Abstract
The importance of immunoproteasomes to antigen presentation has been unclear because animals totally lacking immunoproteasomes have not been previously developed. Here we show that dendritic cells from mice lacking the three immunoproteasome catalytic subunits display defects in presenting multiple major histocompatability (MHC) class I epitopes. During viral infection in vivo, the presentation of a majority of MHC class I epitopes is markedly reduced in immunoproteasome-deficient animals, while presentation of MHC class II peptides is unaffected. By mass spectrometry the repertoire of MHC class I-presented peptides is ~50% different and these differences are sufficient to stimulate robust transplant rejection of wild type cells in mutant mice. These results indicate that immunoproteasomes play a much more important role in antigen presentation than previously thought.
Proteasomes play a vital role in generating peptides for presentation on major histocompatability (MHC) class I molecules1. Each proteasome consists of 14 structural and 6 catalytic subunits (two each of the β1, β2 and β5 subunits)2. In addition to these three catalytic subunits, three alternate catalytic subunits denoted as β1i (LMP2 or Psmb9), β2i (MECL1 or Psmb10), and β5i (LMP7 or Psmb8) are constitutively expressed in a number of hematopoietic cells and are induced in other cell types by interferon-γ (IFN-γ) 2,3. When expressed, these alternate subunits preferentially incorporate into newly assembling complexes to form immunoproteasomes3 and change the catalytic activities of these complexes. Compared to the constitutive proteasomes, immunoproteasomes cleave more rapidly after hydrophobic and basic amino acids and less rapidly after acidic ones4–6. Since peptides with hydrophobic or sometimes basic C-termini preferentially bind to MHC class I molecules7, it has long been hypothesized that immunoproteasomes play a specialized role in creating antigenic peptides. However, knock-out (KO) mice lacking individual immunoproteasome catalytic subunits have relatively modest effects on antigen presentation. For example,β 5i (LMP7) KO mice show a modest (~50%) decrease in MHC class I surface expression8 and decreased or increased efficiency of presenting only a few epitopes, while the majority of immunogenic peptides examined are presented normally8–15. These analyses only examined the presentation of known epitopes and it is unknown whether and how often immunoproteasome-deficient mice present different peptides than wild-type (WT) mice.
To determine whether the modest phenotypes of these mice were due to some contribution from the remaining immunoproteasome catalytic subunits, we created an immunoproteasome triple KO mouse, lacking all the immune-subunits. Because the genes for β1i (Psmb9) and β5i (Psmb8) are so close together on chromosome 17, making the chance of generating a double knock by crossing β5i −/− with β1i −/− mice vanishingly small, we chose to create a novel sequential KO of these two genes. We then bred the β1iβ5i double KO mice to β2i −/− (MECL1 KO) mice to create the immunoproteasome triple KO (TKO) animal. We found that the TKO mice had altered presentation of most of the epitopes we tested, both in vitro and in vivo, and that these changes in antigen presentation were sufficient to case TKO mice to reject WT cells.
Results
Generation of immunoproteasome triple KO mice
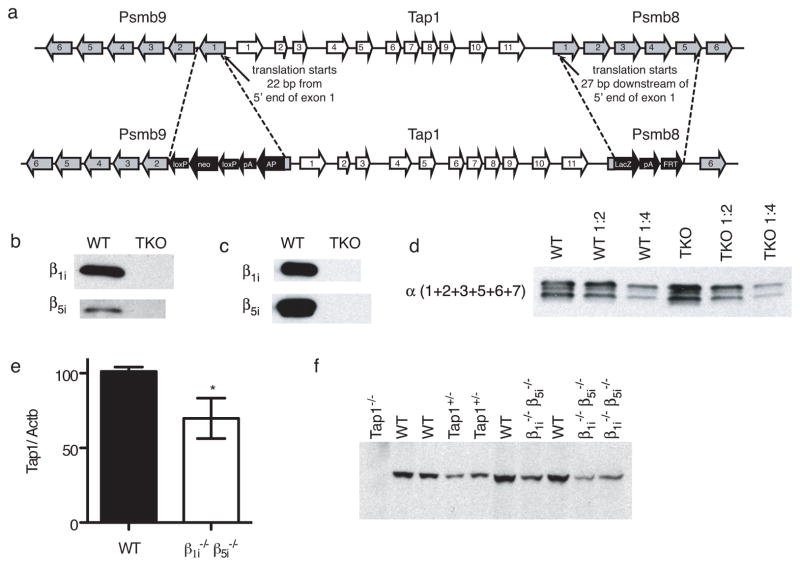
To generate the β1i and β5i double-deficient animals, we designed a sequential KO strategy (Fig. 1a). First a LacZ-FRT-neo-FRT construct was fused in frame to the start codon (27 bp downstream of the 5′ end of exon 1) of Psmb8 (which encodes β5i), removing the remainder of exon 1 plus exons 2 through 5 by homologous recombination. The Neo gene was then removed by FLPe activity in the bacteria. An alkaline phosphatase-loxP-neo-loxP construct was then fused in frame to the start codon (22 bp from the 5′ end of exon 1) of Psmb9 (which encodes β1i, removing the remainder of exon 1 by homologous recombination. The double KO was created on a 129 background, and mice were backcrossed 9 times onto the C57BL/6J background. These mice were then bred to β2i KO16 mice to yield an immunoproteasome triple KO. By the end of this process the resulting animals had been backcrossed 10 generations onto the C57BL/6 background. The progeny of these animals were analyzed for 110 SNPs spanning the genome and were found to be fully backcrossed to C57BL/6.
Fig. 1. β1i and β5i double KO mice.
(a) Exons targeted for the sequential KO of both Psmb9 and Psmb8 to generate double deficient mice. β1i and β5i proteins are not detected in spleen cell lysates (b) or proteasomes purified from splenocytes (c) (equivalent protein loaded in each lane). (d) The amount of proteasomes in WT and TKO spleens is similar, as measured by alpha subunits in serial dilutions of proteasome pellets from equal numbers of spleens. (e) Normalized TAP1 mRNA expression in WT and β5iβ1i double KO splenocytes, determined by RT-qPCR. Bar indicates mean +/− SD of 5 animals for each strain. Asterisk indicates P < 0.05 (Two-tailed, unpaired t-test).(f) Immunoblotting of splenocyte whole cell lysates from the indicated strains, using anti-TAP1 antibody (equivalent protein loaded in each lane).
