Abstract
BACKGROUND:
Relationship between premature menopause and presence, severity and life-threatening events of coronary artery disease (CAD) has been suggested in recent observations. The present study tried to assess relationship between age of menopause and severity of CAD in a sample of women with suspected CAD.
METHODS:
In a cross-sectional study, we included 189 consecutive women with suspected CAD that were candidate for coronary angiography and admitted to the Shafa hospital in Kerman city. Our final population for analysis included women who underwent natural menopause (n = 148) or premature menopause (n = 41). CAD severity was classified according to the number of coronary artery stenosis ≥ 50% in coronary angiography.
RESULTS:
Among 189 study patients with suspected CAD, 22.0% of those with early menopause and 23.6% of those with normal menopause suffered three coronary vessels involvement, while normal angiography features was shown in 39.0%o and 40.5%>, respectively. Regarding severity of CAD and left main lesions, no significant differences were found between the patients with and without premature menopause. According to the multivariable logistic regression model and with the presence of other patients’ variables as cofounders, age of menopause could not predict the presence and severity of CAD in patients with suspected CAD. However, patients’ age (OR: 1.11, p < 0.001) and family history of CAD (OR: 2.05, p = 0.04) were main predictors of the severity of CAD in these patients.
CONCLUSIONS:
Premature menopause does not predict occurrence or severity of CAD in women with suspected CAD, but women age and their family history of CAD are main predictors of the severity of CAD.
KEYWORDS: Coronary Artery Disease, Risk Factor, Age, Menopause, Premature Menopause
The use of exogenous estrogen has been hypothesized to be associated with reducing the risk of coronary artery disease (CAD) during postmenopausal period.1 It has been also demonstrated that the surgical menopause in younger individuals results in the increase of CAD risk if hormone therapy is not taken.2 Although relationship between premature menopause and presence, severity, and even life-threatening events of cardiovascular disease has been suggested, a few studies focused on demonstrating the relationship of a broad range of ages at menopause with risk of CAD. In a study by van der Schouw and his colleagues,3 the rate of cardiovascular mortality was not significantly associated with later age at natural menopause. This non-significant association was also observed in similar studies.4,5 Contrarily, McVay et al.6 observed an overall significant association between risk of CAD and younger age at menopause among women who experienced natural menopause and never used hormone therapy. It seems that the obtained results were strongly influenced by some study limitations such as effects of other important cofounders such as smoking or inappropriate age cut-off points.6,7
Hence, the present study tried to assess relationship between age of menopause and severity of CAD with the presence of other affecting factors in a sample of women with suspected CAD.
Methods
In a cross-sectional study, we included 189 consecutive women with suspected CAD that were candidate for coronary angiography and admitted to the Shafa hospital in Kerman city between February 2009 and September 2010. Early diagnosis was based on clinical evidences and non-invasive tests, including typical chest pain, increase in serum creatine kinase (CK) level, and diagnostic specific changes in ECG.8 We excluded women who reported having a previous history of coronary heart disease (CHD) or underwent coronary interventions at baseline. On the questionnaires filled by the trained practitioners, menopausal status was determined by asking whether the participants’ menstrual periods had ceased permanently and, if so, at what age and for what reason (occurring naturally or after radiation treatment or surgery). Our final population for analysis included women who underwent natural menopause (n = 148) or premature menopause (n = 41) and never received hormone therapy or had previous history of hysterectomy. Premature menopause was defined as cessation of menses before age 40 years.9 The study was approved by the ethics committee of the Kerman University of Medical Sciences and informed consent was obtained from all patients.
Demographic characteristics and clinical information of these patients were extracted from hospital recorded files as well as face to face interviewing if required and entered into a computerized database form. Information on other potential CHD risk factors were assessed including participants’ age, smoking, weight, drug history within two months before admission, and history of diabetes (symptoms of diabetes plus at least one of the following conditions: plasma glucose concentration ≥ 11.1 mmol/1, fasting plasma glucose ≥ 7.0 mmol/1 or 2-hpp ≥ 11.1 mmol/1),10 hypertension (systolic blood pressure ≥ 140 mmHg and/or diastolic ≥ 90 mmHg and/or on antihypertensive treatment)11, hypercholesterolemia (total cholesterol ≥ 5.0 mmol/1, HDL-cholesterol ≥ 1.0 mmol/1 in men, or ≥ 1.1 mmol/1 in women, and triglycerides ≥ 2.0 mmol/1),12 and opium addiction (regularly consumption of opium by inhalation more than three times per week and/ or daily oral opium defined based on the DSM-IV Criteria for Substance Dependence).13 Patients underwent two-dimensional echocardiography for assessing left ventricular ejection fraction and ruling our other structural abnormalities as well as coronary angiography for determining presence and severity of CAD. All coronary angiography procedures were performed by the femoral approach using the standard Judikin's technique14 and the coronary angiograms were analyzed by a cardiologist. The lesion in the left main coronary artery (LM), left anterior descending coronary artery (LAD), left circumflex coronary artery (LCX) and right coronary artery (RCA) were recorded, the 1-vessel disease, 2-vessel disease and 3-vessel disease was classified according to the number of coronary artery stenosis ≥ 50%.
