Abstract
BACKGROUND:
Some studies indicate that psychological factors and extra-intestinal symptoms affect health related quality of life (HRQoL) in patients with irritable bowel syndrome (IBS) more than what bowel symptoms themselves. Type D personality characterized by global traits including negative affectivity and social inhibition has been proposed to be related to HRQoL. The aim of this study was to determine the association between type D personality and HRQoL inpatients with IBS.
METHODS:
In a cross-sectional study, 194 consecutive patients with IBS referred to two referral gastrointestinal clinics affiliated with Isfahan University of Medical Sciences were selected in respect of inclusion and exclusion criteria. The patients completed type D personality (DS-14), IBS quality of life and the IB severity scoring (IBS-SSS) scales. The patients were divided into two groups with and without type D personality using DS-14. The data was analyzed using ANCOVA and multiple regression.
RESULTS:
The findings indicated that 40.7% of the patients had type D personality. The results of ANCOVA with controlling for the influence of severity of IBS and treatment duration showed significant difference between the two groups in health related quality of life (F = 11.89, p < 0.01). Multiple regression analysis indicated negative affectivity (ß =-0.283, p < 0.01), severity of symptoms (ß = 0.279, p = 0.000) and duration of treatment (ß =-0.189, p < 0.05) as the significant predictors for HRQoL in patients with IBS.
CONCLUSIONS:
Type D personality may be an important determinant of individual differences in HRQoL among IBS patients. Negative affectivity as one of type D dimensions may have an adverse effect on HRQoL in patient with IBS. Therefore, additional attention is needed in IBS patients with type D personality.
KEYWORDS: Type D Personality, Negative Affectivity, Social Inhibition, Irritable Bowel Syndrome, Quality of Life, Psychosomatic Disorders
Irritable bowel syndrome (IBS) is a common chronic functional gastrointestinal disorder1 which negatively affects health related quality of life (HRQoL) among the patients.2,3 Previous studies showed that psychological factors and extra-intestinal symptoms affect HRQoL in patients with IBS more than bowel symptoms themselves do.1,4 Psychological factors such as personality factors have been shown to play a role in IBS.5 In addition, personality traits have been shown to be associated with poor HRQoL.6
Personality is an important mediator of chronic stress.7 Recently, a new personality construct, type D or ‘distressed’ personality, has been proposed.6,8 This construct is a result of an investigation on coping styles in men with coronary heart disease.7–9
The taxonomy of type D personality is based on two global and stable personality traits, namely negative affectivity (NA) and social inhibition (SI).10 NA refers to the tendency to experience negative emotions across time or situations.7,8 High-NA individuals experience more feelings of dysphoria, anxiety, and irritability. They also have a negative view of self and scan the world for signs of impending trouble. SI refers to the tendency to inhibit the expression of emotions or behaviors in social interactions to avoid disapproval by others. High-SI individuals tend to feel inhibited, tense, and insecure when with others.8 People with type D personality experience more stress in their lives and are more vulnerable to psychological distress.8,10
Type D patients are at increased risk for a wide range of adverse health outcomes.6,10 Finally, Type D patients are at risk for clustering of psychological risk factors, including depression, anxiety, and irritability, and low levels of self-esteem, well-being, and positive affect.11 The evidence showed that type D personality decreases HRQoL in patients with cardiovasular disorders.6 However, not much data is available about the effect of type D personality on quality of life in patients with non-cardiac disorders. For example, only in a recent study Hansel et al. found that type D personality is associated with decreased perceived HRQoL in patients with functional gastrointestinal disorders.12 However, there is no study about the association between type D personality and HRQoL in patients with IBS. Identifying and modifying determinants of HRQoL in IBS patients can help policy makers to make proper decisions.
Therefore, the aim of this study was to determine the association between type D personality and HRQoL in IBS patients.
Methods
This study was a cross-sectional survey for examining the relationship between type D personality and HRQoL in patients with IBS. The study was approved by the research council of Behavioral Sciences Research Center at Isfahan University of Medical Sciences. An informed consent was obtained from each patient and the study protocol conformed to the ethical guidelines of the research center.
