Abstract
The gap between current breastfeeding practices and the Healthy People 2020 breastfeeding goals is widest for black women compared with all other ethnic groups. Also of concern, Hispanic and black women have the highest rates of formula supplementation of breast-fed infants before 2 d of life. These disparities must be addressed through the scale-up of effective interventions. The objective of this critical review is to identify and evaluate U.S.-based randomized trials evaluating breastfeeding interventions targeting minorities and highlight promising public health approaches for minimizing breastfeeding disparities. Through PubMed searches, we identified 22 relevant publications evaluating 18 interventions targeting minorities (peer counseling [n = 4], professional support [n = 4], a breastfeeding team [peer + professional support, n = 3], breastfeeding-specific clinic appointments [n = 2], group prenatal education [n = 3], and enhanced breastfeeding programs [n = 2]). Peer counseling interventions (alone or in combination with a health professional), breastfeeding-specific clinic appointments, group prenatal education, and hospital/Special Supplemental Nutrition Program for Women, Infants, and Children enhancements were all found to greatly improve breastfeeding initiation, duration, or exclusivity. Postpartum professional support delivered by nurses was found to be the least effective intervention type. Beyond improving breastfeeding outcomes, 6 interventions resulted in reductions in infant morbidity or health care use. Future research should include further evaluations of successful interventions, with an emphasis on determining the optimal timeframe for the provision of support, the effect of educating women’s family members, and the impact on infant health care use and cost-effectiveness.
Introduction
Breast milk is recognized as the optimal source of nutrition for infants because of its unique nutritional and immunological characteristics. The American Academy of Pediatrics recommends exclusive breastfeeding for the first 6 mo of an infant’s life, followed by the introduction of appropriate complementary foods along with continued breastfeeding until at least 12 mo of age (1). Despite the well-documented benefits of breastfeeding for the infant and the mother, breastfeeding outcomes lag behind public health goals.
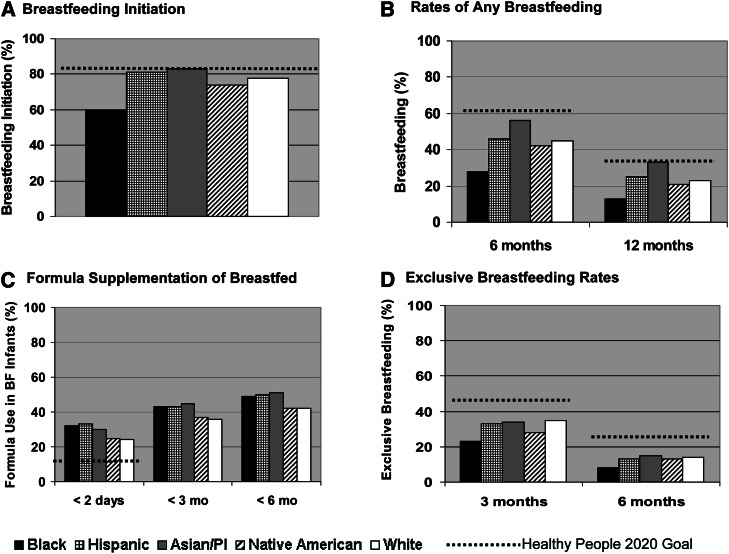
Disparities in the breastfeeding practices of U.S. women are quite evident when comparing the 2007 National Immunization Survey data by ethnic group (2). Breastfeeding initiation rates are markedly lower among black women (60%) compared with other ethnic groups (Fig. 1A). Hispanic and Asian women are currently meeting the Healthy People 2020 (HP2020)4 breastfeeding initiation goal of 81.9%, whereas Native American and white women are close to attaining the goal. The widest variations in breastfeeding outcomes by ethnicity are reflected in the rates of any breastfeeding at 6 mo post partum (PP) (Fig. 1B), in which no ethnic groups are meeting the HP2020 goals. At both 6 and 12 mo PP, Asian women have the highest rates of any breastfeeding, whereas black women have the lowest. The rates of any breastfeeding at 6 and 12 mo among Hispanic, Native American, and white women are quite similar, but still require substantial improvement to meet the HP2020 goals of 61% at 6 mo, and 34% at 12 mo. Exclusive breastfeeding (i.e., provision of only breast milk and vitamin/mineral drops to infants [3]) rates are suboptimal for all ethnic groups. On average, 24% of the breast-fed infants in the United States receive formula supplementation by 2 d of life (4), with this practice being most common among Hispanic (33%) and black (32%) infants (Fig. 1C). At this point, no ethnic group is meeting the HP2020 goal to reduce supplementation of 2-d-old breast-fed infants to 14%. Exclusive breastfeeding rates at 3 and 6 mo PP follow a similar pattern, with the lowest rates observed among black women (Fig. 1D).
Figure 1.
Breastfeeding and supplementation rates by ethnicity/race: National Immunization Survey data (2,4). A. Breastfeeding Initiation: Black women have the lowest rates; B. Rates of Any Breastfeeding: Black women have the lowest rates of any breastfeeding at 6 and 12 months; C. Formula Supplementation: Excessive formula supplementation of breastfed infants in all ethnic groups; D. Exclusive Breastfeeding Rates: Lowest rates among black women, but no ethnic group meets Healthy People 2020 goals.
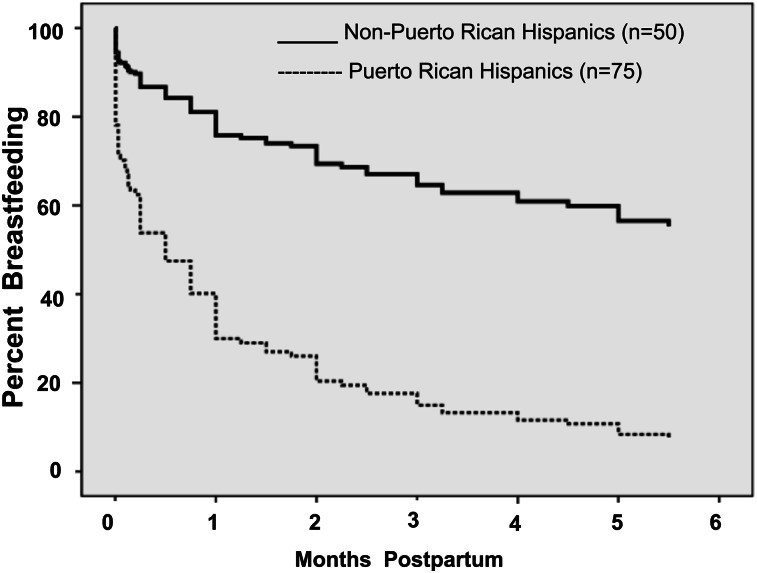
Figure 2.