Results were reported as mean ± standard deviation (SD) for the quantitative variables and percentages for the categorical variables. Variables between the two subgroups were compared using the chi-square test for categorical variables and the student-t test or Mann Whitney U test for the continuous variables. Multivariate logistic regression analysis was used to investigate association between age of menopause and presence of CAD while the model was adjusted for baseline data as cofounders. P-values of 0.05 or less were considered statistically significant. All the statistical analyses were performed using SPSS version 13.0 (SPSS Inc., Chicago, IL, USA) for Windows.
Results
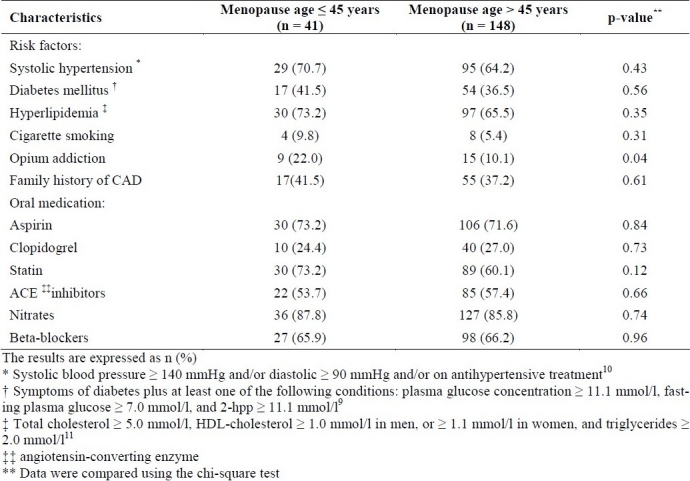
There were no significant differences between the two study groups with premature and normal menopause in terms of mean age (58.61 ± 7.27 versus 60.26 ± 7.06, p = 0.20) as well as mean weight (64.49 ± 15.08 versus 63.79 ± 10.20, p = 0.78). Among general risk factors for coronary artery disease (Table 1), except for opium addiction that was more prevalent in the group with early menopause, overall prevalence of other risk factors was similar between two groups. Furthermore, cardiovascular-related drugs were similarly administered in the two groups. The mean of left ventricular ejection fraction was significantly higher in the patients with premature menopause (57.50 ± 5.24 versus 49.33 ± 11.21, p = 0.01). The number of parity in the patients with and without early menopause was similar (7.43 ± 2.92 versus 7.55 ± 2.65, p = 0.80). No significant difference was also observed in the number of babies between them (6.15 ± 2.24 versus 6.44 ± 2.22, p = 0.47).
Table 1.
Baseline characteristics and clinical data of the study subjects
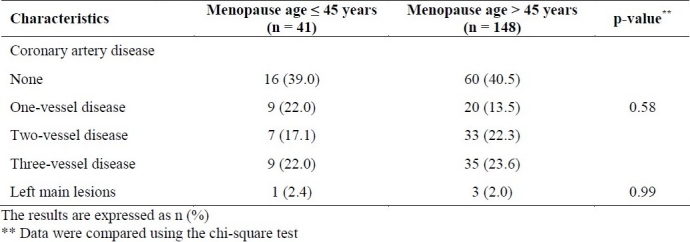
Among study patients with suspected CAD, 22.0% of those with early menopause and 23.6% of those with normal menopause suffered three coronary vessels involvement, while normal angiography features was found in 39.0% and 40.5%, respectively (Table 2). Regarding severity of CAD and left main lesions, no significant differences were found between the patients with and without premature menopause (Table 2).
Table 2.
