [PubMed] [Google Scholar]
- 42.Cohn WF, Ropka ME, Pelletier SL, et al. Health Heritage, a web-based tool for the collection and assessment of family health history: Initial user experience and analytic validity. Public Health Genomics. 2010;13:477–491. doi: 10.1159/000294415. [DOI] [PubMed] [Google Scholar]
- 43.Acheson L, Wiesner G, Zyzanski S, Goodwin M, Stange K. Family history taking in community family practice: implications for genetic screening. Genet Med. 2000;2:180–185. doi: 10.1097/00125817-200005000-00004. [DOI] [PubMed] [Google Scholar]
- 44.Au M, Cornett S, Nick T, et al. Familial risk for chronic disease and intent to share family history with a health care provider among urban Appalachian women, southwestern Ohio, 2007. Prev Chronic Dis 2010. 2010;7(1) [PMC free article] [PubMed] [Google Scholar]
- 45.ConnectKentucky Setting the pace: accelerating broadband expansion. Progress Report. 2008 Retrieved on 7-10-11 from http://connectkentucky.org/_documents/ConnectKentuckyProgressReport2008.pdf2008.
- 46.Kaphingst K, Lachance C, Gepp A, Hoyt D'Anna L, Rios-Ellis B. Educating Underserved Latino Communities about Family Health History Using Lay Health Advisors. Public Health Genomics. 2009 doi: 10.1159/000272456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Valdez R, Yoon PW, Qureshi N, Green RF, Khoury MJ. Family history in public health practice: A genomic tool for disease prevention and health promotion. Annual Review of Public Health. 2010;31:69–87. doi: 10.1146/annurev.publhealth.012809.103621. [DOI] [PubMed] [Google Scholar]
- 48.Kagawa-Singer M, Dadia AV, Yu MC, Surbone A. Cancer, culture, and health disparities. CA Cancer J Clin. 2010;60:12–39. doi: 10.3322/caac.20051. [DOI] [PubMed] [Google Scholar]
- 49.Fine LJ, Philogene GS, Gramling R, Coups EJ, Sinha S. Prevalence of multiple chronic disease risk factors: 2001 National Health Interview Survey. American J of Preventive Medicine. 2004;27:18–24. doi: 10.1016/j.amepre.2004.04.017. [DOI] [PubMed] [Google Scholar]
- 50.Unger JB. Stages of change of smoking cessation: Relationships with other health behaviors. American Journal of Preventive Medicine. 1996;12(2):134–138. [PubMed] [Google Scholar]
- 51.Nagaya T, Yoshida H, Takahashi H, Kawai M. Cigarette smoking weakens exercise habits in healthy men. Nicotine and Tobacco Research. 2007;9(10) doi: 10.1080/14622200701591575. 9(10):1027-1032. [DOI] [PubMed] [Google Scholar]
- 52.Edington DW. Emerging research: A view from one research center. American Journal Health Promotion. 2001;15(5):341–349. doi: 10.4278/0890-1171-15.5.341. [DOI] [PubMed] [Google Scholar]
- 53.Amonkar MM, Madhavan S. Compliance rates and predictors of cancer screening recommendations among Appalachian women. Journal of Health Care for the Poor and Underserved. 2002;13(4):443–460. doi: 10.1353/hpu.2010.0582. [DOI] [PubMed] [Google Scholar]
- 54.Leach C, Schoenberg N. The vicious cycle of inadequate early detection: a complementary study on barriers to cervical cancer screening among middle-aged and older women. Prev Chronic Dis. 2007;4(4):A95. [PMC free article] [PubMed] [Google Scholar]