Abstract
Endoscopic submucosal dissection (ESD) with a knife is a technically demanding procedure associated with a high complication rate. The shortcomings of this method are the deficiencies of fixing the knife to the target lesion, and of compressing it. These shortcomings can lead to major complications such as perforation and bleeding. To reduce the risk of complications related to ESD, we developed a new grasping type scissors forceps (Clutch Cutter®, Fujifilm, Japan) which can grasp and incise the targeted tissue using an electrosurgical current. Esophagogastroduodenoscopy on a 59-year-old Japanese man revealed a 16mm esophageal submucosal nodule with central depression. Endoscopic ultrasonography demonstrated a hypoechoic solid tumor limited to the submucosa without lymph node involvement. The histologic diagnosis of the specimen obtained by biopsy was granular cell tumor. It was safely and accurately resected without unexpected incision by ESD using the CC. No delayed hemorrhage or perforation occurred. Histological examination confirmed that the granular cell tumor was completely excised with negative resection margin.We report herein a case of esophageal granular cell tumor successfully treated by an ESD technique using the CC.
Keywords: Endoscopic submucosal dissection, Esophageal granular cell tumor, Clutch Cutter, Endoscopic therapy, Grasping type scissors forceps
INTRODUCTION
Granular cell tumors (GCT) of the esophagus are rare neoplasms and their diagnosis is mainly based on histopathologic examination of endoscopic biopsies. At present, GCT treatment is not established. Until recently, management consisted of 2 relatively unsatisfactory options: observation without a definitive tissue diagnosis, and surgical resection[1]. Current advances in endoscopic techniques and technology have greatly enhanced the diagnosis and treatment of gastrointestinal malignancy. Endoscopic resection can greatly improve the management of submucosal tumors (SMT) of the gastrointestinal tract[2-6]. SMT can be resected easily and safely using this treatment method. However, endoscopic resection of SMT is sometimes inappropriate for complete resection[7]. Endoscopic submucosal dissection (ESD) has been reported to improve the rate of successful en-bloc resection in early GI tract tumors[8].Furthermore, ESD can accurately control the depth of submucosal exfoliation under endoscopic view. However, ESD, and particularly the process of submucosal dissection, is technically difficult and carries a high risk of perforation and bleeding[9-12]. Conventional devices for submucosal incision such as the IT knife and needle knife merely bring the knife in contact with the submucosal tissue and cutting is performed using an electrosurgical current. These cutting methods without fixing the knife to the target have a potential risk of incomplete resections or major complications due to unexpected incision due to pulsation or respiratory movement. To resolve the problems related to ESD using a conventional knife, we have developed the Clutch Cutter (CC), which can accurately grasp and incise the targeted tissue using an electrosurgical current[13,14]. In our previous study of early gastric neoplasms, we resected 35 tumors safely and easily without unintentional incision by ESD using the CC[15]. In this report, we first describe a new method of ESD using the CC for esophageal granular cell tumor.
CASE REPORT
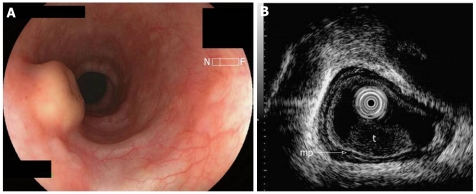
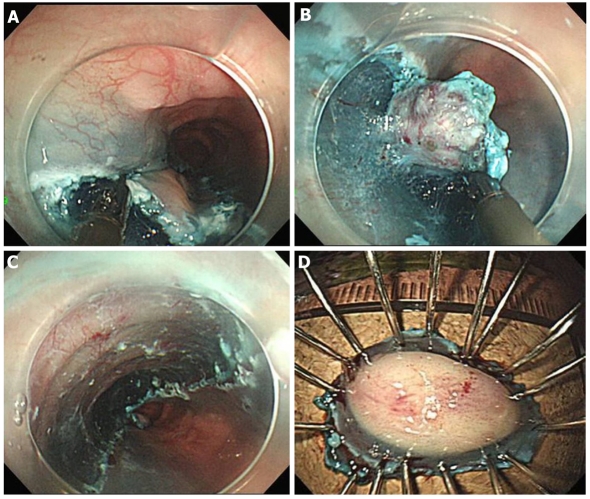
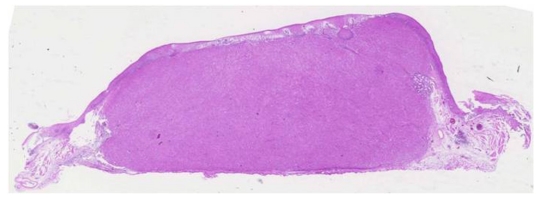
