Abstract
Breast conservation surgery is available to the vast majority of women with breast cancer. The combination of neoadjuvant therapies and oncoplastic surgical techniques allows even large tumours to be managed with a breast-conserving approach. The relationship between breast size and the volume of tissue to be excised determines the need for volume displacement or replacement. Such an approach can also be used in the management of carefully selected cases of multifocal or multicentric breast cancer. The role of novel techniques, such as endoscopic breast surgery and radiofrequency ablation, is yet to be precisely defined.
1. Introduction
The replacement of obligatory mastectomy, be it radical or modified radical, by simple mastectomy or wide local excision and adjuvant radiotherapy, reflected a paradigm shift in the understanding of breast cancer pathology and biology [1]. The combination of multimodal treatments, both locoregional, in the form of conservation surgery and radiotherapy, and systemic endocrine treatment and chemotherapy, has resulted in reduced postsurgical morbidity without compromising oncological outcomes [2]. The concept of downstaging tumours by means of neo-adjuvant chemotherapy or endocrine therapy is increasingly being applied to improve the chance of successful conservation surgery in the same way as it can render operable the inoperable [3, 4]. The adoption of oncoplastic surgical techniques allows larger tumours to be excised safely without compromising cosmetic outcomes. Currently, the only absolute contraindications to breast conservation relate to tumours with chest wall involvement, significant skin involvement, and patients with either extensive malignant microcalcifications or inflammatory carcinoma [5, 6]. Multifocal and multicentric tumours remain relative contraindications to attempts at breast conserving surgery. Such patients need careful counselling regarding the possible need for further surgery if excision is incomplete, and the increased risk of locoregional recurrence. Meticulous preoperative planning is essential if conservation is to be successful in this context [7]. The role of salvage breast conservation surgery in the management of local recurrence, or a metachronous primary cancer, is controversial, and should be considered with caution.
While some studies in the United States have suggested that the increasing incidence of breast cancer may have begun to level off [8], data from European countries does not reflect this change [9, 10]. Survival from breast cancer has certainly improved [11, 12], and it follows, therefore, that there are more patients alive now, having survived breast cancer, than at any other time. Aesthetic concerns and expectations are understandably higher on patients' agenda than previously and remain a source of psychological morbidity after mastectomy or if the results from breast conservation surgery are poor [12, 13]. Thus the importance of the oncoplastic approach, defined as the application of plastic surgery techniques of partial breast reconstruction at the time of breast cancer surgery, to optimising the oncological and cosmetic outcomes of breast conservation, has never been more keenly felt [14–16].
2. Optimisation of Oncological Factors
Tumours may be successfully downstaged with neoadjuvant chemotherapy and/or endocrine therapy, allowing the majority of patients to undergo breast conservation surgery [4, 17]. In this context, the decision to proceed with breast conserving surgery is guided by the clinical and radiological response to neoadjuvant therapy. Magnetic resonance imaging is superior to mammography or ultrasound in evaluating the response to neoadjuvant therapy and should be used in preference [18–20]. Whereas regimens of neoadjuvant chemotherapy usually last approximately six months, the duration of endocrine therapy in the neoadjuvant context is more varied. Although only used for three months in the IMPACT trial [21], reductions in tumour size were sufficient to allow breast conservation treatment in a large proportion. Neoadjuvant endocrine treatment is sometimes associated with a more gradual reduction in tumour size and can safely be continued for longer durations prior to undertaking curative breast conservation surgery [22].
Small lesions, which are impalpable or difficult to feel, should be localised stereotactically or by ultrasound. A number of techniques are available, utilising hookwire localisation, radioactive beads, or injection of radioisotope colloid, the latter being particularly attractive in cases where breast-conserving surgery is performed in conjunction with sentinel lymph node biopsy [23, 24].
The use of intraoperative specimen X-ray helps confirm complete excision of the radiological abnormality [25]. This has been shown to help reduce the need for further surgery because of margin positivity, as a further cavity shave may be taken intraoperatively if the specimen X-ray gives cause for concern [26].
Optimal oncological treatment demands complete excision of malignant tissues with a negative resection margin. What constitutes a negative margin is not well defined. In early studies, only margins of >1 cm were considered negative [27, 28]. A recent meta-analysis showed equivalent rates of local recurrence with margins as close as 1-2 mm [29, 30], but closer margins have been associated with rates of local recurrence similar to those seen in cases with positive margins [31, 32].
The use of intraoperative frozen section for assessment of margins, where available, is helpful in reducing the number of second procedures required to achieve clear margins [33, 34]. A further cavity shave can be taken from any margin found to be positive on intraoperative frozen section. Intraoperative touch imprint cytology can also be used as a means of margin assessment but, as with frozen section, requires the availability of an expert cytopathologist to report slides intraoperatively [35].
The role of routine cavity biopsies is controversial [36]. Hewes et al. (2009) found poor correlation between the status of the resection margin and cavity biopsies. In their series, the status of cavity biopsies was a better predictor of both breast-cancer-specific and overall survival. The two key benefits of this approach are the reduced need for second operations if the specimen margin is positive and the cavity biopsy negative and the diagnosis of otherwise occult multifocal disease, often necessitating mastectomy [37]. Conversely, it can be argued that the practice is both unnecessary, given that discontinuous small foci of disease are adequately treated by radiotherapy [28] and undesirable, as it inevitably results in the excision of more tissue than strictly necessary, having a potentially adverse effect on cosmetic outcomes.
Rates of local recurrence after breast-conserving surgery are significantly reduced by the use of adjuvant radiotherapy, giving rates of overall survival similar to those following mastectomy [38], and therefore should be viewed as a standard of care, unless distant metastases are discovered soon after surgery [39, 40]. Postoperative external beam whole-breast radiotherapy remains the most commonly used technique, although partial breast radiotherapy is possible, and may be performed intraoperatively or postoperatively, via external beam, brachytherapy, or photon emission [41–44]. There is evidence that partial breast radiotherapy may be superior in terms of cosmetic outcome [45]. This is often cited as a major advantage over whole breast radiotherapy, which is associated with a number of unfavourable cosmetic sequelae, such as breast lymphoedema, fibrosis, and shrinkage of the breast tissue, often leading to accentuation of small parenchymal defects and distortion of the nipple. However, although short-term rates of local recurrence after partial breast irradiation seem similar, long-term data (i.e., over 10 years) showing equivalence with traditional whole-breast external beam radiotherapy are not yet available. The importance of reducing rates of 5-year locoregional recurrence is emphasised by its relationship with 15-year mortality. The 20% reduction in 5-year locoregional recurrence associated with the addition of radiotherapy to breast conservation surgery corresponds to a 5% reduction in mortality at 15 years [46].
3. Optimisation of the Cosmetic Outcome after Breast Conservation Surgery
The cosmetic appearance of the breast after breast conservation surgery depends, firstly, on the relative proportion of breast volume excised in order to satisfy oncological requirements and, secondly, on the location of the tumour within the breast.
