Abstract
BACKGROUND:
The aim of this study was to evaluate epidemiological relationship between chronic obstructive pulmonary disease and sleep apnea syndrome in a sample of Persian population.
METHODS:
As a part of a population-based cross-sectional study, 3900 randomly selected individuals aged 15 years or older were invited to take part in the survey; 3770 individuals (96.6%) agreed to fill out the respiratory and sleep questionnaire. Those subjects suspected to have either chronic obstructive pulmonary disease and/or obstructive sleep apnea underwent spirometry and polysomnography test if indicated. Spirometric measurements were performed on 420 invited responders. Polysomnography measurements were performed on 25 of the responders.
RESULTS:
Prevalence rates for sleep apnea, chronic obstructive pulmonary disease and current asthma were 4.98%, 5.7% and 3.1%, respectively. Logistic regression showed independent associations between sleep apnea and chronic obstructive pulmonary disease. There was no significant independent association between sleep apnea symptoms and current asthma and wheeze ever.
CONCLUSIONS:
These observations indicated relationship between chronic obstructive pulmonary disease and obstructive sleep apnea. These observations indicated the necessity of further studies to explain the possible common pathogenic mechanisms involved in two disease entities.
KEYWORDS: Chronic Obstructive Pulmonary Disease, Sleep Apnea Syndrome, Iran
Asthma is one of most common chronic diseases which affects as many as 300 million people worldwide,1 a number that in the absence of new preventive measures might increase up to 400 million by the year 2025.1
Chronic obstructive pulmonary disease (COPD) is recognized as the fourth major killer disease in the united states2 and most of the developed countries,3 and a leading cause of mortality and morbidity all over the world.4
Obstructive sleep apnea (OSA) is a disorder with a high prevalence characterized by instability of the upper airways during sleep, which results in markedly reduced (hypopnea) or absent (apnea) airflow at the nose/mouth.5
The combination of COPD and OSA was named overlap syndrome (OS).6 Some studies evaluating large nonelected groups of patients with OSA suggested that COPD is more frequent among patients with OSA than in the general population.7–9 But, it was not confirmed with other studies.10
A high prevalence of OSA has been reported in asthma clinics,11 and asthma may also be common in OSA.12 Whether COPD is related to OSA has not yet been clarified. We hypothesized that OSA is more frequent in COPD. The purpose of this study was to detect the possible association between obstructive pulmonary disease and sleep apnea in a large sample of randomly selected subjects.
Methods
A cross-sectional study was carried out in 2009–2010 on a randomly selected sample of adults aged 15 years and over. The review board for medical ethics of the Isfahan University of Medical Sciences approved the study and methods. All participants gave their informed written consents.
We used a two-step approach for the survey. In the first step, the Isfahan city area was divided into 100 areas. Then, we randomly selected one lane from each area, by drawing lots, and all the doors of the living places of the selected lanes were knocked and all inhabitants 15 years of age or older were invited to take part in interview and complete the questionnaire.
The questionnaire included two parts. The first part included detailed history of obstructive pulmonary diseases which was taken with special emphasis on symptoms of COPD or asthma. Diagnosis of chronic obstructive pulmonary disease was based on European Respiratory Society (ERS) guidelines.13 The second part consisted of the Berlin questionnaire that is well known worldwide and has been adopted and used in previous studies in Iran.14 The completed questionnaires were reviewed by one pulmonologist, and any subject who admitted to have current asthma, wheeze ever and chronic bronchitis were invited for pulmonary function tests (PFT). The measurement of spirometry were conducted with a commercially available system (MS-IOS; Masterlab-IOS, Erich Jaeger, Germany), which has been described elsewhere, and fulfilled standard recommendations.15
And subjects who were high risk for sleep apnea by Berlin questionnaire were invited for full night polysomnography.
Polysomnography was done in sleep lab using the Somnomedic (Germany) system. The PSG consisted of 14 channel continuous polygraphic recording from surface leads for 2 electroencephalography, 2 electro-oculography, chin electromyography, electrocardiography, sensors for nasal airflow (thermistor), tracheal sounds (microphone), thoracic and abdominal respiratory effort (piezo-electric), finger pulse oximeter, leg movements, body position and light. Apnea was defined as the cessation of airflow at the nostrils and mouth for more than 10 s. Hypopnea was defined as a reduction in oronasal air- flow by at least 30% for 10 s or more accompanied by at least 4% fall from the baseline oxygen saturation (SaO2).
