Abstract
Purpose
The purpose of this study is to assess the utility of inferior orbital septum release compared to lateral canthotomy and inferior cantholysis for the treatment of orbital compartment syndrome.
Method
An experimental study design employing a cadaver model for orbital compartment syndrome was used to compare the efficacy of inferior orbital septum release versus lateral canthotomy and inferior cantholysis. Elevated orbital compartment pressures were created in a total of ten orbits of five fresh cadaver heads. Compartment pressure and intraocular pressure were measured before and after inferior orbital septum release and lateral canthotomy/cantholysis. Additionally, orbital compartment pressure was compared to intraocular pressure at various pressures to assess correlation. Statistical analysis was performed on the collected data for efficacy comparison of the two procedures.
Results
Both procedures were found to significantly lower orbital compartment pressure. Lateral canthotomy and cantholysis was found to lower the pressure by an average of 56 mmHg as compared to inferior septal release that resulted in an average of 52 mmHg reduction. Performing lateral canthotomy and cantholysis first followed by inferior septal release resulted in a total pressure reduction of 73 mmHg; whereas, reversing the order resulted in a reduction of 77 mmHg. Both the first and second step, regardless of the order of procedure, were found to result in a significant pressure reduction (p = 0.009 and 0.004 respectively).
Comparison of a series of data points collected during the induction of the experimental compartment syndrome revealed a statistically significant correlation between orbital compartment pressure and intraocular pressure (Spearman’s correlation of 0.978 and p-value less than 0.001).
Discussion
The study demonstrates that both lateral canthotomy/cantholysis and inferior orbital septum release are equally effective at reducing orbital compartment pressure. Additionally, the data supports an additive, synergistic reduction in compartment pressure when the procedures are performed consecutively. The correlation of orbital compartment pressure to intraocular pressure proves that intraocular pressure can be used as a reliable measurement of orbital pressure during acute changes in orbital mass. The results of this study demonstrate that the use of inferior orbital septum release in conjunction with lateral canthotomy and cantholysis is superior to the gold standard of isolated lateral canthotomy and cantholysis. Hopefully, the implementation of orbital septum release will result in superior visual outcomes.
Introduction
Orbital compartment syndrome is one of the few ocular emergencies requiring immediate intervention to prevent vision loss and possible blindness. The most common etiologies causing an acute rise in orbital pressure include orbital cellulitis and retrobulbar hemorrhage from trauma, surgery, and retrobulbar anesthesia.1 The orbit is a closed, rigid structure with limited space for expansion of orbital contents. Increasing mass can therefore lead to dramatic pressure elevations and permanent vision loss in as little as 30 minutes. As perfusion pressure in the posterior ciliary arteries and central retinal artery is overwhelmed, anterior ischemic optic neuropathy and central artery occlusion can ensue.2,3,4
Decompression of the orbit with emergent lateral canthotomy and inferior cantholysis is the most commonly performed procedure and can be sight saving. The procedure decreases the resistance to the anterior displacement of orbital contents including the globe and consequently decreases orbital pressure.5–8 However, the anterior displacement of the globe may increase the tension on the optic nerve in an already proptotic eye. We theorize that inferior orbital septum release will work as well as lateral canthotomy and cantholysis but utilize a different mechanism: Allowing herniation of orbital contents around the globe. The purpose of this study is to assess the utility of inferior orbital septum release compared to lateral canthotomy and inferior cantholysis for the treatment of orbital compartment syndrome.
Method
An experimental cadaver model similar to that described by Zoumalan et al was utilized.5 Fresh frozen cadaver orbits were utilized with artificially simulated orbital compartment syndrome to compare the efficacy of lateral canthotomy and inferior cantholysis versus inferior orbital septum release in the treatment of elevated orbital pressure. Interventions were performed on ten orbits from five cadavers. The vitreous cavity of each globe was injected with normal saline to return the intraocular pressure to physiologic levels (approximately 15 mmHg). A viscous mixture of glycerin and hydroxyethyl cellulose (KY Jelly®, McNeil-PPC) was injected stepwise into the orbital compartment to simulate a compartment syndrome (Figure 1a). This mixture was chosen secondary to its ability to remain isolated to the orbit and avoid diffusion into surrounding tissues. Attempts to use normal saline and whole blood led to rapid diffusion of the substances out of the orbit and therefore led to immediate loss of orbital pressure.