Comparison of the rates of any breastfeeding by Hispanic subgroups in Hartford, Connecticut . Secondary analysis of randomized control trial data (6).
U.S. national data do not typically report the breastfeeding practices of ethnic subgroups and can thus mask wide variation among subgroups (5). For example, national breastfeeding data for Hispanics reflect breastfeeding practices of Mexicans, Puerto Ricans, and immigrants from several other Spanish-speaking countries. The variability in the breastfeeding practices of ethnic subgroups is clearly demonstrated with data obtained from our previously published breastfeeding peer counseling (PC) randomized trial conducted in Hartford, Connecticut (6). Significantly different patterns of breastfeeding continuation are evident for the Puerto Ricans (median breastfeeding duration, <0.5 mo) versus other Hispanic women derived primarily from Mexico, Peru, and Colombia (median breastfeeding duration, >6.0 mo) in this sample of low-income women ( (P < 0.05). Thus, targeted breastfeeding interventions are needed for ethnic subgroups whose breastfeeding outcomes fall below the national rates for their ethnic/racial group.
The reasons for disparities in breastfeeding practices are complex. Research in this area has moved beyond simply identifying demographic and socioeconomic risk factors for poor breastfeeding outcomes and has identified novel, potentially modifiable risk factors. Some of the potential causes of poor breastfeeding outcomes among black and Puerto Rican women include breastfeeding ambivalence (7), the availability of free formula from the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) (8), a high level of comfort with the idea of formula feeding (9), limited availability and lower intensity of WIC breastfeeding support for minority women (10, 11), and issues surrounding trust building and perceived mistreatment by providers (12). Further research is needed to better understand the root causes of breastfeeding disparities and how these can be addressed through public health interventions.
The consequences of poor breastfeeding practices are substantial. Breastfeeding is associated with a lower risk of the development of several health conditions in the child, including acute otitis media, childhood leukemia, obesity, type 2 diabetes, sudden infant death syndrome, gastroenteritis, and asthma (13). Exclusive breastfeeding is associated with decreased risk of atopic dermatitis, necrotizing enterocolitis, severe lower respiratory tract infections, otitis media, gastroenteritis, and sudden infant death syndrome (13–15). With the exception of otitis media and childhood leukemia, each of these conditions has a documented black/white health disparity, with higher rates observed among black (vs. white) children (16–23). The potential consequences of lower breastfeeding rates among black women is especially concerning because their children experience health disparities for most of the conditions for which breastfeeding is known to be protective. This overlap between conditions for which breastfeeding is protective and conditions for which black/white disparities exist does not necessarily reflect causality. However, it does highlight the need for well-designed research evaluating the relationship between breastfeeding status and common health disparities, which carefully assess breastfeeding duration and exclusivity.
To minimize breastfeeding disparities in the United States, culturally sensitive interventions targeting groups with the worst breastfeeding outcomes need to be developed and evaluated, with widespread dissemination of those that are effective. Currently, there is a growing body of literature describing breastfeeding interventions among minority groups, some of which have been featured in The CDC Guide to Breastfeeding Interventions (24). The objectives of this critical review are to identify and evaluate U.S.-based randomized trials evaluating breastfeeding interventions targeting minorities and highlight promising public health approaches designed to minimize breastfeeding disparities.
Current status of knowledge
To evaluate the current status of knowledge regarding the effectiveness of breastfeeding interventions targeting minorities, we conducted PubMed searches in February 2011 using “breastfeeding” and “randomized trial” along with each of the following descriptors: Latina, Latino, Hispanic, black, African American, Asian, Native American, First Nation, Indian, minority, and low income. Reference lists of relevant articles and lactation conference proceedings were hand searched to identify pertinent research. To be included in this critical review, studies had to be U.S.-based randomized trials evaluating a breastfeeding promotion intervention, reporting breastfeeding outcome data, enrolling primarily minority participants, and conducting analyses by intention to treat. After identifying relevant abstracts, the full text article of each was reviewed to identify those meeting the inclusion criteria.
Based on the main focus of the intervention, included studies were grouped into 1 of the following 6 categories: PC, professional support, breastfeeding team (PC combined with professional support), breastfeeding-specific clinic appointments, group prenatal counseling, and enhanced breastfeeding programs (program add-ons). Unless otherwise noted, breastfeeding outcomes were consistent with the following definitions. Breastfeeding initiation reflects that the infant was ever breast-fed or received breast milk. Post partum breastfeeding rates indicate that the child received breast milk at the specified time point. Exclusive breastfeeding indicates that the infant received only breast milk, allowing for medications and vitamin/mineral drops, consistent with the WHO definition of exclusive breastfeeding (3).
This search yielded 117 abstracts, of which 22 full text relevant articles were reviewed, yielding 20 publications that described 18 interventions. The target populations of these interventions were black women (10/18), Latinas (6/18), and black and Latina groups (2/18). We did not identify a single randomized trial targeting Asians or Native Americans. The identified interventions included PC (n = 4), professional support (n = 4), a breastfeeding team (peer + professional support, n = 3), breastfeeding-specific clinic appointments (n = 2), group prenatal education (n = 3), and enhanced breastfeeding programs (n = 2). The details of each randomized trial are summarized in Table 1.
Table 1.