Apnea–hypopnea index (AHI) was defined as the total number of apnea and hypopnea events per hour of sleep and was calculated during total sleep time.
All of the measurements were made by one trained technician. The output report of each subject was scrutinized qualitatively by one pulmonary physician (B.A.) before inclusion for statistical analysis.
Definitions
-
(1)
High risk for sleep apnea based on Berlin sleep questionnaire categories.14
-
(2)
Asthma ever was defined as any history of dyspnea attacks combined with wheezy breathing any time in life.4
-
(3)
Current asthma was defined as any history of dyspnea attacks combined with wheezy breathing in the last 12 months.4
-
(4)
Chronic bronchitis was defined as productive cough for more than three consecutive months in at least two consecutive years in the absence of any known etiology.4
-
(5)
Obstructive spirometry was applied to those with FEV1/FVC ratios of less than 70%.4
-
(6)
OSAS was diagnosed in patients who had an AHI> 5.5
Statistical analysis
Statistical analysis was performed using SPSS software version 15.0 (SPSS, Inc. Chicago, IL). The data were expressed as frequency number and percent. Those variables with initially significant effect (P<0:05) where selected for logistic regression analysis and, Odds ratios and 95% confidence intervals (CIs) were calculated and recorded.
Results
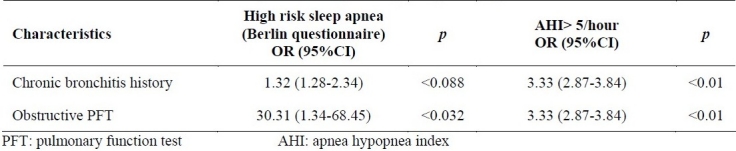
The actual adult population of the selected 100 lanes was 3900 of whom 3,770 subjects (96.6%) agreed to take part in the study. The population consisted of 2002 females (53.1%) and 1768 males (46.8%) aged 15–92 years. The study population age groups and smoking status are presented in Table 1. Around half of the population was younger than 40 years. 298 (7.9%) of population were smoker. Population disease condition and participation for PFT and PSG are presented in Table 2. The prevalence of wheeze ever, current asthma and chronic bronchitis in the whole group was 6.8 %, 3.1% and 5.7%, respectively Table 2. Using multiple regression analysis, current asthma and wheeze ever, lost their significance and were excluded from results. Chronic bronchitis history and obstructive pulmonary function test had significant association with high risk for sleep apnea and positive polysomnography study which are presented in Table 3.
Table 1.
Population age groups and smoking condition
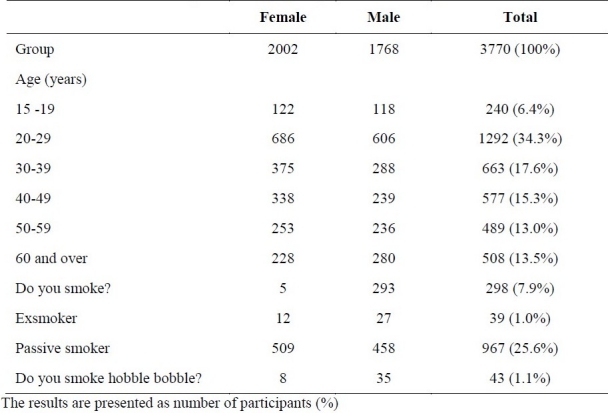
Table 2.
Population disease condition and participation for PFT and PSG
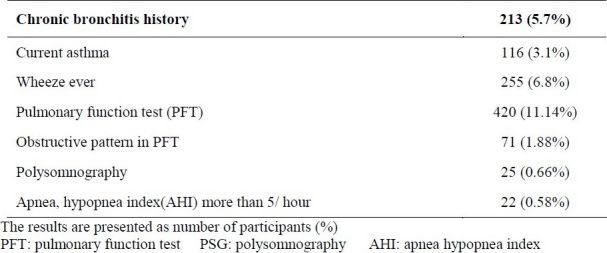
Table 3.
