Abstract
In India, majority of patients on dialysis are ‘self paying’ because of limited health insurance coverage available from government as well as private insurance providers. Hence, cost of treatment becomes one deciding factor to choose between the two modalities of dialysis – hemodialysis (HD) and peritoneal dialysis (PD). Aim is to compare the monthly cost of maintenance hemodialysis and peritoneal dialysis at our center. Majority of patients at our center are on thrice a week hemodialysis and three times a day peritoneal dialysis. These patients were asked to submit their total direct cost of treatment of last three months. It included cost of dialysis, erythropoietin, other medicines, monthly laboratory tests, hospitalization cost, travel cost, and any other directly involved in the treatment. Monthly cost (Indian Rupees,  ) was then calculated by averaging the three month cost for each patient. The monthly cost of hemodialysis and peritoneal dialysis was then compared using ‘independent sample t-test’. Thirty five patients were finally included in the analysis (21 on HD and 14 on PD). Demographic profile between the two groups was similar in terms of age, sex ratio, period on dialysis, hemoglobin, blood urea nitrogen, and creatinine. Total monthly cost of dialysis was similar in both the groups (
) was then calculated by averaging the three month cost for each patient. The monthly cost of hemodialysis and peritoneal dialysis was then compared using ‘independent sample t-test’. Thirty five patients were finally included in the analysis (21 on HD and 14 on PD). Demographic profile between the two groups was similar in terms of age, sex ratio, period on dialysis, hemoglobin, blood urea nitrogen, and creatinine. Total monthly cost of dialysis was similar in both the groups ( 29,252 ± 6859 vs.
29,252 ± 6859 vs.  28,763 ± 5486, P = 0.85). The lower cost of hemodialysis procedure per se as compared to peritoneal dialysis procedure cost (
28,763 ± 5486, P = 0.85). The lower cost of hemodialysis procedure per se as compared to peritoneal dialysis procedure cost ( 14,669 ± 1376 vs.
14,669 ± 1376 vs.  19,528 ± 4072, P = 0.000) was compensated by higher cost of erythropoietin (
19,528 ± 4072, P = 0.000) was compensated by higher cost of erythropoietin ( 7160 ± 3353 vs.
7160 ± 3353 vs.  3093 ± 1889, P = 0.002) and travel cost (
3093 ± 1889, P = 0.002) and travel cost ( 1654 ± 1085 vs.
1654 ± 1085 vs.  76 ± 66, P < 0.0001) to equalize the monthly cost between the two groups. Our analysis showed no difference in the monthly cost of hemodialysis and peritoneal dialysis and hence, for self-paying patient in India, cost of treatment should not be a deciding factor while choosing between the two modalities.
76 ± 66, P < 0.0001) to equalize the monthly cost between the two groups. Our analysis showed no difference in the monthly cost of hemodialysis and peritoneal dialysis and hence, for self-paying patient in India, cost of treatment should not be a deciding factor while choosing between the two modalities.
Keywords: Cost of dialysis, hemodialysis, peritoneal dialysis
Introduction
The two modalities of dialysis – hemodialysis and peritoneal dialysis – are shown to have comparable patient survival.[1] The choice of treatment in most of the cases hence, is on secondary factors like availability, personal suitability or preference and economic implications. In India, most of the patients on dialysis are ‘self-paying’ because of limited availability of health insurance, and so look for comparatively cheaper option of the two dialysis modalities.[2,3] Apparently, peritoneal dialysis is projected and perceived as expensive of the two because of the cost of the dialysate bags.[4,5] However, no comparison is available from our country from patient's perspective. The present study was taken to validate the difference in the monthly cost of maintenance hemodialysis versus peritoneal dialysis.
