Abstract
Metastatic lesions in the superior vena cava and the right atrium are difficult to diagnose: in computed tomography (CT), they are easily misinterpreted as artifacts, and the same region may be difficult to access using echocardiography. We present a case of asymptomatic metastasis of a malignant melanoma which was overlooked initially due to deficiencies in imaging. Using 18F-fluorodeoxyglucose positron emission tomography-CT, the metastasis was clearly identified and finally treated successfully. We discuss the diagnostic value of the various imaging modalities for intracardiac masses.
Keywords: Cardiac metastasis, Staging, Computed tomography, Positron emission tomography
INTRODUCTION
The incidence of primary melanomas has increased significantly[1,2]. In autopsy studies, cardiac metastases are shown to be frequent in malignant melanoma (MM) patients[3]. However, in vivo, the diagnosis is rarely established. Early stages are usually asymptomatic whereas the occurrence of hemodynamic symptoms often indicates inoperability. Follow-up in melanoma patients usually includes whole body computed tomography (CT) examination. In CT scans, however it may be difficult to identify small cardiac masses due to artifacts secondary to movement and contrast media inflow. In this report we compared different imaging modalities and describe the successful diagnosis and treatment of an asymptomatic metastasis of the right heart.
CASE REPORT
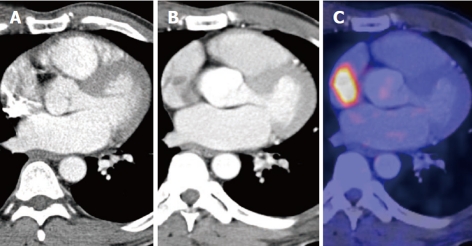
We report the case of a 41-year-old Caucasian with a metastasis in the superior vena cava (SVC). Five years prior to admission, the patient was diagnosed with MM of the left foot. He experienced a 2-year history of recurrent isolated metastases in the ipsilateral groin lymph nodes. Each time the tumors were excised successfully. During his follow-up the patient was asymptomatic and in excellent physical condition. In a whole body contrast-enhanced CT scan, a metastatic lymph node localized near the left common iliac artery was the only pathological finding. An additional 18F-fluorodeoxyglucose positron emission tomography-CT (FDG PET-CT) examination however, showed a high tracer uptake in the SVC close to the right atrium (RA) (Figure 1C). This lesion was not seen in the initial CT scanning due to artifacts caused by contrast media inflow (Figure 1A), but suspected in a CT-scan of better quality (Figure 1 B). Magnetic resonance imaging (MRI,
Figure 1.
Computed tomography scan. A: Initial computed tomography (CT) scan, with artifacts in the right atrium; B: CT of better quality; C: 18F-fluorodeoxyglucose positron emission tomography-CT with specific tracer accumulation.
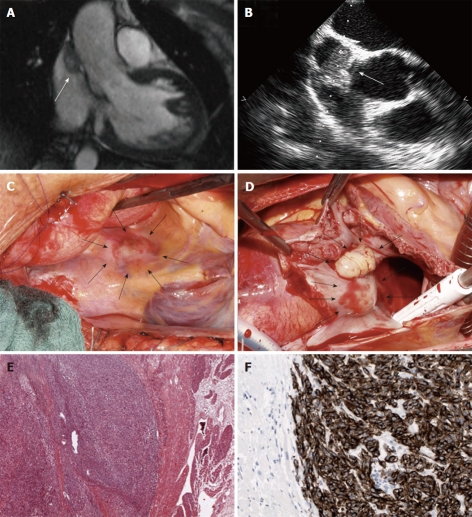
Figure 2A) and transesophageal echocardiography (TEE, Figure 2B) demonstrated a soft tissue nodule in the superior cavo-atrial junction corresponding to the area of PET-CT tracer uptake whereas the tumor was not visible during transthoracic echocardiography (TTE). A combined surgical approach was chosen including resection of the iliac lymph node and the cardiac lesion. Following median sternotomy, the tumor was identified at the superior cavo-atrial confluence. It was completely excised within healthy tissue margins using cardiopulmonary bypass of the beating heart with venous cannulae in the deep jugular and inferior caval veins. The tissue defect was patched with autologous pericardium (Figure 2C and D). The recovery was uneventful and the patient was discharged 7 d after surgery. Histology confirmed a cardiac metastasis of MM (Figure 2E and F).
Figure 2.
Tumor imaging and histology. Magnetic resonance imaging (A) and transesophageal echocardiography (B) showing the tumor in the inflow of the right atrium. Intraoperative views of the superior vena cava from the outside (C) and the inside (D); Histologic examination reveals intracardiac metastasis of a malignant melanoma (E, F). Arrows indicate tumor localization.
DISCUSSION
The present case demonstrates potential deficiencies in the diagnosis of cardiac masses. In particular, lesions in the SVC and the RA are easily overlooked or misinterpreted as artifacts in CT. Moreover, the same region may be difficult to access using TTE. On the other hand, PET-CT, MRI and TEE are expensive and of limited availability. However, one should consider the diagnostic values of the various imaging modalities for specific lesions. In the present case, FDG PET-CT scanning revealed the presence of an asymptomatic cardiac metastasis with significant impact on the therapeutic strategy and possibly on patient survival. FDG PET-CT may be a helpful imaging technique for diagnosis and follow-up, especially in patients with melanoma and other malignancies[4,5], in order to detect or exclude additional metastases, particularly in otherwise asymptomatic patients.
Footnotes
Peer reviewer: Tomás F Cianciulli, MD, FACC, Professor, Director, Echocardiography Laboratory, Division of Cardiology, Hospital of the Government of the City of Buenos Aires “Dr. Cosme Argerich”, C1155AHB Buenos Aires, Argentina
S- Editor Cheng JX L- Editor Cant MR E- Editor Zheng XM
References
- 1.Bichakjian CK, Halpern AC, Johnson TM, Foote Hood A, Grichnik JM, Swetter SM, Tsao H, Barbosa VH, Chuang TY, Duvic M, et al. Guidelines of care for the management of primary cutaneous melanoma. American Academy of Dermatology. J Am Acad Dermatol. 2011;65:1032–1047. doi: 10.1016/j.jaad.2011.04.031. [DOI] [PubMed] [Google Scholar]
- 2.Chakera AH, Hesse B, Burak Z, Ballinger JR, Britten A, Caracò C, Cochran AJ, Cook MG, Drzewiecki KT, Essner R, et al. EANM-EORTC general recommendations for sentinel node diagnostics in melanoma. Eur J Nucl Med Mol Imaging. 2009;36:1713–1742. doi: 10.1007/s00259-009-1228-4. [DOI] [PubMed] [Google Scholar]
- 3.Klatt EC, Heitz DR. Cardiac metastases. Cancer. 1990;65:1456–1459. doi: 10.1002/1097-0142(19900315)65:6<1456::aid-cncr2820650634>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 4.Czernin J, Allen-Auerbach M, Schelbert HR. Improvements in cancer staging with PET/CT: literature-based evidence as of September 2006. J Nucl Med. 2007;48 Suppl 1:78S–88S. [PubMed] [Google Scholar]
- 5.Dummer R, Hauschild A, Guggenheim M, Jost L, Pentheroudakis G. Melanoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21 Suppl 5:v194–v197. doi: 10.1093/annonc/mdq188. [DOI] [PubMed] [Google Scholar]