Severity of coronary artery disease according to the angiography features
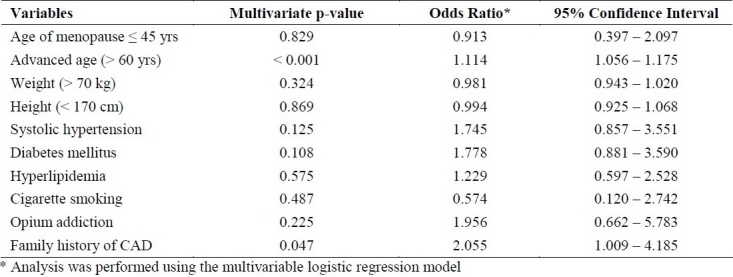
According to the multivariable logistic regression model (Table 3) and with the presence of other patients’ variables as cofounders, age of the menopause could not predict the presence and severity of CAD in patients with suspected CAD. Among other factors, patients’ age (OR: 1.11, p < 0.001) and family history of CAD (OR: 2.05, p = 0.04) were the main predictors of the severity of CAD in this study.
Table 3.
Multivariable analysis of the role of age of menopause for predicting presence and severity of CAD
Discussion
In general, no significant association was found in this study between the appearance of early menopause and severity of CAD among women who had natural or earlier menopause and never used hormone therapy. We even hypothesized that the relation between premature menopause and CAD severity might be influenced by some potential confounders such as current smoking or opium use, however, this relationship was not proved using multivariable models when it was adjusted for con-founding factors. Recently, it has been proposed that the early menopause can be directly associated with higher risk of angina after myocardial infarction, independent of other co-morbidities, and even severity of infarction.15
The largest previous study was conducted by van der Schouw et al.3 who examined the relation of age at menopause with total cardiovascular mortality. There was a significant increased risk with decreased age at menopause for each 1-year, but this inverse association was not statistically significant among women with natural menopause. They found that the inverse association was limited to non-current smokers, but they did not examine the association specifically among never smokers.
PRECADIW study revealed that besides smoking, parental history of premature CVD, diabetes, menopause and hypertension that were the strongest risk markers for premature CAD, early menopause was the most important determinant of premature CAD in a model including the early and late stages of menopause.16 Thus, according to our result, age of menopause does not induce extension of infarction in affected patients, but based on similar researches, early menopause might be a trigger for angina after myocardial infarction or even induced severe CAD that needs further evaluation.
As shown in previous studies,16–19 both cigarette smoking and opium addiction are powerful risk factors for CAD. In our study, current smoking decreased the age of natural menopause by about 1.5 years and opium addiction decreased it by 2.5 year. Thus, incomplete adjustment for smoking or opium addiction in some other studies might have artificially increased the risk of CAD associated with early age of natural menopause. Hence, it is better to reconsider evaluation of this association among never smokers or opium users.
Authors’ Contributions
HN drafted the manuscript, MSh conducted the statistical analysis, YM collected samples and performed the study and this manuscript was derived from his thesis and, AF participated in the study.
Footnotes
Conflict of Interests Authors have no conflict of interests.
References
- 1.Grodstein F, Stampfer M. The epidemiology of coronary heart disease and estrogen replacement in postmenopausal women. Prog Cardiovasc Dis. 1995;38(3):199–210. doi: 10.1016/s0033-0620(95)80012-3. [DOI] [PubMed] [Google Scholar]
- 2.Colditz GA, Willett WC, Stampfer MJ, Rosner B, Speizer FE, Hennekens CH. Menopause and the risk of coronary heart disease in women. N Engl J Med. 1987;316(18):1105–10. doi: 10.1056/NEJM198704303161801. [DOI] [PubMed] [Google Scholar]
- 3.Van Der Schouw YT, van der Graaf Y, Steyerberg EW, Eijkemans JC, Banga JD. Age at menopause as a risk factor for cardiovascular mortality. Lancet. 1996;347(9003):714–8. doi: 10.1016/s0140-6736(96)90075-6. [DOI] [PubMed] [Google Scholar]
