Abstract
Background:
Recent publications suggest that arthroscopic and open rotator cuff repairs have had comparable clinical results, although each technique has distinct advantages and disadvantages. National hospital and ambulatory surgery databases were reviewed to identify practice patterns for rotator cuff repair.
Methods:
The rates of medical visits for rotator cuff pathology, and the rates of open and arthroscopic rotator cuff repair, were examined for the years 1996 and 2006 in the United States. The national incidence of rotator cuff repairs and related data were obtained from inpatient (National Hospital Discharge Survey, NHDS) and ambulatory surgery (National Survey of Ambulatory Surgery, NSAS) databases. These databases were queried with use of International Classification of Diseases, Ninth Revision (ICD-9) procedure codes for arthroscopic (ICD-9 codes 83.63 and 80.21) and open (code 83.63 without code 80.21) rotator cuff repair. We also examined where the surgery was performed (inpatient versus ambulatory surgery center) and characteristics of the patients, including age, sex, and comorbidities.
Results:
The unadjusted volume of all rotator cuff repairs increased 141% in the decade from 1996 to 2006. The unadjusted number of arthroscopic procedures increased by 600% while open repairs increased by only 34% during this time interval. There was a significant shift from inpatient to outpatient surgery (p < 0.001).
Conclusions:
The increase in national rates of rotator cuff repair over the last decade has been dramatic, particularly for arthroscopic assisted repair.
Considerable literature exists regarding the surgical management of rotator cuff tears. Arthroscopic and open rotator cuff repairs have had comparable clinical results in the literature, with distinct advantages and disadvantages to both procedures1,2. Arthroscopy allows for preservation of the deltoid muscle3, improved ability to treat intra-articular lesions3, improved ability to mobilize and release the rotator cuff3, and less immediate postoperative pain4. Open and mini-open repair techniques allow for easier transosseous fixation to better replicate the footprint of the supraspinatus tendon5 and theoretically may provide a better potential for healing5, although transosseous equivalent constructs with use of suture anchors have been described that also show improved pressurized contact area6,7. Open repair and mini-open repair also allow for the placement of a modified Mason-Allen stitch, which, in comparison with the simple stitch, is a stronger method to grasp the tendon8,9.
Several studies have examined geographic variation in the number of rotator cuff surgical procedures performed as well as variations in what surgeons deemed to be indications for rotator cuff surgery. For example, Vitale et al. found a large geographic variation in the number of rotator cuff surgical procedures that were performed in Medicare beneficiaries in 199210. This variation may have reflected a lack of clear operative indications and/or an understanding of the risks and benefits of surgery at the time of the study. With respect to surgical indications, Green et al. reported that surgeon preference was the primary deciding factor for performing inpatient rotator cuff surgery11. Dunn et al. also found significant variation in indications for rotator cuff surgery in a survey of selected members of the American Academy of Orthopaedic Surgeons as of the year 200212. Surgeons who had a higher procedure volume favored rotator cuff surgery more than those who had a lower volume12. Mini-open repair was the most frequently used method of repair (46.2%) followed by open (36.6%) and arthroscopic (14.5%)12.
Despite many publications addressing rotator cuff repair techniques, indications for rotator cuff surgery, and outcomes in selected groups of patients, little information has been reported recently on trends of use at the national level.
The purpose of our study was multifold. First, we sought to determine current trends in resource utilization for rotator cuff repairs, including type and setting of surgical treatment as well as type of anesthesia. The impact of age and sex on resource utilization was also examined. Finally, we also studied other variables (e.g., procedure length) that contribute to health-care costs.
The hypotheses of our study were that (1) surgeons are now performing more arthroscopic rotator cuff repairs, (2) more of these repairs are being performed in ambulatory surgery settings, (3) patients who undergo surgery in an inpatient setting are more likely to be older and have more comorbidities, (4) surgical time is longer for arthroscopic repairs, and (5) the use of interscalene block for anesthesia is increasing.