The cosmetic defect caused by excision of medial tumours, especially in the upper inner quadrant, is more pronounced than for tumours in the outer half of the breast. Estimation of the proportion of breast volume to be excised is therefore an important consideration when planning surgery [47]. Successful oncological and aesthetic outcome depends on adequate preoperative planning. Mammography and ultrasound alone may underestimate the extent of disease and fail to demonstrate multifocality. Magnetic resonance imaging is being used increasingly in this context, as it has been shown to give a more accurate estimate of the true distribution of malignancy, particularly for lobular carcinomas [48, 49].
4. Surgical Principles
Overview.
-
General principles
- choice of incision,
- avoidance of nipple deviation.
Techniques for excision of <10% of breast volume.
-
Techniques for excision of 10–20% breast volume:
- volume displacement,
- central tumours,
- peripheral tumours.
-
Techniques for excision of >20% of breast volume:
- tissue transfer.
Incisions should follow Langer's lines, semicircular, concentric to the edge of the areola, or Kraissl's lines, parallel to the horizontal skin creases. Radial incisions can be useful, but care must be taken to ensure that the nipple-areola complex is not likely to be displaced as the scar contracts during the process of wound healing and radiotherapy. A circumareolar incision can give good access to most lesions except those at the extreme periphery of the breast.
The skin overlying the cancer only needs to be excised if there are concerns regarding skin involvement, for example, if there is in-drawing of the skin or fixed dimpling. Following wide excisions, the resultant scarring and radiotherapy changes tend to cause nipple deviation towards the scar. This can be avoided by undermining the skin and disconnecting the ducts behind the nipple-areola complex. If needed, the remaining glandular tissue can also be undermined to allow rotation and approximation of tissue into the defect. If significant NAC deviation is anticipated, then de-epithelialisation of a crescent of skin from the areolar edge that is opposite to the scar and resiting the nipple to adjust for anticipated deviation often is helpful.
In general, excision of up to 10% of breast volume as a simple wide local excision gives an acceptable cosmetic result [47]. The resultant filling defect can be resolved to some degree by generously undermining the surrounding glandular tissue to allow it to fill the wide excision cavity. For those cases with defects despite breast remodelling the use of autologous fat transfer (Figures 1(a) and 1(b)) is emerging as an attractive option [50]. However, dystrophic calcification following fat necrosis may result in increased recall after screening mammography for biopsy [51].
Figure 1.
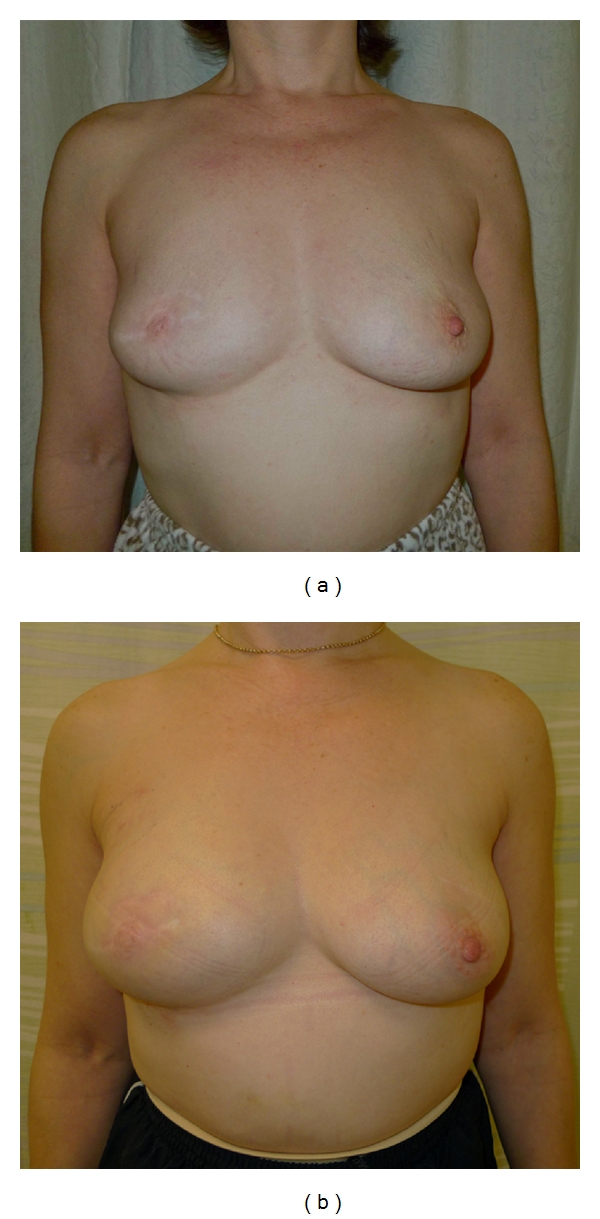
(a) This patient had previously undergone a central wide local excision and nipple reconstruction at the age of 47. Although the contour of the right breast is similar to that of the left, there is a relative lack of projection and the breast has a blunted appearance. (b) Autologous fat transfer, in the form of lipomodelling, successfully fills the defect from previous surgery. The patient also received a subdermal silicone areola prosthesis to improve projection of the reconstructed nipple.
For cancers occupying up to 20% of breast volume, some degree of volume displacement may be required to fill the defect [52]. This is achieved by mobilisation and transposition of neighbouring glandular tissue with or without overlying skin (see Table 1). Suitable patients with adequate breast volume may wish to undergo therapeutic mammoplasty [53]. Surgery to the contralateral breast may be requested to improve symmetry and may take the form of a reduction mammoplasty or mastopexy.
Table 1.
| Mammoplasty techniques for resection of 10–20% of breast volume: | |
| Glandular remodelling | |
| Inferior pedicle | |
| Superior pedicle | |
| Vertical scar | |
| Round block | |
| Grisotti flaps |
For cancers occupying 20–40% of the breast, volume displacement alone may not be sufficient and thus volume replacement by autologous tissue transfer may become necessary.
5. Optimising Cosmesis: Central Tumours Occupying 10–20% of Breast Volume
Subareolar tumours have previously been viewed as an indication for mastectomy but may be safely approached by central excision with resection of the nipple-areola complex [54, 55]. The skin wound can be closed with a purse string or horizontal suture, although this tends to reduce the projection of the breast mound. A central excision with volume displacement using a Grisotti dermoglandular flap is more appropriate for larger breasts with greater degrees of ptosis [56]. After excision of the nipple-areola complex and the underlying tumour, a dermoglandular flap is harvested from the inferolateral breast. The flap is then de-epithelialised apart from the circle of skin destined to reconstruct the nipple. Free rotation depends on the flap being freed from the prepectoral fascia. An inverted-T (WISE pattern) mammoplasty [53], excising the nipple-areola complex, is a popular alternative, with the nipple potentially being reconstructed at a later date.
For central tumours not involving the nipple-areola complex an alternate option would be the use of Benelli's round block technique (Figure 2) [57]. Concentric circles are incised around the areola, and the skin resected, allowing access to the periareolar tissue. This allows reshaping of the breast by mobilising adjacent tissue, and the skin is closed by means of a purse string suture [58]. Alternatively such tumours may be excised in combination with a batwing mastopexy, otherwise known as the omega plasty, while preserving the nipple-areola complex [59]. Briefly, semicircular incisions are made: one circumareolar and the other a short distance away, and these are joined by angled “wings” to each side of the areola. After excision of the breast lesion, the defect is closed by advancing the breast tissue and closing the skin.