Summary of published randomized trials evaluating breastfeeding interventions targeting minority women1
| Study | Study Population | Intervention | Outcomes (I vs. C) |
| Peer counseling | |||
| Chapman et al. (6) | N = 219; 80% Hispanic (mostly Puerto Rican), 9% black | Home visits: 1 prenatal, 3 PP Hospital visits: daily Telephone support and breast pumps available |
Initiation: 91 vs. 77%* BF 1 mo: 64 vs. 51% BF 3 mo: 44 vs. 29% EBF: NS at any time point |
| Anderson et al. (25) | N = 182; 72% Hispanic (mostly Puerto Rican), 18% black | Focus: EBF promotion/support Home visits: 3 prenatal, 9 PP Hospital visits: daily Telephone support and breast pumps |
Initiation: 91 vs. 76%* BF 3 mo: 49 vs. 36% EBF 3 mo: 27 vs. 3%* Infant diarrhea, 3 mo: 18 vs. 38%* Maternal amenorrhea, 3 mo: 52 vs. 33%* |
| Chapman et al. (26) | N = 206; overweight/obese, low-income women, 82% Hispanic (mostly Puerto Rican), 10% black | Focus: specialized PC for obese women, EBF promotion Home visits: 3 prenatal, 11 PP Hospital visits: daily EBF promotion, telephone support, breast pumps and BF sling available |
Initiation: 97 vs. 99% >50% BM feedings, 2 wk PP: 81 vs. 67%* BF 3 mo: 47 vs. 51% EBF 1 mo: 18 vs. 12% Infant rehospitalization 3 mo: 8 vs. 22%* |
| Merewood et al. (27) | N = 101; BF mothers of healthy, preterm, NICU infants (26–37 wk gestational age); 69% black, 19% Hispanic | Focus: BF support for preterm infants Hospital visits: within 72 h of birth and weekly through 6 wk PP (if still hospitalized) Telephone support: weekly after hospital discharge through 6 wk PP |
Feeding at 12 wk: any BF (OR: 2.81, 95% CI: 1.11–7.14; P = 0.03)EBF: NS |
| Professional support | |||
| Bunik et al. (28) | N = 341; 88% Hispanic (mostly Mexican), 6% black | RN support Daily telephone call from bilingual RN (day of discharge through 14 d PP) |
BF 3 mo: 49 vs. 54% BF 6 mo: 28 vs. 37% Sick infant visit, 1 mo: 25 vs. 36%# |
| Grossman et al.(29) | N = 97; 54% black | RN support Hospital visits: 4 RN visits (30–45 min) Telephone support: 4 RN PP calls | BF 3 mo: 35 vs. 48% BF 6 mo: 14 vs. 27% |
| Bonuck et al. (30,31) | N = 304; 57% Hispanic, 36% black | LC support Home visits: 2 prenatal, 1 PP Telephone support as needed Nursing bra provided. Breast pumps provided as needed. | BF through 20 wk: 53 vs. 39%* >50% BM, 1 wk: 69 vs. 37%*** >50% BM, through 9 wk: 46 vs. 33%* EBF: NS at any time point |
| Petrova et al. (32) | N = 104; 88% Hispanic (mostly Mexican), 6% black | LC support Home visits: 2 prenatal Hospital visit/call: 1 Telephone support: 2 calls | BF 3 mo: 78 vs. 63% EBF 1 wk: 46 vs. 29% EBF 1 mo: 30 vs. 24% EBF 3 mo: 14 vs. 11% |
| Breastfeeding team (peer counselor + professional) | |||
| Pugh et al. (33) | N = 41; 93% black | RN + PC team Hospital visits: daily Home visits: 3 (in first month PP) PC telephone support through 6 mo PP | BF 6 mo: 45 vs. 35% EBF 3 mo: 45 vs. 25% EBF 6 mo: 40 vs. 15% |
| Pugh et al. (34) | N = 328; 87% black | RN + PC team Hospital visits: daily Home visits: 3 (in first month PP) PC telephone support through 6 mo Unlimited RN contact via pager | BF 6 wk (OR: 1.72, 95% CI: 1.1–2.8; P = 0.03) BF 12 wk (OR: 1.58, 95% CI: 1.0–2.49; P = 0.05) |
| Wambach et al. (35) | N = 289; teen mothers, 61% black | LC + PC team Prenatal group classes: 2 PC hospital visits: 1 Telephone support by LC or peer counselor: 5 calls through 4 wk PP Breast pump as needed Study groups: 1. Intervention2. Attention control3. Usual care | Unadjusted analyses (1 vs. 2 vs. 3) Initiation: 79 vs. 66 vs. 63%* Median BF duration: 177 vs. 42 vs. 61 d*** EBF 3 wk: 31 vs. 30 vs. 18% |
| Breastfeeding-specific clinic appointment | |||
| Serwint et al. (36) | N = 159; nulliparous, pregnant women, 91% black | Pediatric clinic: prenatal appointment to discuss BF Providers: pediatric residents who had received 3 h of additional BF training |
Response rate: 68% attended appointment Initiation: 42 vs. 31% BF 1 mo: 19 vs. 14% Planned FF, but BF: 45 vs. 14%* |
| Hopkinson et al. (37) | N = 522; 100% Hispanic mixed feeders (mostly Mexican) | Breastfeeding clinic: at hospital discharge, appointment card provided to attend BF clinic at 3–7 d PP Providers: PC with IBCLC supervision |
Response rate: Clinic visit by 1 wk PP: 35% Clinic visit by 3 wk PP: 56% Clinic visit/telephone call, 3 wk PP: 80% BF outcomes at 4 wk PP: EBF: 17 vs. 10%* Water given: 20 vs. 41%** Tea given: 16 vs. 28%** Ounces formula/d: 12 vs. 14* |
| Group prenatal counseling | |||
| Kistin et al. (38) | N = 159; 100% black | Prenatal BF education: 1. Group class (50–80 min) 2. Individual session (15–30 min) 3. Controls (no additional BF education) Providers: midwives | BF Initiation: Group class (OR: 5.2, 95% CI: 2.9–9.3; P = 0.006) Any intervention (OR: 4.3, 95% CI: 2.6–7.0; P = 0.004) Individual session: NS Controls: reference group Planned FF, but BF (1 vs. 2 vs. 3): 21 vs. 38 vs. 8%*** BF 12 wk (1 vs. 2 vs. 3) 15 vs. 4 vs. 4%* |
| Ickovics et al. (39) | N = 1047; 78% black, 13% Hispanic | Group prenatal care model:I: Group prenatal care (20-h contact time) C: Individual (2-h contact time)Providers: usual clinic staff | BF initiation: 67 vs. 55% (OR: 1.73, (95% CI: 1.28–2.35; P = 0.001) |
| Wolfberg et al. (40) | N = 59; 86% black | BF class for fathers I: Dads prenatal BF class (2 h) C: Dads prenatal infant care class (2 h) Same black male instructor for both classes | BF initiation: 74 vs. 41%* BF 1 mo: 38 vs. 35% BF 2 mo: 35 vs. 19% |
| Enhanced Breastfeeding Programs | |||
| Frank et al. (41) | N = 343; 65% black, 19% Hispanic | 1: Research-funded discharge bag (contains BF promotional materials) 2: Research counseling: perinatal visit + 8 telephone calls 3: Research bags + research counseling 4. Controls: standard bag (sterile water, nipples, formula company pamphlets) + standard limited counseling |
