Abstract
Objective:
The aim was to evaluate the effect of honey dressing and silver sulfadiazene (SSD) dressing on wound healing in burn patients.
Materials and Methods:
We retrospectively reviewed the records of 108 patients (14–68 years of age), with first and second degree burns of less than 50% of the total body surface area admitted to our institution, over a period of 5 years (2004–2008). Fifty-one patients were treated with honey dressings and 57 with SSD. Time elapsed since burn, site, percentage, degree and depth of burns, results of culture sensitivity at various time intervals, duration of healing, formation of post-treatment hypertrophic scar, and/or contracture were recorded and analyzed.
Results:
The average duration of healing was 18.16 and 32.68 days for the honey and SSD group, respectively. Wounds of all patients reporting within 1 h of burns became sterile with the honey dressing in less than 7 days while there was none with SSD. All wounds treated with honey became sterile within 21 days while for SSD-treated wounds, this figure was 36.5%. A complete outcome was seen in 81% of all patients in the “honey group” while in only 37% patients in the “SSD group.”
Conclusion:
Honey dressings make the wounds sterile in less time, enhance healing, and have a better outcome in terms of hypertropic scars and postburn contractures, as compared to SSD dressings.
KEYWORDS: Burns, honey dressing, silver sulfadiazine dressing
INTRODUCTION
The exact number of burn cases is difficult to determine; however, in a country like India, with a population of over 1 billion, there are around 700,000–800,000 burn admissions per year.[1] Burn injuries to the skin result in loss of its protective function as a barrier to micro-organisms leading to the high risk of infection. Thus, burn patients face high morbidity than mortality because of the large uncovered burn surface getting infected, healing of which takes long periods of dressings, leading to deformities and contractures.[2] Unfortunately, the management of the burn wounds still remains a matter of debate and an ideal dressing for burn wounds has not been discovered.[2] Moreover, in developing countries, burn management is riddled with difficulties.
Various dressing materials have been used for dressing the burn wounds such as amniotic membrane, boiled potato peel, banana leaf, soframycin cream, silver sulfadiazene, skin grafting, epidermal growth factor, honey dressing, etc. Honey being cheap and easily available is a reasonably good dressing material in developing countries. The present study is aimed to compare the effect of the honey dressing and silver sulfadiazene (SSD) dressing on wound healing.
MATERIALS AND METHODS
The records of patients with burns who had been treated with either honey dressings or silver sulfadiazine dressings at our center over a period of 5 years (January 2004 to December 2008) were reviewed. Records of a total of 108 patients (complete records) of both sexes aged 14–68 years, with first and second degree burns, having a burned area less than 50% of the total body surface area (TBSA) were included. Patients who were in an immunocompromised state, any organ failure, and on chemotherapy were not included. For convenience and comparison, the patients were divided into two groups: “honey group” and “silver sulfadiazine (SSD) group.”
Apart from age/sex and usual patient data, time elapsed since burn to reach the hospital, and results of routine blood investigations and wound swab samples all were collected. Also, the results of the clinical assessment of the wounds done time to time in terms of site, affected surface area, degree, depth, presence or absence of slough, culture sensitivity every seventh day, any additional treatment, and the outcome were also noted.
Along with stabilization, in all the patients, intravenous or oral antibiotics were started as per hospital protocols. Wound swab samples were taken on admission and every seventh day from the time of admission. Antibiotics were changed appropriately according to the results of culture sensitivity. Antibiotics were given for minimum 5 days or after 48 hours of subsidence of fever. Wounds were examined carefully and washed with normal saline. Patients mentioned under the “honey group” were dressed with pure undiluted honey and those in the “SSD group” with SSD cream, everyday. After the application of the dressing material, we preferred to leave the burn area open. Patients were followed up every fortnight for initial 2 months, monthly for next 4 months, and once in 6 months thereafter.
We measured the final outcome, in terms of complete and incomplete recovery. Criteria for a complete recovery included complete healing without any scar or contracture. Formation of a soft scar, hypertrophic scar and/or contracture was labeled as an incomplete recovery.