Patients and Methods
All adult patients (>18 years) who were on dialysis for more than three months and were ‘self payee’ were eligible for the analysis. Included hemodialysis patients were on three times a week dialysis and peritoneal dialysis patients were on three exchanges a day, which is the prevalent practice in our country. Those who had medical reimbursement (government or private) were excluded. Hemodialysis patients, who had hepatitis B or C were also excluded as they were either ‘single use’ dialysis or fewer re-use of the dialyzers. The mean reuse of dialyzer was 10.8 ± 1.6. About 80% patients were on ‘Fresenius F6’ dialyzer and remaining on F8. Hemodialysis patients who were on twice a week dialysis were also excluded. Peritoneal dialysis patients who were on cyclers or were on ‘life-time scheme’, where they pay a prefixed sum and are covered for rest of their lives, were also excluded. Included patients were on three exchanges –6 to 7.5 L, a day.
Patients were given a tabled sheet to write all the direct cost (Indian Rupees,  ) incurred in the previous three months (August 2010 to October 2010), in their treatment. Later, these were categorized as hemodialysis charge, peritoneal dialysate charge, erythropoietin cost, other medicine charges, laboratory charges, travel cost, hospitalization cost, if any, and other charges including other consumables like dialyzers, tubing, transfer set, minicaps, etc. Indirect costs resulting from work loss and time spent in dialysis and transportation of the patient and attendant have not been included in the study. The total monthly cost of treatment for individual patient was compared between hemodialysis and peritoneal dialysis group.
) incurred in the previous three months (August 2010 to October 2010), in their treatment. Later, these were categorized as hemodialysis charge, peritoneal dialysate charge, erythropoietin cost, other medicine charges, laboratory charges, travel cost, hospitalization cost, if any, and other charges including other consumables like dialyzers, tubing, transfer set, minicaps, etc. Indirect costs resulting from work loss and time spent in dialysis and transportation of the patient and attendant have not been included in the study. The total monthly cost of treatment for individual patient was compared between hemodialysis and peritoneal dialysis group.
Analysis
All variables were expressed as mean and standard deviation. Comparison between the two groups was done by independent sample t-test. The data was analyzed using SPSS 17 (SPSS Inc. Chicago, IL, USA).
Results
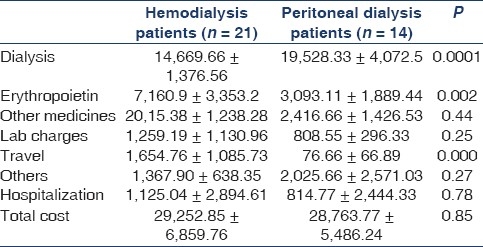
A total of 35 patients – 21 of 61 hemodialysis patients and 14 of 34 peritoneal dialysis patients were finally included in the analysis [Figure 1]. Mean age, sex ratio, mean hemoglobin, blood urea nitrogen and creatinine were similar in both the groups [Table 1]. Mean period on dialysis was also similar in both the groups. Serum albumin was found to be higher in HD as compared to PD group (3.8 ± 0.4 vs. 3.1 ± 0.5, P = 0.003). Hemodialysis procedure cost was significantly lower as compared to the peritoneal dialysis procedure cost (14669 ± 1376 vs. 19528 ± 4072, P = 0.000). Monthly cost of erythropoietin (7160 ± 3353 vs. 3093 ± 1889, P = 0.002) and travel cost to the center (1654 ± 1085 vs. 76 ± 66, P = 0.000) was higher in hemodialysis as compared to PD group. Other direct costs involved in treatment like medicines other than erythropoietin, laboratory charges, hospitalization expenses and other miscellaneous costs like transfer set in PD or dialyzer and tubing in HD group were similar [Table 2]. The total monthly cost of treatment was similar in both HD and PD group (29252 ± 6859 vs. 28763 ± 5486, P = 0.85). A total of four admissions were done in the three months – one peritoneal dialysis patient with pneumonia and three hemodialysis patient for re-do arteriovenous fistula, pneumonia, and pyelonephritis, respectively. None of the patients developed peritonitis in those three months.
Figure 1.