EBF duration: (1 + 3) vs. 4: 60 vs. 42 d** (1-tailed log rank test) Infant rehospitalization, 4 mo 2 vs. 3: 14 vs. 1%* |
| Caulfield et al. (42), Gross et al. (43) | N = 242; 100% black | WIC clinic-based intervention: 1: Peer counselor contact: 3 prenatal visits + weekly contact through 16 wk 2: BF promotion video/pamphlets 3: PC + video/pamphlets 4: Controls | BF initiation: 1 vs. 2 vs. 3 vs. 4: 62 vs. 50 vs. 52 vs. 26%* 1 vs. 4 (OR: 3.8, 95% CI: 1.4–10.2; P < 0.05)* BF termination 4 mo: 1: OR: 0.2, 95% CI: 0.1–0.4* 2: OR: 0.3, 95% CI: 0.1–0.8* 3: OR: 0.3, 95% CI: 0.1–0.6* 4: Reference |
*P < 0.05; **P < 0.01; ***P < 0.001; #P = 0.05. BF, breastfeeding; BM, breast milk; C, control; EBF, exclusive breastfeeding; FF, formula feeding; I, intervention; IBCLC, International Board Certified Lactation Consultant; LC, lactation consultant; PC, peer counseling; PP, postpartum; RN, registered nurse; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Peer counseling
Four randomized trials evaluating PC interventions were identified (Table 1). Three PC trials targeted a low-income, predominantly Puerto Rican sample delivering at a Baby-Friendly Hospital in Hartford, Connecticut (6, 25, 26). Each of these interventions involved PC prenatal home visits, daily in-hospital support, PP home visits, telephone support, and free breast pumps as needed. Chapman et al. (6) evaluated the effectiveness of an existing PC program (vs. standard care), whereas Anderson et al. (25) evaluated the efficacy of a more intensive intervention promoting exclusive breastfeeding (vs. standard care). In the third PC trial (26), a specialized PC intervention targeting overweight and obese women was compared with usual care. The fourth PC trial was conducted by Merewood et al. (27) among predominantly black women who chose to breastfeed their otherwise healthy, premature infants in the neonatal intensive care unit of a Baby-Friendly hospital in Boston, Massachusetts.
The impact of PC on breastfeeding initiation was evaluated in 3 studies (6, 25, 26) that recruited women who were considering breastfeeding. In 2 of these studies (6, 25), considerable increases in breastfeeding initiation rates were observed (91 vs. 77% (P < 0.05), and 91 vs. 76% (P < 0.05), respectively). At the time of the third PC study by this group (26), breastfeeding initiation was nearly universal (97 vs. 99%).
In the study by Merewood et al. (27), the rate of any breastfeeding at 12 wk PP was considerably higher in the intervention group than in controls (OR: 2.81, 95% CI: 1.11–7.14; P = 0.03). In the studies by Chapman et al. (6, 26) and Anderson et al. (25), the rates of any breastfeeding at 3 mo PP were higher in the intervention (vs. control) groups, but this difference did not reach statistical significance.
Improvements in either exclusive breastfeeding rates or in the percentage of feedings derived from breast milk were observed in 2 PC studies, along with improvements in health outcomes. Anderson et al. (25) demonstrated that their PC intervention (vs. control) produced a great improvement in exclusive breastfeeding rates at 3 mo PP (27 vs. 3%, P < 0.05), along with a considerable reduction in infant diarrhea at 3 mo (18 vs. 38%, P < 0.05), and a considerable increase in lactational amenorrhea in their intervention (vs. control) group. In the PC trial targeting overweight/obese women (26), significantly more women in the intervention group gave ≥50% of feedings as breast milk at 2 wk PP than the control group. This may account for the large decrease in the rate of infant rehospitalization in the intervention (vs. control) group (8 vs. 22%, P < 0.05). The other PC trials (6, 27) were not designed to promote exclusive breastfeeding and did not observe improvements in exclusive breastfeeding rates.
In combination, these studies indicate that PC can improve breastfeeding initiation, duration, exclusivity, and select infant health outcomes. These studies may underestimate the true effect of breastfeeding PC due to the relatively high level of breastfeeding support provided to the control groups at each of these Baby-Friendly institutions.
Professional support
We identified 4 randomized trials evaluating breastfeeding interventions delivered by health care professionals, with 2 using nurses (28, 29) and 2 providing LC support (30–32) (Table 1). In Denver, Colorado, Bunik et al. (28) tested an intervention among a Mexican-American population, consisting of daily telephone calls from a bilingual nurse from the date of hospital discharge through PP day 14. In contrast, Grossman et al. (29) evaluated an intervention providing both in-person and telephone support from a nurse (4 hospital visits and 4 telephone calls) to predominantly black mothers from Columbus, Ohio.
Regardless of whether telephone support was provided alone (28) or in combination with in-person support (29), neither intervention resulted in improvements in the rates of any breastfeeding at 3 or 6 mo PP. However, Bunik et al. demonstrated that daily telephone support (vs. controls) resulted in lower rates of health care use for sick infant visits by 1 mo of life (25 vs. 36%, P = 0.05) (28).
Bonuck et al. (30, 31) evaluated an intervention in which LCs provided a multiethnic sample of Bronx, New York, women with 3 visits (2 prenatal plus 1 PP), along with bilingual telephone support as needed. Petrova et al. (32) evaluated a somewhat less intensive LC intervention (3 visits + 2 telephone calls) targeting a predominantly Mexican-American population in New Brunswick, New Jersey.