Participants
The sample population composed of 194 consecutive patients with IBS. Data were gathered from patients attending two referral gastrointestinal clinics affiliated with Isfahan University of Medical Sciences during December, 2008-September, 2009.
Inclusion criteria were 1) fulfilling Rome III criteria for IBS;13 2) aging between 18-65 years; and 3) being able to read and write. Patients were excluded if they had 1) an organic gastrointestinal disorders; 2) a serious illness that decreased life expectancy; 3) a major psychiatric disorder; or 4) a cognitive disorder. The third and fourth exclusion criteria were evaluated according to the patients’ medical profiles and their self-report of the disorder.
The procedure was as follows: First, patients were interviewed by a gastroenterologist and those who fulfilled inclusion criteria and had no exclusion criteria were referred to a medical student in the clinics. Then, the aim and process of the study along with the confidentiality of the gathered information were explained to the patients. If the patient agreed to continue the study, a written consent form was obtained. Then, patients were asked to read and complete 4 questionnaires including type D personality scale (DS14), IBS Quality of Life (IBSQOL),14,15 is the IBS severity scoring scale (IBS-SSS) and the demographic question-naire. Essential information and explanations on filling each questionnaire were provided by the medical students. The Persian version of DS14 contains 14 items categorized into two seven-item subscales regarding NA and SI. The items were answered on a five point Likert scale from 0 (false) to 4 (true) resulting in maximum scores of 28 for NA and SI. A predeter-mined cut-off of > 10 on both subscales was used to determine those with a type D personality.1,12 Examples of items measuring NA were ‘I often make a fuss of unimportant things’, and ‘I often feel unhappy’. ‘I often feel inhibited in social interactions’, and ‘I find it hard to start a conversation’ were examples of items of the SI subscale. In an investigation on psychometric properties of DS14 conducted by Denollet, the NA and SI subscales were internally consistent (α = 0.88/0.86; N = 3678) and stable over a 3-month period (test-retest r = 0.72/0.82). Using this scale, the patients were divided into two groups with and without type D personality.8
Factor analysis of the Persian version of DS14 in a recent Iranian study yielded in the two-factor structure. All of the NA and SI items loaded withn 0.65-0.80 on their corresponding factor. The NA and the SI subscales had good test-retest stability over a 2-month period (test–retest r = 0.86 and 0.77, respectively). In addition, a high internal consistency was found based on Cronbach's alpha coefficient (0.84 for the NA subscale and 0.86 for the SI subscale).14
The IBSQOL-34 questionnaire was a disease-specific quality of life scale designed to evaluate HRQoL in patients with IBS. This scale consisted of 34 items with a Likert scale from 1 to 5. The quality of life (QOL) scores needed be converted into 0 to 100 points. After converting the raw scores on the IBSQOL into 0 to 100, higher values indicated better QOL and lower scores indicated more impaired HRQoL. External and internal reliability and validity of this scale have been proved. Moreover, findings showed the IBSQOL-34 to be responsive to treatment in a referral-based clinical population of patients with functional bowel disorders.15
A recent Iranian study investigating the psychometric properties of Persian version of the IBSQOL-34 showed good internal reliability and validity for the scale and its eight subscales (Cronbach's alpha = 0.93 for the whole questionnaire, and also 0.88 for dysphoria, 0.67 for activities interference, 0.72 for body image, 0.57 for health worry, 0.57 for food abstinence, 0.71 for social reaction, 0.76 for sexual worry, and 0.62 for interpersonal relations). The validity was measured against another quality of life questionnaire (IBSQOL-36) and a significant correlation was found (r = 0.61). Thus, the Persian version of IBSQOL-34 questionnaire was confirmed to be a valid and reliable scale for patients with IBS.16
The IBS-SSS was developed to assess the major gastrointestinal symptoms in IBS patients. This scoring system is simple and consists of only 5 actual scoring questions incorporating severity of abdominal pain, abdominal distension, and dissatisfaction with bowel habits and interference with life in general (QOL). Patients answered each question by scoring their bowel symptoms from 0 to 100 using prompted visual analogue scales, leading to a total possible score of 500. Visual analogue scales have been proved to be a reliable method for recording symptom severity. Similarly, the scale used here has been proved reliable for assessing severity of IBS symptoms.17
A demographic and medical questionnaire was completed for each patient. This questionnaire included questions about demographic characteristics, as well as social and economic factors. The subjects underwent a physical examination. Medical data were obtained from medical records.
