Corneal inflammation is a critical facet of many pathologic conditions. Attempts to control ocular inflammation with corticosteroids are associated with well-known serious complications such as ocular hypertension and cataracts. Azithromycin (AZM), a broad-spectrum macrolide antibiotic, has been reported to have anti-inflammatory and immunomodulatory activities. However, to date, the anti-inflammatory properties of AZM have not been studied or characterized in ocular tissues.
Abstract
Purpose.
To determine the effect of azithromycin (AZM) in a murine model of corneal inflammation.
Methods.
The effect of topical AZM was studied in murine corneal inflammation. Corneal inflammation was induced by thermal cautery in BALB/c mice. Leukocyte infiltration at different time points was analyzed by flow cytometry. At set time points, real-time polymerase chain reaction was performed to quantify the expression of different inflammatory cytokine transcript in the cornea. Corneal samples were analyzed immunohistochemically for the expression of intercellular adhesion molecule-1 (ICAM-1). Corneal neovascularization (CNV) was induced by micropellet (VEGF-A) placement. Mice were then treated topically with either AZM or vehicle. CNV was evaluated morphometrically.
Results.
Eyes receiving AZM showed a significant decrease in corneal infiltration compared with the vehicle-treated group. AZM also significantly decreased messenger RNA expression levels of interleukin-1β (IL-1β), tumor necrosis factor-α (TNF-α) and ICAM-1 in the cornea. There was no significant difference in CNV between the AZM- and vehicle-treated groups.
Conclusions.
After an inflammatory insult, topical AZM significantly reduced leukocyte infiltration into the cornea. This was further supported by an associated decrease in expression of IL-1β, TNF-α, and ICAM-1 in the cornea, indicating AZM may have a potential anti-inflammatory effect on corneal inflammation.
Corneal inflammation is a critical facet of many ocular pathologies, including corneal angiogenesis and corneal allograft rejection, and a leading cause of blindness worldwide.1 Although the normal cornea is avascular and devoid of lymphatics, it has a diverse population of resident bone marrow (BM)–derived cells even in noninflamed conditions. BM-derived antigen-presenting cells (APCs) in the cornea and ocular surface comprise diverse subsets of CD45+ cells, including macrophages (CD11b+) that normally reside in the stroma and CD11c+ dendritic cells in the epithelium.2,3 Innate immunity, the major mechanism for acute inflammatory response, involves cellular trafficking into the cornea in response to traumatic, noxious, or microbial stimuli.2,4–6 Adhesion molecules and cytokines, the molecular components of innate immune responses, coordinate leukocyte migration in immunity and inflammation.3 Among cell adhesion molecules, P-selectin and E-selectin initiate the rolling stage. Then intercellular adhesion molecule-1 (ICAM-1) on vascular endothelial cells (VECs) binds to the integrin leukocyte function-associated antigen-1 (LFA-1) on leukocyte surfaces to arrest the motion of rolling leukocytes and facilitate leukocyte endothelial transmigration into the cornea.7–9
Corneal expression of proinflammatory cytokines (interleukin-1 [IL-1] and tumor necrosis factor-α [TNF-α]) and chemokines leads to the recruitment of innate immune cells and amplifies subsequent leukocyte infiltration. Leukocytes, including resident corneal APCs, can then migrate to the lymphoid compartment, where they can prime T-cell responses and mediate other immune reactions in the cornea.10,11 Resolution of inflammation may be accompanied by scarring of the cornea that can hinder visual acuity.1
Attempts to control ocular inflammation with corticosteroids are associated with well-known serious complications such as ocular hypertension and cataracts. The anti-inflammatory potential of macrolide antibiotics was first established by the effectiveness of low-dose and long-term treatment with erythromycin in diffuse panbronchiolitis.12 Azithromycin (AZM), a macrolide antibiotic, has a role in the treatment of bronchiolitis obliterans syndrome and asthma, associated with its ability to reduce airway neutrophilia.13 AZM suppresses the activation of NF-κB in tracheal aspirate cells from premature infants developing bronchopulmonary dysplasia. After NF-κB suppression, the levels of proinflammatory cytokine IL-6 and IL-8 are decreased.14 Other investigations have shown AZM to enhance the production of IL-10, an immunomodulatory cytokine, in murine dendritic cells (DCs) and naive T cells.15 Recently, the aqueous ophthalmic formulation of AZM (AzaSite, 1% azithromycin ophthalmic solution in DuraSite; Inspire Pharmaceuticals Inc., Durham, NC) was approved by the US Food and Drug Administration for the treatment of bacterial conjunctivitis. However, to date anti-inflammatory properties of AZM have not been studied or characterized in ocular tissues.