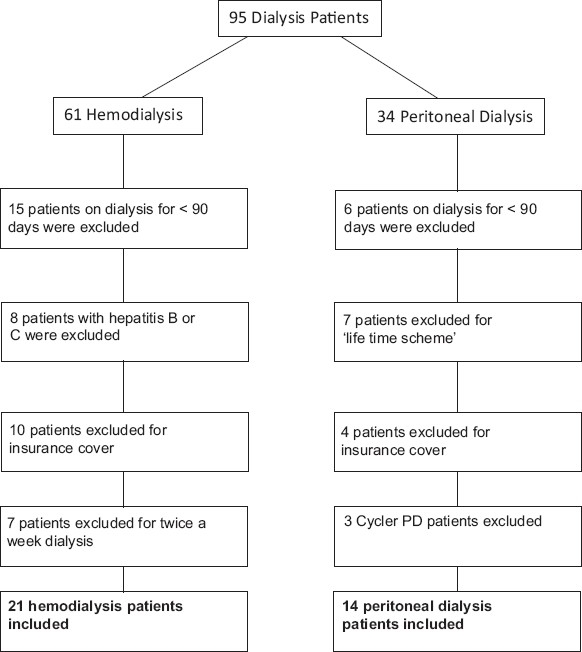
Patient flow included in the study
Table 1.
Demographics of patients on hemodialysis and peritoneal dialysis
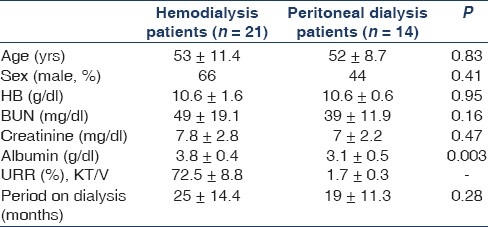
Table 2.
Break-up of monthly cost of maintenance dialysis (all in INR,  )
)
Discussion
Health economic studies comparing the two modalities of dialysis have shown peritoneal dialysis to be cheaper than in-center hemodialysis.[6–8] However, most of these studies are done from ‘caregiver's perspective’ where they have included cost of installation, equipment, and other logistics in initiating a unit. In India, majority of patients are ‘self payee’, and hence decision between the two modalities is greatly influenced by the recurring cost of the treatment. Looking at the ‘dialysis cost’ only, PD apparently looks more costly than HD because of high cost of the dialysate.[7] However, the overhead cost of treatment paid by the patient with each modality is significantly different. We did a pilot study to look at the overall monthly maintenance cost of both the dialysis modalities from patient's perspective rather than from the ‘caregiver's perspective’.
Our study showed that the apparent dialysis cost of PD is much higher than HD when only dialysate cost is compared to hemodialysis procedure cost. This is also shown by Li et al.,[9] in their analysis. However, when the total monthly cost of treatment, including the overheads is compared, there is no difference between the two modalities. The higher cost of dialysate is compensated by lower cost incurred in erythropoietin and travel to the center per month. Cost and requirement of erythropoietin is almost twice in hemodialysis as compared to peritoneal dialysis ( 7160 vs.
7160 vs.  3093, P = 0.002). Higher dose and frequency of erythropoietin requirement in hemodialysis is also shown in a multicenter study done by Coronel et al.,[10] Similarly, travel cost was much higher in hemodialysis (
3093, P = 0.002). Higher dose and frequency of erythropoietin requirement in hemodialysis is also shown in a multicenter study done by Coronel et al.,[10] Similarly, travel cost was much higher in hemodialysis ( 1654 vs.
1654 vs.  76) as patient had to travel three times every week as compared to peritoneal dialysis patients, who come once every month.
76) as patient had to travel three times every week as compared to peritoneal dialysis patients, who come once every month.
