Abstract
BACKGROUND:
A novel version of the Modified Child Dental Anxiety Scale (MCDAS) was developed by addition of faces rating scale to the original numeric form. The aim of this prospective descriptive study was to perform a transcultural adaptation and reliability analysis of the Iranian version of Faces version of Modified Child Dental Anxiety Scale (MCDASf) and the Dental Subscale of the Children's Fear Survey Schedule (CFSS-DS).
METHODS:
To determine the test–retest reliability, 200 school-children aged 8–12 years completed the MCDASf and the CFSS-DS on two separate occasions, 2 weeks apart. To determine the criterion validity, all participants completed two questionnaires at the same sitting. The translated instrument was tested for internal consistency by Cronbach's alpha, inter-item, and item-total correlation coefficients. Correlation between the MCDASf and CFSS-DS mean scores and age were calculated using the Pearson correlation coefficient.
RESULTS:
The intraclass correlation coefficients ranged from 0.158 to 0.658 (P < 0.01) for the individual items of the MCDASf between the first and the second assessments and also, ranged from 0.350 to 0.677 (P < 0.01) for CFSS-DS. The internal consistencies (Cronbach's alpha) were 0.85 and 0.92 for the MCDASf and CFSS-DS, respectively. The correlation between the MCDASf and CFSS-DS was 0.73 (P < 0.001). The MCDASf and the CFSS-DS scores at the first administration were significantly greater than those of the second.
CONCLUSIONS:
The MCDASf is a reliable measure of dental anxiety in Iranian children aged 8–12 years, suggestive of good reliability and validity.
KEYWORDS: Transcultural Adaptation, MCDASf, Childhood Dental Fear, Iran, CFSS-DS
Dental fear in children has persisted to produce numerous interests in pediatric dentistry. This is owing to the management of associated complications. For example, it causes stress for many dentists who should manage such children particularly those who have associated behavioral problems. Additionally, the chair time needed to manage these children is lengthy and some specialized training is also required in successful management of these children.1 Nevertheless, to efficiently manage this problem, it is essential to determine its prevalence in a population to facilitate scheduling of public health services.
On the other hand, tools are required to assist diagnosing its presence and the severity in individuals to help modify individual treatment. At last, there is also a need for tools which can measure treatment required and successes of management. This would be facilitated with monitoring and assessing treatment outcomes.
A variety of measures have been developed in a proposition to develop a standardized method of evaluating and grading dental fear in children. Many of these measures quantify dental fear by measuring, scoring and summarizing the results. The development of a measure that can document the incidence, help in identifying treatment needs and precedence and help in monitoring and assessment of treatment outcomes would be ideal.
This is for the reason that such a measure would help in ensuring standardization in treatment planning and help in assessment of various results. The Modified Child Dental Anxiety Scale (MCDAS)2 consists of eight questions to evaluate dental anxiety about specific dental procedures.
The scale incorporates a question about local anaesthetic, and other dental procedures that possibly will distress children, such as extraction, dental general anaesthesia (DGA), and relative analgesia (RA).3 Total scores on the MCDAS ranged from 5 (little or no dental anxiety) to 40 (extreme dental anxiety).
The MCDAS has been utilized in 8- to 15-year olds and has been revealed to be a rational measure of child dental anxiety demonstrating good internal consistency and validity.4,5,6 Normative data exist for both English4 and Greek–Cypriot schoolchildren.5
The Dental Subscale of the Children's Fear Survey Schedule (CFSS-DS) was developed to evaluate dental fear in children.7,8 The CFSS-DS consists of 15 items to be answered on a 5-point scale ranging from 1 (not afraid at all) to 5 (very afraid) related to not only different features of dental treatment like invasive dental procedures as injections and drilling, but also to more general medical aspects. Total scores accordingly ranged from 15 to 75 and a score of 38 or more has been associated with clinical dental fear.7,9,10
This CFSS-DS has been extensively used in recent researches and has been signified to be a valuable and adequate measure of dental fear in children. Studies in several countries showed the scale to have good reliability and validity.11–16
A numeric rating scale is generally understood by children who have good cognitive functioning; conversely, under the potentially anxiety-provoking environment of the dental situation, the child may go back and show lower level of their cognitive capability.17
With a decrease in cognitive functioning, the MCDAS may not be easy for the regressed child to comprehend. An additional drawback of self-report measures with a numeric rating scale is their incongruity in the evaluation of dental anxiety in the very young ones.
