Abstract
Objective. This study aims to evaluate the effect of a multidisciplinary treatment of obesity on plasma concentrations of several gut hormones in fasting condition and in response to a mixed meal in children. Methods. Complete data were available from 36 obese children (age 13.3 ± 2.0 yr). At baseline and after the 3-month multidisciplinary treatment, fasting and postprandial blood samples were taken for glucose, insulin, ghrelin, peptide YY (PYY), and glucagon-like peptide 1 (GLP-1). Results. BMI-SDS was significantly reduced by multidisciplinary treatment (from 4.2 ± 0.7 to 4.0 ± 0.9, P < .01). The intervention significantly increased the area under the curve (AUC) of ghrelin (from 92.3 ± 18.3 to 97.9 ± 18.2 pg/L, P < .01), but no significant changes were found for PYY or GLP-1 concentrations (in fasting or postprandial condition). The insulin resistance index (HOMA-IR) remained unchanged as well. Conclusion. Intensive multidisciplinary treatment induced moderate weight loss and increased ghrelin secretion, but serum PYY and GLP-1 concentrations and insulin sensitivity remained unchanged.
1. Introduction
Childhood obesity has become a global problem [1]. Understanding the mechanisms that control energy balance and fuel flux in children is of paramount importance for the design of effective strategies to combat this health hazard. The gastrointestinal tract plays a critical role in the control of feeding behavior and fuel metabolism. In response to food intake, the gut produces a variety of hormones that inhibit food intake, promote glucose induced insulin release, and/or facilitate insulin action (e.g., glucagon-like peptide 1 (GLP-1), peptide YY (PYY)) [2–4]. Conversely, in the absence of food, the stomach produces ghrelin, which stimulates appetite to initiate feeding [4, 5].
In a number of studies, plasma levels of ghrelin in obese children were compared with those of normal weight controls. Generally, the plasma ghrelin concentration of obese children is lower in fasting condition [6–10], whereas the decline in response to glucose ingestion varies as a function of insulin sensitivity; the decline appears to be less profound in insulin resistant obese children [6, 11], although the data are equivocal [12]. Weight loss tends to normalize circulating ghrelin levels [8, 10, 13], although this is still a subject for debate [5, 14].
In fasting condition, plasma GLP-1 and PYY levels were reported to be similar in obese and lean children [9, 15–18], but in other studies lower PYY [19] and lower GLP-1 were found in obese children [20]. Postprandial concentrations of the two hormones are consistently lower in obese versus normal weight peers [15, 20, 21]. The few studies that have examined the effect of weight loss on the release of these hormones in obese children found significantly increased fasting PYY [19] and (surprisingly) decreased fasting GLP-1 [18] after weight reduction.
Because gut hormones are intimately involved in the control of energy balance, better understanding of intestinal endocrine (mal) function in obese children may contribute to the development of strategies to treat their condition. Here we aim to evaluate the effect of a 3-month multidisciplinary intervention program to reduce the bodyweight of obese children on plasma gut hormone concentrations in fasting condition and in response to a standard meal.
2. Materials and Methods
2.1. Participants, Study Design, and Settings
This study is part of a randomized clinical trial on the effect of multidisciplinary treatment on childhood obesity [22]. Here the effects of lifestyle intervention on various clinical and physiological features of the obese children in the intervention group are analyzed. Characteristics of the obese control group as well as treatment effect over the course of 1 and 2 years followup were the topic of a previous study [23]. The study inclusion criteria were simple obesity (as defined by Cole [24]), age 8–17 years, and referral to a pediatrician. Potential participants were excluded if their knowledge of the Dutch language, intelligence, or social skills were insufficient to participate in the trial. Other exclusion criteria were use of medication that might have an effect on weight loss, medical comorbidity (e.g., hypothyroidism, high dose of glucocorticoids, diabetes mellitus) that could affect trial outcome, or previous enrollment in another cognitive behavioral treatment program with a focus on reducing body weight. Forty children were randomized to the intervention group, of whom 36 completed the treatment. The study was conducted according to the “Declaration of Helsinki”, and approval was obtained from the regional medical ethical committee South West Holland. All parents and children gave their written informed consent after they had been given detailed written explanations of the aims of the study, discomfort, and inconvenience, and the option to withdraw at any time.