Materials and Methods
Data Source
The rates of open and arthroscopic rotator cuff repairs for the years 1996 and 2006 in the United States were examined. We used publicly available national health-care surveys conducted by the Centers for Disease Control and Prevention (CDC) for our study. The national estimates of rotator cuff repairs and related data were obtained from the National Hospital Discharge Survey (NHDS), which is an inpatient database, and the National Survey of Ambulatory Surgery (NSAS), which is an outpatient surgery database. Data on ambulatory medical services utilization were obtained from two databases: (a) the annual National Ambulatory Medical Care Survey (NAMCS), which records physician office visits, and (b) the National Hospital Ambulatory Medical Care Survey (NHAMCS), which includes emergency department and hospital outpatient department visits.
Population data were obtained from the U.S. Census Bureau13. The NAMCS, the NHAMCS, the NSAS, and the NHDS are each National Center for Health Statistics (NCHS) surveys that are designed to be representative of health-care services delivered by non-federally employed health-care providers. They each may include disproportionate sampling in an effort to achieve a meaningful national sample that allows subgroup analysis. The NSAS collects data from a sample of hospital and freestanding ambulatory surgery centers and describes outpatient procedures performed at short-stay hospitals located in all fifty states and the District of Columbia. The NHDS is a national probability sample designed to meet the need for information on characteristics of inpatient discharges from non-federal short-stay hospitals in the United States. The NHDS collects data from a national sample of about 500 non-federal short-stay hospitals, defined as hospitals with an average length of stay of fewer than thirty days, and including major medical centers. Federal, military, and Department of Veterans Affairs hospitals as well as hospital units of government institutions (such as prison hospitals), and hospitals with fewer than six beds are excluded from both the NSAS and the NHDS. The weighting procedure used in the NSAS and the NHDS produces essentially unbiased national estimates. These numbers are derived from a multistage estimate procedure that includes three basic components: inflation by reciprocals of the probabilities of sample selection, adjustment for no response, and population weighting ratio adjustments.
The NAMCS and the NHAMCS are nationally representative surveys with similar methodologies, collecting chart review data from a probability sample of outpatient visits to physician offices, while the NHAMCS collects similar data from hospital outpatient departments and emergency departments. Data for NAMCS are collected from 112 geographic areas located among the fifty states and the District of Columbia, including 3000 physicians and consisting of 25,000 annual visits for national estimations. Data for NHAMCS are also collected from 112 geographic areas located among the fifty states and the District of Columbia, including 500 hospitals with 400 emergency departments and 250 outpatient departments and consisting of 37,000 emergency and 35,000 outpatient department visits. Combined NAMCS and NHAMCS databases for 2006 provided a national estimation of 1,123,353,924 ambulatory visits.
Study Population
Hospitalizations from the NHDS or the NSAS were identified by ICD-9 procedure codes for arthroscopic (ICD-9 codes 83.63 and 80.21) and open (code 83.63 without code 80.21) rotator cuff repair (Table I). We examined where the surgery was performed (inpatient or ambulatory surgery center) and patient characteristics, including age, sex, and comorbidities. ICD-9 diagnosis codes identified as having a high frequency of association with rotator cuff procedures in the NHDS and NSAS databases were used to query NAMCS and NHAMCS databases to identify ambulatory medical visits for rotator cuff tears. These codes included: 726.10 (rotator cuff syndrome of shoulder, disorder of bursae and tendons in shoulder region, unspecified), 726.11 (calcifying tendinitis of shoulder), 726.19 (other specified rotator cuff syndrome of shoulder and allied disorders), 727.61 (complete rupture of rotator cuff, nontraumatic), and 840.4 (sprains and strains of rotator cuff) (Table II).
TABLE I.
ICD-9 Procedure Codes Used for Analysis*
| ICD-9 Procedure Code | Description |
| 83.63 with 80.21 | Arthroscopic rotator cuff repair |
| 83.63 | Open rotator cuff repair |
ICD-9 = International Classification of Diseases, Ninth Revision.
TABLE II.
ICD-9 Diagnosis Codes Used for Analysis*
| ICD-9 Diagnosis Code | Description |
| 726.10 | Rotator cuff syndrome of shoulder, disorder of bursae and tendons in shoulder region, unspecified |
| 726.11 | Calcifying tendinitis of shoulder |
| 726.19 | Other specified rotator cuff syndrome of shoulder and allied disorders |
| 727.61 | Complete rupture of rotator cuff, nontraumatic |
| 840.4 | Sprains and strains of rotator cuff |
ICD-9 = International Classification of Diseases, Ninth Revision.