To provide information regarding the potential usefulness of AZM for ocular inflammatory diseases, we herein sought to evaluate its potential effect on corneal inflammation. We used thermal cautery, a standardized model for inducing corneal inflammation,16 and intrastromal micropellet implantation to induce corneal neovascularization. We investigated different phenotypes of leukocyte infiltration and evaluated the expression of ICAM-1 and cytokines in the AZM- and vehicle-treated groups.
Methods
Mice and Anesthesia
Male 6- to 8-week-old BALB/c (Taconic Farms, Germantown, NY) mice were used in all experiments. Each animal was deeply anesthetized with intraperitoneal injection of ketamine (120 mg/kg body weight) and xylazine (20 mg/kg body weight) mixture before all surgical procedures. Carbon dioxide inhalation was applied to euthanatize the animal before we harvested cornea. All experimental protocols were approved by the Schepens Eye Research Institute Animal Care and Use Committee, and all animals were treated in accordance with the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research.
Thermal Cautery of the Corneal Surface
To induce the mobilization of inflammatory cells into the corneal tissue, thermal cautery, a non–antigen-specific acute stimulation, was applied to the mouse corneal surface.16 Mice were anesthetized and placed under the operating microscope. Using the tip of a hand-held thermal cautery (Aaron Medical Industries Inc., St. Petersburg, FL), six light burns were applied to the central 50% of the cornea as an experimental model for corneal inflammation without associated neovascularization, as previously described,16,17 followed by the application of bacitracin-neomycin-polymyxin (Vetropolycin; Dechra Veterinary Products, Overland Park, KS) ophthalmic ointment. Mice were randomly divided into three groups receiving the following formulations topically twice daily: 1% AZM ophthalmic solution in DuraSite (AzaSite; Inspire Pharmaceuticals) or the relevant vehicle (DuraSite; InSite Vision, Inc., Alameda, CA) or prednisolone acetate 1%. All treatments were started after surgery and applied throughout the study period. Corneas were excised at days 1, 3, 7, 10, and 14 after cautery application, harvested, and assessed with studies, as described in the flow cytometry, real-time polymerase chain reaction (RT-PCR), and immunostaining sections.
Corneal Micropellet Implantation
High-dose (160 ng) VEGF-A (gift from BRB Preclinical Repository, National Cancer Institute) micropellets were prepared as previously described.18 First, an initial half-thickness linear incision was made at the center of cornea using a disposable 30° microknife (F.S.T., Foster City, CA). A lamellar pocket incision was then made parallel to the corneal plane using a Von Graefe knife (F.S.T.) and advanced to the temporal limbus at the lateral canthal area. The pellets were positioned into the pocket 1.0 mm apart from the limbal vascular arcade, and bacitracin-neomycin-polymyxin (Vetropolycin) ophthalmic ointment was applied to the eye after pellet implantation.
Flow Cytometry
Mice were killed at different times. After enucleation, corneas were harvested and pooled from BALB/c recipients (n = 5 for AZM-, prednisolone-, or vehicle-treated group per time point per experiment; n = 10 for naive per experiment) at days 1, 3, 7, 10, and 14. Corneas were digested with collagenase D (Sigma-Aldrich, St. Louis, MO) and DNase at 37°C for 50 minutes. Total cells were collected after they were passed through a mesh. On blockade by anti–FcR mAb, these cells were labeled with CY5-conjugated anti–CD-45 (catalog no. 15–0451-82; eBioscience, San Diego, CA), AlexaFluor 488 anti–CD-11b (catalog no. 557672; BD Bioscience, Franklin Lakes, NJ), FITC-conjugated anti–Gr-1 (catalog no. 11–5931-82; eBioscience), and PE-conjugated anti–CD11c (catalog no. 553802; BD Bioscience) at 4°C for 45 minutes. Cells were subsequently washed and analyzed using a flow cytometer (Epics XL; Beckman Coulter, Fullerton, CA). The percentage of these cells in the total cells of the cornea was calculated with respect to isotype control staining.
