Abstract
Glomus tumours are rare, benign tumours of the glomus body, most frequently located in the subungual region of digits, palms and soles, but they have been reported throughout the body. Our patient is a 65-year-old man who presented with a 3-year history of a very painful area on his left upper arm. The overlying skin was normal and there was no lesion to palpate, but the symptoms were very striking, warranting further investigation. An exploratory operation identified a prominent vein with a noticeable bulge in the vessel wall. The vein was ligated and excised. On dissection of the vein, a tumour was present within its lumen. Histological examination and immune profile of the tumour confirmed an intravascular glomus tumour. Following surgical excision, symptoms resolved.
Background
The neuromyoarterial glomus body is an arteriovenous anastamosis thought to be involved with temperature regulation.1–3 Glomus tumours are benign tumours of the glomus body,1 most frequently located in the subungual region of digits, palms and soles, but they have been reported throughout the body.1 2 Glomus tumours are uncommon, accounting for about 2% of soft tissue tumours.1 2 The first case of an intravascular glomus tumour was described in 1991.4 Since then there have been a small number of other cases reported in the literature.5 6
Case presentation
Our patient presented with a 3-year history of a very painful localised area on his left upper arm. Over the preceding 6 months he had experienced shooting pains, which he described as ‘like being stabbed’. These lasted several seconds before subsiding and he had 2–3 attacks per day. His history included rheumatoid arthritis, for which he took methotrexate, requiring monitoring blood tests. The tourniquet was situated directly over the painful spot, and it was this that drew his attention to the problem. The overlying skin was entirely normal and there was no lesion to palpate, but the symptoms were very striking, warranting further investigation.
Investigations
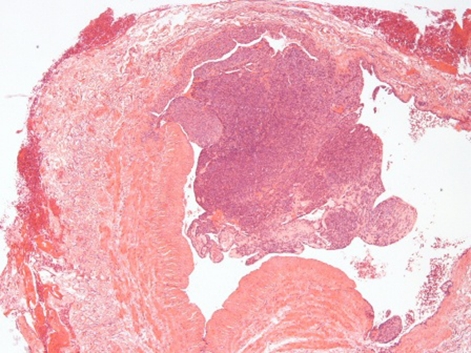
An exploratory operation was carried out. The skin was unremarkable, but a prominent vein was identified, with a noticeable bulge in the vessel wall. The vein was ligated and excised. On dissection of the vein, a tumour was present within its lumen. Histological examination of the tumour showed a lesion composed of small vessels with normal endothelium, surrounded by uniformly round small cells (figure 1). These possessed eosinophilic cytoplasm and central, regular nuclei. There was no cytonuclear atypia, and no mitotic figures were present. Focal extension of the lesion into the wall of the vein was also identified.
Figure 1.
Intravascular lesion composed of glomus cells. These extend into the vessel wall (H&E, original magnification x40).
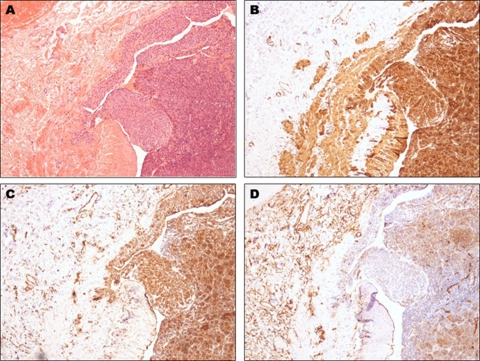
Immunohistochemistry was performed. The tumour cells showed positive staining with smooth muscle actin, vimentin and CD34 (figure 2). They did not stain with S100, MNF-116 or CD31. Reticulin and elastic Van Gieson stains highlighted the involvement of the vein wall described.
Figure 2.
(A) Figure 1 at x100 magnification. (B) Smooth muscle actin staining both the glomus cells and the smooth muscle of the vessel walls (original magnification x100). (C) Strong vimentin staining of the glomus cells (original magnification x100). (D) Patchy CD34 staining of the glomus cells with background staining of endothelial cells and interstitial dermal dendritic cells (original magnification x100).
Both the histological appearance and immunoprofile of the lesion were those of a glomus tumour, in this instance located intravascularly.
Differential diagnosis
The differential diagnosis of painful skin lesions includes: eccrine spiradenoma, neurilemmoma, leiomyoma, angiolipoma and neuroma. As the surface of the skin was normal, the cause of the pain was most likely due to pathology in deeper structures as identified during the minor operation.
Treatment
The intravascular glomus tumour was excised completely during the exploratory operation and no further treatment was required.
Outcome and follow-up
Following surgical excision, our patient’s symptoms resolved with no recurrence of the lesion.