Demographic characteristics included age, gender, marital status, level of education, and socioeconomic status. Education was categorized in three levels: low (primary school), medium (lower vocational training or secondary school), and high (higher vocational training or university degree). Socioeconomic status was assessed using the criteria based on current employment of the subjects or their last jobs if they were retired, accommodation, living area, income, and education level. Socioeconomic status was categorized in three levels: low, medium and high.
Statistical analysis
Student t-test and chi-square test were used for continuous variables and categorical variables, respectively. Then, ANCOVA test was utilized to define the association between type D personality and HRQoL in patients with IBS. In addition, multiple regression (enter method) was used to determine the independent association between the predictive variables and HRQoL in IBS patients. A p = 0.05 was defined as statistically significant. SPSS version 16.0 (SPSS Inc., Chicago, IL, USA) for windows was applied for data analysis.
Results
One hundred and ninety four patients with IBS enrolled in this study. Some characteristics of patients are listed in Table 1. The average age of the subjects was 35.55 ± 11.53 years. The population included 64.8% females (with female to male ratio of 1.84), 73.1% married individuals. Moreover, 92.8% of the patients were from urban areas. Using the cut-off point of 10 for either subscale of NA and SI, 79 patients (40.7%) had type D personality. There was no significant difference between demographic characteristics of patients with and without type D personality (p > 0.05).
Table 1.
Comparison of the characteristics of patients with and without type D personality
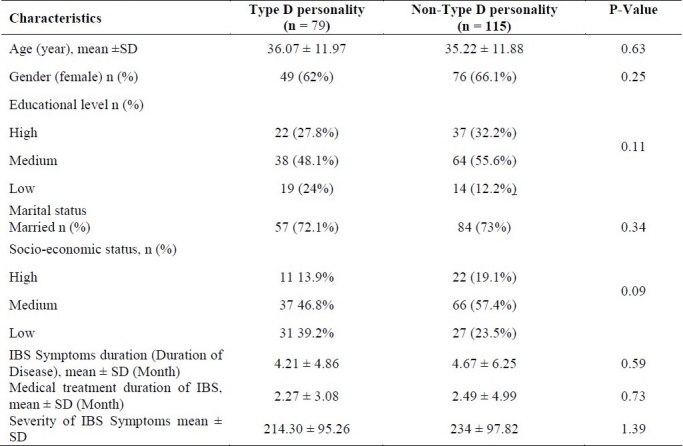
The mean score of IBSQOL for type D patients was 58.02 ± 22.80 and the mean score of IBSQOL for patients without type D personality was 66.82 ± 20.15. The maximum QOL score was 100 points.
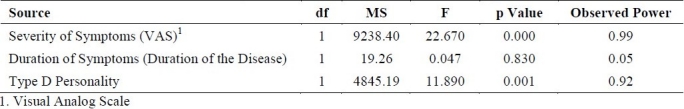
Type D personality together with covariants of symptom severity and duration of symptoms was analyzed by ANCO VA test (Table 2). The results of ANCOVA showed a significant difference (F = 11.89, p < 0.01) between the two groups (with and without Type D personality) in HRQoL (Table 2).
Table 2.