Predictors of risk of high risk Berlin questionnaires and AHI> 5/hour using multiple logistic regressions.
Discussion
The main finding of our study was that in a large randomly selected group of an Isfahan population, prevalence of COPD in the high risk group of sleep apnea by Berlin questionnaire was more than that in the rest of the studied population. We also have shown that COPD diagnosed by pulmonary function test, and sleep apnea syndrome diagnosed by polysomnography occurred more frequently together than expected and that the condition s were independently associated with each other. In this cross sectional study, we have shown that obstructive sleep apnea was not more frequent in patients with asthma. Our study was based on a random sample of population more than 15 years old in Isfahan-Iran. The methodology used in this study was robust. Sampling was accurately random, the overall response was good at 96.6% but female sex preponderance might indicate lower participation rates for men. Some previous studies have reported a higher prevalence of snoring among asthmatic patients compared with non-asthmatic patients16 and some other had reported high prevalence of asthma in patients with OSA.12
But, in our study no significant correlation was found between OSA and current asthma or wheeze ever. In a recently published study, authors stated that OSA appeared to be common in patients with COPD or asthma in an urban outpatient pulmonary clinic. But, they said that the high prevalence of OSA in OAD patients appeared to be due to obesity, and reduced pulmonary function was not an independent risk factor for OSA.17 But, in our study we found that sleep apnea syndrome was more frequent in patients with obstructive pulmonary function test.
The available data have shown conflicting results also for COPD, with one study showing an association between COPD and OSA,18 while another study in COPD patients showed that COPD in subjects with OSAS was as frequent as that in the general population.19
Our study has shown that patients with COPD had around 3 times more sleep apnea by polysomnography. In agreement with us, one published study from primary care clinic in Greece stated that COPD patients are twice as likely as others to present sleepiness symptoms.18
Another study observed significant differences in both quantity and quality of sleep between patients with stable mild to moderate chronic obstructive pulmonary disease and respective controls.20 Our study had potential limitations. First of all, due to very low response rate for polysomnographic study, less than half of the group studied underwent full PSG. Second, most of our data were derived based on the questionnaire results. In conclusion, in these preliminary results, our data suggested that there was direct relation between OSA and COPD; and COPD and OSA may mechanistically be linked.
This could be proved with further ongoing studies with more polysomnographic and spirometric measurements. We recommended screening of OSA in COPD patients.
Authors’ Contributions
BA, IF, TP, TW and MG designed the study. BA, MG gathered the data. MG analyzed data. All authors read and approved the final manuscript.
Footnotes
Conflict of Interests Authors have no conflict of interests.
References
- 1.Desalu OO, Desalu OO, Oluboyo PO. Self reported risk factors of asthma in a Nigerian.adult population. Tur Toraks Der. 2009;10:56–62. [Google Scholar]
- 2.Sullivan SD, Ramsey SD, Lee TA. The economic burden of COPD. Chest. 2000;117(2 Suppl):5S–9S. doi: 10.1378/chest.117.2_suppl.5s. [DOI] [PubMed] [Google Scholar]
- 3.Halbert RJ, Natoli JL, Gano A, Badamgarav E, Buist AS, Mannino DM. Global burden of COPD: systematic review and meta-analysis. Eur Respir J. 2006;28(3):523–32. doi: 10.1183/09031936.06.00124605. [DOI] [PubMed] [Google Scholar]
- 4.Melville AM, Pless-Mulloli T, Afolabi OA, Stenton SC. COPD prevalence and its association with occupational exposures in a general population. Eur Respir J. 2010;36(3):488–93. doi: 10.1183/09031936.00038309. [DOI] [PubMed] [Google Scholar]