For 1996, the NSAS database produced a national estimation of 21,236,913 ambulatory surgical procedures of which 58,846 (0.3%) were estimated to be rotator cuff repairs. For 2006, the national estimate was 34,738,440 ambulatory surgical procedures of which 272,148 (0.8%) were rotator cuff repairs. There were 34,470,485 inpatient hospitalizations in 1996 and 50,754 (0.15%) inpatient rotator cuff repairs based on the NHDS database. In 2006, the number of inpatient hospitalizations increased to 38,873,777 while the number of inpatient rotator cuff repairs decreased to 20,433 (0.05%).
Statistics
We used the SAS survey procedures (SAS Institute, Cary, North Carolina) to estimate the variance of data regarding the number of rotator cuff repairs and the number of ambulatory medical visits with a diagnosis related to rotator cuff tears. The analysis took into account survey design, including sampling weights, primary sample units, stratification, and clustering. Univariate analyses were conducted with use of t tests for continuous variables and the chi-square test for dichotomous variables (i.e., sex, comorbidities, insurance status, anesthesia type, and surgical intervention). Significance was expressed as both probability values and 95% confidence interval (CI). Values of p < 0.05 were considered significant. Data sets were analyzed with SAS version 9.13 statistical software (SAS Institute).
We used a direct adjustment procedure to account for changes in sex and age in the U.S. population over time. The U.S. population in 2000 was selected as the standard population. The age and sex-adjusted rates were calculated by applying the age-specific and sex-specific rates to the standard population and dividing by the total in the standard population. Rates adjusted for age and sex were presented as the number of rotator cuff repairs per 100,000 standard population.
Source of Funding
No external funding source was used for this study.
Results
There was a substantial growth in the number of medical visits for shoulder pain over the ten-year study period: visits increased from 1070 per 100,000 population in 1996 to 1524 per 100,000 population in 2006. Furthermore, there was an increase in the number of rotator cuff surgical procedures performed per visit for shoulder pain. In 1996, there were twenty-six nonsurgical visits per one rotator cuff repair, and, in 2006, there were sixteen visits per one rotator cuff repair.
The use of both open and arthroscopic repairs increased substantially during the decade of study (Fig. 1). Open repairs increased by 34% (from approximately thirty-two per 100,000 population in 1996 to approximately forty-three per 100,000 population in 2006), while arthroscopic repairs increased by 600% (from approximately eight per 100,000 population in 1996 to approximately fifty-eight per 100,000 population in 2006). Overall, there was a 141% increase in the number of rotator cuff repairs performed (from approximately forty-one per 100,000 population in 1996 to approximately ninety-eight per 100,000 population in 2006).
Fig. 1.
Comparison of volume of open and arthroscopic rotator cuff repairs in 1996 and 2006.
With use of the U.S. population in 2000 as a control, the age and sex-adjusted rates for rotator cuff repairs are shown in Table III. After excluding the impact of changes in population structure over the decade on the rates of rotator cuff repairs, there was an overall 115% increase in the number of rotator cuff repairs performed. Open repairs increased by 21%, while arthroscopic repairs increased by 530%.
TABLE III.