To overcome these potential difficulties, a pictographic version of the MCDAS (the MCDASf) (Figure 1) was developed for the use in 7-9-year-old children, replacing pictorial response cards for the original response scale.18
Limited information is available for the reliability and validity of the pictorial modification of the MCDASf and the CFSS-DS. Also, there is no Iranian version of the MCDASf and the CFSS-DS available in the literature. Consequently, the purpose of the present study was to perform a transcultural adaptation and reliability analysis of the Iranian version of the MCDASf and the CFSS-DS to produce a reliable instrument that can be used for both clinical and research objects in the future.
Methods
The study was performed between October 2008 and September 2009 in 200 schoolchildren after obtaining approval from the Ethics Committee of the University. Before entering the research, each parent and child received written information explaining the study design and confirming that contribution was voluntary. Written consent from both parent and child was obtained for inclusion.
To be enrolled in the study, the subjects had to be 8-12 years and native Iranian speakers. The most important object in the translation/adaptation process was to maintain the clarity, objectivity, and straightforwardness of the questionnaire. In this process, some terminology was modified, rendering the questionnaire more comprehensible.
In this way, scales used in different cultures to that of the original version thus undertaking a precise process of translation, transcultural adaptation, and validation. The translation/adaptation process followed the guidelines of the International Quality of Life assessment (IQOLA) Project.19
Starting with the original English version, two independent translations into Iranian language were carried out by two different translators. These Iranian versions were subsequently back-translated by another two independent translators. Two of the translators were native English speakers and two were native Iranian speakers. Consequently, the two versions were compared and a final version was developed by agreement of the entire working group.
During the transcultural adaptation of the MCDASf and the CFSS-DS, only minor cultural adaptations were required. The children were informed that the MCDASf and the CFSS-DS were a computer package planned to measure how children feel about going to the dentist. At least one researcher and one teacher were present when the children were completing the measures. The items on the paper measures were read aloud to, and completed, in a class/group.
To evaluate the test-retest reliability, the MCDASf and CFSS-DS were completed by participants on two separate occasions, 2 weeks apart. The age and gender of the participants was recorded on all questionnaires, which were finalized under standardized conditions. To examine the criterion validity of the MCDASf and CFSS-DS, all participants completed two questionnaires at the same sitting.
The age and gender of the participants were recorded on all questionnaires, which were completed under standardized situations. Data from all school children who had completed the MCDASf and CFSS-DS on one occasion in the test-retest or criterion validity study were used to give normative data for a child population.
Concordance between Iranian and back-translated versions of the MCDASf and CFSS-DS along with test–retest reliability of the Iranian version was determined by the intraclass correlation coefficient (ICC).20 The translated instrument was tested for internal consistency by Cronbach's alpha, inter-item, and item-total correlation coefficients.21 Correlation between the MCDASf and CFSS-DS mean scores and age were calculated using the Pearson correlation coefficient. In addition, comparisons between the MCDASf and CFSS-DS total mean scores for genders were performed using Student t-test. Differences with P values less than 0.05 were regarded as statistically significant. Analyses were carried out with SPSS version 17.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
Two hundred schoolchildren aged 8–12 years with a mean age of 9.82 (95% CI: 9.61-10.04; median: 10, SD = 1.54), who had completed the MCDASf and CFSS-DS on two separate occasions were included in the statistical analysis. Of 200 patients enrolled in the study, 98 (49%) were female. No participant was excluded.
MDASf and CFSS-DS scores for all participants and for males and females separately, at the first and the second administrations are shown in Table 1. CFSS-DS at the first and the second administrations were significantly higher in females (P < 0.05, Table 1).
Table 1.