RNA Isolation and Molecular Analysis Using RT-PCR
Corneas were carefully dissected to ensure that the conjunctival and iris tissue were not included. Two corneas were pooled as a sample in each group. Each experiment was repeated three times. Five microliters of total cDNA, synthesized from 400 ng total RNA with random hexamers using reagent (Superscript III Reverse Transcriptase; Invitrogen, Carlsbad, CA), was loaded into each well, and assays were performed in duplicate. Quantitative PCR was performed (TaqMan Universal PCR Master Mix and FAM-MGB dye-labeled predesigned primers [Applied Biosystems, Foster City, CA]) for IL-10 (assay ID Mm00439616_m1), IL-6 (assay ID Mm00446190_m1), IL-1β (assay ID Mm00434228_m1), TNF-α (assay ID Mm9999068_m1), and ICAM-1 (assay ID Mm00516024_g1). PCR conditions were 2 minutes at 50°C and 10 minutes at 95°C, followed by 35 cycles at 95°C for 15 seconds and 60°C for 1 minute (ABI PRISM 7900 HT; Applied Biosystems). PCR amplification of the housekeeping gene encoding GAPDH (assay ID Mm99999915_g1) was performed during each run for each sample to allow normalization between samples. Results were analyzed by the comparative threshold cycle (CT) method. The relative expression level of each sample was expressed as fold change from normal control.
Immunohistochemical Analysis of ICAM-1
Eyes were frozen in OCT compound (Tissue-Tek; Miles, Elkhart, IN) and stored at −70°C until ready for sectioning. Monoclonal antibodies against ICAM-1 (catalog no. 116114; Biolegend) and CD31 (catalog no. Sc-18916; Santa Cruz Biotechnology, Santa Cruz, CA) were used. Corneal cryosections were rinsed in phosphate-buffered saline (PBS; pH 7.2–7.4). To block nonspecific staining, slides were incubated in 2% bovine serum albumin (BSA) in PBS. Antibodies were applied to the tissue sections overnight. Each step was followed by three thorough washings in PBS. Finally, sections were covered with mounting medium (Vector, Burlingame, CA), and the slides were analyzed and photographed with a confocal microscope.
Immunohistochemistry of Hemangiogenesis (Angiogenesis)
Five mice per group were killed at days 7 and 14 after implantation of a VEGF-A micropellet and were treated with either AZM or vehicle. Corneal flat mounts were prepared for immunohistochemical staining with FITC-conjugated CD31 (Santa Cruz Biotechnology). Digital pictures of immunostained corneal flat mounts were taken with the fluorescence microscope, and the area covered by CD31 blood vessels (BVs) was calculated using ImageJ software (developed by Wayne Rasband, National Institutes of Health, Bethesda, MD; available at http://rsb.info.nih.gov/ij/index.html). Hemangiogenesis was evaluated by measuring the percentage of the total corneal area covered by BVs.
Statistical Analysis
A two-tailed t-test was performed for analysis; P < 0.05 was deemed statistically significant. Results are presented as mean ± SEM of at least three experiments.
Results
AZM Treatment Downregulates Cell Infiltration into the Cornea
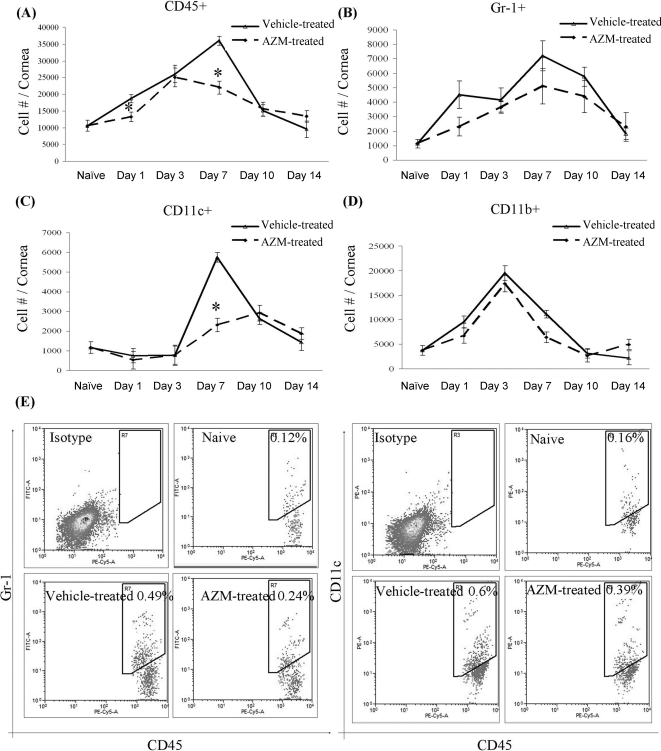