The β1i and β5i subunits were undetectable by immunoblots in lysates or proteasome preparations from the KO spleens, as expected (Fig. 1b,c). Also as expected the total amount of proteasomes were the same in the TKO and WT spleens as assessed by immunoblotting for an invariant alpha subunit in proteasome preparations (Fig. 1d). We also found that the amount of ubiquitinated proteins were not different between the TKO and WT cells (Supplementary Fig. 1).
Because the Psmb8 and Psmb9 genes flank the transporter 1, ATP-binding cassette, sub-family B (MDR/TAP) gene (Tap1), we evaluated the expression of Tap1 in the β1iβ5i double KO mice to see if it was affected. There was a partial (~50%) reduction in the expression of Tap1 mRNA levels (Fig. 1b) and amount of protein (Fig. 1c). The amount of Tap1 protein expressed in the KOs was similar to that of Tap1 +/− heterozygous mice (Fig. 1c) and therefore the latter mice were used as controls in some experiments.
The TKO mice were viable, fertile and appeared healthy. The overall cellularity of their thymuses and spleens were not different from wild type animals (Supplementary Fig. 2a,b). However, there was a reduction of ~50% in the number of mature CD8 T cells in the immunoproteasome-deficient thymus and spleen (Supplementary Fig. 2c,d), which was similar to what had been observed in β1i single KO mice9. There was no reduction in their number of B cells, which although different from that observed in β1i -deficient mice11,17, was similar to the findings in β1iβ2i -double deficient mice17.
MHC class I expression in TKO mice
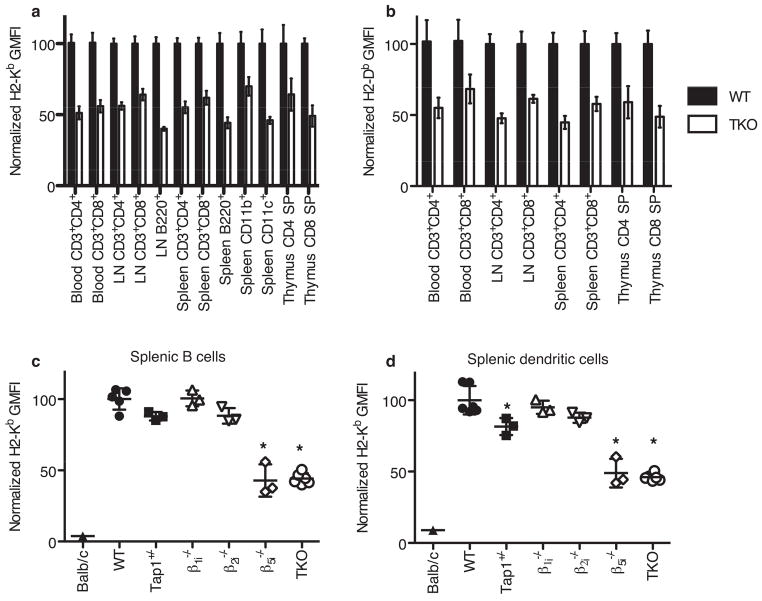
MHC class I molecules must bind peptides in order to be released from the endoplasmic reticulum and traffic to the cell surface18. Consequently, the surface expression of MHC class I molecules are a proxy for the overall supply of peptides for antigen presentation. Therefore, we evaluated the surface expression of MHC class I molecules in the mutant mice by analyzing cells stained with anti-MHC class I molecules by flow cytometry. Cells lacking all three immunoproteasome catalytic subunits had only ~50% of MHC I surface expression compared to WT cells (Fig. 2a,b). Both H2-Kb and H2-Db molecules were similarly affected. There was a decrease in MHC class I surface expression on CD4+ and CD8+ T cells in the blood, spleen, lymph nodes and thymus of TKO mice as well as on lymph node B cells (B220+ cells) and splenic macrophages, dendritic cells (DC) and B cells (CD11b+, CD11c+ and B220+ splenocytes, respectively). These findings were similar to those with cells lacking only β5i, whereas cells lacking β1i or β2i expressed MHC class I molecules at levels more similar to WT cells (Fig. 2c,d), as previously reported8,9,16. We found no defect in MHC class I surface expression in Tap1+/− T or B cells, although we did see a slight decrease in H2-Kb expression in splenic DC. Therefore, the reduction in MHC surface expression on the TKO cells was not due to their modest reduction of Tap1.
Fig. 2. MHC class I surface expression in TKO and immunoproteasome single KO animals.
Blood or organs were harvested from mice of the indicated strains (a) H2-Kb and (b) H2-Db surface expression on cells from WT and TKO mice. In both cases, MHC class I surface expression in TKO mice are significantly reduced compared to WT mice. (Two-way ANOVA, P < 0.0001, n between 3 and 33 depending on the strain and tissue). Bar graphs indicate mean +/− SD. H2-Kb surface expression on splenocytes gated on B220+ (B cells) (c) or CD11c (dendritic cells) (d). Scatter plots indicate individual animals with mean +/− SD indicated. Asterisks indicate a significant difference from WT (P < 0.05, One-way ANOVA followed by Dunnet’s Multiple Comparison Test, n of 3 to 6 for each strain). All results are normalized to the average of WT controls in each experiment.
To assay the relative stability of peptide-MHC I (pMHCI) complexes at the surface of TKO cells, we treated WT and TKO splenocytes with brefeldin A (BFA) for 4 hours, and monitored the MHC class I on the cell surface. We found no evidence of decreased stability of pMHCI (H2-Kb or H2-Db) complexes in TKO animals (Supplementary Fig. 3). The decreased surface expression, therefore, is most likely the result of decreased export of mature pMHCI complexes as opposed to increased degradation of MHC I molecules unstably bound to suboptimal peptides.
Defects in in vitro antigen presentation
Because the surface expression of MHC class I is reduced on a broad range of lymphoid and myeloid cells, we inferred that there were defects in antigen processing that limited the overall supply of peptides to MHC class I molecules. To evaluate antigen presentation more directly, we examined the presentation of a number of well-characterized epitopes by these cells. We used DC for many of these assays because they have been shown to constitutively express the immunoproteasome catalytic subunits19,20.