2.2. Intervention
The multidisciplinary lifestyle treatment of the intervention group consisted of a screening phase of individual counseling of the children with their parents, followed by an intensive phase of group sessions during three months. The group treatment consisted of 7 group meetings for the children, 5 separate parent meetings, and 1 parent meeting together with the children. Meetings of 2.5 hours were held once every 2 weeks. The children meetings were held on weekday afternoons at the hospital. The 5 separate parent meetings were provided on weekdays after working hours. Subsequently, refresh follow-up sessions (2-3 sessions/year) were offered for a total period of two years (Table 1).
Table 1.
Characteristics of the family-based multidisciplinary lifestyle intervention.
| Components | Description |
|---|---|
| Screening phase/individual counseling | During the screening phase, children and their parents were interviewed at two separate occasions and all individually by the multidisciplinary team consisting of a dietitian, a child physiotherapist, a child psychologist, and a social worker. Throughout those two separate meetings, an individual advice was given by the multidisciplinary team, based on the personal situation of each participating family. |
|
| |
| Individual nutritional advice | A 3-day dietary recall (1 weekend day included) was used by the dietitian to get more insight in dietary habits of the children. Information was provided about nutrition and healthy eating behavior according to the traffic light nutritional list [25]. The traffic light nutritional list identifies several main food groups (fruits, vegetables, grains, milk and other dairy products, meat, fish, and others). Foods within each group were color-coded so as to reflect the caloric density per average serving and Dutch standards for healthy nutrition. The colors are green for “go”, orange for “approach with caution”, and red for “stop”. The children and parents were involved in planning their own daily diet for themselves according to the traffic light nutritional list. |
|
| |
| Individual physical activity counseling | To obtain insight in the child's general physical activity behavior during the week, a physical activity questionnaire was filled out by a child physiotherapist. Children were asked about how they traveled to school (by foot, by bicycle, by public transportation, or by car), physical fitness classes at school, spire time sport activities, and daily computer and TV use as well as the duration spend at all these activities. The information from this questionnaire was used for advice on how to increase and optimize physical activity during everyday life, such as walking to nearby destinations and reducing sedentary activities (computer and TV use). |
|
| |
| Individual psychological counseling | By means of motivational interviewing, the child psychologist helped the children to adapting to a new lifestyle in order to reduce body weight. Before the child started with the group sessions, individual treatment goals (reduction of 10% of body weight during 3 months of group sessions) were written down in a contract to avoid disappointment. |
|
| |
| Children's group meetings | Most children with obesity have negative experiences with group activities. For example, they are often not included in social events or chosen last by peers during sport activities. Therefore, during the first session much time is spent in getting acquainted with each other. A good group bond is important for the effect of the treatment because peer support can be very helpful in the treatment of obese children. The main educational focus of the first two meetings is on nutritional information of a healthy eating pattern and the balance between energy intake and energy expenditure. During the subsequent meetings, emphasis was put in self-control techniques to cope with difficult situations (e.g., birthday parties, holidays, lunch breaks at school, being at home alone). Problem solving alternatives are debated (e.g., to avoid a situation, doing something else, participate in a situation and eat less, or participate followed by extra exercise afterwards). Other psychoeducational topics reviewed were self-reward (when coping well with a difficult situation) and self-regulation situations (making a plan how to integrate healthy behavior in daily living). Stimulus control was also one of the psychoeducational topics (remove unhealthy stimuli at home, encourage healthy behavior, eat at the dinner table, reduction of environmental stimuli linked to eating). Topics of the last two meetings were self-image (focus on positive things about themselves) and coping strategies on dealing with teasing. |
|
| |
| Parent group meetings | Topics discussed during the parent meetings included the necessity to change their own lifestyle as well, information on healthy nutrition (product information, quantities, eating moments, eating locations), and how to help their children. Parents received advice on parenting styles (boundaries setting with regard to eating behavior, giving positive feedback). During the last meeting, a therapist discusses the role of all other family members with regard to the treatment in the family (e.g., are other family members supportive, how do they cope with the lifestyle changes). |
|
| |
| Follow-up meetings | In order to maintain the newly learned behavior, refresh follow-up meetings were given during the first two years (2-3 meetings/year). The child psychologist and the social worker organize this follow-up meetings. The topics repeated were problem solving techniques and relapse prevention techniques. |
2.3. Clinical Measures
In this paper, the measurements taken at baseline (T1) and after 3 months treatment (T2) are analyzed and discussed. Weight was measured to the nearest of 0.1 kg using an electronic scale (SECA 911, Vogel & Halke, Hamburg, Germany) and height to the nearest of 0.1 cm with a stadiometer (Holtain, limited, Crymych, Dyfed, Britain) in underwear and barefoot by an experienced assistant. The BMI was calculated as weight/height squared (kg/m2). Subjects were classified as obese using BMI gender- and age-specific international cutoff levels [24]. BMI was expressed as standard deviation score (SDS) for Dutch references using the LMS method [26]. Pubertal development was recorded by the pediatrician according to Tanner [27].