We first investigated the potential effect of AZM in suppressing the migration of leukocytes into the cornea compared with the vehicle-treated group. To accomplish this, we used corneal thermal cauterization because it is an established method to induce corneal inflammation16 and measured the infiltration of leukocytes (CD45+) by flow cytometry. We found that within 24 hours of cauterization, leukocytic infiltration into the vehicle-treated corneas was apparent and peaked by day 7 (Fig. 1A). In contrast, corneas treated with AZM led to a 30% reduction in leukocyte infiltration at day 1 and a 39% reduction at day 7 (Fig. 1A). Furthermore, to determine whether this reduced leukocyte recruitment in the AZM-treated corneas was selective for any specific leukocyte population, corneal infiltrates in the AZM- and vehicle-treated groups were analyzed by three-color flow cytometry for CD45+, Gr-1+, CD11c+, and CD11b+ cells. Analysis of the corneal infiltrate in the AZM-treated group revealed that most of the reduction in the CD45+ cells by AZM treatment was found among Gr-1+ cells and CD11c+ populations. The reduction of infiltration at day 1 predominantly consisted of neutrophils (25% reduction; Fig. 1B), whereas the reduction of infiltration at day 7 consisted primarily of CD11c+ cells (35%; Fig. 1C). CD11b+ macrophages peaked at day 3 in all groups, and there was no statistically significant difference between the AZM-treated eyes compared with the vehicle control group, though the level was modestly lower in the AZM-treated group at day 7 (6% reduction; Fig. 1D). Compared with the vehicle-treated eyes, topical prednisolone decreased CD45+ infiltration at days 3, 7, and 10 (36%, 50%, and 30%, respectively) and neutrophil infiltration by 30% at day 3, 48% at day 7, and 44% at day 10. Treatment with prednisolone also reduced CD11c+ cell infiltration by 40% and decreased macrophage infiltration at day 7 by 20%.
Figure 1.
Amelioration of corneal inflammation by topical AZM. Corneas were harvested, and single-cell suspensions were prepared and triple stained with (A) anti–CD45 PE-Cy5, (B) anti–Gr-1 FITC, (C) anti–CD11c PE, and (D) anti–CD11b FITC. (E) Representative flow cytometric data plots show CD11c+/CD45+ and Gr-1+/CD45+ cell (in all corneal cells) infiltration to the cornea at day 7 after cautery. Topical AZM treatment led to a significant decrease in total cell infiltration, specifically in CD11c+ cells. Data shown are representative of three independent experiments. Results depicted are the mean number of total cell infiltrations ± SEM.
Topical AZM Regulates Inflammatory Cytokine Expression in the Cornea
It has been shown that the proinflammatory cytokines IL-1β, TNF-α, and IL-6 are elevated in the cornea after inflammation.19–22 To determine whether the reduced infiltration afforded by AZM treatment of the inflamed cornea is reflected by altered cytokine expression, quantitative RT-PCR was used to quantify the transcripts encoding for IL-1β, TNF-α, IL-10, and IL-6 in cauterized corneas treated with either AZM or vehicle. In among-group comparisons, we found that AZM treatment led to significantly decreased expression of IL-1β at days 7 (P = 0.03) and 10 (P = 0.05; Fig. 2A). Topical therapy with AZM significantly decreased mRNA levels of TNF-α at days 1 and 7 (P = 0.03) compared with the vehicle-treated eyes (Fig. 2B).
Figure 2.
Time course of corneal cytokine expression. RT-PCR analysis showing transcript levels of IL-1β, IL-10, IL-6, and TNF-α in the cornea. Treatment with topical AZM significantly decreased relative expression of (A) IL-1β and (B) TNF-α transcripts. Corneas treated with AZM increased the expression level of (C) IL-10 at all time points. The relative expression of (D) IL-6 was variable at different time points. Horizontal line: results normalized to messenger RNA (mRNA) expression levels in the corneas of naive mice. Bars represent SEM.