Summary of the results from covariance analysis model
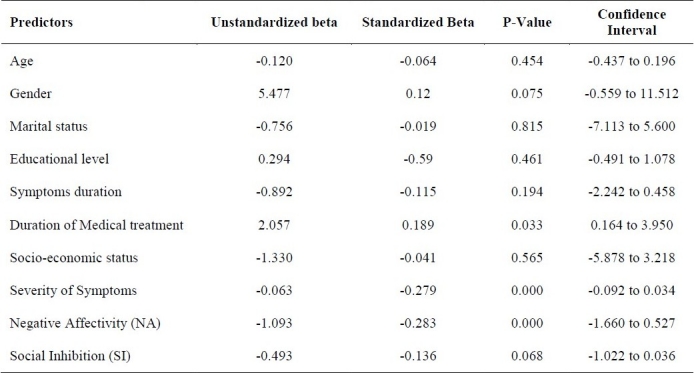
Regression analysis adjusted for some demographic and clinical characteristics showed that NA (ß = -0.283, p < 0.01), severity of symptoms (ß = 0.279, p < 0.01) and duration of treatment (ß = -0.189, p < 0.05) remained strong independent determinants of HRQoL in patients with IBS (Table 3). Although SI was not significantly associated with HRQoL (ß = -0.135, p = 0.068), there was a tendency for significance in this variable.
Table 3.
Summary of the results from multiple regression model for predictors of quality of life
Discussion
HRQoL has been an interesting issue in medical research. Today, the necessity of identifying determinants of QOL in patients with IBS is also becoming important for clinicians. IBS, as a common chronic functional gastrointestinal disorder, may cause impaired QOL.4,18 Many research studies have identified some of the factors that affect QOL in IBS patients. Impairment in HRQoL of IBS patient depends on several factors particularly, psychological factors.19 Thus, many studies are still done to clarify what psychological factors affect HRQoL in patient with IBS. Personality factors are likely to partly determine the amount of QOL impairment among IBS patients. However, little is known about these factors at the present time. To our knowledge, this is the first study to determine the association between type D personality and HRQoL in patients with IBS.
The present findings showed that type D personality significantly decreased HRQoL in patients with IBS. When controlling for the influence of severity of IBS symptoms and duration of disease by covariance analysis, type D remained a strong independent determinant of impaired HRQoL. Therefore, type D patients were more likely to have poor HRQoL compared with non-type D subjects. In general, personality may be an important determinant of individual differences in HRQoL in IBS that has often been overlooked.
These findings are in line with those of previous studies on type D personality and impaired HRQoL in patients with heart disease and other medical conditions. Previous studies have shown the links between type D personality and worse health status including poor HRQoL in patients with cardiovascular disorders20 and non-cardiac illnesses such as chronic tinnitus,21 obstructive sleep apnea syndrome,22 diabetic foot syndrome,23 chronic pain,24 melanoma,25 vertigo26 and older primary care,27 In a recent study, type D patients with gastrointestinal symptoms showed lower HRQoL compared with people without type D personal-ity.12 Moreover, a wide variety of other medical populations may be negatively affected by type D personality. The findings of this study and the studies mentioned above support that type D personality is an important psychological variable that may affect not only HRQoL in people with heart disease but also in those with IBS and other medical conditions. This issue was also confirmed by Floortje Mols in a recent review article.20
Regression analysis adjusted for the influence of some demographic and clinical characteristics showed that NA, severity of symptoms and duration of treatment remained strong predictors of impaired HRQoL.
In addition, the findings indicated that NA, as one of type D dimensions, may have an adverse effect on HRQoL in patient with IBS. It is also positively correlated with neuroticism in Eysenck's and Big Five models.8 Neuroticism and aggression are reported to be higher in patients with functional gastrointestinal disease without psychiatric comorbidity. Personality traits are also believed to influence pain reports.28
Although SI was not significantly associated with HRQoL, there was a tendency effect which may be clinically notable. The trait “social inhibition” refers to the tendency to inhibit the expression of emotions/behaviors in social interactions to avoid disapproval by others.8 Although inhibited individuals seem quiet on the surface, they actually feel tense and insecure when with others and tend to experience substantial personal distress. Therefore, social isolation may amplify the adverse effect of negative emotions on HRQoL of patients with IBS. In addition, inhibition may be associated with non-compliance.29 Moreover, the socially inhibited individuals may also be less likely to engage in health-promoting behaviors.30
Another finding was that severity of symptoms and duration of treatment were significantly associated with HRQoL. Overall, the severity of IBS symptoms is strongly related to QOL.31 Clinically, the impact of IBS severity on work and daily activities, and cognitive beliefs about IBS are clear. Also in many studies IBS patients reported integration of the disease into their lives to the extent that the disease becomes a part of their identity.31,32 Thus, to study the links between the strategies used by IBS patients to manage symptoms and their QOL is proposed for future research.