Faces version of the Modified Dental Anxiety Scale (MDASf) Scores and Dental Subscale of the Children's Fear Survey Schedule (CFSS-DS) at first and second administration of participants in the study
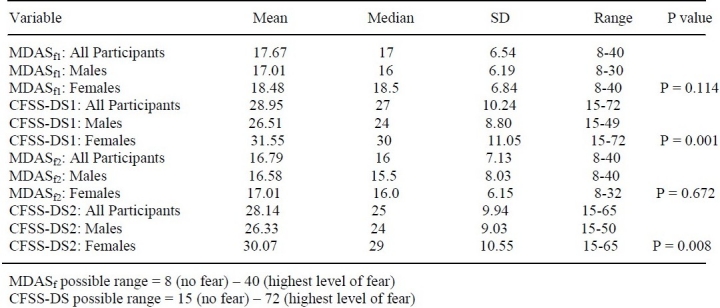
MDASf and CFSS-DS scores across different age groups, at the first and the second administrations are shown in Table 2. The MCDASf score at the first administration (mean: 17.67, 95% CI: 16.76, 18.59; median: 17, SD: 6.54) was significantly greater than that of the second (mean: 16.79, 95% CI: 15.79, 17.79, median: 16, SD: 7.13) (t= 2.15, P = 0.033).
The CFSS-DS score at the first administration (mean: 28.95, 95% CI: 27.52, 30.39, median: 27, SD: 10.24) was not significantly different from that of the second (mean: 28.14, 95% CI: 26.75, 29.53, median: 25, SD: 9.94) (t= 1.68, P = 0.095).
The intraclass correlation coefficients ranged from 0.158 to 0.658 (P < 0.01) for the individual items of the MCDASf between the first and the second assessments and from 0.350 to 0.677 (P < 0.01) for CFSS-DS.
The intraclass correlation coefficient for the mean overall score for the MCDASf was 0.641 (P < 0.001) between the first and the second assessments and 0.770 (P < 0.001) for the CFSS-DS.
The internal consistencies (Cronbach's alpha) were 0.85 and 0.92 for the MCDASf and CFSS-DS, respectively. The correlation between the MCDASf and CFSS-DS was 0.73 (P < 0.001).
The correlations between MCDASf and CFSS-DS and for males and females separately are shown in Table 3. These correlations ranged from 0.644 to 0.809, and were significant at P < 0.001.
Correlations between the MCDASf and CFSS-DS for the different age levels separately are shown in Table 4. These correlations ranged from 0.611 to 0.918, and were significant at P < 0.001.
Discussion
In our study, we found good evidence for the internal consistencies and test-retest reliabilities of the Iranian translations of both MCDASf and CFSS-DS. Accordingly, it seems that the Iranian versions of these measures operate in comparable manners to the same degree they have in other languages.
Even though there was a significant decrease in the MCDASf scores between the first and the second administrations of the questionnaire, this was possible to have been caused by a decrease in the experimental state anxiety of the participants as they would have been more familiar with the MCDASf at the second administration.
A satisfactory level of internal consistency of the MCDASf was shown, with a Cronbach's alpha of 0.85. This corresponded to the homogeneity of the scale indicating that all items on the scale used a similar paradigm. An acceptable Cronbach's alpha is regarded as greater than 0.70, but not greater than 0.9014. The internal consistency of the MCDASf was comparable to that of the CFSS-DS which has been reported as 0.92.
The MCDASf was consequently noticed to be a reliable measure of child dental anxiety, which revealed good test-retest reliability and good internal consistency. As expected, there was a high correlation between the MCDASf and the ‘gold standard’ measure of the child dental anxiety inventory, the CFSS-DS,13 with the MCDASf explaining over 73% of the CFSS-DS score variance.
The MCDASf has the advantage of being shorter and consequently faster to complete than the 15-item CFSS-DS. It was expected that those children with a higher level of obvious decay experience would be more dentally anxious than those with a lower level of obvious decay experience.
Bedi and colleagues22 showed that adolescents with high dental anxiety had a significantly higher DMFT than their contemporaries with low dental anxiety. This finding has been substantiated for younger children, as dentally anxious 5-year-olds were found to have had significantly more caries than non-dentally anxious children.23
Dental extractions, sedation and DGA are deemed to be the most traumatic treatment interferences, and consequently it was expected that those children with DGA experience would be more dentally anxious, substantiating the findings of Milsom and colleagues23 who described increased dental anxiety in 5-year-old children with DGA experience.