The intervention tested by Bonuck et al. (31) yielded impressive results with significantly higher rates of any breastfeeding through 20 wk PP, with the exception of week 18 (53 vs. 39%, P < 0.05) and greater breastfeeding intensity (defined as more than half of feedings derived from breast milk in this study) through 9 wk (46 vs. 33%, P < 0.05) in the intervention (vs. control) group. Petrova et al. (32) evaluated exclusive breastfeeding rates through 3 mo PP and found improved rates in their intervention group; however, the difference did not reach statistical significance. The difference in the magnitude of the results between these 2 LC interventions may be attributable to the fact that the Bonuck et al. study used bilingual staff, whereas Petrova et al. relied on a translating service when needed. In addition, Bonuck et al. assessed breastfeeding intensity (based on the percentage of feedings derived from breast milk) compared with the stricter assessment of exclusive breastfeeding used by Petrova et al.
Breastfeeding interventions delivered by nurses appear to be less successful than similar interventions delivered by LCs. However, the 2 studies evaluating LC interventions yielded different results. It is possible that the more successful LC interventions (31) were partially due to an increased acceptance of health messages delivered by the bilingual LCs who had built a strong rapport with their clients.
Breastfeeding team.
Three publications were identified that evaluated a breastfeeding team in which a PC and a professional work together to provide breastfeeding support. Pugh et al. (33) conducted a pilot study in 2002 that paired a nurse and a PC to form a breastfeeding team who provided breastfeeding education and support to a low-income, predominantly black population. Based on the encouraging, but not statistically significant, results of the pilot study, they conducted a larger study (34), with the intervention consisting of daily in-hospital visits and 3 PP home visits from the team, PC telephone support through 6 mo PP, and unlimited access to a nurse via pager.
In adjusted analyses, this intervention yielded a considerable improvement in the rate of any breastfeeding at 6 wk vs. controls (OR: 1.7, 95% CI: 1.1–2.8; P = 0.03) with marginally significant improvements in the rate of any breastfeeding at 12 wk (OR: 1.6, 95% CI: 1.0–2.5; P = 0.05). The results of this study should be interpreted with caution because the breastfeeding team collected breastfeeding outcome data from the intervention group, thus introducing the potential for bias.
Wambach et al. (35) evaluated the impact of a breastfeeding team composed of an LC and a peer counselor on the breastfeeding outcomes of black adolescents residing in the Midwestern United States. This intervention consisted of 2 prenatal group classes, 1 PC hospital visit, 5 PP telephone calls by the peer counselor or LC, and provision of breast pumps as needed. In this study, the intervention group was compared with an attention control group (taught prenatal and childbirth material by an advanced practice nurse + peer counselor) and a usual care group (controls). The main effect of this intervention was a significant, nearly 3-fold increase in the median duration of any breastfeeding among the intervention compared with the attention control and usual care groups (177 vs. 42 vs. 61 d, respectively; P < 0.001). Bivariate analyses showed a significant difference between the groups regarding breastfeeding initiation rate (79 vs. 66 vs. 63%, respectively; P < 0.05) for the intervention, attention control, and usual care groups. However, when adjusting for factors such as breastfeeding knowledge, intentions, and social support, the group effect was not significant. There were no noteworthy differences in exclusive breastfeeding rates at 3 wk. The large effect on the duration of any breastfeeding may be partially attributed to the social support created in this teen clinic. The concept of the breastfeeding team clearly has potential and needs to be further evaluated.
Breastfeeding-specific clinic appointment.
We identified 2 studies that randomized women to receive an additional clinic appointment focused on breastfeeding. Serwint et al. (36) assigned pregnant, nulliparous, predominantly black women to receive a mailed appointment card to attend a prenatal pediatric clinic appointment that focused on breastfeeding. The clinic was staffed by pediatric residents who had received 3 h of additional breastfeeding training. The response rate for the clinic appointment was 68%. This study was underpowered because enrollment was curtailed when prenatal pediatric clinic appointments became the standard of care. This likely contributed to the nonsignificant difference in breastfeeding initiation and duration rates between the study groups. However, the intervention successfully affected breastfeeding decisions. Among breastfeeding mothers, 45% of those in the intervention group had not planned to breastfeed, but changed their minds and decided to breastfeed compared with 14% of controls (P < 0.05).
In another randomized trial, Hopkinson et al. (37) randomly assigned Hispanic mixed feeders to receive a breastfeeding clinic appointment card at hospital discharge. The clinic was staffed by peer counselors working under the supervision of an LC. Phone consults were offered to women who could not attend the clinic. The intervention clinic was well attended, with 80% of the intervention group having a clinic appointment or telephone consult by 3 wk PP. At 4 wk PP, the intervention group had a significantly higher rate of exclusive breastfeeding than controls (based on 24-h recall). This increase in exclusive breastfeeding was achieved by substantial reductions in the provision of water, tea, and formula.
The concept of additional clinic appointments designed to promote breastfeeding appears promising. Further research is needed to better understand the optimal timing of the clinic appointment (prenatal vs. PP), as well as the effect for specific target populations (i.e., mixed feeders vs. those exclusively breastfeeding; primiparae vs. multiparae).
Group prenatal education.
We identified 3 publications evaluating the impact of a group prenatal counseling format on breastfeeding outcomes, with each study assessing a different intervention (Table 1). In 1990, Kistin et al. (38) evaluated the impact of midwives providing either a group prenatal breastfeeding class (50–80 min), individual breastfeeding education sessions (15–30 min), or standard care (no additional breastfeeding education) among black women in Chicago, Illinois. Building on the group education concept, Ickovics et al. (39) evaluated the impact of the group prenatal care model on breastfeeding initiation. In their study, predominantly black (78%) and Hispanic (13%) women from New Haven, Connecticut, and Atlanta, Georgia, were randomly assigned to receive all their prenatal care either in a group setting (20 h of contact time) or during individual appointments (2 h of contact time). Using a unique approach, Wolfberg et al. (40) evaluated a breastfeeding class targeting the male partners of pregnant, predominantly black women. This 2-h intervention consisted of an informal, interactive breastfeeding class taught by a black father in which men learned the benefits of breastfeeding, ways to support their partners’ decision to breastfeed, and strategies to deal with those who may not be supportive of breastfeeding.