Esophagogastroduodenoscopy (EGD) on a 59-year-old man revealed a 16mm esophageal submucosal nodule with a central depression (Figure1A). The histologic diagnosis of the specimen obtained by biopsy was granular cell tumor. Subsequent endoscopic ultrasonography (EUS) demonstrated a hypoechoic solid tumor in the submucosa without lymph node involvement (Figure 1B). It was treated by endoscopic submucosal dissection using a newly developed grasping type scissors forceps (Clutch Cutter®, DP2618DT; Fujifilm, Odawara, Japan) (Figure 2)[13] after obtaining written informed consent from the patient. A two channel multi-bending endoscope (GIF-2T240M; Olympus, Tokyo, Japan) was used in this case. During ESD, the patient was sedated with an intravenous injection of flunitrazepam (0.4 mg) and pethidine (35mg). The ESD technique using the CC was as follows: Marking dots were placed approximately a few millimeters outside the margin of the lesion with a hook knife (KD-620LR; Olympus, Tokyo, Japan) and a coagulation current 20W (Forced coagulation mode) created by an electrosurgical generator (ICC 200; Erbe, Tübingen, Germany). Next, a hyaluronic acid solution (MucoUp: Johnson and Johnson Co., Tokyo, Japan) mixed with a small volume of epinephrine and indigo carmine dye was injected into the submucosal layer around the target lesion to lift the entire lesion. The lesion was separated from the surrounding normal mucosa (Figure 3A) around the lesion with the CC using an electrosurgical current (Autocut mode 120W). A piece of submucosal tissue was grasped and cut with the CC (Autocut mode 120W) to achieve submucosal excision. During the submucosal dissection, ESD using the CC accurately controlled the depth of submucosal excision under endoscopic vision (Figure 3B). Finally, the lesion was completely resected (en bloc resection) by CC (Figures 3C-D). ESD was completed in 59 min. Macroscopically, the mass was yellowish-white and solid, measuring 16 mm × 10 mm in diameter. Microscopically, the tumor was composed of small uniform cells, arranged in small nests and cords and with an anastomosing ribbon-like pattern in the submucosal layer. These cells had abundant granular cytoplasm and small round nuclei. Immunohistochemically, the tumor cells were positive for S-100 protein. The vertical and horizontal cut margins were negative. There was no lymphovascular invasion. These findings established curative resection of the granular cell tumor (Figure 4). After ESD, the patient remained in hospital and was prohibited from eating until the third day after ESD. Laboratory findings and chest and abdominal X-ray showed no negative changes after ESD. He was permitted oral soft food and discharged 6 d after the procedure. No hemorrhage, perforation, or other complications occurred.
Figure 1.
Pretherapeutic examinations of esophageal granular cell tumor. A: Endoscopic view of the yellowish submucosal tumor with a central depression in the middle esophagus; B: Endoscopic ultrasonography showing a hypoechoic solid tumor (t) in the submucosa; Arrow-mp: Muscularis propria.
Figure 2.
Distal tip of the Clutch Cutter. The outer side of the forceps is insulated so that electrosurgical current energy is concentrated at the blade to avoid burning the surrounding tissue.
Figure 3.
Endoscopic view of the procedure of endoscopic submucosal dissection using the Clutch Cutter. A: Endoscopic view of partial circumferential incision of the tumor using the Clutch Cutter (CC); B: Endoscopic view of the submucosal exfoliation under the tumor using the CC; C: The lesion is cut completely from the muscle layer; D: The resected specimen showing curative en bloc resection of the lesion.
Figure 4.
Microscopic appearance of the tumor. The resected tumor is covered with normal mucosa (hematoxylin and eosin; original magnification, x 2).