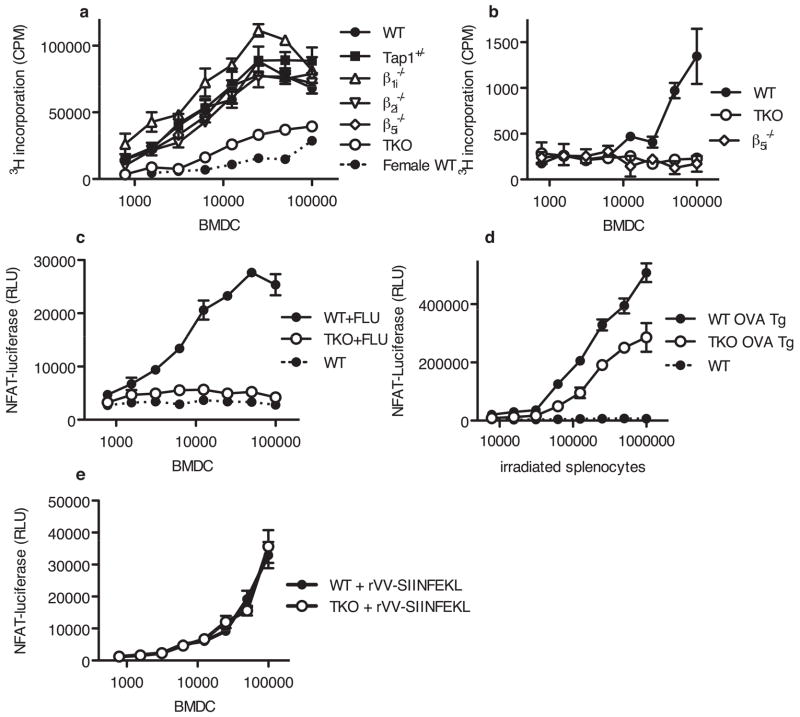
To examine presentation of the male H-Y antigen-derived peptide antigen Smcy 738–746, we measured proliferation of Smcy-specific purified H-Y TCR transgenic T -cells21,22 in response to male C57BL/6 and TKO bone marrow-derived DC (BMDCs). The proliferation of H-Y T-cells cocultured with male (antigen bearing) TKO dendritic cells was extremely low, and was in fact similar to that of H-Y T-cells cocultured with DCs from C57BL/6 females, which lack the Smcy antigen (Fig. 3a). In contrast, the presentation of the Smcy epitope by DCs derived from the three immunoproteasome single KO or Tap1+/− mice was similar to that seen with WT DCs.
Fig. 3. Presentation of H-Y antigens, influenza and OVA by immunoproteasome triple KO dendritic cells is decreased.
(a) BMDC from the indicated mouse strains (male unless otherwise indicated) were serially diluted and combined with 3×104 purified HY CD8+ T cells per well. After 3 d of co-incubation, 3H-Thymidine was added and cells were harvested 5 h later. Representative of 4 experiments. (b) Uty antigen presentation in male BMDC of the indicated strains was assayed using 11p9z hybridoma cells. Secreted IL-2 was measured using the CTLL bioassay. Representative of 3 experiments. (c) After a 4 h influenza infection NP366 antigen presentation by infected WT and TKO BMDC was assayed by co-incubating with 12.64-CD8αβ-LUC hybridoma for 12 h. Relative luciferase units (RLU) are shown. Representative of 4 experiments. (d) SIINFEKL antigen presentation by irradiated splenocytes from WT, OVA transgenic or TKO OVA transgenic animals was assayed using RF33.70-LUC hybridoma cells. Representative of 2 experiments. (e) WT and TKO BMDC were infected with rVV-SIINFEKL and fixed after 2 h. SIINFEKL presentation was assayed using RF33.70-LUC hybridoma cells. Representative of 2 experiments. For panels A through D, responses to TKO cells were significantly different from responses to WT cells (Two-way ANOVA, P < 0.0001). Responses were not significantly different between WT and TKO cells in panel E. Error bars indicate S.D. of triplicate values.
We also measured the presentation of the male antigen Uty 246–254 to the T-T hybridoma 11p9z23,24. TKO DCs also had severely impaired presentation of this epitope (Fig. 3b). Consistent with previously published results13, we found that the β5i single KO also showed defective presentation in this assay.
To further assess potential deficiencies in antigen processing and presentation by TKO cells we employed two other systems. First, we measured presentation of influenza peptide NP366 by influenza-infected BMDC to the 12.64-CD8αβ-LUC hybridoma (a derivative of 12.6425 expressing firefly luciferase under the control of the NFAT promoter) and found that TKO BMDC presented this epitope extremely poorly, especially at early time points (Fig. 3c). Previous reports have found no effect of β2i deficiency or β5i -β2i double deficiency14 on NP366 presentation, but reports have differed as to whether there is an effect of β1i single-deficiency on NP366 presentation (varying from no effect to a partial reduction)9,10,14. Second, we measured presentation of the OVA257–264 epitope (SIINFEKL) by splenocytes from OVA transgenic and TKO OVA trangenic mice to the RF33.70-LUC hybridoma (a derivative of RF33.7026 expressing firefly luciferase under the control of the NFAT promoter), and found that the TKO spleens presented less of this epitope than WT cells (Fig. 3d). In contrast, we found that cells that were infected with recombinant vaccinia (rVV) expressing a minigene that did not require cleavage, presentation of SIINFEKL was not reduced in TKO cells (Fig. 3e). In contrast previous studies have shown that β1i KO9, β5i KO12 and β5i -β2i double KO animals15 present this antigen normally. Overall these analyses revealed that cells lacking immunoproteasomes had a broad defect in antigen presentation that affected all the four epitopes examined.
Decreased presentation of LCMV epitopes in vivo
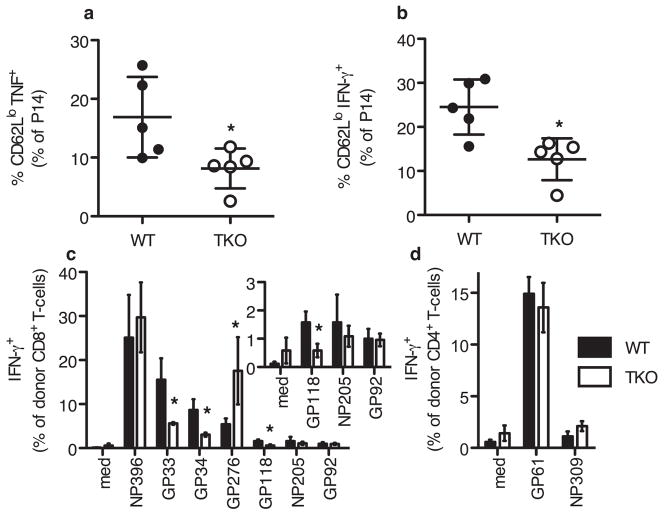
To measure antigen presentation in vivo, we transferred WT P14 TCR transgenic T cells (specific for GP33 viral epitopes) into lymphochoriomeningitis virus (LCMV)-infected WT and TKO mice and assayed their stimulation. Two days after infection with LCMV, WT and TKO mice were injected with naïve BFA-treated P14 lymphocytes (and in addition BFA to maintain the secretion block). Splenocytes were then harvested 4 hours later from these animals, and the production of tumor necrosis factor α (TNFα) and IFN-γ by the P14 cells was detected by intracellular cytokine staining and quantified by flow cytometry. This protocol allowed us to quantify activation of the TCR transgenic T cells by their cognate antigen within the first 4 hr of stimulation by antigen-presenting cells in vivo. Of note, there was no relative loss of the P14 T cells transferred into TKO mice, because the time point we analyzed was much too early for immune-based rejection to occur (an issue discussed below). Both TNFα and IFN-γ production by P14 cells were significantly reduced in TKO mice compared to WT controls (Fig. 4a,b), consistent with decreased presentation of the GP33 epitope in TKO hosts.