Regarding the effects of IBS severity in various aspects of QOL including work and daily activities, cognitive beliefs about IBS and finally psychological functioning, it is apparent that the treatment of the disease improves patient's QOL by reducing symptoms.
Although, the prevalence of type D personality among patients with IBS in this study was 40.7% which is high compared with rates reported from general population (21 %),10 this rate was similar to the rates in patients with cardiovascular disorders (18-53%).20 However, there is no data available about the prevalence of type D personality among patients with IBS.
Regarding the findings of current study, additional attention is warranted for patients with IBS having type D personality. Although type D personality seems to be a stable state, it should not be assumed that the IBS patient's level of distress affecting their HRQoL could not be modified. IBS patients with type D personality may have the limitations in their coping strategies for adjustment with stressful life events and their medical conditions. Thus, psychological interventions including coping strategy training and quality of life therapy are suggested for IBS patients with type D personality. Future research on the effects of psychological interventions on improving quality of life in type D patients with IBS is needed.
The findings of this study should be interpreted with some caution. First, although the results suggested that type D personality is a risk factor that may decrease HRQoL in patients with IBS, these results were based on a relatively small sample of 194 patients. Future studies with larger sample sizes are required to further confirm this association. Second, the present study was cross-sectional. Therefore, this possibility cannot be rule out that experience of IBS symptoms in during the time of study could have influenced the results; scores on the NA and SI subscales of the type D scale and hence the prevalence of patients with type D personality. Third, patients with major psychological disorders were excluded only based on their medical profile and their self-report.
Authors’ Contributions
RBS coordinated the study, carried out the design, analyzed the data, and prepared the manuscript. HA, PA and HD provided assistance in the design of the study, data collection supervising, and revising the manuscript. JF and FA involved in study design and data collection. All authors have read and approved the content of the manuscript.
Acknowledgments
Thanks are due to the staff of psychosomatic and gastrointestinal clinics affiliated with Isfahan University of Medical Sciences for their corporation. This project was supported by Behavioral Sciences Research Center at Isfahan University of Medical Sciences (Project No. 388474).
Footnotes
Conflict of Interests Authors have no conflict of interests.
References
- 1.Seres G, Kovacs Z, Kovacs A, Kerekgyarto O, Sardi K, Demeter P, et al. Different associations of health related quality of life with pain, psychological distress and coping strategies in patients with irritable bowel syndrome and inflammatory bowel disorder. J Clin Psychol Med Settings. 2008;15(4):287–95. doi: 10.1007/s10880-008-9132-9. [DOI] [PubMed] [Google Scholar]
- 2.Gralnek IM, Hays RD, Kilbourne A, Naliboff B, Mayer EA. The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology. 2000;119(3):654–60. doi: 10.1053/gast.2000.16484. [DOI] [PubMed] [Google Scholar]