Newly developed Grasping type Scissors Forceps (Clutch Cutter®)
The Clutch Cutter® (DP2618DT, Fujifilm Corporation, Odawara, Japan) (Figure 2) can grasp and cut a piece of tissue with an electrosurgical current. It has a 0.4 mm wide and 3 mm long serrated cutting edge to facilitate grasping the tissue. The outer side of the forceps is insulated so that electrosurgical current energy is concentrated at the blade to avoid burning the surrounding tissue. Furthermore, the forceps can be rotated to the desired orientation. The diameter of the forceps is 2.7 mm. The CC is available for standard endoscopes with a working channel width of 2.8 mm or more. This device, which is disposable and not reusable, was used for marking, circumferential marginal incision, submucosal dissection and hemostatic treatment.
Ethical considerations
The advantages and disadvantages of ESD using the CC, as well as alternative endoscopic options (ESD using conventional device, endoscopic mucosal resection, etc), were discussed with the patient. The patient was aware of the experimental nature of the planned treatment. He gave his written informed consent for the designated intervention. This study was reviewed and approved by the ethics committee of Aso Iizuka Hospital. It was conducted in accordance with the ethical principles of the Declaration of Helsinki and in compliance with good clinical practice.
DISCUSSION
Esophageal GCT account for one-third of gastrointestinal tract GCT. Esophageal GCT are generally considered benign, although a few malignant GCT have been reported[16,17]. Six histologic criteria were assessed: necrosis, spindling, vesicular nuclei with large nucleoli, increased mitotic activity (> 2 mitoses/10 high power fields at 200× magnification), high nuclear to cytoplasmic (N:C) ratio, and pleomorphism[18]. Neoplasms that met three or more of these criteria were classified as histologically malignant; those that met one or two criteria were classified as atypical; and those that displayed only focal pleomorphism but fulfilled none of the other criteria were classified as benign. Ordinary endoscopic biopsy involving a small amount of tissue is unlikely to yield diagnostic tissue because the tumor typically is covered by normal mucosa. Therefore, preoperative diagnosis is difficult without total resection of the tumor. When we make a diagnosis of GCT endoscopically, we should consider the possibility of malignancy.
For this reason, endoscopic resection is currently considered an appropriate approach for total resection of GCT[2-4,19]. However,various modified endoscopic therapies, such as endoscopic mucosal resection (EMR)[2], endoscopic aspiration lumpectomy (EAL)[5], strip biopsy[6], endoscopic mucosal resection using a ligating device (EMRL)[4] and EUS-guided endoscopic resection using band ligation[19] have been reported. Submucosal tumors smaller than 1 cm in diameter and separate from the muscularis propria can be resected by endoscopic therapy. However, endoscopic resection of submucosal tumor is sometimes inappropriate for complete resection[7]. Use of conventional methods is often associated with marginal involvement by residual tumor requiring subsequent intervention.
In such circumstances, ESD should be applied[20]. ESD was originally developed to obtain one-piece resection for early gastric cancers[10-14]. ESD has the advantage of permitting en bloc resection and histologically complete resection. On the other hand, this method has the disadvantages of a long procedure time and a high frequency of complications, as well as demanding a high level of technical skill. However, ESD can control the depth of submucosal dissection under endoscopic view[9-14]. Therefore, ESD is a theoretically suitable therapeutic option for GCT located within the submucosa[21]. If the tumor invades the muscularis propria, ESD is a contraindication due to the risk of perforation and metastasis. Pretherapeutic EUS is vital for decision making concerning the indication of ESD for this disease.
Endoscopic removal with ESD of a granular cell tumor of the esophagus was first described by Aoki et al[22] in 2005. Since this first report, there have been at least 2 documented reports of esophageal GCT successfully removed with ESD. In these three cases, a knife device was used for ESD[21-23]. Incision using knife devices merely brings the knife in contact with the tissue and cut using electrosurgical current. These cutting processes without fixing the device to the targeted tissue make it difficult to place the knife accurately during electrosurgical incision because of cardiac beat, respiratory movement, and peristalsis. Lack of complete endoscopy control can cause unwanted incision and may result in incomplete resection or severe complications such as perforation and bleeding[9-12].