In addition, treatment with topical AZM modestly increased the expression level of IL-10 compared with the vehicle-treated group; this was not statistically significant (Fig. 2C). In addition, there was no statistically significant difference between the AZM-treated eyes and vehicle-treated eyes in IL-6 expression (Fig. 2D).
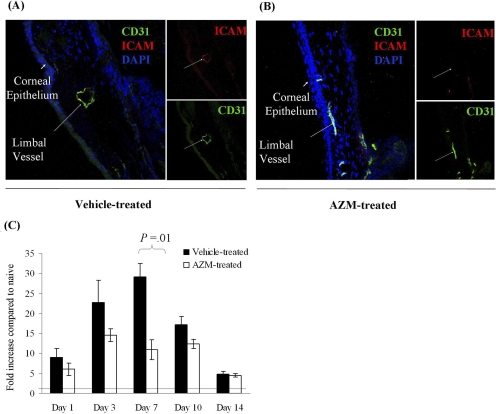
Topical Treatment with AZM Downregulates the Expression Level of ICAM-1 on Vascular Endothelial Cells
Our laboratory has shown that ICAM-1 expression by the normal limbal area of the cornea is undetectable; however, after an inflammatory insult, ICAM-1 expression was significantly upregulated.24 Given that ICAM-1 expression is critical for the mobilization of cells from the intravascular compartment to the matrix, we examined the effect of AZM on ICAM-1 expression and found that its topical application suppressed the upregulation of ICAM-1 induced in this model compared with the vehicle treatment (Fig. 3A). Furthermore, RT-PCR showed a decreased expression of ICAM-1 at all time points, though statistical significance was only achieved on day 7 (P = 0.04; Fig. 3B).
Figure 3.
Suppression of vascular endothelial cell ICAM-1 expression by AZM. Eyes of BALB/c mice were treated with topical AZM or vehicle alone after the induction of corneal inflammation. Corneal sections were immunostained with anti–ICAM-1 antibody at different time points. Seven days after corneal cauterization, limbal vessels of eyes treated with (A) vehicle alone showed significant ICAM-1 staining, in contrast to (B) AZM-treated eyes in which the vascular endothelium remained ICAM-1 negative. (C) RT-PCR analysis showed transcript levels of ICAM-1 in the cornea. Relative expression of ICAM-1 in the cornea was significantly decreased in the AZM-treated eyes at day 7. Horizontal line: normalized to mRNA expression levels in the corneas of naive mice. Bars represent SEM.
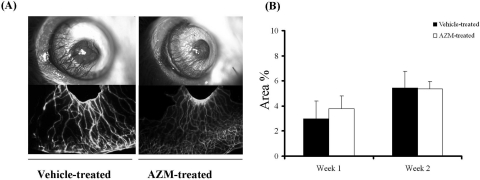
Topical AZM Does Not Suppress Corneal Neovascularization
Because the growth of blood vessels into the normally avascular corneal bed is an attribute of many forms of severe chronic corneal inflammation, we examined the effect of AZM on corneal neovascularization. Corneal angiogenesis was induced by 160 ng VEGF-A pellets, and eyes were treated with either AZM or the relevant vehicle. At days 7 and 14, mice were euthanatized and corneas were dissected around the limbus for immunohistochemical studies. The area covered by CD31hi BVs was evaluated by measuring the percentage of the total corneal area covered by BVs using ImageJ software. There was no significant difference in angiogenesis between the AZM-treated and vehicle-treated groups (Fig. 4).
Figure 4.
Analysis of corneal angiogenesis after treatment with AZM. After the induction of new blood vessels, the eyes of BALB/c mice were treated with either AZM or vehicle. Corneal whole mounts were immunostained with anti–CD31 antibody (A). The area covered by CD31hi BV was evaluated by measuring the percentage of the total corneal area covered by BV (B). Data are presented as mean ± SD.
Discussion
Visual impairment from corneal inflammation is common.1 The currently available pharmaceutical armamentarium to ameliorate corneal inflammation is principally composed of corticosteroids. Although topical corticosteroids continue to be the mainstay of treatment, their long-term use can be associated with serious side effects such as cataract formation, elevated intraocular pressure (glaucoma), opportunistic infection, and corneal thinning. Azithromycin has been reported to have nonocular anti-inflammatory and immunomodulatory activities.12–15,24–26 Given these, we hypothesized that AZM could be used as a therapeutic agent for ameliorating corneal inflammation.