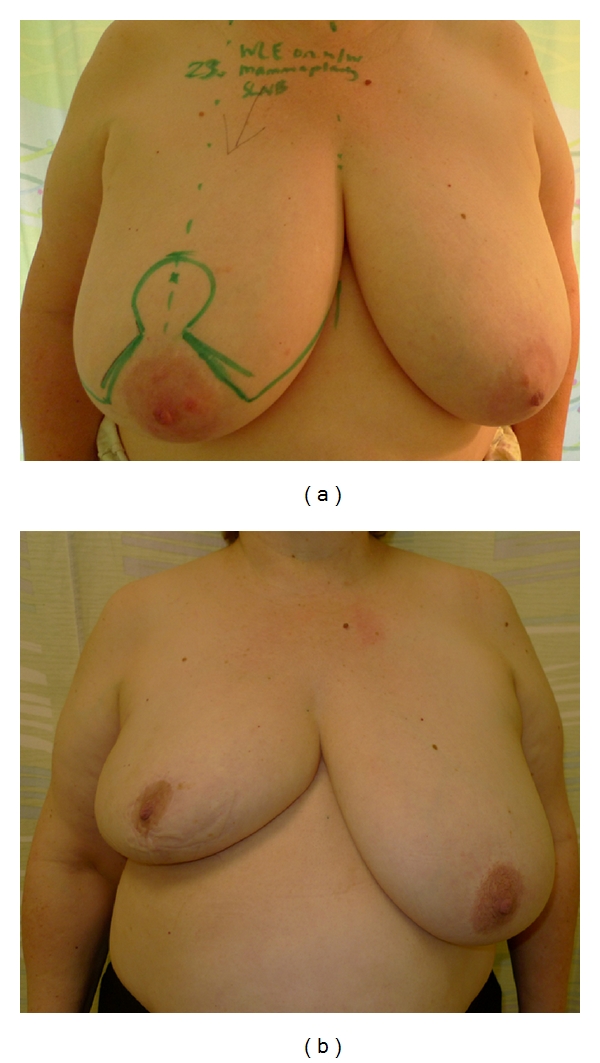
Figure 2.

This patient presented with a 1 cm tumour located in the upper inner quadrant of the right breast. The tumour was excised via a periareolar incision and the remaining breast tissue was mobilised to close the defect. The round block technique ensured that the nipple-areolar complex remained in the correct position.
6. Optimising Cosmesis: Peripheral Tumours Occupying 10–20% of Breast Volume
Different oncoplastic techniques lend themselves to excision of lesions in certain locations (see Table 2). Tumours above the nipple-areola complex may be excised and the defect filled with an inferior pedicle mammoplasty.
Table 2.
Oncoplastic techniques suitable for excision of lesions in specified locations.
| Tumour location | Oncoplastic technique |
|---|---|
| Superior to NAC | Periareolar (Benelli) mammoplasty |
| Inferior pedicle (Grisotti) mammoplasty | |
| Lateral to NAC | Lateral mammoplasty |
| Medial to NAC | Medial mammoplasty |
| Lower outer/inner quadrant | L-mammoplasty |
| J-mammoplasty | |
| Inferior to NAC | Vertical scar mammoplasty |
| Inverted T (WISE) mammoplasty | |
| Inframammary fold | IMF-plasty |
Excision of tumours in the lateral aspect of the breast: tumours inferior to the nipple-areola complex may be excised by means of a vertical mammoplasty [60, 61] or nipple-sparing inverted-T mammoplasty [53] (Figures 3(a) and 3(b)). Moderately sized tumours in the lower outer quadrant may be resected using a modified approach, sometimes referred to as the J-mammoplasty, with larger tumours excised via an inverted-T or L-mammoplasty.
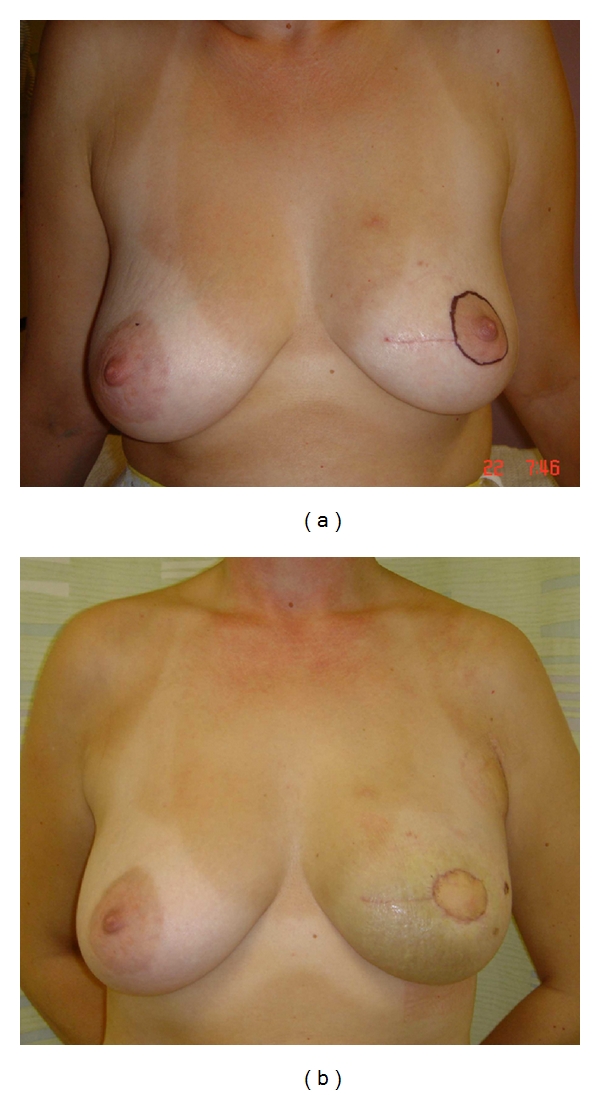
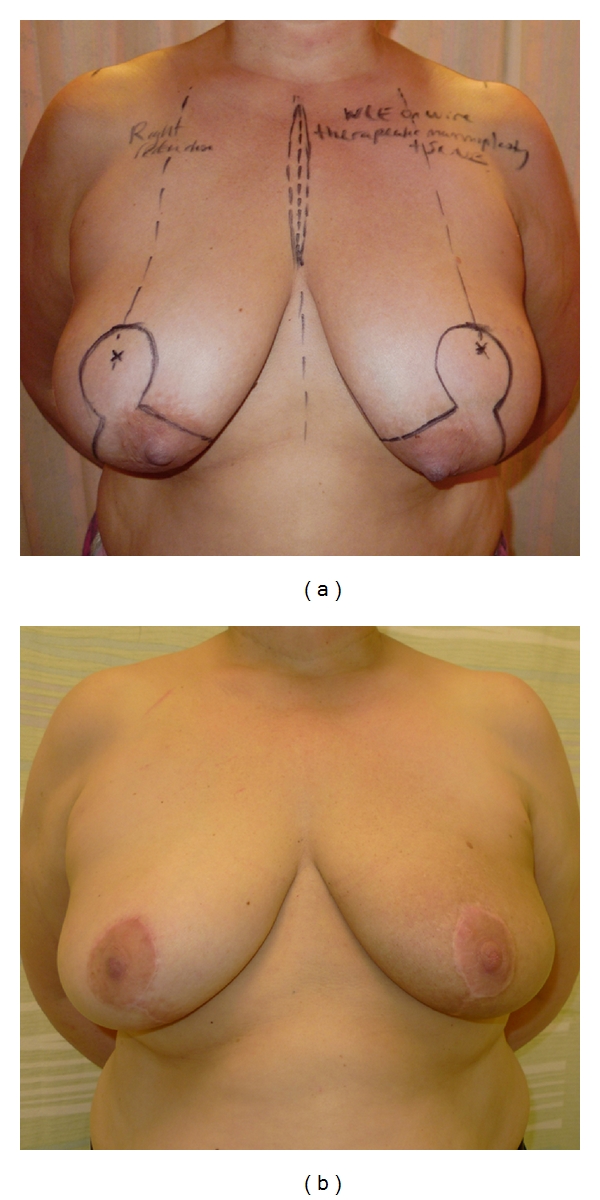
Figure 3.