Our approach was to perform endoscopic resection with a CC which can be passed through the ordinary working channel. This device was developed by us for ESD of early gastric cancer[13,14]. It has a thin serrated cutting edge to facilitate grasping the tissue. The outer side of the forceps is insulated so that electrosurgical current energy is concentrated at the blade to avoid burning the surrounding tissue. Furthermore, the forceps can be rotated to the desired orientation. Theoretically, the main advantage of the CC for ESD is the fixed device, which can accurately control the depth of submucosal exfoliation with good endoscopic vision[14].The CC can be used to grasp the targeted tissue again if necessary, before electrosurgical cutting. The maximal advantage of the CC is having the visual confirmation step for accurate and safe targeting by the device before cutting during the grasping stage. Furthermore, the CC can reduce post-cut hemorrhage by a compression effect similar to a polypectomy snare[14]. Thus,the grasping step before cutting allows accurate targeting and compression of the vessel, and reduces the chance of incomplete resection (positive vertical margin) and major complications (perforation and bleeding). In this case, it was safe and accurate to resect the esophageal GCT with sufficient negative resection margin using the CC. We believe this technique has the potential to become the method of choice for removal of GI tract GCT when the tumor is limited to the submucosa.
Footnotes
Peer reviewer: Satoru Kakizaki, MD, PhD, Assistant Professor, Department of Medicine and Molecular Science, Gunma University, Graduate School of Medicine, 3-39-15 Showa-machi, Maebashi, Gunma 371-8511, Japan
S- Editor Yang XC L- Editor Webster JR E- Editor Yang XC
References
- 1.Waxman I, Saitoh Y, Raju GS, Watari J, Yokota K, Reeves AL, Kohgo Y. High-frequency probe EUS-assisted endoscopic mucosal resection: a therapeutic strategy for submucosal tumors of the GI tract. Gastrointest Endosc. 2002;55:44–49. doi: 10.1067/mge.2002.119871. [DOI] [PubMed] [Google Scholar]
- 2.Yasuda I, Tomita E, Nagura K, Nishigaki Y, Yamada O, Kachi H. Endoscopic removal of granular cell tumors. Gastrointest Endosc. 1995;41:163–167. doi: 10.1016/s0016-5107(05)80604-2. [DOI] [PubMed] [Google Scholar]
- 3.Esaki M, Aoyagi K, Hizawa K, Nakamura S, Hirakawa K, Koga H, Yao T, Fujishima M. Multiple granular cell tumors of the esophagus removed endoscopically: a case report. Gastrointest Endosc. 1998;48:536–539. doi: 10.1016/s0016-5107(98)70102-6. [DOI] [PubMed] [Google Scholar]
- 4.Shikuwa S, Matsunaga K, Osabe M, Ofukuji M, Omagari K, Mizuta Y, Takeshima F, Murase K, Otani H, Ito M, et al. Esophageal granular cell tumor treated by endoscopic mucosal resection using a ligating device. Gastrointest Endosc. 1998;47:529–532. doi: 10.1016/s0016-5107(98)70257-3. [DOI] [PubMed] [Google Scholar]
- 5.Yazumi S, Takahashi R, Kajiyama T, NakaseH , WatanabeN , OhanaM , MatsumotoS , SenoH , SawadaM , UchidaK , et al. Comparison of histological analysis and endosonographic features in esophageal granular cell tumors. Digestive Endoscopy. 2003;15:284–288. [Google Scholar]
- 6.Urabe M, Daibo M, Gonda H, Sakakibara N. Three cases of esophageal granular cell tumor. Digestive Endoscopy. 1996;8:32–37. [Google Scholar]
- 7.Wehrmann T, Martchenko K, Nakamura M, Riphaus A, Stergiou N. Endoscopic resection of submucosal esophageal tumors: a prospective case series. Endoscopy. 2004;36:802–807. doi: 10.1055/s-2004-825814. [DOI] [PubMed] [Google Scholar]
- 8.Hirao M, Masuda K, Asanuma T, Naka H, Noda K, Matsuura K, Yamaguchi O, Ueda N. Endoscopic resection of early gastric cancer and other tumors with local injection of hypertonic saline-epinephrine. Gastrointest Endosc. 1988;34:264–269. doi: 10.1016/s0016-5107(88)71327-9. [DOI] [PubMed] [Google Scholar]