Figure 1.
a) Cadaver setup with compartment pressure monitor probe (green) in the superotemporal orbit and 20-gauge needle in the superonasal orbit with attached syringe for injecting viscous mixture of glycerin and hydroxyethyl cellulose.
b) Performance of inferior orbital septum release after induction of artificial compartment syndrome.
After creating an elevated compartment pressure, orbits underwent both lateral canthotomy/cantholysis and inferior orbital septum release. Five eyes received canthotomy/cantholysis first, followed by orbital septum release. One orbit was excluded from data analysis in this group secondary to a visibly incompetent orbital septum on dissection that resulted in spurious data. In the other five eyes, orbital septum release was the first procedure performed.
The lateral canthotomy and cantholysis was performed using the standard technique referenced in numerous articles.1,5,6,7 The inferior septal release was performed by creating a sub-ciliary skin incision using a Bard-Parker fifteen blade. Alternatively in an emergency setting, sharp dissection with the same scissors used to create the lateral canthotomy and cantholysis could be utilized. Sharp dissection using curved tenotomy scissors in a sub-orbicularis plain was performed to the inferior orbital rim to expose the entire inferior septum. The septum was than transected using the tenotomy scissors. (Figure 1b)
Orbital compartment pressures and intraocular pressures were obtained prior to induction of compartment syndrome, with rising orbital volume, at maximal volume/pressure, and immediately following each procedure. Intraocular pressure measurements were obtained with a Medtronic Tono-Pen® at each volume filling increment. Simultaneous orbital compartment pressures were obtained with a Synthes Compartment Pressure Monitor.9 The probe for the compartment pressure monitor was introduced into the superior lateral orbit through a large bore needle to a depth of two centimeters. The needle was then removed leaving the probe within the orbital compartment. (Figure 1A) The monitor was connected to the probe and provided a digital read out of orbital pressures in millimeters of mercury. Data was compiled in an Excel spreadsheet.
Results
Both lateral canthotomy and cantholysis and inferior orbital septum release were found to significantly lower orbital compartment pressure. Lateral canthotomy and cantholysis was found to lower the pressure by an average of 56 mmHg (Table 1) as compared to inferior orbital septum release that resulted in an average of 52 mmHg reduction (Table 2). Performing lateral canthotomy and cantholysis first followed by inferior septal release resulted in a total pressure reduction of 73 mmHg; whereas, reversing the order resulted in a reduction of 77 mmHg (Table 1, 2). Performing both procedures sequentially was also found to result in a statistically significant reduction in pressure but the difference between the two groups after each step was not significant. Wilcoxon signed-rank test was used to compare the pressure before and after the procedure. The results indicated that there was a significant pressure reduction after the first procedure and after the second procedure (p = 0.009 and p = 0.004). Linear models were performed with the robust standard errors. The pressure reduction after the first step was 53.78 mmHg (95% CI: 48.07 – 59.49) and after the second step was 20.78 mmHg (95% CI: 15.07–26.49).
Table 1.
Data for orbits where lateral canthotomy and cantholysis was performed first. All pressure measurements are in millimeters of mercury.
| Eye/Orbit # | Initial Compartment Pressure |
Compartment Pressure after Canthotomy/Cantholysis |
Compartment Pressure after Inferior Septotomy |
|---|---|---|---|
| 1 | 104 | 43 | 31 |
| 2 | 104 | 60 | 47 |
| 3 | 110 | 60 | 35 |
| 4 | 106 | 12 | NA* |
| 5 | 109 | 40 | 25 |
|
Average Reduction by Canthotomy/Cantholysis |
Average Reduction by Both Procedures |
||
| 56 mmHg | 72.8 mmHg |
Insufficient orbital septum- Removed from analysis
Table 2.