2.4. Mixed Meal Tolerance Test
The children were asked to consume a daily amount of at least 150 g carbohydrates three days prior to the mixed meal tolerance test and to continue their normal daily physical activities. The day before the test the subjects were asked not to consume any food or drinks after 10 pm, with the exception of tap water. On the morning of the mixed meal tolerance test, the fasting state was verbally confirmed by the participant and a parent. A catheter was placed in an antecubital vein for blood sampling. Fasting blood samples were taken twice with a 15-minute interval (t = −15 and t = 0). After the second fasting blood sample was taken, the participants received a mixed meal bolus of 200 mL (Nutridrink Yoghurt Style, Nutricia, Zoetermeer, The Netherlands). The mixed meal bolus consisted of 49% carbohydrates, 35% lipids, and 16% proteins, with a total caloric content of 300 kcal. After the consumption of the mixed meal bolus, blood samples were taken two more times with a 15-minute interval (t = 15 and t = 30) and four times with 30-minute intervals (t = 60, t = 90, t = 120, and t = 150). Blood samples were analyzed for total ghrelin, PYY, GLP-1, glucose, and insulin.
2.5. Laboratory Analysis
Tubes for blood collection of GLP-1, PYY, and ghrelin and the inhibitor dipeptidyl peptidase IV (DPP-IV) (Linco Research, St. Charles, MO, USA) were placed on ice. Immediately after blood sampling, DPP-IV was added to tubes for measurement of GLP-1 and PYY to prevent degradation of these hormones. Blood samples for GLP-1, PYY, and ghrelin were centrifuged within one hour after sampling and stored at −80°C until analyzed. Baseline and T2 samples were analyzed in the same batches for all three hormones. Serum GLP-1 concentrations were measured by a highly specific enzyme-linked immunosorbent assay (human active GLP-1 ELISA Kit EGLP-35K, Linco Research, St. Charles, MO, USA; intra-assay coefficient of variation 8 ± 4.8%; interassay coefficient of variation 7.4 ± 1.1%; sensitivity 2 pM/L). PYY (3–36) concentration was determined by human radioimmunoassay (RIA) (PYY-67HK RIA Kit A 0.056, LincoResearch, St. Charles, MO, USA; intra-assay coefficient of variation 5.5–8.5%; interassay coefficient of variation 2.9–9.4%; accuracy 86.9 ± 5.2%). Total serum ghrelin was determined by human RIA as well (Ghrelin Total RIA GHRT-89HK Kit A 0.056 MBQ, Linco Research, St. Charles, MO, USA; intra-assay coefficient of variation 0.9–1.3%; interassay coefficient of variation 6.2–7.8%; sensitivity 30 pg/mL).
Glucose was analyzed from lithium heparine plasma by the glucose-oxydase method with the Unicel D × C 800 (Beckman Coulter, Woerden, the Netherlands). Plasma insulin concentration was measured by RIA (DSL-1600, Beckman Coulter, Woerden, the Netherlands; intra-assay coefficient of variation 4.5–8.3%; interassay coefficient of variation 4.7–12.2%; sensitivity 1.3 μU/mL). An index for insulin resistance was calculated according to the Homeostasis Assessment Model for insulin resistance (HOMA-IR) formula: (fasting insulin (μU/mL) × fasting glucose (mmol/L))/22.5 [28].
2.6. Statistical Analysis
The analysis was performed using the Statistical Package for Social Science SPSS, version 17.0 for Windows (SPSS Inc., Chicago, IL, USA), and the level of significance was set at P < .05. Data were checked for normality before analysis, using descriptive statistics for skewness, kurtosis, and Shapiro-Wilk test. The outcome variables for insulin were transformed to the natural logarithm. Data were expressed as mean ± standard deviation (continuous variables) and as count and percentage (categorical variables) unless otherwise defined. Values for the area under the curve (AUC) of 165 min (from t = −15 to t = 150 min) were calculated according to the trapezoid rule.