(a) This 63-year-old patient with large ptotic breasts presented with a tumour in the right breast. The skin markings show the planned incisions for a therapeutic inverted-T mammoplasty. (b) Postoperative images of the same patient after completion of adjuvant chemotherapy and prior to commencing radiotherapy. The inverted-T mammoplasty gives a satisfactory result and is in proportion to the patient's body habitus. Reduction mammoplasty of the contralateral breast, to improve symmetry, is planned to be performed six months after completion of adjuvant radiotherapy.
Tumours close to the inframammary fold may be removed by excising an ellipse of skin and breast tissue and simply closing the resulting defect. Although this reduces the distance from nipple to inframammary fold, this is often not apparent in patients with preexisting ptosis.
7. Optimising Cosmesis after Extensive Excision of 20–40% of Breast Volume: Techniques of Tissue Transfer
When more than 20% of breast volume is excised, tissue mobilisation alone may not succeed in achieving a satisfactory result and, unless the patient desires a much smaller breast, volume replacement by tissue transfer may be necessary. Most commonly, this entails use of a pedicled latissimus dorsi miniflap (Figures 4(a) and 4(b)), which can be mobilised to fill a defect in any quadrant [62, 63]. The first stage of the procedure involves excision of the breast lesion, and then the latissimus dorsi miniflap is used to fill the defect after a delay of one or two weeks to allow the margin status to be assessed [64]. If intraoperative analysis of surgical margins by frozen section is available, then a single stage procedure is feasible [65, 66]. Alternatives include mobilisation of axillary tissue on a thoracodorsal artery perforator lipodermal flap [7] or use of intercostal artery perforator flaps [66]. One novel approach adopted in our unit is to laparoscopically harvest an omental flap (Figures 5(a) and 5(b)) to fill the local defect [67]. Whereas pedicled flaps usually withstand radiotherapy, albeit with a substantial rate of complications, the use of free flaps in this context is contraindicated.
Figure 4.
(a) This 41-year-old patient had previously undergone wide local excision of a tumour in the left breast. The lateral margin was involved, necessitating a further central wide local excision to include the nipple-areolar complex. (b) In view of the predicted loss of volume, a latissimus dorsi miniflap was utilised to both fill the resultant defect and also replace the skin of the areola. The volume of the partially reconstructed breast is very similar to that of the contralateral side, although postoperative swelling is apparent.
Figure 5.
(a) This patient had previously undergone wide local excision and adjuvant radiotherapy for a cancer located in the lower inner quadrant of the left breast. The resulting defect causes significant distortion to the breast shape and nipple deviation toward the midline. (b) An omental flap was harvested laparoscopically in order to partially reconstruct the breast, achieving a high degree of symmetry with the contralateral breast.
8. Optimising Management of Multifocal and Multicentric Tumours
The management of multifocal tumours, within the same quadrant, and multicentric tumours, in different quadrants or in the same quadrant but widely separated (>5 cm), is controversial. Traditionally these scenarios would dictate mastectomy as the only oncologically sound procedure. If a conservative procedure is to be considered in these patients, careful selection is required with regard to tumour location and breast size and shape and counselled regarding the increased likelihood of further surgery should margins be positive, and possible increased risk of local recurrence, which may entail completion mastectomy. There have been no randomised controlled trials to address the issue of the oncological safety of breast conservation surgery in this context [7]. A retrospective study comparing outcomes of patients with multifocal and unifocal cancers showed equivalent overall survival and no increase in risk of locoregional recurrence [68].
In general, tumours closely spaced within the breast may be removed together utilising an appropriate technique such as an omegaplasty or inverted-T mammoplasty as listed above, whereas separate wide excisions are more appropriate for tumours separated by >5 cm. Careful preoperative planning is of paramount importance. This may often include the use of magnetic resonance imaging, and image-guided localisation of all lesions to be excised is essential. Access to intraoperative frozen section histology, while desirable in terms of reducing the need for further surgery in case of margin involvement, is not an absolute prerequisite.
9. Optimising Management of Local Recurrence or Metachronous Ipsilateral Primary Breast Cancer
The role of further attempts at breast conservation in patients who have previously undergone wide local excision for an ipsilateral cancer is controversial. Whole-breast radiotherapy can only be given once, and therefore further breast conservation surgery alone, versus mastectomy, is subject to the same disparity in efficacy as when wide local excision, without radiotherapy, is compared with mastectomy for primary breast cancer [28]. Thus, perhaps as many as 40% of women treated in this way will have further problems with local recurrence. Given these odds, many women will opt for mastectomy rather than any further attempt at breast conservation, but partial breast radiotherapy may be used in this context in an attempt to reduce the risk of failure [69]. At present, partial breast radiotherapy is only offered to a minority of patients. As these techniques gain wider acceptance and enter routine practice, a greater proportion of patients may be eligible for further breast conservation surgery to manage local recurrence or metachronous ipsilateral primary breast cancer.
10. Optimising Symmetry: When to Perform Contralateral Surgery
Large volume excisions, in patients for whom breast reduction is desirable, often result in noticeable asymmetry, which should be corrected. There is no consensus regarding the optimal timing of contralateral surgery. Simultaneous procedures are attractive in terms of reducing patient inconvenience and the need for a second admission and general anaesthetic (Figures 6(a) and 6(b)). Conversely, postradiotherapy changes can be unpredictable, and, therefore, some prefer to perform the contralateral reduction after these have had time to settle, to improve the chance of achieving good symmetry. A delayed approach also takes into account the possibility that further surgery may be required in the form of excision of margins or completion mastectomy if excision is incomplete [59]. If contralateral reduction is planned as a simultaneous procedure, then slightly more tissue should be excised and the nipple placed marginally higher, to mimic the predicted postradiotherapy shape [55].