Data for orbits where inferior septum release was performed first. All pressure measurements are in millimeters of mercury.
| Eye/Orbit # | Initial Compartment Pressure |
Compartment Pressure after Inferior Septotomy |
Compartment Pressure after Canthotomy/Cantholysis |
|---|---|---|---|
| 1 | 100 | 50 | 21 |
| 2 | 110 | 60 | 30 |
| 3 | 112 | 59 | 33 |
| 4 | 123 | 58 | 40 |
| 5 | 97 | 55 | 36 |
|
Average Reduction by Inferior Septotomy |
Average Reduction by Both Procedures |
||
| 52 mmHg | 76.4 mmHg |
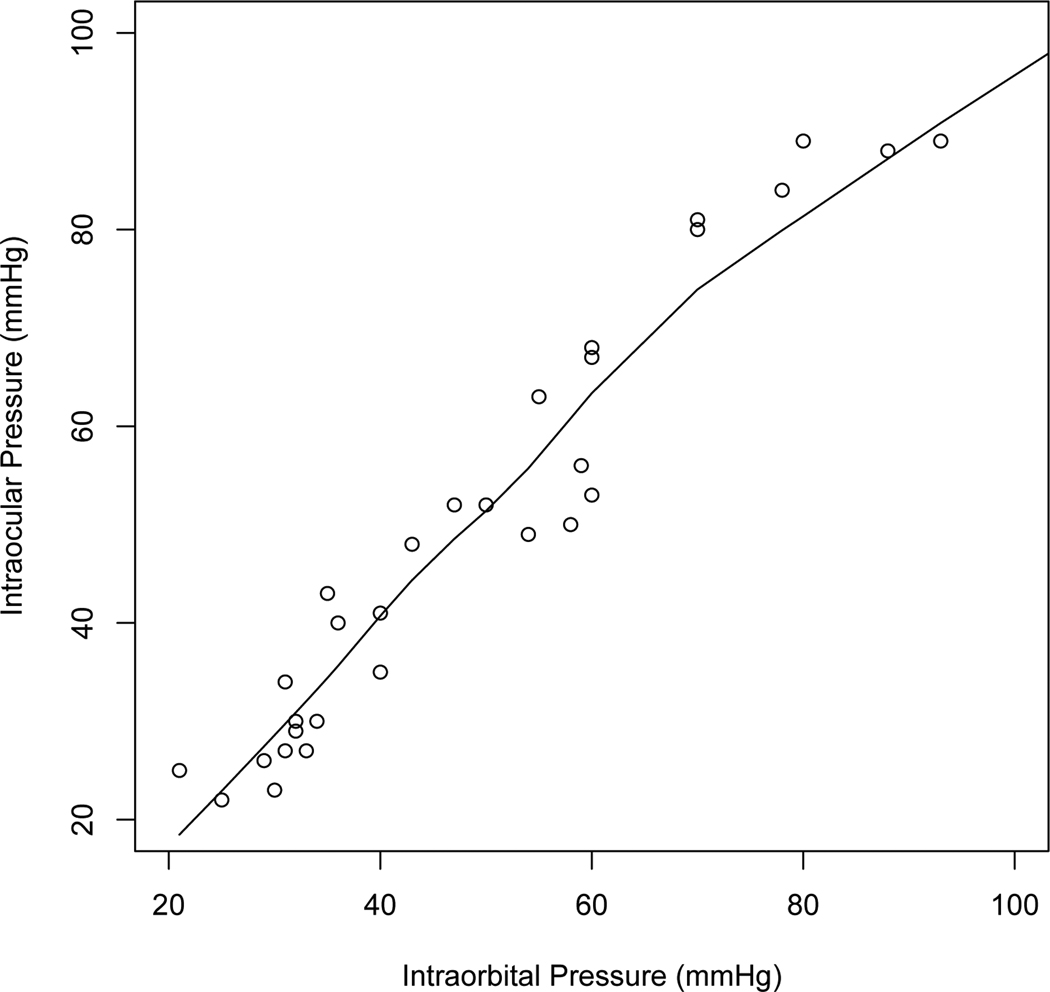
Comparison of a series of data points collected during the induction and treatment of the experimental compartment syndrome revealed a statistically significant correlation between orbital compartment pressure and intraocular pressure. The Spearman’s correlation between intraocular pressure and the intraorbital pressure was 0.978 with p-value less than 0.001, indicating that these two pressures are highly correlated (Figure 2).