Paired t-tests were used to explore difference of the outcome variables after treatment, in total 16 paired t-tests were performed. A separate ANCOVA analysis was performed to determine if the change in AUC of the gut hormones over time (T2 versus T1) was effected by gender, age, pubertal stage, or change in BMI-SDS. In the ANCOVA analysis, the changes in AUC of the gut hormones were used as dependent variables, time (T2 versus T1) and gender as fixed variables, and age, pubertal stage, and change in BMI-SDS as covariates.
3. Results
3.1. Subjects
Forty subjects (18M/22F; age: 13.3 ± 2.0 years) were enrolled in the study, and 36 children completed both study occasions. One subject withdrew before all baseline measurements were completed, one discontinued treatment and two did not show up at T2 for personal reasons. No significant difference in baseline BMI-SDS or age was observed between completers (4.2 ± 0.7 SDS; 13.3 ± 1.8 years) and noncompleters (4.3 ± 0.3; 13.3 ± 3.1 years). Results are presented for the 36 children completing both study occasions (18M/18F).
3.2. Anthropometry and Metabolic Parameters
Changes between both study occasions in anthropometry and metabolic parameters are shown in Table 2. A significant reduction of BMI-SDS was found after 3 months of multidisciplinary lifestyle treatment.
Table 2.
Clinical and physiological parameters of the subjects with complete data (N = 36).
| Variables | Baseline (T1) | After (T2) | P Value* |
|---|---|---|---|
| BMI-SDS | 4.2 ± 0.7 | 4.0 ± 0.9 | .003 |
| HOMA-IR | 4.2 ± 2.5 | 4.1 ± 3.0 | NS |
| Glucose (fasting) (mmol/L) | 5.2 ± 0.4 | 5.3 ± 0.4 | NS |
| Glucose AUC (165 min × mmol/L) | 905 ± 67 | 896 ± 86 | NS |
| Insulin (fasting) (mU/L) | 18.0 ± 10.7 | 17.4 ± 12.5 | NS |
| Insulin AUC (165 min × U/L)† | 10.3 ± 6.1 | 11.0 ± 8.0 | NS |
| Ghrelin (fasting) (pg/mL) | 612 ± 143 | 641 ± 144 | NS |
| Ghrelin AUC (165 min × pg/L)† | 92.3 ± 18.3 | 97.9 ± 18.2 | .006 |
| PYY (fasting) (pg/mL) | 90.2 ± 34.6 | 95.5 ± 32.8 | NS |
| PYY AUC (165 min × pg/L) | 16.3 ± 4.6 | 15.3 ± 5.0 | NS |
| GLP-1 (fasting) (pM/L) | 2.6 ± 0.9 | 2.5 ± 0.9 | NS |
| GLP-1 AUC (165 min × pM/L) | 567 ± 192 | 552 ± 197 | NS |
*P value T2 versus T1 (paired t-test).
Fasting plasma glucose and insulin concentrations (and consequently HOMA-IR) were similar at baseline (T1) and after treatment (T2). The AUC of plasma glucose and insulin concentrations in response to the meal was also not affected by intervention (Figures 1(a) and 1(b)).
Figure 1.