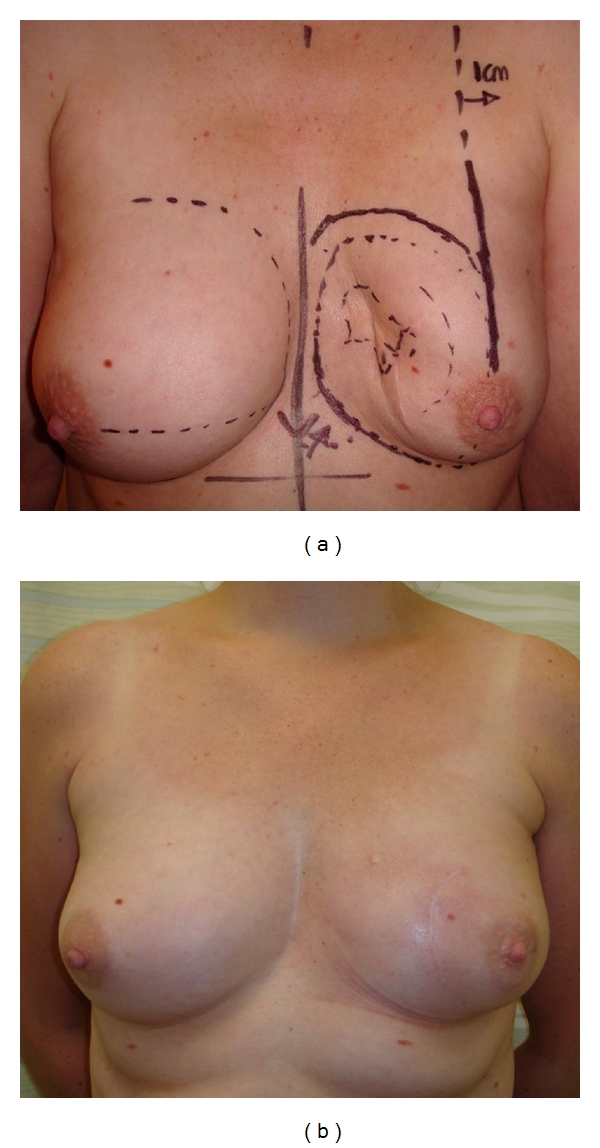
Figure 6.
(a) This 51-year-old patient with large, ptotic breasts and nipple-areola complexes situated medial to the breast meridian presented with a left breast cancer. These images show the skin markings used to plan a therapeutic inverted-T mammoplasty and simultaneous contralateral reduction mammoplasty for symmetrisation. (b) Adjuvant radiotherapy to the left breast has resulted in mild changes in skin pigmentation but symmetry is still good with the contralateral breast being still satisfactory.
11. Novel Technologies and the Future of Optimising Breast Conservation
Endoscopic breast surgery for benign and malignant disease has been described in a number of small case series [70, 71]. Carbon dioxide insufflation creates a working space and both subcutaneous mastectomy and wide local excision have been performed using this technique. Although usually employed in the management of ductal carcinoma in situ, excision of T1 carcinomas has also been successfully performed [72]. The ability to reliably excise tumours with clear surgical margins is not well established due to the small size of these case reports, and more work is needed before they will be readily adopted into routine practice [73].
Radiofrequency ablation for small breast tumours is currently under evaluation [74]. The procedure can be monitored intraoperatively by ultrasound and postoperatively by magnetic resonance imaging. Wide local excision may be performed after radiofrequency ablation to ensure adequate oncological treatment [75]. Concerns regarding the ability to accurately assess response by magnetic resonance imaging alone currently preclude the use of this technique in isolation [76]. Fine-needle aspiration cytology in conjunction with magnetic resonance imaging has been used to assess response in patients not undergoing excision [77], but this approach should not be employed outside of clinical research given its unproven sensitivity and inability to adequately sample the “margin” of ablation and because of the paucity of data related to long-term outcomes.
12. Conclusion
The role of surgery in the management of breast cancer has changed markedly since the days of Halsted, reflecting the change in the way breast cancer is perceived as a systemic, rather than locoregional, disease process. Multimodal therapies, especially in the form of neoadjuvant chemotherapy and endocrine therapy, have increased the proportion of women eligible for breast conservation. The adoption of relatively straightforward surgical techniques to achieve volume displacement can give superior cosmetic outcomes for patients with larger tumours. Techniques of volume replacement are more demanding but are within the remit of surgeons with an interest in oncoplastic surgery or can be performed in conjunction with a plastic surgeon.
The management of multifocal or multicentric cancers and the management of further conservation surgery for recurrence or metachronous ipsilateral primary after previous wide local excision are contentious issues. Ideally, multicentre randomised controlled trials should be designed to address these issues. Surgery to the contralateral breast to improve symmetry should be offered to all patients. The timing of such surgery, and the merits of synchronous versus delayed approaches, should be discussed with patients in full.
In the future, endoscopic breast cancer surgery and radiofrequency ablation therapy are likely to become more popular, but larger studies with longer periods of followup are needed to evaluate their oncological safety prior to their widespread adoption.
Now that patients are benefiting from improved disease-free and overall survival, the cosmetic outcome is of great importance as patients seek to come to terms with the aftermath of breast cancer and its treatment. The importance of cosmesis, in terms of emotional and psychosexual well-being [78–80], demands that the principles of an oncoplastic approach to breast conservation surgery be employed in treating all women with breast cancer.