Figure 2.
Plot of Intraocular pressure versus Intraorbital pressure
Discussion
Orbital compartment syndrome is a potentially vision threatening condition. Upon diagnosis, treatment should be executed immediately. Treatment has historically included medical and surgical management, but urgent surgical decompression of the orbit is the most accepted approach. The gold standard treatment is lateral canthotomy and inferior cantholysis when there is no previous surgical wound to explore.5,6,7 Several authors support extension of this procedure to include superior cantholysis and, if needed, inferolateral anterior orbitotomy if pressure doesn’t decrease to a safe level.8 Others advocate decompression by removal of orbital bone, but this is invasive, time consuming, and requires an operating room.10–11
Several previous reports had proven the efficacy of lateral canthotomy and cantholysis in reducing intraocular pressure and orbital pressure.5–8 Zoulaman et al had additionally presented a limited form of septal release laterally through the canthotomy; however, to our knowledge no previous paper has evaluated the effectiveness of total septal release to lower intraocular pressure and comparison of that procedure to lateral canthotomy and cantholysis. This study shows that inferior orbital septum release, which can be performed at bedside, compares favorably to the current gold standard. Performing a release of the inferior orbital septum lowered orbital pressure by an average of 52 mmHg (48% reduction) in our study. This proved to be equally efficacious to the gold standard of lateral canthotomy and cantholysis, which lowered orbital pressure by an average of 56 mmHg (52% reduction). When both procedures are done sequentially, regardless of order, the orbital compartment pressure was lowered by an average of 74.6 mmHg (70% reduction). The order of procedure did not change the pressure reduction but performing the lateral canthotomy and cantholysis first creates a smaller skin incision and the second procedure may not be necessary if pressure normalizes. Indeed, there are clinical situations in which performing these two procedures sequentially is merited and this study shows the additive effects of performing both. Importantly, both procedures are efficient in an emergent situation and neither requires significant technical skill to perform. Inferior orbital septum release can be performed in as little as 15 seconds, avoids damaging important structures, and is easily repaired after resolution of the compartment syndrome.
Hopefully this data will support the use of inferior orbital septum release as an additional procedure in the physician’s armamentarium for the treatment of orbital compartment syndrome. We believe that superior orbital septum release may also be efficacious and future studies will examine this procedure’s utility in the treatment of orbital compartment syndrome.
Of further interest, intraocular pressure measurements utilizing the Tono-pen® were found to correlate well with the intraorbital pressure in our study (p-value less than 0.001). Thus, while managing an orbital compartment syndrome, the treating ophthalmologist or emergency department physician can assume that the Tono-pen® measurements are accurate estimates of actual orbital pressure.
Table 3.
Statistical analysis of procedures
| Pressure reduction | Canthotomy/Inferior Septum Release (N=5) |
Inferior Septum Release/Canthotomy (N=5) |
|---|---|---|
| After 1st procedure | 48.5 55.5 63.0 (56.0±11.2) | 50.0 50.0 53.0 (52.0±8.3) |
| After 2nd procedure | 12.8 14.0 17.5 (16.2±6.0) | 19.0 26.0 29.0 (24.4±5.6) |
| Total | 69.0 74.0 77.2 (72.2±11.2) | 79.0 79.0 80.0 (76.4±8.8) |
a b c represent the lower quartile a, the median b, and the upper quartile c for continuous variables. x±s represents x±1SD.