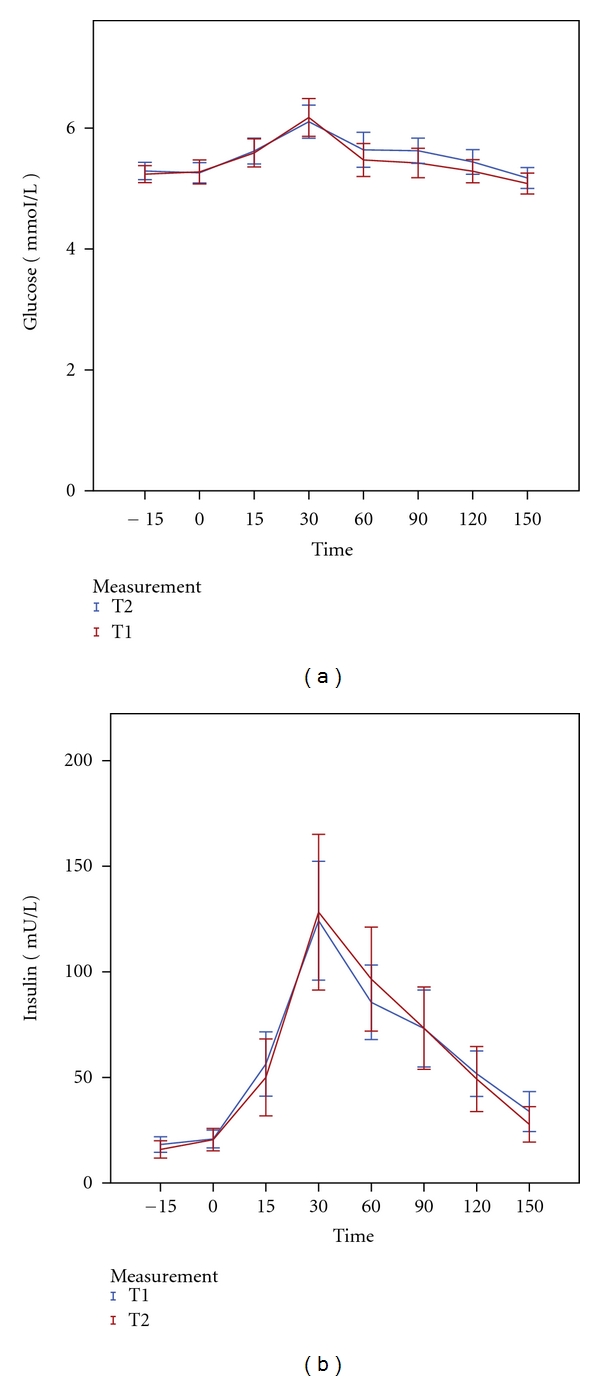
Mean plasma levels (±2SE) of Glucose (a) and Insulin (b) in response to a mixed meal at baseline (T1) versus after intervention (T2).
3.3. Gut Hormones
The ghrelin AUC in response to the meal was slightly, but significantly increased after treatment. Fasting levels were not significantly affected (Figure 2(a)). The treatment did not affect either fasting or postprandial plasma GLP-1 and PYY concentrations (Figures 2(b) and 2(c)).
Figure 2.
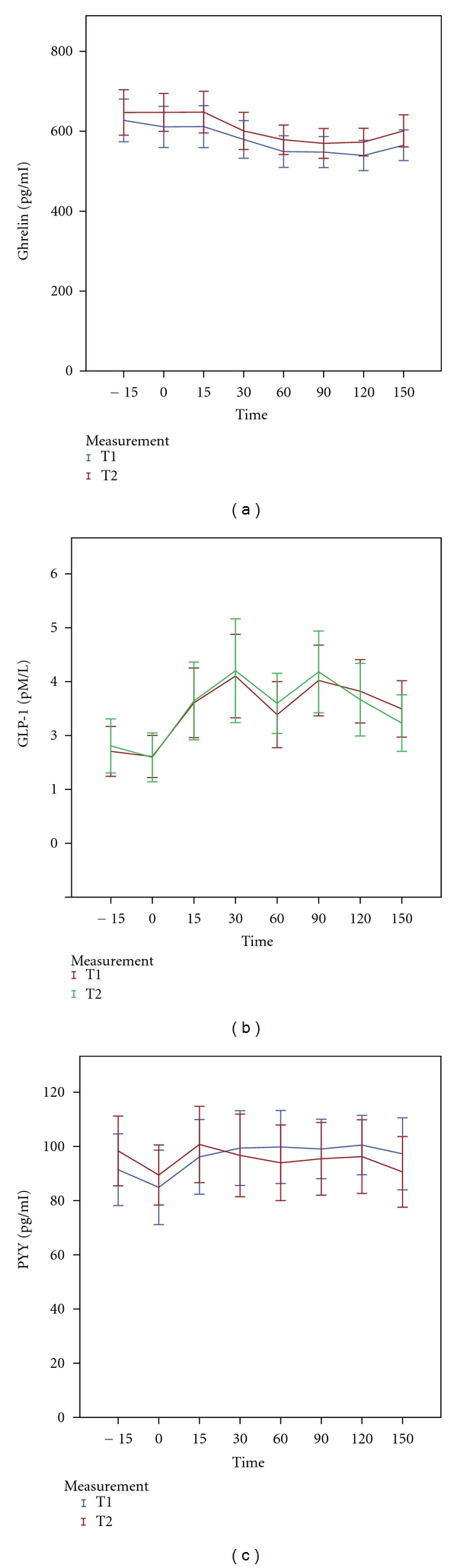
Mean plasma levels (±2SE) of Ghrelin (a), GLP-1 (b), and PYY (c) in response to a mixed meal at baseline (T1) versus after intervention (T2).