Observed and Adjusted Rates of Rotator Cuff Repair in 1996 and 2006 with Use of the U.S. Population in 2000 as the Control
| Observed Rate |
Adjusted Rate |
Percent Change for Adjusted Rates (2006 vs. 1996) | |||
| 1996 | 2006 | 1996 | 2006 | ||
| Inpatient | |||||
| Men | 22.04 | 7.12 | 23.20 | 6.62 | –71% |
| Women | 15.78 | 6.58 | 16.34 | 6.32 | –61% |
| Overall | 18.84 | 6.85 | 19.71 | 6.47 | –67% |
| Ambulatory | |||||
| Men | 31.41 | 103.06 | 32.97 | 96.99 | 194% |
| Women | 12.68 | 79.72 | 13.23 | 74.08 | 460% |
| Overall | 21.84 | 91.21 | 22.91 | 85.32 | 272% |
| Inpatient and ambulatory combined | |||||
| Men | 53.44 | 110.19 | 56.16 | 103.62 | 84% |
| Women | 28.46 | 86.30 | 29.57 | 80.40 | 172% |
| Overall | 40.68 | 98.06 | 42.62 | 91.79 | 115% |
| Arthroscopic rotator cuff repair | |||||
| Men | 11.18 | 61.19 | 11.67 | 57.37 | 392% |
| Women | 5.50 | 54.77 | 5.62 | 51.03 | 808% |
| Overall | 8.28 | 57.93 | 8.59 | 54.14 | 530% |
| Open rotator cuff repair | |||||
| Men | 41.58 | 48.82 | 43.80 | 46.40 | 6% |
| Women | 22.90 | 37.13 | 23.89 | 35.33 | 48% |
| Overall | 32.04 | 42.89 | 33.66 | 40.76 | 21% |
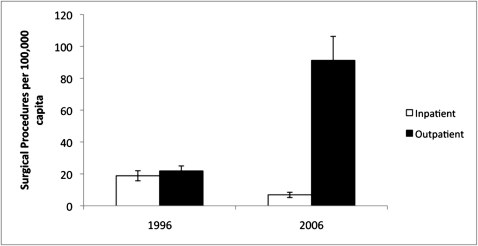
As the total number of procedures performed during the decade increased, there was substantial growth of the number of surgical procedures performed in an ambulatory surgery setting. The observed rate of outpatient surgical procedures more than quadrupled during the decade (from twenty-two to ninety-one per 100,000 capita) while inpatient surgical procedures decreased 63%, from nineteen per 100,000 to seven per 100,000 capita (Fig. 2). This increase in outpatient surgery centers correlated with the shift from open surgery to arthroscopic surgery. In fact, the rate of arthroscopic surgery in outpatient centers increased from six per 100,000 population in 1996 to fifty-four per 100,000 population in 2006.
Fig. 2.
Comparison of volume of inpatient versus outpatient rotator cuff repairs in 1996 and 2006.
As would be expected, the patients who had inpatient surgery had significantly more comorbidities (diabetes [p = 0.007], hypertension [p < 0.0001], chronic obstructive pulmonary disease [p < 0.0001], and coronary artery disease [p = 0.0002]) than the ambulatory surgery group had.
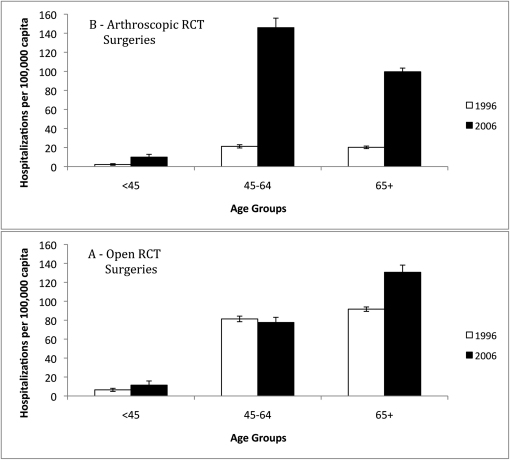
Several trends were seen with age (Fig. 3). The total number of open repairs increased both for patients who were younger than forty-five years (from six to eleven repairs per 100,000 capita younger than forty-five years of age) and those who were sixty-five years of age or older (from ninety-two to 131 patients per 100,000 capita sixty-five years of age or older). For the age group from forty-five to sixty-four years old, open repairs actually decreased during this period of time (from eighty-one to seventy-seven per 100,000 capita age forty-five to sixty-four years). During this same period of time, the number of arthroscopic repairs increased among all age groups. For those who were younger than forty-five years, the increase was from two to ten per 100,000 capita, for those who were forty-five to sixty-four years of age, the increase was from twenty-one to 146 per 100,000 capita, and for those who were sixty-five years or older, the increase was from twenty to ninety-nine per 100,000 capita.
Fig. 3.
Comparison of volume of open (Fig. 3-A) and arthroscopic (Fig. 3-B) rotator cuff repairs by age group in 1996 and 2006. RCT = rotator cuff tear.