Each of these studies demonstrated a significant improvement in breastfeeding initiation rates in the intervention group. Of the 2 studies (38, 40) evaluating the impact of the intervention on PP breastfeeding rates, only Kistin et al. (38) demonstrated a significant improvement. Kistin et al. observed higher rates of any breastfeeding at 12 wk among women receiving the group class compared with the individual session and controls (P < 0.05). Additionally, similar to the findings of Serwint et al. (36), the individual session (vs. control and classes) resulted in a significant increase in breastfeeding initiation among women who had planned to formula feed (38 vs. 8 vs. 21%, respectively; P < 0.001). None of these studies evaluated breastfeeding exclusivity.
These studies demonstrate that group prenatal education can have a significant impact on breastfeeding initiation. Further research is needed to determine whether extending groups into the PP period or developing groups for other family support members (i.e., Hispanic grandmothers) would have a significant impact on breastfeeding duration or exclusivity.
Enhanced breastfeeding programs.
We identified 2 studies that evaluated the effectiveness of program add-ons on breastfeeding outcomes. Frank et al. (41) evaluated a combination of hospital-based interventions (research discharge bags vs. research counseling) versus both (research bags + research counseling) versus standard care (commercial discharge packs and limited breastfeeding counseling)) among predominantly minority women (65% black, 19% Hispanic). Although there were no important differences in breastfeeding duration between groups, there was a considerably longer duration of exclusive breastfeeding (which was defined as providing only breast milk for the previous 24 h, but did allow formula less than once per week) among women receiving the research bags (either alone or in combination with the research counseling [P < 0.01, 1-tailed log rank test]) versus those not receiving research bags. Infants receiving the research bags + research counseling were significantly less likely to be rehospitalized by 4 mo of age (P < 0.05, 2 sided test) compared with those receiving research counseling only. The results of this study should be evaluated in light of the use of a nonstandard definition of exclusive breastfeeding.
Caulfield et al. (42) and Gross et al. (43) describe the results of a WIC intervention in which similar WIC clinics serving black women were randomized to offer enhanced breastfeeding services (PC vs. breastfeeding video/pamphlets in the waiting room vs. both interventions combined vs. standard WIC care). Adjusted analyses demonstrate that attendance in the clinic offering only PC services was significantly associated with an increased breastfeeding initiation rate (42). Among women who initiated breastfeeding, the risk of breastfeeding termination by 4 mo PP was significantly lower in all the intervention clinics compared with the control clinic (P < 0.05) (43).
These studies demonstrate that enhanced hospital practices and WIC-based services can have a considerable impact on breastfeeding outcomes and serve as part of the impetus for both the widespread adoption of PC within the WIC program and breastfeeding promotion campaigns.
Conclusions
This critical review identified several interventions that successfully improved breastfeeding outcomes among minority women in the United States, including PC, breastfeeding teams (a peer counselor working with a health professional), group prenatal classes, breastfeeding-specific clinic appointments, and hospital/WIC policy change. Breastfeeding interventions provided by nurses working alone were generally less effective than the other types of interventions. This may highlight the need for a more diverse health care workforce who develops a better rapport with minority women (8).
The efforts needed to minimize the disparities in breastfeeding outcomes in the United States will likely require a multifaceted effort, involving several types of interventions evaluated in this critical review. Breastfeeding PC has been demonstrated to be an effective intervention (44) and is being scaled-up through widespread use of breastfeeding peer counselors in the WIC program. Similarly, many U.S. hospitals are working toward Baby-Friendly certification, which would prohibit distribution of free formula and formula promotional materials, including discharge bags.
Further research is needed to provide an in-depth evaluation of some of the more promising interventions. For example, we need to determine the optimal timing and amount of PC services and evaluate how PC services can be best tailored to meet the needs of teens, obese women, and specific ethnic groups. Both ongoing prenatal classes and the group prenatal care model show potential for improving breastfeeding initiation, and further research should evaluate the impact of the PP continuation of these groups on breastfeeding duration and exclusivity. The scheduling of a medical appointment that completely focuses on breastfeeding appears effective in improving breastfeeding outcomes, possibly because it reflects the endorsement of breastfeeding by the medical community. Similarly, a single prenatal breastfeeding class specifically targeting male partners effectively increased breastfeeding initiation. Further research is needed to evaluate both the impact of classes targeting other family members (i.e., Hispanic grandmothers) and the degree to which ongoing (vs. one-time) classes can improve breastfeeding duration and exclusivity.
Our critical review identified key research gaps that should be addressed. The first is in regard to the definition of exclusive breastfeeding. Although most of the included studies used the WHO definition of exclusive breastfeeding (3), few clearly indicated the timeframe within which exclusive breastfeeding was assessed. For example, some categorized women as exclusively breastfeeding using the strictest definition (i.e., if the child had not received anything except breast milk, allowing for medications and vitamin/mineral drops since birth). Others evaluated exclusive breastfeeding based on a single 24-h recall. Obviously, the latter would overestimate the true incidence of exclusive breastfeeding. These discrepancies make it difficult to compare exclusive breastfeeding outcomes among studies. Where possible, it is recommended that researchers clarify the timeframe of the exclusive breastfeeding assessment or to assess it in multiple timeframes (i.e., since birth, in the past month, week, or day).
Another research gap is that there were no published randomized trials evaluating interventions targeting Native Americans or Asians. Native Americans have high rates of breastfeeding initiation, but breastfeeding continuation and exclusivity decrease more rapidly than in most other ethnic groups (except blacks) (2). Similarly, Asians have high rates of breastfeeding initiation, but unfortunately have the highest rates of formula supplementation of breast-fed infants at 6 and 12 mo (2). Qualitative research in this area would be useful to better understand the decision-making process resulting in formula supplementation.
