Empirical evidence continues to accumulate indicating that early life nutrition disparities are likely to explain, at least in part, higher risks for maternal disease (e.g., gestational diabetes) and childhood obesity among ethnic/racial minority groups. Minority women are more likely to be overweight or obese when they become pregnant. This condition may trigger a series of events including excessive weight gain during pregnancy compared with the Institute of Medicine recommendations (1), altered glucose and lipid metabolism, suboptimal infant feeding outcomes, and postpartum weight retention that, when combined, may explain, at least in part, a higher obesity risk among their offspring. This supplement from Advances in Nutrition follows a life cycle approach to first understanding disparities, if any, in prepregnancy BMI, weight gain during pregnancy, gestational diabetes, and infancy/early childhood risk factors for childhood obesity including suboptimal infant feeding practices. Second, each article attempts to provide possible solutions for addressing documented disparities.
The collection of 5 review articles that follows this introduction represents an important advance in synthesizing the knowledge in an area that is critical to better understanding how to improve public health in the United States and beyond. Three of these articles focus on maternal outcome disparities before, during, and after pregnancy (2–4), and 2 focus primarily on the infancy/early childhood period (5, 6). Whenever possible, the authors of the articles included in this special issue examine the effectiveness of local community programs and federal food assistance programs in reversing health disparities in maternal and infant health.
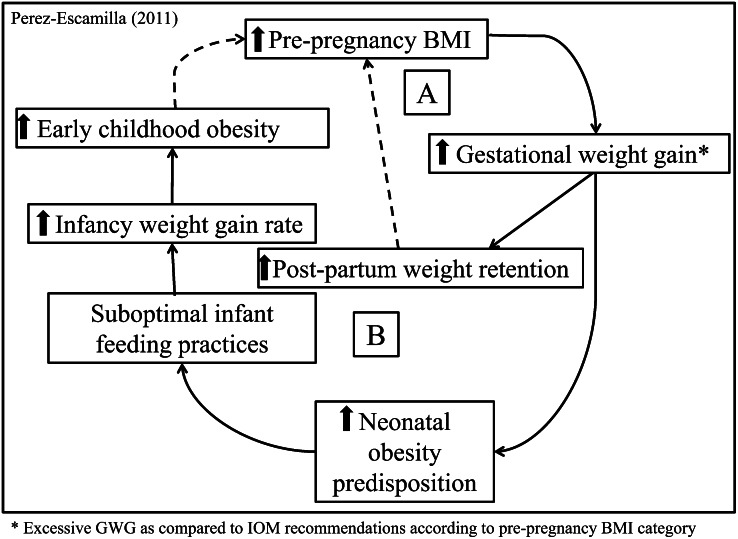
As reported by Siega-Riz (2) in this supplement, minority women are not only more likely to be overweight/obese when becoming pregnant for the first time, but they are also more likely to become pregnant at younger ages and have more children than their white counterparts. Thus, they are also more likely to go through the mother-child obesity cycle (Fig. 1) more times during their reproductive life than white women. Therefore, their increased risk of excessive body fat accumulation, in relation to that of their white counterparts, may also be the result of more “exposures” to the obesity cycle and not only to the weight differentials when becoming pregnant for the first time. Headen et al. (3) confirm in their review that minority women are more likely to experience inadequate weight gain during pregnancy and that there are no disparities with regard to excessive gestational weight in relation to their white counterparts. The authors found that black women were more likely to retain excessive weight postpartum compared with Hispanic and white women. Headen et al. also document that interventions seeking to improve gestational weight gain and postpartum weight retention outcomes have thus far yielded mixed results. A major finding from their review is the lack of studies that explicitly address reasons for racial/ethnic differences in pregnancy-related weight. Studies in this area are urgently needed to develop effective pregnancy-related weight-control interventions among minority women. Chasan-Taber (4) reviewed the literature to determine whether physical activity, diet, and excessive weight gain during pregnancy are associated with impaired glucose tolerance/gestational diabetes among pregnant Latinas. This review provides support for an inverse association between exercise during pregnancy and risk of gestational diabetes among Latinas. Based on limited evidence, it also found support for an association between certain nutrient intakes (fewer saturated fatty acids and energy-dense foods, higher intakes of fiber, and a higher polyunsaturated:saturated fatty acid ratio) and lower risk of abnormal glucose tolerance, independent of gestational weight gain. This review also provides support for an association between excessive gestational weight gain (especially among overweight/obese women) and gestational diabetes mellitus as well as milder abnormal glucose tolerance. These 3 symposium papers, all focusing on maternal nutrition disparities, collectively suggest that there is a need to better understand the following: a) biological, behavioral, and social mechanisms likely to explain ethnic/racial-specific outcomes associated with maternal prepregnancy obesity; inadequate or excessive weight gain during pregnancy; and postpartum weight retention and b) how to improve mother/offspring outcomes through effective, culturally appropriate interventions that target different stages of the life cycle (preconception, pregnancy, postpartum), taking into account the social determinants of health. Headen et al. also remind us that it is important to not only focus our attention on excessive weight gain during pregnancy but also on inadequate weight gain that often leads to small-for-gestational age infants who are also more likely to become obese and in whom chronic diseases develop later on in life, perhaps via epigenetic mechanisms.