RESULTS
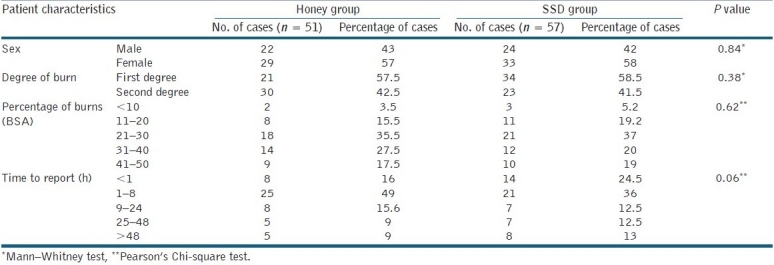
Patients’ characteristics and time elapsed after burns to reach the hospital are shown in Table 1. Out of a total of 108 patients, a majority (n = 36) reported within 1–8 h of burns. Sixty-five patients presented within first 24 h of burns [Table 1]. There were no significant differences among patients in both groups as far as patients’ characteristics were concerned except that more patients in the "honey group" presented within first 8 h.
Table 1.
Patients’ characteristics and time of reporting after burns
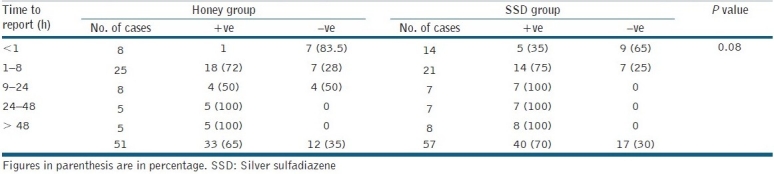
Only one patient in the “honey group,” among those who presented in less than 1 h of the burn, had his wound swab cultures positive at the time of admission, while the corresponding figure for the “SSD group” was 35%. Patients who came within 1–8 h following burns (83% and 75% in two groups, respectively) had wound swab cultures positive at the time of admission. All patients in both groups reporting after 24 h (100%) had wound swab cultures positive on admission [Table 2].
Table 2.
Time elapsed after burns and till reporting, and the “wound swab culture” at admission in both groups
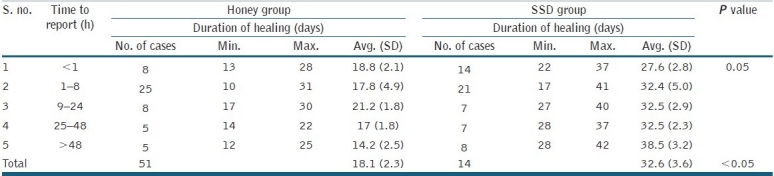
The average duration of wound healing among patients in the “honey group” coming within 1, 2–8, and 9–24 h, and more than 48 h was 18.8, 17.8, 21.25, and 14.25 days, respectively. Among patients in the “SSD group” average durations of healing were 27.6, 32.4, 32.5, 32.5, and 38.6 days for similar times of reporting [Table 3]. Thus average durations of healing of patients in the “honey group” (18.1 days, SD = 2.3) was significantly lower than that of patients in the “SSD group” (32.6 days, SD = 3.6, P < 0.05).
Table 3.
Time elapsed after burns till reporting, and “healing” with treatment
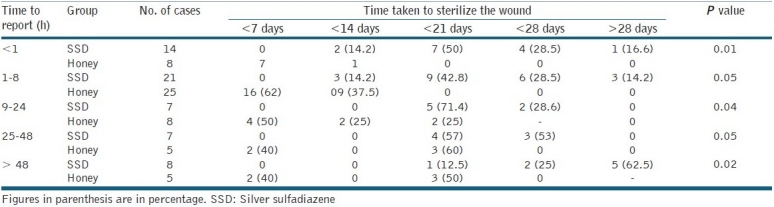
Among patients treated with honey dressings, wound swab cultures became negative in less than 7 days, in 62%, 50%, and 40% of the total number of patients reporting in 2–8, 9–24, and after 48 h, respectively [Table 4]. Among patients treated with SSD dressings, none of the patient's wound became sterile in less than 7 days. Wounds of half (50%) of the patients who presented within less than 1 h of burns became sterile in less than 21 days, those of 14% in less than 14 days, and of 16% in more than 28 days. Among patients who presented within 2–8 h, 28.5% had their wounds sterile in less than 28 days, 42.8% in less than 21 days, and 14.2% in more than 28 days. Among patients who presented after 48 h, 62.5% had their wounds sterile in more than 28 days, and 25% and 14.2% in less than 28 and 21 days, respectively [Table 4]. All these differences were significantly in favor of the honey dressing.