To provide justification for the scale-up of effective breastfeeding interventions, it is essential to assess not only breastfeeding outcomes, but also health care use and program costs. Significant decreases in infant morbidity/rehospitalization were reported in 6 of the randomized trials included in this review (25, 26, 28, 30, 33, 41). It is not known whether these data were collected in other studies. Where possible, future studies should strive to collect data on infant rehospitalization and morbidity to capture the full effect of the tested interventions. Data on intervention costs were presented in relatively few studies (33, 39). Although cost-benefit analyses have been conducted that evaluated breastfeeding (45), more work is needed in this area to allow the allocation of limited health care resources to the most effective interventions. Future collaborations with health economists will provide valuable cost-benefit analyses, which can help to determine the most cost-effective means of improving breastfeeding outcomes.
Acknowledgments
Both authors read and approved the final manuscript.
Footnotes
Author disclosures: Donna J. Chapman and Rafael Pérez-Escamilla, no conflicts of interest.
Abbreviations used: HP2020, Healthy People 2020; LC, lactation consultant; PC, peer counseling; PP, postpartum; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Literature Cited
- 1.Gartner LM, Morton J, Lawrence RA, Naylor AJ, O'Hare D, Schanler RJ, Eidelman AI. Breastfeeding and the use of human milk. Pediatrics. 2005;115:496–506 [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Provisional breastfeeding rates by sociodemographic factors, among children born in. 2007 (percent +/− half 95% confidence interval). Available from: http://www.cdc.gov/breastfeeding/data/NIS_data/2007/socio-demographic_any.htm. [Google Scholar]
- 3.World Health Organization Infant and young child nutrition: global strategy on infant and young child feeding, vol. A55. Geneva, Switzerland: World Health Organization; 2002 [Google Scholar]
- 4.Centers for Disease Control and Prevention Provisional formula supplementation of breast milk rates by socio-demographic factors, among children born in 2007. Available from: http://www.cdc.gov/breastfeeding/data/NIS_data/2007/socio-demographic_formula.htm [Google Scholar]
- 5.Chapman DJ, Perez-Escamilla R. US national breastfeeding monitoring and surveillance: current status and recommendations. J Hum Lact. 2009;25:139–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chapman DJ, Damio G, Young S, Perez-Escamilla R. Effectiveness of breastfeeding peer counseling in a low-income, predominantly Latina population: a randomized controlled trial. Arch Pediatr Adolesc Med. 2004;158:897–902 [DOI] [PubMed] [Google Scholar]
- 7.Kaufman L, Deenadayalan S, Karpati A. Breastfeeding ambivalence among low-income African American and Puerto Rican women in north and central Brooklyn. Matern Child Health J. 2010;14:696–704 [DOI] [PubMed] [Google Scholar]
- 8.Cricco-Lizza R. The milk of human kindness: environmental and human interactions in a WIC clinic that influence infant-feeding decisions of Black women. Qual Health Res. 2005;15:525–38 [DOI] [PubMed] [Google Scholar]
- 9.Nommsen-Rivers LA. Chantry CJ, Cohen RJ, Dewey KG. Comfort with the idea of formula feeding helps explain ethnic disparity in breastfeeding intentions among expectant first-time mothers. Breastfeed Med. 2010;5:25–33 [DOI] [PubMed] [Google Scholar]
- 10.Beal AC, Kuhlthau K, Perrin JM. Breastfeeding advice given to African American and white women by physicians and WIC counselors. Public Health Rep. 2003;118:368–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Evans K, Labbok M, Abrahams SW: WIC and breastfeeding support services: does the mix of services offered vary with race and ethnicity? Breastfeed Med. Epub 2011 Mar 31 [DOI] [PubMed] [Google Scholar]
- 12.Cricco-Lizza R. Black non-Hispanic mothers’ perceptions about the promotion of infant-feeding methods by nurses and physicians. J Obstet Gynecol Neonatal Nurs. 2006;35:173–80 [DOI] [PubMed] [Google Scholar]
- 13.Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, Trikalinos T, Lau J. Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Rep). 2007;(153):1–186 [PMC free article] [PubMed] [Google Scholar]
- 14.Hauck FR, Thompson JM, Tanabe KO, Moon RY, Vennemann MM. Breastfeeding and reduced risk of sudden infant death syndrome: a meta-analysis. Pediatrics. 2011;128:103–10 [DOI] [PubMed] [Google Scholar]
- 15.Quigley MA, Cumberland P, Cowden JM, Rodrigues LC. How protective is breast feeding against diarrhoeal disease in infants in 1990s England? A case-control study. Arch Dis Child. 2006;91:245–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use, and mortality: United States, 2005–2009. Natl Health Stat Report. 2011;(32):1–14 [PubMed] [Google Scholar]
- 17.Beckles GL, Zhu J, Moonesinghe R. Diabetes - United States, 2004 and 2008. MMWR Surveill Summ. 2011;60(Suppl):90–3 [PubMed] [Google Scholar]
- 18.Iwane MK, Edwards KM, Szilagyi PG, Walker FJ, Griffin MR, Weinberg GA, Coulen C, Poehling KA, Shone LP, Balter S, et al. Population-based surveillance for hospitalizations associated with respiratory syncytial virus, influenza virus, and parainfluenza viruses among young children. Pediatrics. 2004;113:1758–64 [DOI] [PubMed] [Google Scholar]
- 19.Kitsantas P, Gaffney KF. Racial/ethnic disparities in infant mortality. J Perinat Med. 2010;38:87–94 [DOI] [PubMed] [Google Scholar]
- 20.Moorman JE, Zahran H, Truman BI, Molla MT. Current asthma prevalence - United States, 2006–2008. MMWR Surveill Summ. 2011;60:(Suppl:84–6 [PubMed] [Google Scholar]
- 21.Moss BG, Yeaton WH. Young children's weight trajectories and associated risk factors: results from the Early Childhood Longitudinal Study-Birth Cohort. Am J Health Promot. 2011;25:190–8 [DOI] [PubMed] [Google Scholar]