Ocular surface inflammation is characterized by increased levels of inflammatory cytokines such as IL-1β, IL-6, IL-8, and TNF-α.20–23 IL-1β upregulates the expression of various cytokines that further mediate the influx of inflammatory cells. In our study, topical therapy with AZM showed a significant decrease in corneal expression of IL-1β and TNF-α. These cytokines have been involved in the pathogenesis of corneal ulceration, uveitis, and corneal transplant rejection.27,28
Our laboratory has previously shown that early expression of IL-1 by the inflamed cornea can lead to profound upregulation in the expression of ICAM-1 by the limbal vascular endothelium, which precedes the recruitment of leukocytes to the cornea.27 In our model, cauterization of the cornea led to a significant stimulation of ICAM-1 on limbal vascular endothelial cells and a time-dependent ingress of innate immune cells into the cornea.23 Interestingly, in our study, AZM treatment was effective in decreasing the corneal expression of ICAM-1 in response to an acute inflammatory insult. Our study showed that topical AZM markedly downregulated the recruitment of neutrophils and dendritic cells into the cornea. Because ICAM-1 upregulation occurs in response to inflammation, decreased leukocyte infiltration in the AZM-treated corneas may be due in part to the decreased ICAM-1 expression afforded by AZM. Accordingly, the mechanism of reduction of inflammation by AZM might be, at least in part, mediated through the suppression of IL-1β and ICAM-1 expression.
IL-6 produced by macrophages may act as both a proinflammatory and an anti-inflammatory cytokine, and it plays a regulatory role in both local and systemic acute inflammatory responses.29 Our data showed variable expression of IL-6 at different time points. These findings may be due to both the proinflammatory and the anti-inflammatory nature of IL-6.29 IL-10, an anti-inflammatory and immunoregulatory cytokine, is produced by activated macrophages and some lymphocytes. The major activities of IL-10 are to inhibit IL-1 and TNF production by macrophages and to inhibit the accessory function of APCs (including macrophages) in T-cell activation through the reduced expression of major histocompatibility complex class II.11 Consequently, IL-10 inhibits both innate and adaptive immunity. The enhanced IL-10 expression may represent a regulatory mechanism in the ocular surface to promote quiescence and maintain normal homeostasis.
Previously in our laboratory, after application of non–antigen-specific inflammatory stimulus (cauterization) to the ocular surface, IL-1 alone, TNF-α alone, or combined IL-1 and TNF-α blockade was compared to topical corticosteroid therapy in the ability to arrest the migration of antigen-presenting Langerhans cells (LCs) into the cornea. These data have shown that prednisolone and IL-1Ra are most effective in suppressing LC mobilization, with the efficacy of sTNFR nearly half that of prednisolone alone.30 In our present study, treatment with AZM reduced dendritic cell infiltration to the cornea to levels comparable to those of prednisolone. Importantly, however, the effect of treatment with prednisolone starts earlier and lasts longer than topical treatment with AZM.
The anti-inflammatory effects of topical AZM, are mixed, at least at the dose and frequency tested. Corneal angiogenesis, a common morbidity seen in chronic inflammation, which itself amplifies immunoinflammatory responses and portends a poor prognosis for transplants, was not affected by AZM treatment. This suggest that the anti-inflammatory and therapeutic benefits of AZM are rather limited for the more severe inflammatory insults to the cornea, which may require treatment with corticosteroids or other antiangiogenic therapies, such as topical anti-VEGF agents.31,32
In conclusion, treatment with topical AZM in our model of surgically induced ocular surface inflammation led to significant suppression of corneal inflammation at the molecular and cellular levels, although AZM did not show any antiangiogenic effects. The results of our study, along with the high tissue concentration and long half-life of AZM,33–36 suggest that this macrolide may be used as an antibiotic with anti-inflammatory effects in the ocular surface. Some additional investigations are required to confirm these findings in the clinical population and to more precisely define which patient subgroups are most likely to respond to topical AZM, in addition to determining the optimal dosage and duration of therapy.
Acknowledgments
The authors thank the BRB Preclinical Repository, National Cancer Institute, for providing VEGF-A.
Footnotes
Supported in part by Inspire Pharmaceuticals.