Fig. 4. Altered T cell responses in LCMV-infected TKO mice.
(a,b)Two days post LCMV infection, WT and TKO animals were injected with BFA and BFA-treated P14 Tg splenocytes. Spleens were harvested 4 hours later, stained (surface and intracellular) and analyzed by flow cytometry. Representative of 3 experiments. (c,d)To prevent rejection of adoptively transferred cells, host T cells were depleted in WT Thy1.1+Thy1.2+ and TKO Thy1.1+Thy1.2+ mice using anti-Thy1.2. 3×107 LCMV-immune WT Thy1.1 splenocytes were injected i.v. one day before LCMV infection. 5.5 days post-infection, animals were sacrificed and spleens were harvested. Cells analyzed by in vitro restimulation followed by surface and intracellular cytokine staining. Mean and standard deviation of 3 animals of each strain, representative of two experiments. Inset shows low abundance CD8 T-cell responses, enlarged from (c). Asterisk indicated P<0.05, by two-tailed, unpaired t-test.
To evaluate the role of immunoproteasomes in presentation of other LCMV antigens in vivo, we transferred LCMV-immune WT splenocytes into WT and TKO mice and 24 hours later infected the animals with LCMV. To prevent rejection of the adoptively transferred cells, we depleted the host T cells with anti-Thy1.2 antibody, and, as expected, there was no relative loss of the transferred cells in TKO hosts (see below). We then harvested splenocytes from WT and TKO hosts at 5.5 days post infection and quantified the activation of different peptide specific T cells by in vitro re-stimulation and intracellular cytokine staining. CD8 T cell responses to GP33 were reduced, confirming the results obtained with the P14 transgenic T cells, which recognize this peptide. Moreover, responses to most other epitopes in vivo were significantly reduced, consistent with a defect in processing and presentation of a broad array of epitopes in the TKO mice (Fig. 4c). Although it is formally possible that the responses of WT T cells in TKO animals could be affected by host factors, such as regulatory T cells, the decreased responses of the transferred T cells in TKO animals most likely reflect reduced antigen presentation, especially because the host was depleted of T cells. On the other hand it should be noted that since the responding T cells are WT, this experimental design excludes any possible defect in the proliferative responses of immunoproteasome-deficient T cells (although we have not seen any such defects in responses of TKO T cells to antigens, Supplementary Fig. 4, or homeostatic proliferation in two experiments in which these cells were transferred to lymphopenic RAG-deficient hosts, not shown) or in their repertoire.
Responses to three peptides, NP396, GP276 and GP92, were not reduced, and the response to NP205 was reduced, but did not reach the level of statistical significance (Fig. 4c and inset). In the case of the NP396 epitope, it is possible that our assay system could miss a reduction in its presentation if the number of peptide-MHC complexes are in excess of what is needed to maximally stimulate the T cells; this might occur in a viral infection because the NP396 peptide has a very high binding affinity to H2-Db27. The LCMV GP276 epitope, on the other hand, seems to be produced better by the TKO animals. This epitope has been previously shown to be destroyed by β1i in vitro 28, so its increased presentation may reflect decreased destruction of this epitope in TKO APC.
Because responses to GP33 and GP34 were decreased in TKO mice while the responses to NP396 were not significantly different, the immunodominance hierarchy was dramatically altered in the TKO mice. The defects in T cell responses in TKO mice are significantly more widespread than what has been reported in single KO animals. β1i KO11 and β2i KO16 mice have been shown to have decreased CD8 T-cell responses to LCMV GP276 and NP205 but normal responses to NP396, GP33 and several other LCMV epitopes. β5i KO mice were reported to have normal responses to all LCMV peptides11.
We found no defects in CD4 T cell responses to the MHC class II epitopes GP61 and NP309 (Fig. 4d) in these mice, although the NP309 responses were very close to background. We also looked at CD4 T cell responses in unmanipulated WT and TKO mice infected with LCMV and found that the responses to these epitopes were not decreased in TKO mice (Supplementary Fig. 4), and that the NP309 were easier to detect above the background. The normal CD4 T cells responses in LCMV infected TKO mice suggest that neither APC nor T cells are globally affected in these mice, but that the defects are specific to MHC class I antigen presentation.