- 22.Singleton RJ, Wirsing EA, Haberling DL, Christensen KY, Paddock CD, Hilinski JA, Stoll BJ, Holman RC. Risk factors for lower respiratory tract infection death among infants in the United States, 1999–2004. Pediatrics. 2009;124:e768–76 [DOI] [PubMed] [Google Scholar]
- 23.Shaw TE, Currie GP, Koudelka CW, Simpson EL. Eczema prevalence in the United States: data from the 2003 National Survey of Children's Health. J Invest Dermatol. 2011;131:67–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shealy KR, Li R, Benton-Davis S, Grummer-Strawn LM. The CDC Guide to Breastfeeding Interventions. Atlanta: US Department of Health and Human Services, Centers for Disease Control and Prevention, 2005 [Google Scholar]
- 25.Anderson AK, Damio G, Young S, Chapman DJ, Perez-Escamilla R. A randomized trial assessing the efficacy of peer counseling on exclusive breastfeeding in a predominantly Latina low-income community. Arch Pediatr Adolesc Med. 2005;159:836–41 [DOI] [PubMed] [Google Scholar]
- 26.Chapman D, Morel K, Bermudez-Millan A, Young S, Damio G, Kyer N, Perez-Escamilla R. Breastfeeding Education and Support Trial for Obese Women: Effects of a specialized peer counseling intervention on breastfeeding and health outcomes. J Hum Lact. 2011;27:75–76 [Google Scholar]
- 27.Merewood A, Chamberlain LB, Cook JT, Philipp BL, Malone K, Bauchner H. The effect of peer counselors on breastfeeding rates in the neonatal intensive care unit: results of a randomized controlled trial. Arch Pediatr Adolesc Med. 2006;160:681–5 [DOI] [PubMed] [Google Scholar]
- 28.Bunik M, Shobe P, O'Connor ME, Beaty B, Langendoerfer S, Crane L, Kempe A. Are 2 weeks of daily breastfeeding support insufficient to overcome the influences of formula? Acad Pediatr. 2010;10:21–8 [DOI] [PubMed] [Google Scholar]
- 29.Grossman LK, Harter C, Sachs L, Kay A. The effect of postpartum lactation counseling on the duration of breast-feeding in low-income women. Am J Dis Child. 1990;144:471–4 [DOI] [PubMed] [Google Scholar]
- 30.Bonuck KA, Freeman K, Trombley M. Randomized controlled trial of a prenatal and postnatal lactation consultant intervention on infant health care use. Arch Pediatr Adolesc Med. 2006;160:953–60 [DOI] [PubMed] [Google Scholar]
- 31.Bonuck KA, Trombley M, Freeman K, McKee D. Randomized, controlled trial of a prenatal and postnatal lactation consultant intervention on duration and intensity of breastfeeding up to 12 months. Pediatrics. 2005;116:1413–26 [DOI] [PubMed] [Google Scholar]
- 32.Petrova A, Ayers C, Stechna S, Gerling JA, Mehta R. Effectiveness of exclusive breastfeeding promotion in low-income mothers: a randomized controlled study. Breastfeed Med. 2009;4:63–9 [DOI] [PubMed] [Google Scholar]
- 33.Pugh LC, Milligan RA, Frick KD, Spatz D, Bronner Y. Breastfeeding duration, costs, and benefits of a support program for low-income breastfeeding women. Birth. 2002;29:95–100 [DOI] [PubMed] [Google Scholar]
- 34.Pugh LC, Serwint JR, Frick KD, Nanda JP, Sharps PW, Spatz DL, Milligan RA. A randomized controlled community-based trial to improve breastfeeding rates among urban low-income mothers. Acad Pediatr. 2010;10:14–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wambach KA, Aaronson L, Breedlove G, Domian EW, Rojjanasrirat W, Yeh HW. A randomized controlled trial of breastfeeding support and education for adolescent mothers. West J Nurs Res. 2011;33:486–505 [DOI] [PubMed] [Google Scholar]
- 36.Serwint JR, Wilson ME, Vogelhut JW, Repke JT, Seidel HM. A randomized controlled trial of prenatal pediatric visits for urban, low-income families. Pediatrics. 1996;98:1069–75 [PubMed] [Google Scholar]
- 37.Hopkinson J, Konefal Gallagher M. Assignment to a hospital-based breastfeeding clinic and exclusive breastfeeding among immigrant Hispanic mothers: a randomized, controlled trial. J Hum Lact. 2009;25:287–96 [DOI] [PubMed] [Google Scholar]
- 38.Kistin N, Benton D, Rao S, Sullivan M. Breast-feeding rates among black urban low-income women: effect of prenatal education. Pediatrics. 1990;86:741–6 [PubMed] [Google Scholar]
- 39.Ickovics JR, Kershaw TS, Westdahl C, Magriples U, Massey Z, Reynolds H, Rising SS. Group prenatal care and perinatal outcomes: a randomized controlled trial. Obstet Gynecol. 2007;110:330–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wolfberg AJ, Michels KB, Shields W, O'Campo P, Bronner Y, Bienstock J. Dads as breastfeeding advocates: results from a randomized controlled trial of an educational intervention. Am J Obstet Gynecol. 2004;191:708–12 [DOI] [PubMed] [Google Scholar]
- 41.Frank DA, Wirtz SJ, Sorenson JR, Heeren T. Commercial discharge packs and breast-feeding counseling: effects on infant-feeding practices in a randomized trial. Pediatrics. 1987;80:845–54 [PubMed] [Google Scholar]
- 42.Caulfield LE, Gross SM, Bentley ME, Bronner Y, Kessler L, Jensen J, Weathers B, Paige DM. WIC-based interventions to promote breastfeeding among African-American Women in Baltimore: effects on breastfeeding initiation and continuation. J Hum Lact. 1998;14:15–22 [DOI] [PubMed] [Google Scholar]
- 43.Gross SM, Caulfield LE, Bentley ME, Bronner Y, Kessler L, Jensen J, Paige VM. Counseling and motivational videotapes increase duration of breast-feeding in African-American WIC participants who initiate breast-feeding. J Am Diet Assoc. 1998;98:143–8 [DOI] [PubMed] [Google Scholar]
- 44.Chapman DJ, Morel K, Anderson AK, Damio G, Perez-Escamilla R. Breastfeeding peer counseling: from efficacy through scale-up. J Hum Lact. 2010;26:314–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bartick M, Reinhold A. The burden of suboptimal breastfeeding in the United States: a pediatric cost analysis. Pediatrics. 2010;125:e1048–56 [DOI] [PubMed] [Google Scholar]