The ANCOVA analysis for change of circulating ghrelin and PYY levels between the two study occasions showed that the change in BMI-SDS during the study period was a significant covariate (P < .01 and P = .01, resp.). This finding suggests that weight loss affects the plasma PYY concentration. Gender, age, and pubertal stage were no significant covariates.
4. Discussion
A 3-month multidisciplinary lifestyle intervention in obese children reduces adiposity (BMI-SDS) and elevates plasma ghrelin levels in response to a meal. In contrast, it does not affect circulating PYY and GLP-1 concentrations in fasting condition nor in response to food intake. Notably, changes of ghrelin and PYY AUC were significantly influenced by the change of BMI-SDS, which suggests that the production of these gut peptides is sensitive to body weight (change). We speculate that the impact of our intervention on BMI was too modest to reach statistical significance for the difference between average levels.
Various studies have shown an increase of fasting plasma ghrelin levels after weight loss in obese children [8, 10, 13]. However, the amount of weight lost was substantially greater in these studies than in ours. Other studies in which weight loss was more modest did not observe significant changes of fasting circulating ghrelin levels either [5, 14]. Interestingly, the change of plasma ghrelin concentrations was significantly and inversely associated with the change of BMI-SDS, which confirms that body weight (or caloric restriction) does influence ghrelin levels. This suggests that the effect of our intervention on weight reduction was too small to affect average fasting circulating ghrelin. It has been suggested that weight loss achieved by dietary or exercise treatment initiates compensatory changes in appetite and energy expenditure that hinders maintenance of the reduced body weight [4, 5]. Ghrelin release increases before a meal to initiate food intake [4, 29]. Thus, it is conceivable that higher (fasting) ghrelin concentrations in response to weight loss set off a greater hunger signal, which obviously renders the treatment goal more difficult to reach.
It is unclear why serum ghrelin levels are low in obese children. Perhaps overfeeding is involved (feeding dampens ghrelin release) and the metabolic changes associated with obesity, such as insulin resistance [4]. Indeed, a previous study revealed that the change of HOMA-IR after weight loss correlates inversely with the change in plasma ghrelin in obese children, suggesting that these changes are mechanistically linked [5, 8].
GLP-1 and PYY are gut peptides produced in response to food intake. Both peptides provide a satiety signal to the brain to terminate eating [4]. Fasting plasma concentrations of either peptide were reported to be normal [9, 15–18] or reduced [19, 20] in obese children, whereas postprandial levels are consistently lower [15, 20, 21]. We show that modest weight reduction does not have an impact on fasting or postprandial GLP-1 and PYY levels in obese children. This is in apparent contrast to the results of the very few previous studies evaluating the effect of weight loss on plasma gut hormone levels in children. Substantial weight loss (≥0.5 BMI-SDS) appears to be accompanied by an increase in fasting PYY [19] and (surprisingly) a decrease in (fasting) GLP-1 [15, 18].
It is important to emphasize that our multidisciplinary lifestyle treatment resulted in a statistically significant but only modest weight reduction. It is therefore conceivable that a more substantial average weight reduction of ≥0.5 BMI-SDS would have had more explicit effects on (average) gut hormone concentrations. This postulate is supported by other studies, but also by our own data showing that the amount of weight loss is correlated with counterregulatory changes of plasma ghrelin and PYY concentrations, which can contribute to the difficulties that patients encounter when they try to lose weight. Thus, GLP-1 analogues or dipeptidyl-peptidase IV inhibitors may help obese children to lose weight in response to lifestyle measures.
In conclusion, only a few studies so far have evaluated the effect of weight reduction on (postprandial) PYY, GLP-1, or ghrelin concentrations in children with obesity. We show that modest weight reduction by lifestyle intervention slightly elevates ghrelin levels, whereas it does not affect PYY or GLP-1 concentrations.
Conflict of Interests
The study was partly funded by an unrestricted educational grant by Pfizer and an unrestricted educational grant by a nonprofit foundation (de Stichting Vrienden van het JKZ). The sponsors had no role in the study design, data collection and analysis, nor the content of the paper. The corresponding author has full access to all data in the study. All authors declare no conflict of interests. This research was carried out at the Department of Pediatrics, Juliana Children's Hospital, The Hague, The Netherlands.