- 5.McNicholas WT. Diagnosis of obstructive sleep apnea in adults. Proc Am Thorac Soc. 2008;5(2):154–60. doi: 10.1513/pats.200708-118MG. [DOI] [PubMed] [Google Scholar]
- 6.Flenley DC. Sleep in chronic obstructive lung disease. Clin Chest Med. 1985;6(4):651–61. [PubMed] [Google Scholar]
- 7.Larsson LG, Lindberg A, Franklin KA, Lundback B. Obstructive sleep apnoea syndrome is common in subjects with chronic bronchitis. Report from the Obstructive Lung Disease in Northern Sweden studies. Respiration. 2001;68(3):250–5. doi: 10.1159/000050506. [DOI] [PubMed] [Google Scholar]
- 8.Guilleminault C, Cummiskey J, Motta J. Chronic obstructive airflow disease and sleep studies. Am Rev Respir Dis. 1980;122(3):397–406. doi: 10.1164/arrd.1980.122.3.397. [DOI] [PubMed] [Google Scholar]
- 9.Chaouat A, Weitzenblum E, Krieger J, Ifoundza T, Oswald M, Kessler R. Association of chronic obstructive pulmonary disease and sleep apnea syndrome. Am J Respir Crit Care Med. 1995;151(1):82–6. doi: 10.1164/ajrccm.151.1.7812577. [DOI] [PubMed] [Google Scholar]
- 10.Zamarron C, Garcia P V, Morete E, del Campo MF. Association of chronic obstructive pulmonary disease and obstructive sleep apnea consequences. Int J Chron Obstruct Pulmon Dis. 2008;3(4):671–82. doi: 10.2147/copd.s4950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Auckley D, Moallem M, Shaman Z, Mustafa M. Findings of a Berlin Questionnaire survey: comparison between patients seen in an asthma clinic versus internal medicine clinic. Sleep Med. 2008;9(5):494–9. doi: 10.1016/j.sleep.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 12.Alharbi M, Almutairi A, Alotaibi D, Alotaibi A, Shaikh S, Bahammam AS. The prevalence of asthma in patients with obstructive sleep apnoea. Prim Care Respir J. 2009;18(4):328–30. doi: 10.4104/pcrj.2009.00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siafakas NM, Vermeire P, Pride NB, Paoletti P, Gibson J, Howard P, et al. Optimal assessment and management of chronic obstructive pulmonary disease (COPD).The European Respiratory Society Task Force. Eur Respir J. 1995;8(8):1398–420. doi: 10.1183/09031936.95.08081398. [DOI] [PubMed] [Google Scholar]
- 14.Amra B, Farajzadegan Z, Golshan M, Fietze I, Penzel T. Prevalence of sleep apnea-related symptoms in a Persian population. Sleep Breath. 2010 doi: 10.1007/s11325-010-0353-4. [In Press] [DOI] [PubMed] [Google Scholar]
- 15.Golshan M, Nematbakhsh M, Amra B, Crapo RO. Spirometric reference values in a large Middle Eastern population. Eur Respir J. 2003;22(3):529–34. doi: 10.1183/09031936.03.00003603. [DOI] [PubMed] [Google Scholar]
- 16.Ekici A, Ekici M, Kurtipek E, Keles H, Kara T, Tunckol M, et al. Association of asthma-related symptoms with snoring and apnea and effect on health-related quality of life. Chest. 2005;128(5):3358–63. doi: 10.1378/chest.128.5.3358. [DOI] [PubMed] [Google Scholar]
- 17.Sharma B, Feinsilver S, Owens RL, Malhotra A, McSharry D, Karbowitz S. Obstructive airway disease and obstructive sleep apnea: effect of pulmonary function. Lung. 2011;189(1):37–41. doi: 10.1007/s00408-010-9270-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karachaliou F, Kostikas K, Pastaka C, Bagiatis V, Gourgoulianis KI. Prevalence of sleep-related symptoms in a primary care population - their relation to asthma and COPD. Prim Care Respir J. 2007;16(4):222–8. doi: 10.3132/pcrj.2007.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bednarek M, Plywaczewski R, Jonczak L, Zielinski J. There is no relationship between chronic obstructive pulmonary disease and obstructive sleep apnea syndrome: a population study. Respiration. 2005;72(2):142–9. doi: 10.1159/000084044. [DOI] [PubMed] [Google Scholar]
- 20.Valipour A, Lavie P, Lothaller H, Mikulic I, Burghuber OC. Sleep profile and symptoms of sleep disorders in patients with stable mild to moderate chronic obstructive pulmonary disease. Sleep Med. 2011;12(4):367–72. doi: 10.1016/j.sleep.2010.08.017. [DOI] [PubMed] [Google Scholar]