Disclosure: Z. Sadrai, None; A.R. Hajrasouliha, None; S. Chauhan, None; D.R. Saban, None; M.H. Dastjerdi, None; R. Dana, None
References
- 1. Streilein JW. Immunology and immunopathology of corneal transplantation. Chem Immunol. 1999;73:186–206 [DOI] [PubMed] [Google Scholar]
- 2. Dana MR. Corneal antigen-presenting cells: diversity, plasticity, and disguise: the Cogan lecture. Invest Ophthalmol Vis Sci. 2004;45:722–727 [DOI] [PubMed] [Google Scholar]
- 3. Delves PJ, Roitt IM. The immune system: first of two parts. N Engl J Med. 2000. 6;343:37–49 [DOI] [PubMed] [Google Scholar]
- 4. Hamrah P, Huq SO, Liu Y, Zhang Q, Dana MR. Corneal immunity is mediated by heterogeneous population of antigen presenting cells. J Leukoc Biol. 2003;74:172–178 [DOI] [PubMed] [Google Scholar]
- 5. Hamrah P, Zhang Q, Liu Y, Dana MR. Novel characterization of MHC class II–negative population of resident corneal Langerhans cell–type dendritic cells. Invest Ophthalmol Vis Sci. 2003;43:639–646 [PubMed] [Google Scholar]
- 6. Hamrah P, Zhang Q, Liu Y, Dana MR. The corneal stroma is endowed with a significant number of resident dendritic cells. Invest Ophthalmol Vis Sci. 2003;44:581–589 [DOI] [PubMed] [Google Scholar]
- 7. Biswas PS, Banerjee K, Kim B, Rouse BT. Mice transgenic for IL-1 receptor antagonist protein are resistant to herpetic stromal keratitis: possible role for IL-1 in herpetic stromal keratitis pathogenesis. J Immunol. 2004;172:3736–3744 [DOI] [PubMed] [Google Scholar]
- 8. Muller WA, Weigl SA, Deng XH, Phillips DM. PECAM-1 is required for transendothelial migration of leukocytes. J Exp Mecl. 1993;178:449–460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vaporciyan AA, DeLisser HM, Yan HC, et al. Involvement of platelet-endothelial cell adhesion molecule-1 in neutrophil recruitment in vivo. Science. 1993;262:1580–1582 [DOI] [PubMed] [Google Scholar]
- 10. Dana MR, Hamrah P. Corneal antigen-presenting cells: function and identity. In: Zierhut M, Stern ME, Sullivan DA. eds. Immunology of the Lacrimal Gland, Tear Film, and Ocular Surface. London: Taylor and Francis Group; 2005:141–149 [Google Scholar]
- 11. Baggiolini M. Chemokines in pathology and medicine. J Intern Med. 2001;250:91–104 [DOI] [PubMed] [Google Scholar]
- 12. Kudoh S, Azuma A, Yamamoto M. Improvement of survival in patients with diffuse panbronchiolitis treated with low-dose erythromycin. Am J Respir Crit Care Med. 1998;157:1829–1832 [DOI] [PubMed] [Google Scholar]
- 13. Verleden GM, Vanaudenaerde BM, Dupont LJ, Van Raemdonck DE. Azithromycin reduces airway neutrophilia and interleukin-8 in patients with bronchiolitis obliterans syndrome. Am J Respir Crit Care Med. 2006;174:566–570 [DOI] [PubMed] [Google Scholar]
- 14. Aghai ZH, Kode A, Saslow JG, et al. Azithromycin suppresses activation of nuclear factor-kappa B and synthesis of pro-inflammatory cytokines in tracheal aspirate cells from premature infants. Pediatr Res. 2007;62:483–488 [DOI] [PubMed] [Google Scholar]
- 15. Sugiyama K, Shirai R, Mukae H, et al. Differing effects of clarithromycin and azithromycin on cytokine production by murine dendritic cells. Clin Exp Immunol. 2007;147:540–546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dekaris I, Zhu SN, Dana MR. TNF-alpha regulates corneal Langerhans cell migration. J Immunol. 1999;162:4235–4239 [PubMed] [Google Scholar]
- 17. Hamrah P, Liu Y, Zhang Q, Dana MR. Alterations in corneal stromal dendritic cell phenotype and distribution in inflammation. Arch Ophthalmol. 2003;121:1132–1140 [DOI] [PubMed] [Google Scholar]
- 18. Kenyon BM, Voest EE, Chen CC, Flynn E, Folkman J, D'Amato RJ. A model of angiogenesis in the mouse cornea. Invest Ophthalmol Vis Sci. 1996;37:1625–1632 [PubMed] [Google Scholar]