Acknowledgments
The authors thank all members of the multidisciplinary team, for their time and patience in treating the children, and the participating children and their families. They also like to thank the members of the short-stay unit and the staff of the Clinical Chemical Laboratory, Juliana Children's Hospital, The Hague, The Netherlands and of the Clinical Chemical Laboratory, Leiden University Medical Centrum, Leiden, The Netherlands, for their assistance in annualizing the blood samples.
References
- 1.Lobstein T, Baur L, Uauy R. Obesity in children and young people: a crisis in public health. Obesity Reviews. 2004;5(supplement 1):4–104. doi: 10.1111/j.1467-789X.2004.00133.x. [DOI] [PubMed] [Google Scholar]
- 2.Murphy KG, Bloom SR. Gut hormones and the regulation of energy homeostasis. Nature. 2006;444(7121):854–859. doi: 10.1038/nature05484. [DOI] [PubMed] [Google Scholar]
- 3.Neary MT, Batterham RL. Gut hormones: implications for the treatment of obesity. Pharmacology and Therapeutics. 2009;124(1):44–56. doi: 10.1016/j.pharmthera.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 4.Roth CL, Reinehr T. Roles of gastrointestinal and adipose tissue peptides in childhood obesity and changes after weight loss due to lifestyle intervention. Archives of Pediatrics and Adolescent Medicine. 2010;164(2):131–138. doi: 10.1001/archpediatrics.2009.265. [DOI] [PubMed] [Google Scholar]
- 5.Reinehr T, Roth CL, Alexy U, Kersting M, Kiess W, Andler W. Ghrelin levels before and after reduction of overweight due to a low-fat high-carbohydrate diet in obese children and adolescents. International Journal of Obesity. 2005;29(4):362–368. doi: 10.1038/sj.ijo.0802913. [DOI] [PubMed] [Google Scholar]
- 6.Bacha F, Arslanian SA. Ghrelin suppression in overweight children: a manifestation of insulin resistance? Journal of Clinical Endocrinology and Metabolism. 2005;90(5):2725–2730. doi: 10.1210/jc.2004-1582. [DOI] [PubMed] [Google Scholar]
- 7.Baldelli R, Bellone S, Castellino N, et al. Oral glucose load inhibits circulating ghrelin levels to the same extent in normal and obese children. Clinical Endocrinology. 2006;64(3):255–259. doi: 10.1111/j.1365-2265.2006.02441.x. [DOI] [PubMed] [Google Scholar]
- 8.Soriano-Guillen L, Barrios V, Campos-Barros A, Argente J. Ghrelin levels in obesity and anorexia nervosa: effect of weight reduction or recuperation. Journal of Pediatrics. 2004;144(1):36–42. doi: 10.1016/j.jpeds.2003.10.036. [DOI] [PubMed] [Google Scholar]
- 9.Stock S, Leichner P, Wong AC, et al. Ghrelin, peptide YY, glucose-dependent insulinotropic polypeptide, and hunger responses to a mixed meal in anorexic, obese, and control female adolescents. Journal of Clinical Endocrinology and Metabolism. 2005;90(4):2161–2168. doi: 10.1210/jc.2004-1251. [DOI] [PubMed] [Google Scholar]
- 10.Zou CC, Liang L, Wang CL, Fu JF, Zhao ZY. The change in ghrelin and obestatin levels in obese children after weight reduction. Acta Paediatrica. 2009;98(1):159–165. doi: 10.1111/j.1651-2227.2008.00997.x. [DOI] [PubMed] [Google Scholar]
- 11.Galli-Tsinopoulou A, Stylianou C, Farmakiotis D, Rousso I, Karamouzis M, Nousia-Arvanitakis S. Ghrelin serum levels during oral glucose tolerance test in prepubertal obese children with insulin resistance. Journal of Pediatric Endocrinology and Metabolism. 2007;20(10):1085–1092. doi: 10.1515/jpem.2007.20.10.1085. [DOI] [PubMed] [Google Scholar]
- 12.Wang XM, Jiang YJ, Liang L, Du LZ. Changes of ghrelin following oral glucose tolerance test in obese children with insulin resistance. World Journal of Gastroenterology. 2008;14(12):1919–1924. doi: 10.3748/wjg.14.1919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krohn K, Boczan C, Otto B, et al. Regulation of ghrelin is related to estimated insulin sensitivity in obese children. International Journal of Obesity. 2006;30(10):1482–1487. doi: 10.1038/sj.ijo.0803399. [DOI] [PubMed] [Google Scholar]