When applied to younger children, standard self-report measures have been customized by the addition of picture response scales or moveable barometers;24,25 in the present study, the MCDAS was modified by face picture response scale. These were selected owing to the clarity of the images and their correspondence with the descriptors of the interval of the five-point numeric format.
The MCDASf was completed by children as young as 8 years in a clinical setting. To help the younger children, the nurse read the questions while the children pointed to the appropriate face on the scale to show their anxiety. Older children completed the scale without help. The MCDASf was completed by children aged 8-12 years in a school setting.
We found that Iranian girls scored significantly higher on both fear measures, compared with boys, which has been commonly reported in other studies of dental fear.26 Vassiliou et al.27 showed that Greek women were more anxious in general, compared with Greek men, which was consistent with another investigation on gender differences in anxiety.28
The results of our study showed that dentists working with Iranian populations can expect females to have higher levels of dental fear, compared with males. The MCDASf would seem to be valid and reliable as well as practical in the evaluation of dental anxiety in a wide age range of children attending dental clinics.
It is concluded that the MCDASf may be used with certainty to evaluate dental anxiety in children. The MCDASf is a reliable measure of dental anxiety in children aged 8–12 years, signifying good reliability and validity. This implies that dentists and researchers working with Iranian-speaking populations may use either or both measures to evaluate levels of dental fear. The tendency for dentists to rate Iranian females as being more anxious all through dental treatment, compared with males, may be consistent with our results that Iranian females have significantly higher levels of dental fear.
Authors’ Contributions
SHJ carried out the design of the study and preparation of the manuscript. MM contributed in data gathering and preparation of the manuscript .ZF was responsible for data analysis and interpretation of results. All authors have read and approved the content of the manuscript.
Footnotes
Conflict of Interests Authors have no conflict of interests.
References
- 1.Folayan MO, Idehen E. Factors influencing the use of behavioral management techniques during child management by dentists. J Clin Pediatr Dent. 2004;28(2):155–61. doi: 10.17796/jcpd.28.2.18w2v457t8878p69. [DOI] [PubMed] [Google Scholar]
- 2.Wong HM, Humphris GM, Lee GT. Preliminary validation and reliability of the Modified Child Dental Anxiety Scale. Psychol Rep. 1998;83(3 Pt 2):1179–86. doi: 10.2466/pr0.1998.83.3f.1179. [DOI] [PubMed] [Google Scholar]
- 3.Humphris GM, Mair L, Lee GTR, Birch H. Dental anxiety, pain and uncooperative behaviour in child dental patients. Anxiety, Stress & Coping: An International Journal. 1991;4(1):61–77. [Google Scholar]
- 4.Christophorou S, Lee GTR, Humphris GH. The reliability and validity of the Modified Child Dental Anxiety Scale: a study of Greek Cypriot school children. Eur J Paediatr Dent. 2000;1:75–81. [Google Scholar]
- 5.Buchanan H. Development of a computerised dental anxiety scale for children: validation and reliability. Br Dent J. 2005;199(6):359–62. doi: 10.1038/sj.bdj.4812694. [DOI] [PubMed] [Google Scholar]
- 6.Cuthbert MI, Melamed BG. A screening device: children at risk for dental fears and management problems. ASDC J Dent Child. 1982;49(6):432–6. [PubMed] [Google Scholar]
- 7.Scherer MW, Nakamura CY. A fear survey schedule for children (FSS-FC): a factor analytic comparison with manifest anxiety (CMAS) Behav Res Ther. 1968;6(2):173–82. doi: 10.1016/0005-7967(68)90004-1. [DOI] [PubMed] [Google Scholar]