- 3.Frank L, Kleinman L, Rentz A, Ciesla G, Kim JJ, Zacker C. Health-related quality of life associated with irritable bowel syndrome: comparison with other chronic diseases. Clin Ther. 2002;24(4):675–89. doi: 10.1016/s0149-2918(02)85143-8. [DOI] [PubMed] [Google Scholar]
- 4.Lea R, Whorwell PJ. Quality of life in irritable bowel syndrome. Pharmacoeconomics. 2001;19(6):643–53. doi: 10.2165/00019053-200119060-00003. [DOI] [PubMed] [Google Scholar]
- 5.Mousavinasab SM, Gorganinezhad-Moshiri M, Saberifirouzi M, Dehbozorgi G, Mehrabani D. Personality characteristics and irritable bowel syndrome in Shiraz, southern Iran. Saudi J Gastroenterol. 2007;13(4):168–71. doi: 10.4103/1319-3767.36746. [DOI] [PubMed] [Google Scholar]
- 6.Pedersen SS, Denollet J. Type D personality, cardiac events, and impaired quality of life: a review. Eur J Cardiovasc Prev Rehabil. 2003;10(4):241–8. doi: 10.1097/00149831-200308000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Bagherian Sararoodi R. Type D personality. Journal of Research in Behavioural Sciences. 2009;7(1):75–87. [Google Scholar]
- 8.Denollet J. DS14: standard assessment of negative affectivity, social inhibition, and Type D personality. Psychosom Med. 2005;67(1):89–97. doi: 10.1097/01.psy.0000149256.81953.49. [DOI] [PubMed] [Google Scholar]
- 9.Sher L. Type D personality: the heart, stress, and cortisol. QJM. 2005;98(5):323–9. doi: 10.1093/qjmed/hci064. [DOI] [PubMed] [Google Scholar]
- 10.Mols F, Denollet J. Type D personality in the general population: a systematic review of health status, mechanisms of disease, and work-related problems. Health Qual Life Outcomes. 2010;8:9. doi: 10.1186/1477-7525-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Denollet J, Vaes J, Brutsaert DL. Inadequate response to treatment in coronary heart disease: adverse effects of type D personality and younger age on 5-year prognosis and quality of life. Circulation. 2000;102(6):630–5. doi: 10.1161/01.cir.102.6.630. [DOI] [PubMed] [Google Scholar]
- 12.Hansel SL, Umar SB, Lunsford TN, Harris LA, Dibaise JK, Crowell MD. Personality traits and impaired health-related quality of life in patients with functional gastrointestinal disorders. Clin Gastroenterol Hepatol. 2010;8(2):220–2. doi: 10.1016/j.cgh.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 13.Drossman DA, Dumitrascu DL. Rome III: New standard for functional gastrointestinal disorders. J Gastrointestin Liver Dis. 2006;15(3):237–41. [PubMed] [Google Scholar]
- 14.Bagherian R, Bahrami Ehsan H. Psychometric Properties of The Persian Version of Type D scale (DS14) Among MI Patients. Iran J Psychiatr Behav Sci. (In Press) [PMC free article] [PubMed] [Google Scholar]
- 15.Drossman DA, Patrick DL, Whitehead WE, Toner BB, Diamant NE, Hu Y, et al. Further validation of the IBSQOL: a disease-specific quality-of-life questionnaire. Am J Gastroenterol. 2000;95(4):999–1007. doi: 10.1111/j.1572-0241.2000.01941.x. [DOI] [PubMed] [Google Scholar]
- 16.Haghayegh A, Kalantari M, Solati Dehkordi K, Molavi H, Adibi P. Study on Validity of Farsi Version of Irritable Bowel Syndrome Quality of Life Questionnaire (IBS-QOL-34) Govaresh Journal. 2008;13(2):99–105. [Google Scholar]
- 17.Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther. 1997;11(2):395–402. doi: 10.1046/j.1365-2036.1997.142318000.x. [DOI] [PubMed] [Google Scholar]
- 18.El Serag HB, Olden K, Bjorkman D. Health-related quality of life among persons with irritable bowel syndrome: a systematic review. Aliment Pharmacol Ther. 2002;16(6):1171–85. doi: 10.1046/j.1365-2036.2002.01290.x. [DOI] [PubMed] [Google Scholar]