Table 4.
Sterilization of wounds of different reporting times achieved by honey and SSD
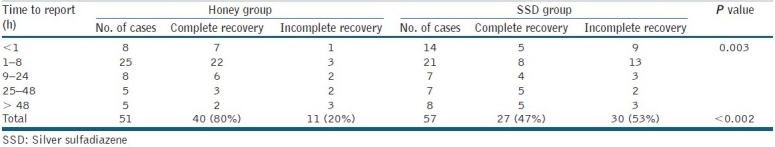
Among 41 patients treated with honey dressings who reported within 24 h, 32 patients (80%) had a complete recovery while 9 had incomplete. Two among these nine progressed to the third degree. Out of total 51 patient treated with honey dressings, 41 (81%) had a complete recovery. In the SSD group out of 42 patients presenting within 24 h, only 17 patients (45%) had a complete outcome, and out of total 57 patients, only 27 (47%) achieved a complete outcome. Three patients in the SSD group evolved to the third degree. These differences were statistically significant (P = 0.002 for 24 h, and P = 0.003 for 48 h results; [Table 5]).
Table 5.
Final outcome in the “honey group” and “SSD group” in relation to different times of reporting after burns
DISCUSSION
For at least 2700 years, honey has been used to treat a variety of ailments through topical application, but only recently its antiseptic and antibacterial properties have been chemically explained. The antibacterial activity of honey is mainly due to the presence of inhibines, which consist of hydrogen peroxide, flavonoids, phenolic acids, and many other unidentified substances.[3–5] Other features that impart antibacterial properties to honey are its low water activity causing osmosis[5] and high acidity.[6]
Although, Moore et al.,[7] through a review of previous randomized controlled trials comparing honey with other materials, concluded that the confidence in a conclusion that honey is a useful treatment for superficial wounds or burns is low, however, recently in 2004, Professor Peter Molan from New Zealand, based on his work at Honey Research Unit at the University of Waikato said that honey might be useful in treating methicillin-resistant Staphylococcus aureus (MRSA) infections.[8] The topical use of honey prevents the dressing from sticking to the healing wound, and may reduce odors, swelling, and scarring when used to treat wounds.[6]
Infection is one of the most frequent complications of wound healing despite the use of antibiotics and modern sterile techniques; it accounts for considerable patient morbidity, discomfort, and prolonged hospitalization and it must be avoided to permit proper healing.[9] Burn patients have great chances of infection due to the presence of necrotic tissue in the burn wounds. Delayed reporting has been found to be an important factor that causes an increase in wound infection and thus morbidity.[10] This is a major problem in the third world counties like India, owing to poor transport conditions, illiteracy, and distant tertiary health care centers. Delay and inadequate fluid resuscitation and overwhelming infection were the major factors in the morbidity and mortality.[11] Honey because of its antiseptic and antibacterial properties can thus be a useful dressing material in such regions.
In the presence of infection, healing becomes very slow or does not take place at all. The situation becomes worse as the antibiotics are ineffective in this setting, and antiseptics cause tissue damage, further slowing the wound healing. Honey on the other hand does not cause tissue damage, and appears to actually promote the healing process, decreasing the average duration of wound healing.[12] Patients treated with honey had a significantly lower average duration of wound healing than those who were treated with SSD [Table 3]. A similar type of result was found in the previous study done by Subrahmanyam.[13]
In the present study, among patients in the honey group, 100% of patients’ wounds who reported within 1 h of burns became sterile in less than 7 days. Those who reported within 2–8 and 9–24 h and more than 48 h of burn (62.5%, 50%, and 50%, respectively) had got their wounds sterile within 7 days [Table 4]. This observation is also comparable with another study done by Subrahmanyam.[14]
Honey also has a positive effect in reducing the oxidative stressful state in burn trauma that results in rapid wound healing.[15] On the other hand, although there is evidence of the antibacterial effect, there is no direct evidence of improved wound healing or reduced infection by SSD dressings in burn patients.[16] Subrahmanyam[13] noted sustained inflammatory reaction even on epithelialization in SSD-treated burn wounds, but the early subsidence of acute inflammatory changes, better control of infection, and quicker wound healing were seen in those treated with honey.[13]
From the present study, it is clear that the increase in the time elapsed after burn trauma and admission to the hospital has adverse effects on wound healing and complications at follow-up. SSD dressings have been found to be lesser effective in counteracting this when compared to honey.[14] Subrahmanyam[14] found better relief of pain and lower incidence of hypertrophic scars and postburn contractures with the honey dressing that, along with its low cost and easy availability, make it an ideal dressing in the treatment of burns.