- 4.Snowdon DA, Kane RL, Beeson WL, Burke GL, Sprafka JM, Potter J, et al. Is early natural menopause a biologic marker of health and aging? Am J Public Health. 1989;79(6):709–14. doi: 10.2105/ajph.79.6.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooper GS, Sandler DP. Age at natural menopause and mortality. Ann Epidemiol. 1998;8(4):229–35. doi: 10.1016/s1047-2797(97)00207-x. [DOI] [PubMed] [Google Scholar]
- 6.McVay MA, Copeland AL. Smoking cessation in peri- and postmenopausal women: a review. Exp Clin Psychopharmacol. 2011;19(3):192–202. doi: 10.1037/a0023119. [DOI] [PubMed] [Google Scholar]
- 7.Pokoradi AJ, Iversen L, Hannaford PC. Factors associated with age of onset and type of menopause in a cohort of UK women. Am J Obstet Gynecol. 2011 doi: 10.1016/j.ajog.2011.02.059. [DOI] [PubMed] [Google Scholar]
- 8.Wright RS, Anderson JL, Adams CD, Bridges CR, Casey DE, Jr, Ettinger SM, et al. 2011 ACCF/AHA focused update incorporated into the ACC/AHA 2007 Guidelines for the Management of Patients with Unstable Angina/Non-ST-Elevation Myocardial Infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in collaboration with the American Academy of Family Physicians, Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;57(19):e215–e367. doi: 10.1016/j.jacc.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 9.Eshtiaghi R, Esteghamati A, Nakhjavani M. Menopause is an independent predictor of metabolic syndrome in Iranian women. Maturitas. 2010;65(3):262–6. doi: 10.1016/j.maturitas.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Diagnosis and classification of diabetes mellitus. Diabetes Care. 2008;31(Suppl 1):S55–S60. doi: 10.2337/dc08-S055. [DOI] [PubMed] [Google Scholar]
- 11.Chalmers J, MacMahon S, Mancia G, Whitworth J, Beilin L, Hansson L, et al. 1999 World Health Organization-International Society of Hypertension Guidelines for the management of hypertension. Guidelines sub-committee of the World Health Organization. Clin Exp Hypertens. 1999;21(5-6):1009–60. doi: 10.3109/10641969909061028. [DOI] [PubMed] [Google Scholar]
- 12.Wood D, De Backer G, Faergeman O, Graham I, Mancia G, Pyorala K. Prevention of coronary heart disease in clinical practice.Recommendations of the Second Joint Task Force of European and other Societies on coronary prevention. Eur Heart J. 1998;19(10):1434–503. doi: 10.1016/s0021-9150(98)90209-x. [DOI] [PubMed] [Google Scholar]
- 13.Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR (Text Revision) 4th ed. Washington DC: Amer Psychiatric Pub; 2000. American Psychiatric Association. [Google Scholar]
- 14.Berti S, Feres F, Castro D, Gusmao M, Staico R, Padilha R, et al. [Coronary arteriography with a very low profile catheter: efficacy and safety of the procedure and of the 60 minute hospital discharge] Arq Bras Cardiol. 1998;70(1):3–7. doi: 10.1590/s0066-782x1998000100002. [DOI] [PubMed] [Google Scholar]
- 15.Parashar S, Reid KJ, Spertus JA, Shaw LJ, Vaccarino V. Early menopause predicts angina after myocardial infarction. Menopause. 2010;17(5):938–45. doi: 10.1097/gme.0b013e3181e41f54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lubiszewska B, Kruk M, Broda G, Ksiezycka E, Piotrowski W, Kurjata P, et al. The impact of early menopause on risk of coronary artery disease (PREmature Coronary Artery Disease In Women - PRECADIW case-control study) Eur J Cardiovasc Prev Rehabil. 2011 doi: 10.1177/1741826710394269. [DOI] [PubMed] [Google Scholar]
- 17.Sadr Bafghi SM, Rafiei M, Bahadorzadeh L, Namayandeh SM, Soltani MH, Motafaker M, et al. Is opium addiction a risk factor for acute myocardial infarction? Acta Medica Iranica. 2011;43(3):218–22. [Google Scholar]
- 18.Asgary S, Sarrafzadegan N, Naderi GA, Rozbehani R. Effect of opium addiction on new and traditional cardiovascular risk factors: do duration of addiction and route of administration matter? Lipids Health Dis. 2008;7:42. doi: 10.1186/1476-511X-7-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sadeghian S, Graili P, Salarifar M, Karimi AA, Darvish S, Abbasi SH. Opium consumption in men and diabetes mellitus in women are the most important risk factors of premature coronary artery disease in Iran. Int J Cardiol. 2010;141(1):116–8. doi: 10.1016/j.ijcard.2008.11.063. [DOI] [PubMed] [Google Scholar]