Acknowledgments
Financial Support:
Unrestricted Grant from Research to Prevent Blindness to the Hamilton Eye Institute
In-Kind Grant from the Medical Education and Research Institute (MERI) Memphis, TN
Supported in part by the Vanderbilt CTSA grant UL1 RR024975 from NCRR/NIH
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Poster Presentation
1) 2010 ASOPRS Annual Scientific Symposium, October 2010, Chicago, IL
Proprietary interest statement: The authors of this submission have no disclosures
References
- 1.Lima V, Burt B, Leibovitch I, et al. Orbital compartment syndrome: the ophthalmic surgical emergency. Surv Ophthalmol. 2009 Jul–Aug;54(4):441–449. doi: 10.1016/j.survophthal.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 2.Hayreh SS, Jonas JB. Optic disk and retinal nerve fiber layer damage after transient central retinal artery occlusion: an experimental study in rhesus monkeys. Am J Ophthalmol. 2000;129(6):786–795. doi: 10.1016/s0002-9394(00)00384-6. [DOI] [PubMed] [Google Scholar]
- 3.Dolman PJ, Glazer LC, Harris GJ, et al. Mechanisms of visual loss in severe proptosis. Ophthal Plast Reconstr Surg. 1991;7:256–260. doi: 10.1097/00002341-199112000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Hargaden M, Goldberg SH, Cunningham D, et al. Optic neuropathy following simulation of orbital hemorrhage in the nonhuman primate. Ophthal Plast Reconstr Surg. 1996;12(4):264–272. doi: 10.1097/00002341-199612000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Zoumalan CI, Bullock JD, Warwar RE, et al. Evaluation of intraocular and orbital pressure in the management of orbital hemorrhage: An experimental model. Arch Ophthalmol. 2008;126:1257–1260. doi: 10.1001/archopht.126.9.1257. [DOI] [PubMed] [Google Scholar]
- 6.Yung C, Moorthy RS, Lindley D, et al. Efficacy of lateral canthotomy and cantholysis in orbital hemorrhage. Ophthal Plast Reconstr Surg. 1994;10:137–141. doi: 10.1097/00002341-199406000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Goodall KL, Brahma A, Bates A, Leatherbarrow B. Lateral canthotomy and inferior cantholysis: an effective method of urgent orbital decompression for sight threatening acute retrobulbar haemorrhage. Injury. 1999;30(7):485–490. doi: 10.1016/s0020-1383(99)00137-0. [DOI] [PubMed] [Google Scholar]
- 8.Burkat CN, Lemke BN. Retrobulbar hemorrhage: Inferolateral anterior orbitotomy for emergent management. Arch Ophthalmol. 2005;123(9):1260–1262. doi: 10.1001/archopht.123.9.1260. [DOI] [PubMed] [Google Scholar]
- 9.Kratky V, Hurwitz JJ, Avram DR. Orbital compartment syndrome. Direct measurement of orbital tissue pressure: 1. Technique. Can J Ophthalmol. 1990;25:293–297. [PubMed] [Google Scholar]
- 10.McCartney DL, Char DH. Return of vision following orbital decompression after 36 hours of postoperative blindness. Am J Ophthalmol. 1985;100(4):602–604. doi: 10.1016/0002-9394(85)90690-7. [DOI] [PubMed] [Google Scholar]
- 11.Otto AJ, Koornneef L, Mourits MP, Deen-van Leeuwen L. Retrobulbar pressures measured during surgical decompression of the orbit. Br J Ophthalmol. 1996;80(12):1042–1045. doi: 10.1136/bjo.80.12.1042. [DOI] [PMC free article] [PubMed] [Google Scholar]