TKO mice reject WT splenocytes
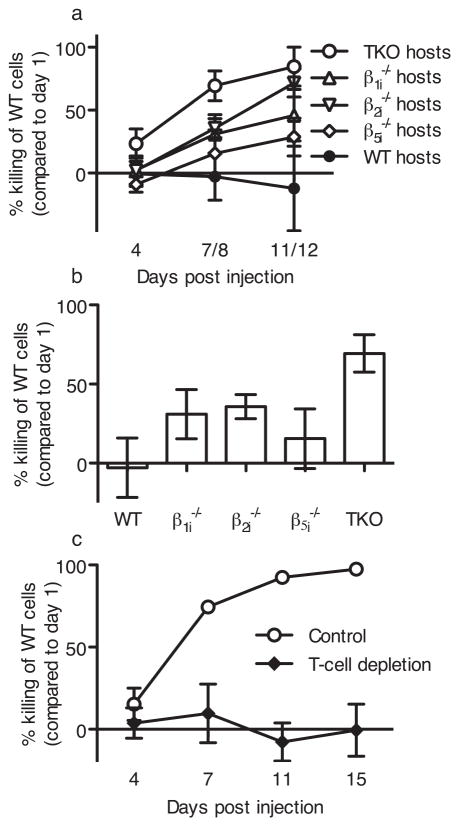
The finding that immunoproteasome-deficient APC have marked differences in the presentation of a majority of tested T cell epitopes raised the possibility that these mutant cells might not just have quantitative difference in antigen presentation but also be generating a different set of peptides than WT cells. If this were the case TKO T cells would not be tolerant to many of the self peptides presented on immunoproteasome-expressing WT cells and would be stimulated to reject these cells. To test this hypothesis, we injected TKO mice with a mixture of carboxyfluorescein diacetate succinimidyl ester (CFSE)-labeled WT and TKO splenocytes and then monitored the proportion of WT to TKO splenocytes in the blood of host animals over 11 to 12 days. On ~day 4 after transfer the WT cells progressively disappeared in TKO hosts and were profoundly depleted by 11 days post injection (Fig. 5a). We also performed these experiments with the 3 single immunoproteasome KO strains, and found that WT cells were also rejected by the single KO animals, albeit with much slower kinetics (Fig. 5a,b). These results suggest that WT splenocytes present a markedly different, repertoire of peptides than those found in either the thymus or periphery of TKO animals, resulting in recognition of this immunoproteasome-derived repertoire as foreign epitopes. Moreover, the data are consistent with a defect in the generation of presented peptides in TKO mice that is substantially greater than in any of the single immunoproteasome subunit-deficient mice. To confirm that the recognition and rejection of the WT cells was CD8 T cell mediated, we depleted host T cells using an anti-Thy1.2 specific antibody. TKO animals whose T cells had been depleted did not reject WT splenocytes (Fig. 5c).
Fig. 5. TKO hosts reject WT splenocytes.
(a) Mice of the indicated strain were injected with WT and KO cells differentially labeled with CFSE. Mice were bled at the indicated times, and the selective killing of WT cells was assessed. Mean ±SD from: TKO, 14 mice, 3 experiments; β1i, 10 mice, 3 experiments; β5i, 5 mice, 1 experiment; β2i, 7 mice, 2 experiments. (b) Killing of WT splenocytes by single and TKO mice at day 7 or 8 (One way ANOVA, with Dunnett’s Multiple Comparison test, asterisk indicates P < 0.05). (c) Similar to (a) except the TKO host T cells were depleted with anti-Thy1.2 antibody (30H12) before injection of WT splenocytes.
In reciprocal experiments we injected a mixture of CFSE-labeled WT and TKO splenocytes into WT mice. In contrast to the results observed in the TKO host, both cell populations survived in WT hosts (Supplementary Fig. 5). This difference between the WT hosts and TKO hosts is not surprising. The TKO host has never seen any of the unique peptides generated by immunoproteasomes and therefore would not be tolerant to them. In contrast, WT mice express constitutive proteasomes and immunoproteasomes, so the animals would be expected to be tolerant to the peptides generated by both types of proteolytic complex.
Changes in MHC I peptide repertoire
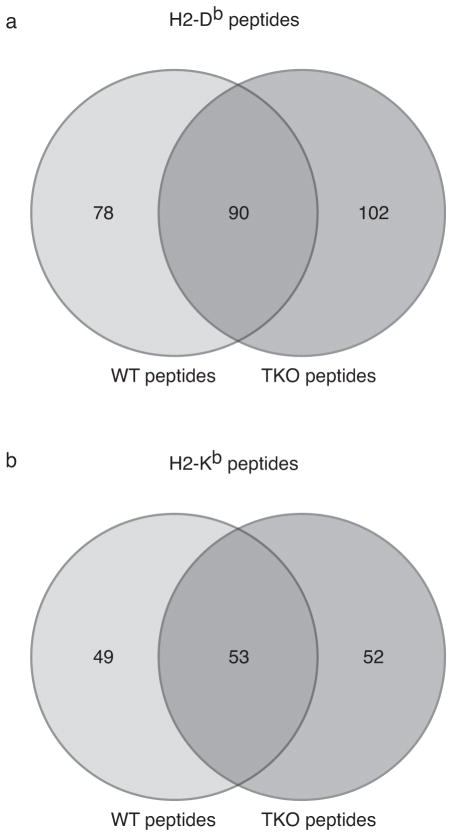
Having found a difference in the peptides presented by WT and TKO splenocytes as measured by immune-based rejection, we wanted to look in more detail at the peptides bound to MHC class I in the two strains. To identify naturally processed peptides, we isolated H2-Kb or H2-Db molecules from splenocytes, eluted the peptides, fractionated them by high pressure liquid chromatography and analyzed the results by mass spectrometry. Because TKO splenocytes present approximately half as much MHC class I on the cell surface as WT splenocytes, we needed to use more TKO spleens to achieve similar yields of peptides from the two strains. In the raw (unvalidated) data from two independent experiments, we identified 398 distinct peptide sequences in the material extracted from WT H2-Kb (81% of which were not found in TKO),. 581 sequences from WT H2-Db (78% not found in TKO), 331 sequences from TKO H2-Kb (77% not found in WT) and 570 sequences from TKO H2-Db (78% not found in WT). This data represents unvalidated masses and based on our previous experience includes a large number of erroneously assigned sequences. Valid peptide sequences were identified with high confidence using an initial search with Spectrum Mill algorithm followed by expert manual spectral validation. We identified a total of 270 WT and 297 TKO validated peptide sequences. While some validated peptides were shared by the two strains, we identified a large proportion of peptides that were found only in one strain (Fig. 6 and Supplementary Tables 1, 2, 3 and 4). Although WT mice can express both the constitutive and immune proteolytic subunits, WT splenocytes express only minor amounts of the constitutive subunits29, so the peptides unique to TKO are presumably the products of constitutive proteasomes. The mass spectrometry technique that we used did not allow us to determine the relative frequency of each peptide in each strain, so our data likely underestimate the differences between the peptide repertoires of the two strains. The results show that despite the transport-selectivity of Tap1 and the binding-selectivity of the MHC I molecules themselves, the differences in the biochemical activities of the proteasome and immunoproteasome subunits results in different peptides bound to MHC class I.
Fig. 6. Distinct peptides presented on WT and TKO splenocytes.
Comparison of peptides identified by tandem mass spectrometry (MS/MS) in WT and TKO animals. pMHCI complexes were isolated with anti H2-Db (a) or anti H2-Kb (b) antibodies. Numbers indicate the number of identified peptides that were unique to WT splenocytes, unique to TKO splenocytes or shared by both.