- 8.Klingman A, Melamed BG, Cuthbert MI, Hermecz DA. Effects of participant modeling on information acquisition and skill utilization. J Consult Clin Psychol. 1984;52(3):414–22. doi: 10.1037//0022-006x.52.3.414. [DOI] [PubMed] [Google Scholar]
- 9.Klingberg G, Berggren U, Noren JG. Dental fear in an urban Swedish child population: prevalence and concomitant factors. Community Dent Health. 1994;11(4):208–14. [PubMed] [Google Scholar]
- 10.Alvesalo I, Murtomaa H, Milgrom P, Honkanen A, Karjalainen M, Tay KM. The Dental Fear Survey Schedule: a study with Finnish children. Int J Paediatr Dent. 1993;3(4):193–8. doi: 10.1111/j.1365-263x.1993.tb00083.x. [DOI] [PubMed] [Google Scholar]
- 11.Klingberg G. Reliability and validity of the Swedish version of the Dental Subscale of the Children's Fear Survey Schedule, CFSS-DS. Acta Odontol Scand. 1994;52(4):255–6. doi: 10.3109/00016359409029055. [DOI] [PubMed] [Google Scholar]
- 12.Aartman IH, van ET, Hoogstraten J, Schuurs AH. Self-report measurements of dental anxiety and fear in children: a critical assessment. ASDC J Dent Child. 1998;65(4):252–30. [PubMed] [Google Scholar]
- 13.Klingberg G, Berggren U, Carlsson SG, Noren JG. Child dental fear: cause-related factors and clinical effects. Eur J Oral Sci. 1995;103(6):405–12. doi: 10.1111/j.1600-0722.1995.tb01865.x. [DOI] [PubMed] [Google Scholar]
- 14.Melamed BG, Yurcheson R, Fleece EL, Hutcherson S, Hawes R. Effects of film modeling on the reduction of anxiety-related behaviors in individuals varying in level of previous experience in the stress situation. J Consult Clin Psychol. 1978;46(6):1357–67. doi: 10.1037//0022-006x.46.6.1357. [DOI] [PubMed] [Google Scholar]
- 15.Milgrom P, Jie Z, Yang Z, Tay KM. Cross-cultural validity of a parent's version of the Dental Fear Survey Schedule for children in Chinese. Behav Res Ther. 1994;32(1):131–5. doi: 10.1016/0005-7967(94)90094-9. [DOI] [PubMed] [Google Scholar]
- 16.Freud A. Normality and Pathology in Childhood: Assessments of Development 1965. Madison CT: International Universities Press; 1974. p. 198. [Google Scholar]
- 17.Wright FA, Lucas JO, McMurray NE. Dental anxiety in five-to-nine-year-old children. J Pedod. 1980;4(2):99–115. [PubMed] [Google Scholar]
- 18.Gandek B, Ware JE., Jr Methods for validating and norming translations of health status questionnaires: the IQOLA Project approach. International Quality of Life Assessment. J Clin Epidemiol. 1998;51(11):953–9. doi: 10.1016/s0895-4356(98)00086-9. [DOI] [PubMed] [Google Scholar]
- 19.Bartko JJ, Carpenter WT., Jr On the methods and theory of reliability. J Nerv Ment Dis. 1976;163(5):307–17. doi: 10.1097/00005053-197611000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334. [Google Scholar]
- 21.Bedi R, Sutcliffe P, Donnan P, Barrett N, McConnachie J. Dental caries experience and prevalence of children afraid of dental treatment. Community Dent Oral Epidemiol. 1992;20(6):368–71. doi: 10.1111/j.1600-0528.1992.tb00701.x. [DOI] [PubMed] [Google Scholar]
- 22.Milsom KM, Tickle M, Humphris GM, Blinkhorn AS. The relationship between anxiety and dental treatment experience in 5-year-old children. Br Dent J. 2003;194(9):503–6. doi: 10.1038/sj.bdj.4810070. [DOI] [PubMed] [Google Scholar]
- 23.Milgrom P, Mancl L, King B, Weinstein P. Origins of childhood dental fear. Behav Res Ther. 1995;33(3):313–9. doi: 10.1016/0005-7967(94)00042-i. [DOI] [PubMed] [Google Scholar]
- 24.Weinstein P, Getz T, Milgrom P. Treating Fearful Dental Patients: A Patient Management Handbook. 2nd ed. Washington: University of Washington; 1995. [Google Scholar]
- 25.Vassiliou V, Georgas JG, Vassiliou G. Variations in manifest anxiety due to sex, age, and education. J Pers Soc Psychol. 1967;6(2):194–7. doi: 10.1037/h0024572. [DOI] [PubMed] [Google Scholar]
- 26.Feingold A. Gender differences in personality: a meta-analysis. Psychol Bull. 1994;116(3):429–56. doi: 10.1037/0033-2909.116.3.429. [DOI] [PubMed] [Google Scholar]