References
- 1.Fisher B. Laboratory and clinical research in breast cancer—a personal adventure: the David A. Karnofsky memorial lecture. Cancer Research. 1980;40(11):3863–3874. [PubMed] [Google Scholar]
- 2.McCready D, Holloway C, Shelley W, et al. Surgical management of early stage invasive breast cancer: a practice guideline. The Canadian Journal of Surgery. 2005;48(3):185–194. [PMC free article] [PubMed] [Google Scholar]
- 3.Valero VV, Buzdar AU, Hortobagyi GN. Locally advanced breast cancer. Oncologist. 1996;1(1-2):8–17. [Google Scholar]
- 4.Makris A, Powles TJ, Ashley SE, et al. A reduction in the requirements for mastectomy in a randomized trial of neoadjuvant chemoendocrine therapy in primary breast cancer. Annals of Oncology. 1998;9(11):1179–1184. doi: 10.1023/a:1008400706949. [DOI] [PubMed] [Google Scholar]
- 5.Baildam A, Bishop H, Boland G, et al. Oncoplastic breast surgery—a guide to good practice. The European Journal of Surgical Oncology. 2007;33(supplement 1):S1–S23. doi: 10.1016/j.ejso.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 6.Audretsch W, Andree C. Is mastectomy still justified—and if, in which patients? Onkologie. 2006;29(6):243–245. doi: 10.1159/000093477. [DOI] [PubMed] [Google Scholar]
- 7.Patani N, Carpenter R. Oncological and aesthetic considerations of conservational surgery for multifocal/multicentric breast cancer. Breast Journal. 2010;16(3):222–232. doi: 10.1111/j.1524-4741.2010.00917.x. [DOI] [PubMed] [Google Scholar]
- 8.Ravdin PM, Cronin KA, Howlader N, et al. The decrease in breast-cancer incidence in 2003 in the United States. The New England Journal of Medicine. 2007;356(16):1670–1674. doi: 10.1056/NEJMsr070105. [DOI] [PubMed] [Google Scholar]
- 9.Louwman WJ, Voogd AC, van Dijck JA, et al. On the rising trends of incidence and prognosis for breast cancer patients diagnosed 1975–2004: a long-term population-based study in southeastern Netherlands. Cancer Causes and Control. 2008;19(1):97–106. doi: 10.1007/s10552-007-9075-8. [DOI] [PubMed] [Google Scholar]
- 10.Héry C, Ferlay J, Boniol M, Autier P. Quantification of changes in breast cancer incidence and mortality since 1990 in 35 countries with Caucasian-majority populations. Annals of Oncology. 2008;19(6):1187–1194. doi: 10.1093/annonc/mdn025. [DOI] [PubMed] [Google Scholar]
- 11.Tryggvadóttir L, Gislum M, Bray F, et al. Trends in the survival of patients diagnosed with breast cancer in the Nordic countries 1964–2003 followed up to the end of 2006. Acta Oncologica. 2010;49(5):624–631. doi: 10.3109/02841860903575323. [DOI] [PubMed] [Google Scholar]
- 12.Sant M, Allemani C, Santaquilani M, Knijn A, Marchesi F, Capocaccia R. EUROCARE-4. Survival of cancer patients diagnosed in 1995–1999. Results and commentary. The European Journal of Cancer. 2009;45(6):931–991. doi: 10.1016/j.ejca.2008.11.018. [DOI] [PubMed] [Google Scholar]
- 13.Al-Ghazal SK, Fallowfield L, Blamey RW. Comparison of psychological aspects and patient satisfaction following breast conserving surgery, simple mastectomy and breast reconstruction. The European Journal of Cancer. 2000;36(15):1938–1943. doi: 10.1016/s0959-8049(00)00197-0. [DOI] [PubMed] [Google Scholar]
- 14.Baildam AD. Breast reconstruction—state of the art. Breast. 2006;15(supplement 2):S27–S30. doi: 10.1016/S0960-9776(07)70014-0. [DOI] [PubMed] [Google Scholar]
- 15.Clough K, Nos C, Fitoussi A. Oncoplastic surgery for breast cancer. Operative Techniques in Plastic and Reconstructive Surgery. 1999;6(1):50–60. [Google Scholar]
- 16.Audretsch W. Reconstruction of the partial mastectomy defect: classification and method. In: Spear S, editor. Surgery of the Breast: Principles and Art. Philadelphia, Pa, USA: Lippincott Raven; 1998. pp. 155–196. [Google Scholar]
- 17.Bonadonna G, Veronesi U, Brambilla C, et al. Primary chemotherapy to avoid mastectomy in tumors with diameters of three centimeters or more. Journal of the National Cancer Institute. 1990;82(19):1539–1545. doi: 10.1093/jnci/82.19.1539. [DOI] [PubMed] [Google Scholar]
- 18.Keune JD, Jeffe DB, Schootman M, Hoffman A, Gillanders WE, Aft RL. Accuracy of ultrasonography and mammography in predicting pathologic response after neoadjuvant chemotherapy for breast cancer. The American Journal of Surgery. 2010;199(4):477–484. doi: 10.1016/j.amjsurg.2009.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu SV, Melstrom L, Yao K, Russell CA, Sener SF. Neoadjuvant therapy for breast cancer. Journal of Surgical Oncology. 2010;101(4):283–291. doi: 10.1002/jso.21446. [DOI] [PubMed] [Google Scholar]
- 20.Yeh E, Slanetz P, Kopans DB, et al. Prospective comparison of mammography, sonography, and MRI in patients undergoing neoadjuvant chemotherapy for palpable breast cancer. The American Journal of Roentgenology. 2005;184(3):868–877. doi: 10.2214/ajr.184.3.01840868. [DOI] [PubMed] [Google Scholar]
- 21.Smith IE, Dowsett M, Ebbs SR, et al. Neoadjuvant treatment of postmenopausal breast cancer with anastrozole, tamoxifen, or both in combination: the Immediate Preoperative Anastrozole, Tamoxifen, or Combined with Tamoxifen (IMPACT) multicenter double-blind randomized trial. Journal of Clinical Oncology. 2005;23(22):5108–5116. doi: 10.1200/JCO.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 22.Krainick-Strobel UE, Lichtenegger W, Wallwiener D, et al. Neoadjuvant letrozole in postmenopausal estrogen and/or progesterone receptor positive breast cancer: a phase IIb/III trial to investigate optimal duration of preoperative endocrine therapy. BMC Cancer. 2008;8, article 62 doi: 10.1186/1471-2407-8-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barros A, Cardoso MA, Sheng PY, Costa PA, Pelizon C. Radioguided localisation of non-palpable breast lesions and simultaneous sentinel lymph node mapping. The European Journal of Nuclear Medicine and Molecular Imaging. 2002;29(12):1561–1565. doi: 10.1007/s00259-002-0936-9. [DOI] [PubMed] [Google Scholar]
- 24.Moreno M, Wiltgen JE, Bodanese B, Schmitt RL, Gutfilen B, da Fonseca LM. Radioguided breast surgery for occult lesion localization—correlation between two methods. Journal of Experimental and Clinical Cancer Research. 2008;27(1, article 29) doi: 10.1186/1756-9966-27-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dixon JM, Ravi Sekar O, Walsh J, Paterson D, Anderson TJ. Specimen-orientated radiography helps define excision margins of malignant lesions detected by breast screening. The British Journal of Surgery. 1993;80(8):1001–1002. doi: 10.1002/bjs.1800800822. [DOI] [PubMed] [Google Scholar]
- 26.Coombs NJ, Vassallo PP, Parker AJ, Yiangou C. Radiological review of specimen radiographs after breast localisation biopsy is not always necessary. The European Journal of Surgical Oncology. 2006;32(5):516–519. doi: 10.1016/j.ejso.2006.02.019. [DOI] [PubMed] [Google Scholar]