In general, patients who underwent ambulatory surgery were younger than those who had an inpatient procedure (57.3 years old versus 61.6 years old, p = 0.002) and the age difference increased over time; in 1996, the difference in average age was three years (57.4 vs. 60.4, p = 0.065) and in 2006, it was approximately seven years (57.2 years old versus 64.5 years old, p = 0.0003). In general, female patients who underwent rotator cuff repair were significantly older than their male counterparts (average age, 60.6 years for women and 56.1 years for men; p = 0.0034). This was reflected in both inpatients (average age, 65.4 years for women and 58.5 years for men; p = 0.0006) and ambulatory patients (average age, 59.5 years for women and 55.7 years for men, p = 0.0315). However, there was a trend toward increasing age among men who underwent inpatient repair (average age, 56.3 years in 1996 compared with 64.7 years in 2006, p = 0.0128).
Overall, there were more men than women who underwent rotator cuff repair; however, this difference diminished over the decade. Ambulatory surgery in 1996 revealed a dramatic difference, with women representing just 29.7% of the patients and men representing 70.3% of the patients. However, sex disparities have decreased over time. By 2006, 44.4% of patients who underwent ambulatory rotator cuff repair were women and 55.6% were men. Interestingly, the sex difference in 1996 was far less among patients who had an inpatient procedure: 42.8% of the patients were women and 57.2% were men. This difference narrowed further in 2006, when 48.8% of the patients were women and 51.2% were men.
We were able to examine surgical, operating room, and post-anesthesia care unit (PACU) time for ambulatory patients in 2006. Surgical time was defined as time from the first incision to the time of wound closure, operating room time was defined as total time that the patient spent in the operating room, and PACU time was defined as the time that the patient spent in the recovery room until discharge. We observed a significantly longer surgical time when the arthroscopic technique was used (eighty-four minutes; 95% CI = seventy-six to ninety-two minutes) as compared with when the open technique was used (sixty-six minutes; 95% CI = fifty-seven to seventy-five minutes) (p = 0.0047). Operating room time for arthroscopic procedures (120 minutes; 95% CI = 111 to 129 minutes) as compared with open procedures (104 minutes; 95% CI = ninety-two to 117 minutes) (p = 0.0454) was also significantly longer. However, no notable difference was detected in the amount of time in the PACU for either technique: the average time for an arthroscopic technique was 107 minutes (95% CI = ninety-four to 120 minutes), and the average time for the open technique was 100 minutes (95% CI = eighty-six to 114 minutes) (p = 0.464).
Over the decade, there was a significant increase in the use of general anesthesia supplemented by a regional nerve block for open procedures (from 3.07% of patients in 1996 to 14.55% of patients in 2006, p = 0.0164). During that same time period, the use of general anesthesia alone decreased significantly (from 83.68% to 68.42% of patients, p = 0.0355). When examined together, anesthesia for arthroscopic and open procedures demonstrated significant increases in the use of combined general anesthesia and a regional nerve block (from 3.79% to 15.42% of patients over the ten-year period examined [p = 0.0072]). The databases were examined for patients who underwent surgery with regional anesthesia alone; however, the numbers were too small to identify any trends.
Discussion
The number of visits for rotator cuff pathology increased from 1996 to 2006, as did the ratio of subsequent surgical procedures performed per visit. This overall increase in repairs was seen for both open and arthroscopic procedures. Interestingly, the number of open repairs increased for patients who were younger than forty-five years of age. However, there was a much greater increase in the number of arthroscopic repairs, and this increase was seen across all age groups. The number of surgical procedures performed in an ambulatory setting also increased, with a concomitant decrease in inpatient surgery. As would be expected, inpatients tended to be older and had more comorbidities.
The popularization and expansion of outpatient surgery centers have been seen in recent years, and some have questioned the effect that this trend will have on larger hospitals. Some have reported concern for the demand placed on hospitals to care for only the sickest patients needing advanced care14. The findings of this study may support such a concern.