Figure 1.
The childhood obesity epidemic: a life cycle framework for understanding ethnic/racial disparities. Women who become pregnant when they are overweight/obese are more likely to gain excessive weight during pregnancy [compared with the Institute of Medicine gestational weight gain recommendations according to prepregnancy BMI category (1)] and to retain more weight postpartum. Minority women tend to have more children; thus, they are exposed more times to cycle A. Women who are overweight/obese and/or gain excessive weight during pregnancy are more likely to deliver newborns predisposed to becoming obese early on in life, especially if optimal infant feeding practices are not followed (cycle B). This may set the child on a track that can lead a girl to remaining overweight/obese by the time she gets pregnant for the first time, starting her exposure to cycle A and the transfer of the obesity risk to the next generation (cycle B) (7).
Moving on to the infancy/early childhood period, the review by Dixon et al. (5) documents that ethnic/racial minority children are already more likely to be obese by 2 years of age compared with their white counterparts. In addition, they document that both nutrition-related (e.g., excessive weight gain during infancy, lower likelihood to breastfeed exclusively, premature introduction of complementary foods, maternal restrictive feeding style, sugar-sweetened beverages, and fast food) and non-nutritional (e.g., maternal prenatal depression, failure to meet sleep recommendations, TV in bedroom after 2 y of age) early life risk factors for childhood obesity are more prevalent among minority children. Chapman and Pérez-Escamilla (6) confirm that ethnic/racial minority infants are less likely to be exclusively breast-fed and that breastfeeding initiation is less likely to occur among black infants compared with white and Hispanic newborns. Furthermore, their systematic review confirms the availability of efficacious health facility- and community-based interventions to improve breastfeeding outcomes among minority infants.
Integrating the findings presented in the 5 symposium articles leads us to recommend a more comprehensive and better coordinated approach to mother/child health and nutrition services than what are currently available in the United States. An approach that can simultaneously decrease childhood obesity risk and improve maternal health outcomes needs to be conceptualized based on a life cycle approach (Fig. 1). Given how difficult it has been to identify effective ways to optimize gestational weight gain once mothers are overweight/obese, it is crucial to pay particular attention to preventing excessive preconception weight and to encourage women to avoid retaining excessive postpartum weight. In addition, it is key for women to receive adequate support for breastfeeding their infants and to introduce them to safe, nutritious complementary foods at the right age. It is also important for families to receive the needed information about how to prevent novel risk factors for childhood obesity including maternal depression and lack of sufficient sleep. This approach will require a much better integration of family and mother/child mental, medical, and child development services that often are not coordinated with each other.
Acknowledgments
Both authors read and approved the final manuscript.
Footnotes
Supported in part by NIH-NCMHD grant P20 MD001765-05 to R.P.-E. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center on Minority Health and Health Disparities or the National Institutes of Health.
Author disclosures: R. Pérez-Escamilla and O. Bermúdez, no conflicts of interest.
Literature Cited
- 1.Institute of Medicine (IOM) Weight gain during pregnancy: reexamining the guidelines. Washington, DC: National Academies Press, 2009 [PubMed] [Google Scholar]
- 2.Siega-Riz AM. Prepregnancy obesity: determinants, consequences, and solutions. Adv Nutr. 2012; 105–107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Headen IE, Davis EM, Mujahid MS, Abrams B. Racial-ethnic differences in pregnancy related weight. Adv Nutr. 2012; 83–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chasan-Taber L. Physical activity and dietary behaviors associated with weight gain and impaired glucose tolerance among pregnant Latinas. Adv Nutr. 2012; 108–118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dixon B, Peña MM, Taveras EM. Lifecourse approach to racial/ethnic disparities in childhood obesity. Adv Nutr. 2012; 73–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chapman D, Pérez-Escamilla R. Breastfeeding among minority women: moving from risk factors to interventions. Adv Nutr. 2012; 95–104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pérez-Escamilla R. The 2010 Dietary Guidelines: Lessons learned for 2015; Focus: Childhood obesity. 6th Biennial Childhood Obesity Conference, San Diego, June 29, 2011 [Google Scholar]