- 27.Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. The New England Journal of Medicine. 2002;347(16):1227–1232. doi: 10.1056/NEJMoa020989. [DOI] [PubMed] [Google Scholar]
- 28.Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. The New England Journal of Medicine. 2002;347(16):1233–1241. doi: 10.1056/NEJMoa022152. [DOI] [PubMed] [Google Scholar]
- 29.Houssami N, Macaskill P, Marinovich ML, et al. Meta-analysis of the impact of surgical margins on local recurrence in women with early-stage invasive breast cancer treated with breast-conserving therapy. The European Journal of Cancer. 2010;46(18):3219–3232. doi: 10.1016/j.ejca.2010.07.043. [DOI] [PubMed] [Google Scholar]
- 30.Groot G, Rees H, Pahwa P, Kanagaratnam S, Kinloch M. Predicting local recurrence following breast-conserving therapy for early stage breast cancer: the significance of a narrow (</ = 2 mm) surgical resection margin. Journal of Surgical Oncology. 2011;103(3):212–216. doi: 10.1002/jso.21826. [DOI] [PubMed] [Google Scholar]
- 31.Smitt MC, Nowels K, Carlson RW, Jeffrey SS. Predictors of reexcision findings and recurrence after breast conservation. International Journal of Radiation Oncology Biology Physics. 2003;57(4):979–985. doi: 10.1016/s0360-3016(03)00740-5. [DOI] [PubMed] [Google Scholar]
- 32.Anscher MS, Jones P, Prosnitz LR, et al. Local failure and margin status in early-stage breast carcinoma treated with conservation surgery and radiation therapy. Annals of Surgery. 1993;218(1):22–28. doi: 10.1097/00000658-199307000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dener C, Inan A, Sen M, Demirci S. Interoperative frozen section for margin assessment in breast conserving energy. Scandinavian Journal of Surgery. 2009;98(1):34–40. doi: 10.1177/145749690909800107. [DOI] [PubMed] [Google Scholar]
- 34.Fukamachi K, Ishida T, Usami S, et al. Total-circumference intraoperative frozen section analysis reduces margin-positive rate in breast-conservation surgery. The Japanese Journal of Clinical Oncology. 2010;40(6):513–520. doi: 10.1093/jjco/hyq006. [DOI] [PubMed] [Google Scholar]
- 35.Bakhshandeh M, Tutuncuoglu SO, Fischer G, Masood S. Use of imprint cytology for assessment of surgical margins in lumpectomy specimens of breast cancer patients. Diagnostic Cytopathology. 2007;35(10):656–659. doi: 10.1002/dc.20704. [DOI] [PubMed] [Google Scholar]
- 36.Veronesi U. How important is the assessment of resection margins in conservative surgery for breast cancer? Cancer. 1994;74(6):1660–1661. doi: 10.1002/1097-0142(19940915)74:6<1660::aid-cncr2820740603>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 37.Hewes JC, Imkampe A, Haji A, Bates T. Importance of routine cavity sampling in breast conservation surgery. The British Journal of Surgery. 2009;96(1):47–53. doi: 10.1002/bjs.6435. [DOI] [PubMed] [Google Scholar]
- 38.Rutqvist LE, Rose C, Cavallin-Ståhl E. A systematic overview of radiation therapy effects in breast cancer. Acta Oncologica. 2003;42(5-6):532–545. doi: 10.1080/02841860310014444. [DOI] [PubMed] [Google Scholar]
- 39.Veronesi U, Saccozzi R, Del Vecchio M, et al. Comparing radical mastectomy with quadrantectomy, axillary dissection, and radiotherapy in patients with small cancers of the breast. The New England Journal of Medicine. 1981;305(1):6–11. doi: 10.1056/NEJM198107023050102. [DOI] [PubMed] [Google Scholar]
- 40.de Csepel J, Tartter PI, Gajdos C. When not to give radiation therapy after breast conservation surgery for breast cancer. Journal of Surgical Oncology. 2000;74(4):273–277. doi: 10.1002/1096-9098(200008)74:4<273::aid-jso6>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 41.Perera F, Engel J, Holliday R, et al. Local resection and brachytherapy confined to the lumpectomy site for early breast cancer: a pilot study. Journal of Surgical Oncology. 1997;65(4):263–268. doi: 10.1002/(sici)1096-9098(199708)65:4<263::aid-jso7>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 42.Baum M, Vaidya JS. Targeted intra-operative radiotherapy-TARGIT for early breast cancer. Annals of the New York Academy of Sciences. 2008;1138:132–135. doi: 10.1196/annals.1414.019. [DOI] [PubMed] [Google Scholar]
- 43.Vaidya JS, Baum M, Tobias JS, et al. Targeted intra-operative radiotherapy (Targit): an innovative method of treatment for early breast cancer. Annals of Oncology. 2001;12(8):1075–1080. doi: 10.1023/a:1011609401132. [DOI] [PubMed] [Google Scholar]
- 44.Patel RR, Das RK. Image-guided breast brachytherapy: an alternative to whole-breast radiotherapy. The Lancet Oncology. 2006;7(5):407–415. doi: 10.1016/S1470-2045(06)70692-1. [DOI] [PubMed] [Google Scholar]
- 45.Lemanski C, Azria D, Gourgon-Bourgade S, et al. Intraoperative radiotherapy in early-stage breast cancer: results of the montpellier phase II trial. International Journal of Radiation Oncology Biology Physics. 2010;76(3):698–703. doi: 10.1016/j.ijrobp.2009.02.039. [DOI] [PubMed] [Google Scholar]
- 46.Clarke M, Collins R, Darby S, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. The Lancet. 2005;366(9503):2087–2106. doi: 10.1016/S0140-6736(05)67887-7. [DOI] [PubMed] [Google Scholar]
- 47.Cochrane RA, Valasiadou P, Wilson AR, Al-Ghazal SK, Macmillan RD. Cosmesis and satisfaction after breast-conserving surgery correlates with the percentage of breast volume excised. The British Journal of Surgery. 2003;90(12):1505–1509. doi: 10.1002/bjs.4344. [DOI] [PubMed] [Google Scholar]
- 48.Boetes C, Veltman J, van Die L, Bult P, Wobbes T, Barentsz JO. The role of MRI in invasive lobular carcinoma. Breast Cancer Research and Treatment. 2004;86(1):31–37. doi: 10.1023/B:BREA.0000032921.10481.dc. [DOI] [PubMed] [Google Scholar]
- 49.Turnbull LW, Brown SR, Olivier C, et al. Multicentre randomised controlled trial examining the cost-effectiveness of contrast-enhanced high field magnetic resonance imaging in women with primary breast cancer scheduled for wide local excision (COMICE) Health Technology Assessment. 2010;14(1):1–152. doi: 10.3310/hta14010. [DOI] [PubMed] [Google Scholar]
- 50.Missana MC, Laurent I, Barreau L, Balleyguier C. Autologous fat transfer in reconstructive breast surgery: indications, technique and results. The European Journal of Surgical Oncology. 2007;33(6):685–690. doi: 10.1016/j.ejso.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 51.Chan CW, McCulley SJ, Macmillan RD. Autologous fat transfer—a review of the literature with a focus on breast cancer surgery. Journal of Plastic, Reconstructive and Aesthetic Surgery. 2008;61(12):1438–1448. doi: 10.1016/j.bjps.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 52.de Lorenzi F. Oncoplastic surgery: the evolution of breast cancer treatment. Breast Journal. 2010;16(supplement 1):S20–S21. doi: 10.1111/j.1524-4741.2010.00997.x. [DOI] [PubMed] [Google Scholar]