There are several possible reasons for the increase in rotator cuff repairs. First, the complexion of the U.S. population is changing. With medical advances, patients are living longer, and a larger percentage of our population is in the elderly demographic (by 2030, approximately 20% of the population will be sixty-five years of age or older)15. Older age has clearly been associated with an increase in the prevalence of rotator cuff tears16,17, and our age-adjusted numbers were consistent with this observation. However, an increase in arthroscopic repairs and a decrease in inpatient surgical procedures were also seen with rate-adjusted numbers, reflecting a change in practice. Surgeons have become more aggressive with regard to early surgical repair after the results of studies demonstrated that older age18,19 and larger tear size20 are associated with failure to heal after rotator cuff repair. In addition, a recent study found that, even with a successful repair, preoperative muscle atrophy and fatty infiltration did not improve, and muscle atrophy played an important role in postoperative functional outcomes21. In patients with symptomatic rotator cuff tears, an asymptomatic tear in the contralateral shoulder is likewise at risk of size and symptom progression with time22. Furthermore, arthroscopy enables the diagnosis and repair of lesions (e.g., partial-thickness rotator cuff tears and upper-margin subscapularis tears) that may not have been as commonly addressed with open surgery.
The dramatic increase in arthroscopic repairs could be influenced by several factors. First, there have been dramatic improvements in both surgical instrumentation and technique that facilitate arthroscopic repair. Younger surgeon age, higher volume of shoulder arthroscopies, and higher volume of rotator cuff repairs have also been associated with significantly higher rates of arthroscopic repair23. Fellowship-trained shoulder and sports-medicine surgeons are also more likely to perform arthroscopic repairs than those whose training was limited to orthopaedic residency23.
With the evolution of advanced arthroscopic techniques, there no longer exists a “gold standard” method for rotator cuff repair. The advantages of arthroscopic as compared with mini-open repair include the ability to mobilize and release the rotator cuff, decreased surgical insult to the deltoid muscle, improved ability to evaluate and treat pathology of the glenohumeral joint, improved visualization, decreased immediate postoperative pain, decreased postoperative stiffness, and no limitation in the size of the tear that can be addressed24. Open repair allows the surgeon to perform tendon transfers. There is consensus that functional outcome after rotator cuff repair is dependent on the integrity of the repair1,25-27. Even with experienced surgeons performing the repair, recurrent tears of the rotator cuff have been reported after both open25-27 and arthroscopic repairs20. Recent studies have failed to demonstrate a difference in functional outcome scores or complications between the two procedures2.
In our study, arthroscopic repairs were associated with a significantly longer surgical and operating-room time than open repairs were. The longer operating-room time seen with arthroscopic repair is consistent with the findings of previous studies28. The longer surgical time of arthroscopic repairs is attributable to several factors. Arthroscopic rotator cuff repair demands a high level of technical skill, which is associated with a steep learning curve. Guttmann et al. found that the arthroscopic rotator cuff repair time per procedure was significantly longer (mean time plus standard deviation, 96.5 ± 38.7 minutes) in the first ten procedures performed by a single surgeon than it was in the second ten procedures (48.4 ± 35.5 minutes, p < 0.05) performed by that same surgeon29. A significant decrease in operative time occurred as the number of arthroscopic rotator cuff repairs performed increased.
Anesthesia for rotator cuff repairs has likewise evolved. Over the ten-year time period, there was an increase in the number of surgical procedures performed under general anesthesia supplemented with a regional block. An interscalene block has been shown to be a safe and cost-effective method of pain control for shoulder surgery when compared with general anesthesia4,30-32.
Drawing inferences from large datasets about clinical activities has limitations. One in particular is lack of clinical detail. Procedure codes are very general and do not differentiate between partial and full-thickness rotator cuff tears, nor do they distinguish tears by size or duration of time since injury. Thus, we are unable to comment on time from presentation to surgery. Furthermore, there is not enough detail for us to determine if the office visit took place preoperatively or postoperatively. We are also unable to determine which cases were associated with the performance of a mini-open technique and if there were any concomitant procedures (e.g., biceps tenotomy or tenodesis) performed at the time of the arthroscopic procedure. The potential for inaccuracies with coding in a large database also exists33. Nonetheless, we believe that our results highlight important trends in rotator cuff surgery. There has been a shift in practice from open rotator cuff surgery performed in an inpatient setting to arthroscopic surgery performed in an outpatient setting. Interestingly, both age and sex affect aspects of surgical intervention. Although it has been reported that women report more disability with lower or similar levels of pathology compared with men34, women tend to be older than men when they undergo surgery for a rotator cuff repair. Women were also less likely than men to have arthroscopic surgery performed as an outpatient. Future studies could help elucidate which variables are responsible for this difference in utilization of surgical intervention to ensure that appropriate education and access to care are available to all patients.