Discussion
Our results with TKO mice reveal the vital role of immunoproteasomes in creating peptides for MHC class I antigen presentation. The profound defects in antigen presentation that we find in the triple KO APCs, both in vivo and in vitro, are qualitatively and quantitatively much broader than the previously described defects in any of the β1i, β2i or β5i single KO animals and are far greater than the sum of the defects in single knock out animals. The findings suggest that functional overlap between the subunits has masked the true importance of immunoproteasomes.
Of the eleven MHC class I presented antigens we examined, we found clear alterations in nine (i.e. 82%) – eight of which had reduced presentation. In the case of the Smcy antigen, expressed on male cells, there was a significant reduction in presentation by TKO cells even though none of the single KO mice showed a defect. In the case of LCMV GP33 and GP118, there were defects in the response to these epitopes, where none have been previously described with single KO animals11,16. Similarly there was a partial defect in OVA 257–264 presentation not previously seen in single KOs9,12,15 and also a much more marked defect in the presentation of Influenza NP366–3749,10,14. We believe, therefore, that data from single KO animals have substantially underestimated the contribution of the immunoproteasomes to generating peptides for MHC class I antigen presentation.
Our finding that many epitopes are presented poorly by cells that completely lack immunoproteasomes are consistent with inefficient generation of optimal peptides by constitutive proteasomes. Presumably this defect in generating peptides accounts for the approximately 50% decrease in MHC class I surface expression in the TKO mice. Although this decrease in MHC class I is similar to that in β5i single KO animals (our data here and8), the peptides that the two strains present are almost certainly not identical. Compared to β5i.−/− animals, TKO mice present many peptides more poorly and more rapidly reject WT cells. The profound difference in Smcy presentation between β5i KO DCs (which present the antigen normally) and TKO DCs (which present the antigen very poorly) despite the quantitatively similar MHC class I surface expression, suggests that the decreased presentation in the TKO cells cannot be due to the decrease in overall MHC molecules but rather are a result of a poor supply of peptides.
In the absence of immunoproteasomes, there were changes in antigen presentation in vitro in dendritic cells and, importantly, also in vivo. During LCMV infection, we observe changes that affect the magnitude of T cell responses, generally substantially reducing responses. GP276, the one epitope for which we found better presentation by TKO cells, has been previously shown to be destroyed by β1i in vitro 28. The fact that these changes in antigen presentation effect CD8 T cell responses in TKO animals (to the point of altering the immunodominance hierarchy) is impressive in the face of an immunogen as robust as LCMV.
The defects that we observed in vivo selectively affect the MHC class I antigen processing pathway. Loss of immunoproteasomes decreased responses to epitopes from several protein antigens but not from a minigene whose product does not require cleavage for presentation. Moreover, we find no defect in CD4 numbers in response to MHC class II epitopes in vivo, indicating that APC function is not globally decreased. We also conclude that the decreased CD8 T cell responses in TKO mice are not due to pleiotropic effects on T cells, but to antigen presentation defects, since the decreases are found in WT T cells transferred into TKO hosts. Moreover, we also find no defect in CD4 numbers or responses in naïve or LCMV-infected animals.
In addition to the differences we observed in the presentation of 9 of 11 immunogenic epitopes, we found that the peptide repertoire of TKO animals is qualitatively substantially different from WT or any single KO, as evidenced by the robust rejection of WT cells by TKO animals. This is particularly impressive because differences in minor histocompatibility antigens, which are presented peptides that differ between strains due to allelic polymorphisms, stimulate rejection much more slowly. It should be noted that rejection of the WT cells is unlikely to be due to minor histocompatibility differences, because the TKO animals were fully backcrossed. In addition, such histocompatibility differences would be expected to elicit bidirectional responses between the strains, but we found no rejection of TKO cells by WT animals. Instead, this ‘one way’ rejection suggests that cells in WT animals present a substantially different set of peptides than those found in TKO animals, containing epitopes generated by both immunoproteasomes and constitutive ones. Consistent with these results and quite remarkably, comparison of the peptides eluted from matched samples of MHC class I molecules on wild type versus TKO splenocytes revealed that only about one half of the peptides from both Db and Kb were shared between the two strains. This is likely an underestimate because the mass spectrometry analysis detects the presence of abundant peptides but not their precise amount. Therefore, even among the peptides that were in common between the WT and TKO mice there are likely quantitative differences, as we found such differences in the presentation of the majority (82%) of immunogenic epitopes in quantitative assays. When the peptides we identified as unique to immunoproteasome-deficient mice are compared against a larger data set of BL6-presented peptides from the literature, 75–80% are still only present in the TKO pools. The 20–25% of additional ‘shared’ peptides could have been generated by constitutive proteasomes in previous WT preparations and/or by the detection of lower abundance peptides in previous analyses.
Taken together, these results demonstrate the importance of immunoproteasomes in generating peptides for MHC class I antigen presentation, a contribution that has been previously substantially underestimated. A potentially important implication of our findings is that under non-inflammatory conditions the peptides presented by DC, which constitutively express immunoproteasomes, will be substantially different from the ones displayed on parenchymal cells, which contain only constitutive proteasomes. Therefore, T cell responses stimulated by DC may not optimally recognize parenchymal cells until immunoproteasomes are induced in the latter by interferon. This may reduce the effectiveness of CD8 T cell immunity in situations where IFN-γ is not produced. Similarly, this could help pathogenic cells that fail to respond to IFN-γ and/or express immunoproteasomes, such as some tumors or cells infected with viruses that inhibit IFN-γ responses, evade immune responses.
Supplementary Material
Acknowledgments
We thank the following scientists for sharing materials and mouse strains with us: β2i KO mice from Dr. Monaco, University of Cincinnati, Ohio, β1i single KO from Dr. Van Kaer, Vanderbilt University School of Medicine, β5i single KO from Dr. Perreault, University of Montreal, with permission of Dr. Fehling, Institute of Immunology, University Clinics Ulm, Germany, C57BL/6 HY-transgenic mice from B.J. Fowlkes (National Institutes of Health, Bethesda, MD), 11p9z cells from Dr. Nilabh Shastri (University of California, Berkeley), pBMN-IRES-Lyt2a from Dr. Elaine Raines, University of Washington, Seattle, WA, Phoenix cells and plasmids from Michael Green, UMMS, anti-H2-Kb exon 8 antiserum from Drs. Yewdell and Bennick (NIAID, NIH). Freidrich Cruz and Diego Farfan created the RF33.70-LUC and 12.64-CD8alpha/beta-LUC cell lines. Many of the in vivo cytotoxicity experiments were performed by Dushani Palliyaguru. We would like to thank Lawrence Stern and Zu Shen for advice and reagents for optimizing the mass spectrometry. Dr Kenneth Rock is a member of the UMass DERC (DK32520) and this study utilized its core resources.