- 53.Shestak KC, Johnson RR, Greco RJ, Williams SL. Partial mastectomy and breast reduction as a valuable treatment option for patients with macromastia and carcinoma of the breast. Surgery Gynecology and Obstetrics. 1993;177(1):54–56. [PubMed] [Google Scholar]
- 54.Tausch C, Hintringer T, Kugler F, Schmidhammer C, Bauer M, Aufschnaiter M. Breast-conserving surgery with resection of the nipple-areola complex for subareolar breast carcinoma. The British Journal of Surgery. 2005;92(11):1368–1371. doi: 10.1002/bjs.5083. [DOI] [PubMed] [Google Scholar]
- 55.Wagner E, Schrenk P, Huemer GM, Sir A, Schreiner M, Wayand W. Central quadrantectomy with resection of the nipple-areola complex compared with mastectomy in patients with retroareolar breast cancer. Breast Journal. 2007;13(6):557–563. doi: 10.1111/j.1524-4741.2007.00492.x. [DOI] [PubMed] [Google Scholar]
- 56.Galimberti V, Zurrida S, Zanini V, et al. Central small size breast cancer: how to overcome the problem of nipple and areola involvement. The European Journal of Cancer Part A. 1993;29(8):1093–1096. doi: 10.1016/s0959-8049(05)80294-1. [DOI] [PubMed] [Google Scholar]
- 57.Benelli L. A new periareolar mammaplasty: the “round block” technique. Aesthetic Plastic Surgery. 1990;14(2):93–100. doi: 10.1007/BF01578332. [DOI] [PubMed] [Google Scholar]
- 58.Masetti R, Di Leone A, Franceschini G, et al. Oncoplastic techniques in the conservative surgical treatment of breast cancer: an overview. Breast Journal. 2006;12(5, supplement 2):S174–S180. doi: 10.1111/j.1075-122X.2006.00331.x. [DOI] [PubMed] [Google Scholar]
- 59.Anderson BO, Masetti R, Silverstein MJ. Oncoplastic approaches to partial mastectomy: an overview of volume-displacement techniques. The Lancet Oncology. 2005;6(3):145–157. doi: 10.1016/S1470-2045(05)01765-1. [DOI] [PubMed] [Google Scholar]
- 60.Lassus C. Reduction mammaplasty with short inframammary scars. Plastic and Reconstructive Surgery. 1986;77(4):680–681. doi: 10.1097/00006534-198604000-00039. [DOI] [PubMed] [Google Scholar]
- 61.Lassus C. Breast reduction: evolution of a technique—a single vertical scar. Aesthetic Plastic Surgery. 1987;11(2):107–112. doi: 10.1007/BF01575495. [DOI] [PubMed] [Google Scholar]
- 62.Rainsbury RM. Breast-sparing reconstruction with latissimus dorsi miniflaps. The European Journal of Surgical Oncology. 2002;28(8):891–895. doi: 10.1053/ejso.2002.1350. [DOI] [PubMed] [Google Scholar]
- 63.Yelland A, Rainsbury D. The use of the latissimus dorsi musculocutaneous flap for immediate correction of the deformity resulting from breast conservation surgery. The British Journal of Plastic Surgery. 1999;52(5):420–421. [PubMed] [Google Scholar]
- 64.Dixon JM, Venizelos B, Chan P. Latissimus dorsi mini-flap: a technique for extending breast conservation. Breast. 2002;11(1):58–65. doi: 10.1054/brst.2001.0312. [DOI] [PubMed] [Google Scholar]
- 65.Rusby JE, Paramanathan N, Laws SA, Rainsbury RM. Immediate latissimus dorsi miniflap volume replacement for partial mastectomy: use of intra-operative frozen sections to confirm negative margins. The American Journal of Surgery. 2008;196(4):512–518. doi: 10.1016/j.amjsurg.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 66.Munhoz AM, Montag E, Arruda E, et al. Immediate conservative breast surgery reconstruction with perforator flaps: new challenges in the era of partial mastectomy reconstruction? Breast. 2011;20(3):233–240. doi: 10.1016/j.breast.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 67.Zaha H, Inamine S. Laparoscopically harvested omental flap: results for 96 patients. Surgical Endoscopy. 2010;24(1):103–107. doi: 10.1007/s00464-009-0533-0. [DOI] [PubMed] [Google Scholar]
- 68.Oh JL, Dryden MJ, Woodward WA, et al. Locoregional control of clinically diagnosed multifocal or multicentric breast cancer after neoadjuvant chemotherapy and locoregional therapy. Journal of Clinical Oncology. 2006;24(31):4971–4975. doi: 10.1200/JCO.2006.07.6067. [DOI] [PubMed] [Google Scholar]
- 69.Resch A, Fellner C, Mock U, et al. Locally recurrent breast cancer: pulse dose rate brachytherapy for repeat irradiation following lumpectomy—a second chance to preserve the breast. Radiology. 2002;225(3):713–718. doi: 10.1148/radiol.2253011913. [DOI] [PubMed] [Google Scholar]
- 70.Liu H, Huang CK, Yu PC, et al. Retromammary approach for endoscopic resection of benign breast lesions. World Journal of Surgery. 2009;33(12):2572–2578. doi: 10.1007/s00268-009-0225-x. [DOI] [PubMed] [Google Scholar]
- 71.Lee EK, Kook SH, Park YL, Bae WG. Endoscopy-assisted breast-conserving surgery for early breast cancer. World Journal of Surgery. 2006;30(6):957–964. doi: 10.1007/s00268-005-0202-y. [DOI] [PubMed] [Google Scholar]
- 72.Yamashita K, Shimizu K. Transaxillary retromammary route approach of video-assisted breast surgery enables the inner-side breast cancer to be resected for breast conserving surgery. The American Journal of Surgery. 2008;196(4):578–581. doi: 10.1016/j.amjsurg.2008.06.028. [DOI] [PubMed] [Google Scholar]
- 73.Morrow M. Minimally invasive surgery for breast cancer. The British Medical Journal. 2009;338:p. b557. doi: 10.1136/bmj.b557. [DOI] [PubMed] [Google Scholar]
- 74.Singletary SE. Radiofrequency ablation of breast cancer. The American Surgeon. 2003;69(1):37–40. [PubMed] [Google Scholar]
- 75.Manenti G, Bolacchi F, Perretta T, et al. Small breast cancers: in vivo percutaneous US-guided radiofrequency ablation with dedicated cool-tip radiofrequency system. Radiology. 2009;251(2):339–346. doi: 10.1148/radiol.2512080905. [DOI] [PubMed] [Google Scholar]
- 76.Nakamura S, Ishiyama M, Tsunoda-Shimizu H. Magnetic resonance mammography has limited ability to estimate pathological complete remission after primary chemotherapy or radiofrequency ablation therapy. Breast Cancer. 2007;14(2):123–130. doi: 10.2325/jbcs.951. [DOI] [PubMed] [Google Scholar]
- 77.Oura S, Tamaki T, Hirai I, et al. Radiofrequency ablation therapy in patients with breast cancers two centimeters or less in size. Breast Cancer. 2007;14(1):48–54. doi: 10.2325/jbcs.14.48. [DOI] [PubMed] [Google Scholar]
- 78.Sanger CK, Reznikoff M. A comparison of the psychological effects of breast-saving procedures with the modified radical mastectomy. Cancer. 1981;48(10):2341–2346. doi: 10.1002/1097-0142(19811115)48:10<2341::aid-cncr2820481034>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 79.Bartelink H, van Dam F, van Dongen J. Psychological effects of breast conserving therapy in comparison with radical mastectomy. International Journal of Radiation Oncology Biology Physics. 1985;11(2):381–385. doi: 10.1016/0360-3016(85)90161-0. [DOI] [PubMed] [Google Scholar]
- 80.Nicholson RM, Leinster S, Sassoon EM. A comparison of the cosmetic and psychological outcome of breast reconstruction, breast conserving surgery and mastectomy without reconstruction. Breast. 2007;16(4):396–410. doi: 10.1016/j.breast.2007.01.009. [DOI] [PubMed] [Google Scholar]