Footnotes
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. One or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Bishop J, Klepps S, Lo IK, Bird J, Gladstone JN, Flatow EL. Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Shoulder Elbow Surg. 2006;15:290-9 [DOI] [PubMed] [Google Scholar]
- 2.Morse K, Davis AD, Afra R, Kaye EK, Schepsis A, Voloshin I. Arthroscopic versus mini-open rotator cuff repair: a comprehensive review and meta-analysis. Am J Sports Med. 2008;36:1824-8 [DOI] [PubMed] [Google Scholar]
- 3.Yamaguchi K, Levine WN, Marra G, Galatz LM, Klepps S, Flatow EL. Transitioning to arthroscopic rotator cuff repair: the pros and cons. Instr Course Lect. 2003;52:81-92 [PubMed] [Google Scholar]
- 4.Bishop JY, Sprague M, Gelber J, Krol M, Rosenblatt MA, Gladstone J, Flatow EL. Interscalene regional anesthesia for shoulder surgery. J Bone Joint Surg Am. 2005;87:974-9 [DOI] [PubMed] [Google Scholar]
- 5.Apreleva M, Ozbaydar M, Fitzgibbons PG, Warner JJ. Rotator cuff tears: the effect of the reconstruction method on three-dimensional repair site area. Arthroscopy. 2002;18:519-26 [DOI] [PubMed] [Google Scholar]
- 6.Park MC, Cadet ER, Levine WN, Bigliani LU, Ahmad CS. Tendon-to-bone pressure distributions at a repaired rotator cuff footprint using transosseous suture and suture anchor fixation techniques. Am J Sports Med. 2005;33:1154-9 [DOI] [PubMed] [Google Scholar]
- 7.Park MC, ElAttrache NS, Tibone JE, Ahmad CS, Jun BJ, Lee TQ. Part I: footprint contact characteristics for a transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007;16:461-8 [DOI] [PubMed] [Google Scholar]
- 8.Gerber C, Schneeberger AG, Beck M, Schlegel U. Mechanical strength of repairs of the rotator cuff. J Bone Joint Surg Br. 1994;76:371-80 [PubMed] [Google Scholar]
- 9.Gerber C, Schneeberger AG, Perren SM, Nyffeler RW. Experimental rotator cuff repair. A preliminary study. J Bone Joint Surg Am. 1999;81:1281-90 [DOI] [PubMed] [Google Scholar]
- 10.Vitale MG, Krant JJ, Gelijns AC, Heitjan DF, Arons RR, Bigliani LU, Flatow EL. Geographic variations in the rates of operative procedures involving the shoulder, including total shoulder replacement, humeral head replacement, and rotator cuff repair. J Bone Joint Surg Am. 1999;81:763-72 [DOI] [PubMed] [Google Scholar]
- 11.Green LB, Pietrobon R, Paxton E, Higgins LD, Fithian D. Sources of variation in readmission rates, length of stay, and operative time associated with rotator cuff surgery. J Bone Joint Surg Am. 2003;85:1784-9 [DOI] [PubMed] [Google Scholar]
- 12.Dunn WR, Schackman BR, Walsh C, Lyman S, Jones EC, Warren RF, Marx RG. Variation in orthopaedic surgeons’ perceptions about the indications for rotator cuff surgery. J Bone Joint Surg Am. 2005;87:1978-84 [DOI] [PubMed] [Google Scholar]
- 13.CDC Population Information. 2009. http://wonder.cdc.gov/population.html. Accessed 2010 Oct
- 14.Sloss EM, Fung C, Wynn BO, Ashwood JS, Stoto MA. Further analyses of Medicare procedures provided in multiple ambulatory settings. 2006. http://www.medpac.gov/documents/OCT06_Multiple_Ambulatory_CONTRACTOR.pdf. Accessed 2010 Oct
- 15.National Institute on Aging Dramatic changes in U.S. aging highlighted in new census, NIH report. 2006. Mar 9. www.nia.nih.gov/NewsAndEvents/PressReleases/PR2006030965PlusReport.htm. Accessed 2010 Oct
- 16.Kim HM, Teefey SA, Zelig A, Galatz LM, Keener JD, Yamaguchi K. Shoulder strength in asymptomatic individuals with intact compared with torn rotator cuffs. J Bone Joint Surg Am. 2009;91:289-96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88:1699-704 [DOI] [PubMed] [Google Scholar]