- 14.Carnier J, Lofrano MC, Prado WL, et al. Hormonal alteration in obese adolescents with eating disorder: effects of multidisciplinary therapy. Hormone Research. 2008;70(2):79–84. doi: 10.1159/000139148. [DOI] [PubMed] [Google Scholar]
- 15.Chanoine JP, MacKelvie KJ, Barr SI, Wong AC, Meneilly GS, Elahi DH. GLP-1 and appetite responses to a meal in lean and overweight adolescents following exercise. Obesity. 2008;16(1):202–204. doi: 10.1038/oby.2007.39. [DOI] [PubMed] [Google Scholar]
- 16.Lomenick JP, Melguizo MS, Mitchell SL, Summar ML, Anderson JW. Effects of meals high in carbohydrate, protein, and fat on ghrelin and peptide YY secretion in prepubertal children. Journal of Clinical Endocrinology and Metabolism. 2009;94(11):4463–4471. doi: 10.1210/jc.2009-0949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Misra M, Tsai PM, Mendes N, Miller KK, Klibanski A. Increased carbohydrate induced ghrelin secretion in obese vs. normal-weight adolescent girls. Obesity. 2009;17(9):1689–1695. doi: 10.1038/oby.2009.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reinehr T, de SG, Roth CL. Fasting glucagon-like peptide-1 and its relation to insulin in obese children before and after weight loss. Journal of Pediatric Gastroenterology and Nutrition. 2007;44(5):608–612. doi: 10.1097/MPG.0b013e3180406a24. [DOI] [PubMed] [Google Scholar]
- 19.Roth CL, Enriori PJ, Harz K, Woelfle J, Cowley MA, Reinehr T. Peptide YY is a regulator of energy homeostasis in obese children before and after weight loss. Journal of Clinical Endocrinology and Metabolism. 2005;90(12):6386–6391. doi: 10.1210/jc.2005-1357. [DOI] [PubMed] [Google Scholar]
- 20.Tomasik PJ, Sztefko K, Malek A. GLP-1 as a satiety factor in children with eating disorders. Hormone and Metabolic Research. 2002;34(2):77–80. doi: 10.1055/s-2002-20519. [DOI] [PubMed] [Google Scholar]
- 21.Tomasik PJ, Sztefko K, Starzyk J. Cholecystokinin, glucose dependent insulinotropic peptide and glucagon-like peptide 1 secretion in children with anorexia nervosa and simple obesity. Journal of Pediatric Endocrinology and Metabolism. 2004;17(12):1623–1631. doi: 10.1515/jpem.2004.17.12.1623. [DOI] [PubMed] [Google Scholar]
- 22.Vos RC, Wit JM, Pijl H, Kruyff CC, Houdijk ECAM. The effect of family-based multidisciplinary cognitive behavioral treatment in children with obesity: protocol of a randomized controlled trial. Trials. 2011;12(1):p. 110. doi: 10.1186/1745-6215-12-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vos RC, Wit JM, Pijl H, Houdijk ECAM. Long-term effect of lifestyle intervention on adiposity, metabolic parameters, inflammation and physical fitness in obese children: a randomized controlled trial. doi: 10.1038/nutd.2011.5. Nutrition and Diabetes. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. British Medical Journal. 2000;320(7244):1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Epstein LH, Wing RR, Valoski A. Childhood obesity. Pediatric Clinics of North America. 1985;32(2):363–379. doi: 10.1016/s0031-3955(16)34792-7. [DOI] [PubMed] [Google Scholar]
- 26.Fredriks AM, van Buuren S, Wit JM, Verloove-Vanhorick SP. Body index measurements in 1996–7 compared with 1980. Archives of Disease in Childhood. 2000;82(2):107–112. doi: 10.1136/adc.82.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tanner J. Growth at Adolescence: With a General Consideration of the Effects of Hereditary and Enviromental Factors Upon Growth and Maturation from Birth to Maturity. 2nd edition. Oxford, UK: Blackwell Scientific; 1962. [Google Scholar]
- 28.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 29.Nakazato M, Murakami N, Date Y, et al. A role for ghrelin in the central regulation of feeding. Nature. 2001;409(6817):194–198. doi: 10.1038/35051587. [DOI] [PubMed] [Google Scholar]