Discussion
Glomus tumours can be solitary or multiple, the latter are more often hereditary and occur more frequently in children.3 They typically present as a red or purple subcutaneous nodule, most often on the upper limbs and demonstrate an equal sex distribution.1 They are composed of glomus cells, vascular endothelial cells and smooth muscle cells and a number of different histological types have been described.1 Classically they present with pain, localised tenderness and hypersensitivity to cold.2 Twenty to thirty per cent of patients report previous trauma to the area before onset of symptoms.2 In this case, the patient was having regular blood tests for methotrexate monitoring and the site of the tumour lay beneath the area regularly compressed by the tourniquet.
Previous reports of intravascular glomus tumour have postulated several mechanisms to explain this phenomenon. These include extension into the vessel lumen from outside, differentiation of mesenchymal cells of the vessel wall into smooth muscle-like glomus tumour cells, or tumour growth from glomus cells already present in the wall of the vein.4 Previous cases are summarised in table 1.
Table 1.
Previous case reports of intravascular glomus tumours, adapted from Acebo et al6
| Intravascular glomus tumours | |||
|---|---|---|---|
| Authors | Patient age/sex | Site | Size |
| Chen and Ma7 | 61-year-old female | Right ankle | 1.0 cm |
| Beham and Fletcher4 | 40-year-old male | Right forearm | 0.7 cm |
| Googe and Griffin5 | 66-year-old male | Left forearm | 1.5 cm |
| Acebo et al6 | 79-year-old female | Right forearm | 14 cm |
| Present report | 65-year-old male | Left upper arm | 0.6 cm |
| Glomus tumours with intravascular extension | |||
| Haque et al8 | 75-year-old male | Stomach | Widespread subendothelial extension and focal intravascular nodule formation |
| Michal9 | 48-year-old male | Right foot, dorsum | 2.5 cm |
| Slater et al10 | 37-year-old male | Left thigh | 4.6 cm |
Glomus tumours rarely exhibit a malignant potential. Intravascular growth is not thought to suggest aggressive behaviour or increased risk of malignancy. Treatment of glomus tumours is with surgical excision.1 Local recurrence is possible if resection is incomplete.1
Learning points.
-
▶
Glomus tumours are rare, benign tumours of the glomus body, most frequently located in the subungual region of digits, palms and soles.
-
▶
Glomus tumours are one of the causes of painful skin lesions.
-
▶
Only a small number of intravascular glomus tumours have been reported in the literature.
-
▶
The possibility of an intravascular glomus tumour should be considered if the diagnosis is suspected and nothing is found on initial exploration.
-
▶
The mechanism for intravascular growth is unknown, but may be due to extension into the vessel lumen from outside, differentiation of mesenchymal cells of the vessel wall into smooth muscle-like glomus tumour cells, or tumour growth from glomus cells already present in the wall of the vein.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Gombos Z, Zhang PJ. Glomus tumor. Arch Pathol Lab Med 2008;132:1448–52 [DOI] [PubMed] [Google Scholar]
- 2.Schiefer TK, Parker WL, Anakwenze OA, et al. Extradigital glomus tumors: a 20-year experience. Mayo Clin Proc 2006;81:1337–44 [DOI] [PubMed] [Google Scholar]
- 3.Heys SD, Brittenden J, Atkinson P, et al. Glomus tumour: an analysis of 43 patients and review of the literature. Br J Surg 1992;79:345–7 [DOI] [PubMed] [Google Scholar]
- 4.Beham A, Fletcher CD. Intravascular glomus tumour: a previously undescribed phenomenon. Virchows Arch A Pathol Anat Histopathol 1991;418:175–7 [DOI] [PubMed] [Google Scholar]
- 5.Googe PB, Griffin WC. Intravenous glomus tumor of the forearm. J Cutan Pathol 1993;20:359–63 [DOI] [PubMed] [Google Scholar]
- 6.Acebo E, Val-Bernal JF, Arce F. Giant intravenous glomus tumor. J Cutan Pathol 1997;24:384–9 [DOI] [PubMed] [Google Scholar]
- 7.Chen KT, Ma CK. Intravenous leiomyoblastoma. Am J Surg Pathol 1983;7:591–6 [DOI] [PubMed] [Google Scholar]
- 8.Haque S, Modlin IM, West AB. Multiple glomus tumors of the stomach with intravascular spread. Am J Surg Pathol 1992;16:291–9 [DOI] [PubMed] [Google Scholar]
- 9.Michal M. Glomus tumour with intravascular spread. Cesk Patol 1993;29:144–6 [PubMed] [Google Scholar]
- 10.Slater DN, Cotton DW, Azzopardi JG. Oncocytic glomus tumour: a new variant. Histopathology 1987;11:523–31 [DOI] [PubMed] [Google Scholar]