Footnotes
AUTHOR CONTRIBUTIONS
E.Z.K. designed and performed experiments, analyzed data and wrote the paper; J.W.C. designed and performed LCMV experiments and analyzed data; I.Y. designed the β1iβ5i DKO and did the initial backcrossing; H.E. and E.R.-V. performed peptide isolation and mass spectrometry and analyzed data; J.C.D. oversaw the mass spectrometry experimentsand data analysis,; R.M.W. designed and supervised the LCMV experiments; M.L.K.,A.J.M., D.M.V. and G.D.Y. designed the β1β5i DKO; and K.L.R. designed experiments, supervised the experiments and wrote the paper.
COMPETING FINANCIAL INTERESTS
The authors declare no competing financial interests.
References
- 1.Rock KL, et al. Inhibitors of the proteasome block the degradation of most cell proteins and the generation of peptides presented on MHC class I molecules. Cell. 1994;78:761–771. doi: 10.1016/s0092-8674(94)90462-6. [DOI] [PubMed] [Google Scholar]
- 2.Coux O, Tanaka K, Goldberg AL. Structure and functions of the 20S and 26S proteasomes. Annu Rev Biochem. 1996;65:801–847. doi: 10.1146/annurev.bi.65.070196.004101. [DOI] [PubMed] [Google Scholar]
- 3.Tanaka K. Role of proteasomes modified by interferon-gamma in antigen processing. J Leukoc Biol. 1994;56:571–575. doi: 10.1002/jlb.56.5.571. [DOI] [PubMed] [Google Scholar]
- 4.Gaczynska M, Rock KL, Goldberg AL. Gamma-interferon and expression of MHC genes regulate peptide hydrolysis by proteasomes. Nature. 1993;365:264–267. doi: 10.1038/365264a0. [DOI] [PubMed] [Google Scholar]
- 5.Driscoll J, Brown MG, Finley D, Monaco JJ. MHC-linked LMP gene products specifically alter peptidase activities of the proteasome. Nature. 1993;365:262–264. doi: 10.1038/365262a0. [DOI] [PubMed] [Google Scholar]
- 6.Aki M, et al. Interferon-gamma induces different subunit organizations and functional diversity of proteasomes. J Biochem. 1994;115:257–269. doi: 10.1093/oxfordjournals.jbchem.a124327. [DOI] [PubMed] [Google Scholar]
- 7.Rammensee HG, Falk K, Rötzschke O. Peptides naturally presented by MHC class I molecules. Annu Rev Immunol. 1993;11:213–244. doi: 10.1146/annurev.iy.11.040193.001241. [DOI] [PubMed] [Google Scholar]
- 8.Fehling HJ, et al. MHC class I expression in mice lacking the proteasome subunit LMP-7. Science. 1994;265:1234–1237. doi: 10.1126/science.8066463. [DOI] [PubMed] [Google Scholar]
- 9.Van Kaer L, et al. Altered peptidase and viral-specific T cell response in LMP2 mutant mice. Immunity. 1994;1:533–541. doi: 10.1016/1074-7613(94)90043-4. [DOI] [PubMed] [Google Scholar]
- 10.Chen W, Norbury CC, Cho Y, Yewdell JW, Bennink JR. Immunoproteasomes shape immunodominance hierarchies of antiviral CD8(+) T cells at the levels of T cell repertoire and presentation of viral antigens. J Exp Med. 2001;193:1319–1326. doi: 10.1084/jem.193.11.1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nussbaum AK, Rodriguez-Carreno MP, Benning N, Botten J, Whitton JL. Immunoproteasome-deficient mice mount largely normal CD8+ T cell responses to lymphocytic choriomeningitis virus infection and DNA vaccination. J Immunol. 2005;175:1153–1160. doi: 10.4049/jimmunol.175.2.1153. [DOI] [PubMed] [Google Scholar]
- 12.Osterloh P, et al. Proteasomes shape the repertoire of T cells participating in antigen-specific immune responses. Proc Natl Acad Sci USA. 2006;103:5042–5047. doi: 10.1073/pnas.0509256103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Palmowski MJ, et al. Role of immunoproteasomes in cross-presentation. J Immunol. 2006;177:983–990. doi: 10.4049/jimmunol.177.2.983. [DOI] [PubMed] [Google Scholar]
- 14.Pang KC, et al. Immunoproteasome subunit deficiencies impact differentially on two immunodominant influenza virus-specific CD8+ T cell responses. J Immunol. 2006;177:7680–7688. doi: 10.4049/jimmunol.177.11.7680. [DOI] [PubMed] [Google Scholar]
- 15.Deol P, Zaiss DMW, Monaco JJ, Sijts AJAM. Rates of processing determine the immunogenicity of immunoproteasome-generated epitopes. J Immunol. 2007;178:7557–7562. doi: 10.4049/jimmunol.178.12.7557. [DOI] [PubMed] [Google Scholar]
- 16.Basler M, Moebius J, Elenich L, Groettrup M, Monaco JJ. An altered T cell repertoire in MECL-1-deficient mice. J Immunol. 2006;176:6665–6672. doi: 10.4049/jimmunol.176.11.6665. [DOI] [PubMed] [Google Scholar]
- 17.Hensley SE, et al. Unexpected role for the immunoproteasome subunit LMP2 in antiviral humoral and innate immune responses. J Immunol. 2010;184:4115–4122. doi: 10.4049/jimmunol.0903003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Kaer L. Accessory proteins that control the assembly of MHC molecules with peptides. Immunol Res. 2001;23:205–214. doi: 10.1385/IR:23:2-3:205. [DOI] [PubMed] [Google Scholar]
- 19.Macagno A, Kuehn L, de Giuli R, Groettrup M. Pronounced up-regulation of the PA28alpha/beta proteasome regulator but little increase in the steady-state content of immunoproteasome during dendritic cell maturation. Eur J Immunol. 2001;31:3271–3280. doi: 10.1002/1521-4141(200111)31:11<3271::aid-immu3271>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 20.Nil A, Firat E, Sobek V, Eichmann K, Niedermann G. Expression of housekeeping and immunoproteasome subunit genes is differentially regulated in positively and negatively selecting thymic stroma subsets. Eur J Immunol. 2004;34:2681–2689. doi: 10.1002/eji.200425032. [DOI] [PubMed] [Google Scholar]