- 18.Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87:1229-40 [DOI] [PubMed] [Google Scholar]
- 19.Kamath G, Galatz LM, Keener JD, Teefey S, Middleton W, Yamaguchi K. Tendon integrity and functional outcome after arthroscopic repair of high-grade partial-thickness supraspinatus tears. J Bone Joint Surg Am. 2009;91:1055-62 [DOI] [PubMed] [Google Scholar]
- 20.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86:219-24 [DOI] [PubMed] [Google Scholar]
- 21.Gladstone JN, Bishop JY, Lo IK, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007;35:719-28 [DOI] [PubMed] [Google Scholar]
- 22.Yamaguchi K, Tetro AM, Blam O, Evanoff BA, Teefey SA, Middleton WD. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001;10:199-203 [DOI] [PubMed] [Google Scholar]
- 23.Vitale MA, Kleweno CP, Jacir AM, Levine WN, Bigliani LU, Ahmad CS. Training resources in arthroscopic rotator cuff repair. J Bone Joint Surg Am. 2007;89:1393-8 [DOI] [PubMed] [Google Scholar]
- 24.Yamaguchi K, Ball CM, Galatz LM. Arthroscopic rotator cuff repair: transition from mini-open to all-arthroscopic. Clin Orthop Relat Res. 2001;390:83-94 [PubMed] [Google Scholar]
- 25.Gazielly DF, Gleyze P, Montagnon C. Functional and anatomical results after rotator cuff repair. Clin Orthop Relat Res. 1994;304:43-53 [PubMed] [Google Scholar]
- 26.Harryman DT, 2nd, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA., 3rd Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 1991;73:982-9 [PubMed] [Google Scholar]
- 27.Thomazeau H, Boukobza E, Morcet N, Chaperon J, Langlais F. Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Orthop Relat Res. 1997;344:275-83 [PubMed] [Google Scholar]
- 28.Churchill RS, Ghorai JK. Total cost and operating room time comparison of rotator cuff repair techniques at low, intermediate, and high volume centers: mini-open versus all-arthroscopic. J Shoulder Elbow Surg. 2010. Feb 4 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 29.Guttmann D, Graham RD, MacLennan MJ, Lubowitz JH. Arthroscopic rotator cuff repair: the learning curve. Arthroscopy. 2005;21:394-400 [DOI] [PubMed] [Google Scholar]
- 30.Bishop JY, Sprague M, Gelber J, Krol M, Rosenblatt MA, Gladstone JN, Flatow EL. Interscalene regional anesthesia for arthroscopic shoulder surgery: a safe and effective technique. J Shoulder Elbow Surg. 2006;15:567-70 [DOI] [PubMed] [Google Scholar]
- 31.Gonano C, Kettner SC, Ernstbrunner M, Schebesta K, Chiari A, Marhofer P. Comparison of economical aspects of interscalene brachial plexus blockade and general anaesthesia for arthroscopic shoulder surgery. Br J Anesth. 2009;103:428-33 [DOI] [PubMed] [Google Scholar]
- 32.Brown AR, Weiss R, Greenberg C, Flatow EL, Bigliani LU. Interscalene block for shoulder arthroscopy: comparison with general anesthesia. Arthroscopy. 1993;9:295-300 [DOI] [PubMed] [Google Scholar]
- 33.Fisher ES, Whaley FS, Krushat WM, Malenka DJ, Fleming C, Baron JA, Hsia DC. The accuracy of Medicare's hospital claims data: progress has been made, but problems remain. Am J Public Health. 1992;82:243-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Razmjou H, Davis AM, Jaglal SB, Holtby R, Richards RR. Cross-sectional analysis of baseline differences of candidates for rotator cuff surgery: a sex and gender perspective. BMC Musculoskeletal Disord. 2009;24:10-26 [DOI] [PMC free article] [PubMed] [Google Scholar]