- 19. Rosenbaum JT, Planck ST, Huang XN, Rich L, Ansel JC. Detection of mRNA for the cytokines, interleukin-1 alpha and interleukin-8, in corneas from patients with pseudophakic bullous keratopathy. Invest Ophthalmol Vis Sci. 1995;36:2151–2155 [PubMed] [Google Scholar]
- 20. Fukuda M, Mishima H, Otori T. Detection of interleukin-1 in the tear fluid of patients with corneal disease with or without conjunctival involvement. Jpn J Ophthalmol. 1997;41:63–66 [DOI] [PubMed] [Google Scholar]
- 21. Staats HF, Lausch RN. Cytokine expression in vivo during murine herpetic stromal keratitis: effect of protective antibody therapy. J Immunol. 1993;151:277–283 [PubMed] [Google Scholar]
- 22. Biswas PS, Banerjee K, Kim B, Kinchington PR, Rouse BT. Role of inflammatory cytokine-induced cyclooxygenase 2 in the ocular immunopathologic disease herpetic stromal keratitis. J Virol. 2005;79:10589–10600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zhu SN, Dana MR. Expression of cell adhesion molecules on limbal and neovascular endothelium in corneal inflammatory neovascularization. Invest Ophthalmol Vis Sci. 1999;40:1427–1434 [PubMed] [Google Scholar]
- 24. Culic O, Erakovic V, Parnham MJ. Anti-inflammatory effects of macrolide antibiotics. Eur J Pharmacol. 2001;429:209–229 [DOI] [PubMed] [Google Scholar]
- 25. Labro MT. Cellular and molecular effects of macrolides on leukocyte function, Curr Pharm. 2004;10:3067–3080 [DOI] [PubMed] [Google Scholar]
- 26. Tsai WC, Standiford TJ. Immunomodulatory effects of macrolides in the lung: lessons from in-vitro and in-vivo models. Curr Pharm. 2004;10:3081–3093 [DOI] [PubMed] [Google Scholar]
- 27. Dana MR, Zhu SN, Yamada J. Topical modulation of interleukin-1 activity in corneal neovascularization. Cornea. 1998;17:403–409 [DOI] [PubMed] [Google Scholar]
- 28. Connor KM, SanGiovanni JP, Lofqvist C, et al. Increased dietary intake of omega-3-polyunsaturated fatty acids reduces pathological retinal angiogenesis. Nat Med. 2007;13:868–873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Xing Z, Gauldie J, Cox G, et al. IL-6 is an antiinflammatory cytokine required for controlling local or systemic acute inflammatory responses. J Clin Invest. 1998;101:311–320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Dana R. Comparison of topical interleukin-1 versus tumor necrosis factor-alpha blockade with corticosteroid therapy on murine corneal inflammation, neovascularization, and transplant survival (AOS thesis). Trans Am Ophthalmol Soc. 2007;105:330–343 [PMC free article] [PubMed] [Google Scholar]
- 31. Dastjerdi MH, Saban DR, Okanobo A, et al. Effects of topical and subconjunctival bevacizumab (Avastin) in high-risk corneal transplant survival. Invest Ophthalmol Vis Sci. 2009;51:2411–2417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dastjerdi MH, Al-Arfaj KM, Nallasamy N, et al. Topical bevacizumab in the treatment of corneal neovascularization: results of a prospective, open-label, noncomparative study. Arch Ophthalmol. 2009;12:381–389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Liu P, Allaudeen H, Chandra R, et al. Comparative pharmacokinetics of azithromycin in serum and white blood cells of healthy subjects receiving a single-dose extended-release regimen versus a 3-day immediate-release regimen. Antimicrob Agents Chemother. 2007;51:103–109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Schentang JJ, Ballow CH. Tissue-directed pharmacokinetics. Am J Med. 1991;12:5–11 [DOI] [PubMed] [Google Scholar]
- 35. Akpek EK, Vittitow J, Verhoeven RS, et al. Ocular surface distribution and pharmacokinetics of a novel ophthalmic 1% azithromycin formulation. J Ocul Pharmacol Ther. 2009;25:433–439 [DOI] [PubMed] [Google Scholar]