- 19.Frank L, Kleinman L, Rentz A, Ciesla G, Kim JJ, Zacker C. Health-related quality of life associated with irritable bowel syndrome: comparison with other chronic diseases. Clin Ther. 2002;24(4):675–89. doi: 10.1016/s0149-2918(02)85143-8. [DOI] [PubMed] [Google Scholar]
- 20.Mols F, Denollet J. Type D personality among noncardiovascular patient populations: a systematic review. Gen Hosp Psychiatry. 2010;32(1):66–72. doi: 10.1016/j.genhosppsych.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 21.Bartels H, Pedersen SS, Van der Laan BF, Staal MJ, Albers FW, Middel B. The impact of Type D personality on health-related quality of life in tinnitus patients is mainly mediated by anxiety and depression. Otol Neurotol. 2010;31(1):11–8. doi: 10.1097/MAO.0b013e3181bc3dd1. [DOI] [PubMed] [Google Scholar]
- 22.Brostrom A, Stromberg A, Martensson J, Ulander M, Harder L, Svanborg E. Association of Type D personality to perceived side effects and adherence in CPAP-treated patients with OSAS. J Sleep Res. 2007;16(4):439–47. doi: 10.1111/j.1365-2869.2007.00620.x. [DOI] [PubMed] [Google Scholar]
- 23.Simson U, Nawarotzky U, Porck W, Friese G, Schottenfeld-Naor Y, Hahn S, et al. [Depression, anxiety, quality of life and type D pattern among inpatients suffering from diabetic foot syndrome] Psychother Psychosom Med Psychol. 2008;58(2):44–50. doi: 10.1055/s-2007-971001. [DOI] [PubMed] [Google Scholar]
- 24.Barnett MD, Ledoux T, Garcini LM, Baker J. Type D personality and chronic pain: construct and concurrent validity of the DS14. J Clin Psychol Med Settings. 209;14(2):194–9. doi: 10.1007/s10880-009-9152-0. [DOI] [PubMed] [Google Scholar]
- 25.Mols F, Holterhues C, Nijsten T, Van De Poll-Franse LV. Personality is associated with health status and impact of cancer among melanoma survivors. Eur J Cancer. 2010;46(3):573–80. doi: 10.1016/j.ejca.2009.09.016. [DOI] [PubMed] [Google Scholar]
- 26.Valck CF, Denollet J, Wuyts FL, Van De Heyning PH. Increased handicap in vertigo patients with a type-D personality. Audiological Medicine. 2007;5(3):169–75. [Google Scholar]
- 27.Chapman BP, Duberstein PR, Lyness JM. The Distressed personality type: replicability and general health associations. European Journal of Personality. 2007;21(7):911–29. [Google Scholar]
- 28.Tanum L, Malt UF. Personality and physical symptoms in nonpsychiatric patients with functional gastrointestinal disorder. J Psychosom Res. 2001;50(3):139–46. doi: 10.1016/s0022-3999(00)00219-1. [DOI] [PubMed] [Google Scholar]
- 29.Pereira DB, Antoni MH, Danielson A, Simon T, Efantis-Potter J, OSullivan MJ. Inhibited interpersonal coping style predicts poorer adherence to scheduled clinic visits in human immunodeficiency virus infected women at risk for cervical cancer. Ann Behav Med. 2004;28(3):195–202. doi: 10.1207/s15324796abm2803_8. [DOI] [PubMed] [Google Scholar]
- 30.Kirkcaldy BD, Shephard RJ, Siefen RG. The relationship between physical activity and self-image and problem behaviour among adolescents. Soc Psychiatry Psychiatr Epidemiol. 2002;37(11):544–50. doi: 10.1007/s00127-002-0554-7. [DOI] [PubMed] [Google Scholar]
- 31.Farndale R, Roberts L. Long-term impact of irritable bowel syndrome: a qualitative study. Prim Health Care Res Dev. 2011;12(1):52–67. doi: 10.1017/S1463423610000095. [DOI] [PubMed] [Google Scholar]
- 32.Walter S, Hjortswang H, Holmgren K, Hallbook O. Association between bowel symptoms, symptom severity, and quality of life in Swedish patients with fecal incontinence. Scand J Gastroenterol. 2011;46(1):6–12. doi: 10.3109/00365521.2010.513059. [DOI] [PubMed] [Google Scholar]