- 9.Onozato Y, Kakizaki S, Ishihara H, Iizuka H, Sohara N, Okamura S, Mori M, Itoh H. Endoscopic submucosal dissection for rectal tumors. Endoscopy. 2007;39:423–427. doi: 10.1055/s-2007-966237. [DOI] [PubMed] [Google Scholar]
- 10.Ono H, Kondo H, Gotoda T, Shirao K, Yamaguchi H, Saito D, Hosokawa K, Shimoda T, Yoshida S. Endoscopic mucosal resection for treatment of early gastric cancer. Gut. 2001;48:225–229. doi: 10.1136/gut.48.2.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fujishiro M. Endoscopic submucosal dissection for stomach neoplasms. World J Gastroenterol. 2006;12:5108–5112. doi: 10.3748/wjg.v12.i32.5108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neuhaus H, Costamagna G, Devière J, Fockens P, Ponchon T, Rösch T. Endoscopic submucosal dissection (ESD) of early neoplastic gastric lesions using a new double-channel endoscope (the “R-scope”) Endoscopy. 2006;38:1016–1023. doi: 10.1055/s-2006-944830. [DOI] [PubMed] [Google Scholar]
- 13.Akahoshi K, Akahane H, Murata A, Akiba H, Oya M. Endoscopic submucosal dissection using a novel grasping type scissors forceps. Endoscopy. 2007;39:1103–1105. doi: 10.1055/s-2007-966842. [DOI] [PubMed] [Google Scholar]
- 14.Akahoshi K, Honda K, Akahane H, Akiba H, Matsui N, Motomura Y, Kubokawa M, Endo S, Higuchi N, Oya M. Endoscopic submucosal dissection by using a grasping-type scissors forceps: a preliminary clinical study (with video) Gastrointest Endosc. 2008;67:1128–1133. doi: 10.1016/j.gie.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 15.Akahoshi K, Honda K, Motomura Y, Kubokawa M, Okamoto R, Osoegawa T, Nakama N, Kashiwabara Y, Higuchi N, Tanaka Y, et al. Endoscopic submucosal dissection using a grasping-type scissors forceps for early gastric cancers and adenomas. Dig Endosc. 2011;23:24–29. doi: 10.1111/j.1443-1661.2010.01037.x. [DOI] [PubMed] [Google Scholar]
- 16.Orlowska J, Pachlewski J, Gugulski A, Butruk E. A conservative approach to granular cell tumors of the esophagus: four case reports and literature review. Am J Gastroenterol. 1993;88:311–315. [PubMed] [Google Scholar]
- 17.Vuyk HD, Snow GB, Tiwari RM, van Velzen D, Veldhuizen RW. Granular cell tumor of the proximal esophagus. A rare disease. Cancer. 1985;55:445–449. doi: 10.1002/1097-0142(19850115)55:2<445::aid-cncr2820550226>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 18.Fanburg-Smith JC, Meis-Kindblom JM, Fante R, Kindblom LG. Malignant granular cell tumor of soft tissue: diagnostic criteria and clinicopathologic correlation. Am J Surg Pathol. 1998;22:779–794. doi: 10.1097/00000478-199807000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Saito H, Akahoshi K, Oya M, Kubokawa M, Akiho H, Sumida Y, Fujimaru T, Higuchi N, Matsumoto M. EUS-guided endoscopic resection using band ligation of oesophageal granular cell tumour: report of a case. Acta Gastroenterol Belg. 1998;68:272–275. [PubMed] [Google Scholar]
- 20.Fujishiro M. Perspective on the practical indications of endoscopic submucosal dissection of gastrointestinal neoplasms. World J Gastroenterol. 2008;14:4289–4295. doi: 10.3748/wjg.14.4289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hülagü S, Sentürk O, Aygün C, Gürbüz Y, Kocaman O, Celebi A, Konduk T. Granular cell tumor of esophagus removed with endoscopic submucosal dissection. Turk J Gastroenterol. 2007;18:188–191. [PubMed] [Google Scholar]
- 22.Aoki H, Onohara Y, Iizuka H, Sagawa T, Arai H, Takayama H, Abe T, Tomizawa N, Ogawa T, Ishihara H, et al. A case of esophageal granular cell tumor successfully resected by endoscopic submucosal dissection(ESD) Progress of Digestive Endoscopy. 2005;67:2: 54–55. [Google Scholar]
- 23.Okamoto Y, Sasaki Y, Yagihashi N, Yamai K, Sato K, Chiba H, Tinda D, Saito M, Suzuki H, Hachimori H, et al. An esophageal granularcell tumor successfully removed with endoscopic submucosal dissection. Gastroenterol Endosc. 2010;52:1857–1865. [Google Scholar]