CONCLUSION
The delay in hospital admission increases the wound infection, wound contamination, and time in wound sterilization and healing, and has a detrimental effect on the final outcome. Honey dressings improve wound healing, make wound sterile in lesser duration, and have better outcomes in terms of incidence of hypertrophic scars and postburn contractures when compared to SSD dressings.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Jaiswal AK, Aggarwal H, Solanki P, Lubana PS, Mathur RK, Odiya S. Epidemiological and socio-cultural study of burn patients in M.Y. Hospital, Indore, India. Indian J Plast Surg. 2007;40:158–63. [Google Scholar]
- 2.Subrahmanyam M. Honey dressing versus boiled potato peel in the treatment of burns: A prospective randomized study. Burns. 1996;22:491–3. doi: 10.1016/0305-4179(96)00007-1. [DOI] [PubMed] [Google Scholar]
- 3.Wahdan H. Causes of the antimicrobial activity of honey. Infection. 1998;26:26–31. doi: 10.1007/BF02768748. [DOI] [PubMed] [Google Scholar]
- 4.Schepartz AI, Subers MH. Catalase in Honey. J Apic Res. 1966;5:37–43. [Google Scholar]
- 5.Subrahmanyam M. Addition of antioxidant and polyethylene glycole 4000 enhances the healing property of honey in burns. Ann Burns Fire Disasters. 1996;9:93–5. [Google Scholar]
- 6.Waikato Honey Research Unit, University of Waikato, Hamilton, New Zealand. Honey as an Antimicrobial Agent. Available from: http://bio.waikato.ac.nz/honey/honey_intro.shtml .
- 7.Moore OA, Smith LA, Campbell F, Seers K, McQuay HJ, Moore RA. Systematic review of the use of honey as a wound dressing. BMC Complement Altern Med. 2001;1:2. doi: 10.1186/1472-6882-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Angie Knox. Harnessing honey's healing power. BBC– Excerpt from: http://news.bbc.co.uk/2/hi/3787867.stm .
- 9.Goldenheim PD. An appraisal of povidone-iodine and wound healing. Postgrad Med J. 1993;69:97–105. [PubMed] [Google Scholar]
- 10.Ozbek S, Ozgenel Y, Etoz A, Akin S, Kahveci R, Heper Y, et al. The effect of delayed admission in burn centers on wound contamination and infection rates. Ulus Travma Acil Cerrahi Derg. 2005;11:230–7. [PubMed] [Google Scholar]
- 11.Onuba O, Udoidiok E. Hospital management of massive burns in the developing countries. Burns Incl Therm Inj. 1987;13:386–90. doi: 10.1016/0305-4179(87)90129-x. [DOI] [PubMed] [Google Scholar]
- 12.Brånemark PI, Ekholm R, Albrektsson B, Lindstrom J, Lundborg G. Lundskog J.Tissue Injury caused by wound disinfectants. J Bone Joint Surg Am. 1967;49:48–62. [PubMed] [Google Scholar]
- 13.Subrahmanyam M. A prospective randomised clinical and histological study of superficial burn wound healing with honey and silver sulfadiazine. Burns. 1998;24:157–61. doi: 10.1016/s0305-4179(97)00113-7. [DOI] [PubMed] [Google Scholar]
- 14.Subrahmanyam M. Topical application of honey in treatment of burns. Br J Surg. 1991;78:497–8. doi: 10.1002/bjs.1800780435. [DOI] [PubMed] [Google Scholar]
- 15.Nagane NS, Ganu J V, Bhagwat VR, Subramanium M. Efficacy of topical honey therapy against silver sulphadiazine treatment in burns: A biochemical study. Indian J Clin Biochem. 2004;19:173–6. doi: 10.1007/BF02894280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hussain S, Ferguson C. Best evidence topic report. Silver sulphadiazine cream in burns. Emerg Med J. 2006;23:929–32. doi: 10.1136/emj.2006.043059. [DOI] [PMC free article] [PubMed] [Google Scholar]