- 21.Kisielow P, Blüthmann H, Staerz UD, Steinmetz M, von Boehmer H. Tolerance in T-cell-receptor transgenic mice involves deletion of nonmature CD4+8+ thymocytes. Nature. 1988;333:742–746. doi: 10.1038/333742a0. [DOI] [PubMed] [Google Scholar]
- 22.Markiewicz MA, et al. Long-term T cell memory requires the surface expression of self-peptide/major histocompatibility complex molecules. Proc Natl Acad Sci USA. 1998;95:3065–3070. doi: 10.1073/pnas.95.6.3065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sanderson S, Shastri N. LacZ inducible, antigen/MHC-specific T cell hybrids. Int Immunol. 1994;6:369–376. doi: 10.1093/intimm/6.3.369. [DOI] [PubMed] [Google Scholar]
- 24.Greenfield A, et al. An H-YDb epitope is encoded by a novel mouse Y chromosome gene. Nat Genet. 1996;14:474–478. doi: 10.1038/ng1296-474. [DOI] [PubMed] [Google Scholar]
- 25.Deckhut AM, et al. Prominent usage of V beta 8.3 T cells in the H-2Db-restricted response to an influenza A virus nucleoprotein epitope. J Immunol. 1993;151:2658–2666. [PubMed] [Google Scholar]
- 26.Rock KL, Rothstein L, Gamble S. Generation of class I MHC-restricted T-T hybridomas. J Immunol. 1990;145:804–811. [PubMed] [Google Scholar]
- 27.Gairin JE, Mazarguil H, Hudrisier D, Oldstone MB. Optimal lymphocytic choriomeningitis virus sequences restricted by H-2Db major histocompatibility complex class I molecules and presented to cytotoxic T lymphocytes. J Virol. 1995;69:2297–2305. doi: 10.1128/jvi.69.4.2297-2305.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Basler M, Youhnovski N, Van Den Broek M, Przybylski M, Groettrup M. Immunoproteasomes down-regulate presentation of a subdominant T cell epitope from lymphocytic choriomeningitis virus. J Immunol. 2004;173:3925–3934. doi: 10.4049/jimmunol.173.6.3925. [DOI] [PubMed] [Google Scholar]
- 29.Stohwasser R, Standera S, Peters I, Kloetzel PM, Groettrup M. Molecular cloning of the mouse proteasome subunits MC14 and MECL-1: reciprocally regulated tissue expression of interferon-gamma-modulated proteasome subunits. Eur J Immunol. 1997;27:1182–1187. doi: 10.1002/eji.1830270520. [DOI] [PubMed] [Google Scholar]
- 30.Welsh RM, Jr, Lampert PW, Burner PA, Oldstone MB. Antibody-complement interactions with purified lymphocytic choriomeningitis virus. Virology. 1976;73:59–71. doi: 10.1016/0042-6822(76)90060-x. [DOI] [PubMed] [Google Scholar]
- 31.Clipstone NA, Crabtree GR. Identification of calcineurin as a key signalling enzyme in T-lymphocyte activation. Nature. 1992;357:695–697. doi: 10.1038/357695a0. [DOI] [PubMed] [Google Scholar]
- 32.Levkau B, et al. xIAP induces cell-cycle arrest and activates nuclear factor-kappaB: new survival pathways disabled by caspase-mediated cleavage during apoptosis of human endothelial cells. Circ Res. 2001;88:282–290. doi: 10.1161/01.res.88.3.282. [DOI] [PubMed] [Google Scholar]
- 33.Gillis S, Smith KA. Long term culture of tumour-specific cytotoxic T cells. Nature. 1977;268:154–156. doi: 10.1038/268154a0. [DOI] [PubMed] [Google Scholar]
- 34.Sigal LJ, Rock KL. Bone marrow-derived antigen-presenting cells are required for the generation of cytotoxic T lymphocyte responses to viruses and use transporter associated with antigen presentation (TAP)-dependent and -independent pathways of antigen presentation. J Exp Med. 2000;192:1143–1150. doi: 10.1084/jem.192.8.1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oh S, McCaffery JM, Eichelberger MC. Dose-dependent changes in influenza virus-infected dendritic cells result in increased allogeneic T-cell proliferation at low, but not high, doses of virus. J Virol. 2000;74:5460–5469. doi: 10.1128/jvi.74.12.5460-5469.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hilton CJ, Dahl AM, Rock KL. Anti-peptide antibody blocks peptide binding to MHC class I molecules in the endoplasmic reticulum. J Immunol. 2001;166:3952–3956. doi: 10.4049/jimmunol.166.6.3952. [DOI] [PubMed] [Google Scholar]
- 37.Brehm MA, et al. T cell immunodominance and maintenance of memory regulated by unexpectedly cross-reactive pathogens. Nat Immunol. 2002;3:627–634. doi: 10.1038/ni806. [DOI] [PubMed] [Google Scholar]
- 38.Liu F, Whitton JL. Cutting edge: re-evaluating the in vivo cytokine responses of CD8+ T cells during primary and secondary viral infections. J Immunol. 2005;174:5936–5940. doi: 10.4049/jimmunol.174.10.5936. [DOI] [PubMed] [Google Scholar]
- 39.Priyadharshini B, Welsh RM, Greiner DL, Gerstein RM, Brehm MA. Maturation-dependent licensing of naive T cells for rapid TNF production. PLoS ONE. 2010;5:e15038. doi: 10.1371/journal.pone.0015038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Delgado JC, Escobar H, Crockett DK, Reyes-Vargas E, Jensen PE. Identification of naturally processed ligands in the C57BL/6 mouse using large-scale mass spectrometric peptide sequencing and bioinformatics prediction. Immunogenetics. 2009;61:241–246. doi: 10.1007/s00251-009-0360-4. [DOI] [PubMed] [Google Scholar]
- 41.Escobar H, Reyes-Vargas E, Jensen PE, Delgado JC, Crockett DK. Utility of characteristic QTOF MS/MS fragmentation for MHC class I peptides. J Proteome Res. 2011;10:2494–2507. doi: 10.1021/pr101272k. [DOI] [PubMed] [Google Scholar]
- 42.Smith MH, Parker JM, Hodges RS, Barber BH. The preparation and characterization of anti-peptide heteroantisera recognizing subregions of the intracytoplasmic domain of class I H-2 antigens. Mol Immunol. 1986;23:1077–1092. doi: 10.1016/0161-5890(86)90006-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.