There are few limitations of the study. First, it is single center pilot study. Second, the comparison is between three sessions of HD a week and three exchanges of PD a day. However, this is the standard practice in our country and majority of PD patients (68%, as reported by PD registry and Baxter, India) are on three exchanges a day. Similarly, many patients are on twice a week hemodialysis in India, and hence this study may not be applicable to them. Third, in India, cost of PD consumables is more or less similar all over the country while hemodialysis cost varies from one center to another and from one city to another city. Because of this difference in hemodialysis cost, uniform conclusion is difficult to make regarding the comparative cost analysis between the two dialysis modalities. However, considering our dialysis center as a prototype and  1150 as cost of one session of hemodialysis, the monthly total cost of hemodialysis and peritoneal dialysis has been shown to be similar for the patient. So, centers where the cost and practice pattern are comparable can extrapolate possible similar results, centers where the cost of hemodialysis is more than our center may have hemodialysis as more expensive and vice versa, and centers where the charges are less than ours may conclude PD to be more expensive than HD.
1150 as cost of one session of hemodialysis, the monthly total cost of hemodialysis and peritoneal dialysis has been shown to be similar for the patient. So, centers where the cost and practice pattern are comparable can extrapolate possible similar results, centers where the cost of hemodialysis is more than our center may have hemodialysis as more expensive and vice versa, and centers where the charges are less than ours may conclude PD to be more expensive than HD.
To conclude, our study showed no difference in total monthly cost of hemodialysis or peritoneal dialysis and hence decision between the two modalities should not be based on the recurring cost. In view of differences in hemodialysis cost between centers and differences in initiation cost, a multicenter study is being planned to address this issue in a more detailed manner.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Mehrotra R, Chiu YW, Kalantar-zadeh K, Bargman J, Vonesh E. Similar outcomes with hemodialysis and peritoneal dialysis in patients with end-stage renal disease. Arch Intern Med. 2011;171:110–8. doi: 10.1001/archinternmed.2010.352. [DOI] [PubMed] [Google Scholar]
- 2.Jha V. End-stage renal care in developing countries: The Indian Experience. Renal Fail. 2004;26:201–8. doi: 10.1081/jdi-120039516. [DOI] [PubMed] [Google Scholar]
- 3.Jha V. Current status of end-stage renal disease care in south Asia. Ethn Dis. 2009;19:S1-27–32. [PubMed] [Google Scholar]
- 4.Agarwal SK, Srivastava RK. Chronic kidney disease in India: Challenges and solutions. Nephron Clin Pract. 2009;111:197–203. doi: 10.1159/000199460. [DOI] [PubMed] [Google Scholar]
- 5.Khanna U. The economics of dialysis in India. Indian J Nephrol. 2009;19:1–4. doi: 10.4103/0971-4065.50671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Just PM, Charro FT, Tschosik EA, Noe LL, Bhattacharyya SK, Riella MC. Reimbursement and economic factors influencing dialysis modality choice around the world. Nephrol Dial Transplant. 2008;23:2365–73. doi: 10.1093/ndt/gfm939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haller M, Gutjahr G, Kramar R, Harnoncourt F, Oberbauer R. Cost-effectiveness analysis of renal replacement therapy in Austria 2011. Nephrol Dial Transplant. 2011 doi: 10.1093/ndt/gfq780. [In Press] [DOI] [PubMed] [Google Scholar]
- 8.Berger A, Edelsberg J, Inglese GW, Bhattacharyya SK, Oster G. Cost comparison of peritoneal dialysis versus hemodialysis in end-stage renal disease. Am J Manag Care. 2009;15:509–18. [PubMed] [Google Scholar]
- 9.Li PK, Chow KM. The cost barrier tp peritoneal dialysis in the developing world – An Asian perspective. Perit Dial Int. 2001;21:S307–13. [PubMed] [Google Scholar]
- 10.Coronel F, Herrero JA, Montenegro J, Fernandez C, Gandara A, Conesa J, et al. Erythropoietin requirements: A comparative multicenter study between peritoneal dialysis and hemodialysis. J Nephrol. 2003;16:697–702. [PubMed] [Google Scholar]


