Abstract
Objective:
To determine the prevalence of diabetes mellitus (DM) and its associated diabetic complications in rural Goa, India.
Materials and Methods:
A community-based study was carried out in a rural setting in Goa, India. About 1,266 participants were selected by systematic random sampling. The participants were interviewed using a semi-structured questionnaire and were subjected to anthropometric, clinical evaluation and biochemical investigations. American Diabetes Association criteria were used to determine the prevalence of diabetes and standard operational definitions were used to define the diabetic complications. Data was analyzed using SPSS version 14.0 while chi-square and chi-square for trend were the tests used.
Results:
Among the total 1,266 study participants about 130 (10.3%) were diabetics. The prevalence of the associated diabetic complications were as follows viz. neuropathy (60%), CHD (32.3%) and cataract (20%), retinopathy (15.4%), peripheral vascular disease (11.5%) and cerebrovascular accidents (CVAs) (6.9%). A significant rising trend in the prevalence of all diabetic complications was observed with advancing duration of diabetes.
Conclusion:
The prevalence of DM and its associated complications was higher among the diabetic individuals in the rural setting of Goa, India. All the associated diabetic complications observed need to be addressed with appropriate prevention and control strategies.
Keywords: Diabetes Mellitus, rural, complications
Introduction
Diabetes mellitus (DM) is a major public health problem depicting a rising prevalence worldwide.(1) It is currently estimated that 190m people around the world suffer from DM, with over 330 million predicted to have the condition by 2025, and 366 million by the year 2030.(2,3) In fact, diabetes is a growing cause of disability and premature death, mainly through cardiovascular disease and other chronic complications.(4) A substantial body of evidence suggests that it could reach epidemic proportions particularly in developing and newly industrialized countries.(5)
In prediction, India along with China account for nearly a third of the estimated 300 million adult diabetics by the year 2025.(6) Recent surveys indicate that diabetes now affects a staggering 10-16% of urban population and 5-8% of rural population in India, while the actual epidemic is believed to be transpiring in the rural areas.(7,8) Indians are susceptible to premature onset of DM which in turn leads to rapid progression of chronic vascular complications, incurring heavy burden on health care systems in India.
The state of Goa, fairly known for its westernized culture, harbors most of the variables favorable for the development of diabetes and its complications. However, there is no community-based data on diabetes prevalence and its complications. Hence, this study was undertaken in an attempt to study the prevalence of DM and its associated complications in a rural setting in the state.
Materials and Methods
A community-based study was conducted in a rural setting having a population of 6,500 and catered to by Rural Health and Training centre in Goa, India. House to house survey was conducted to obtain a sampling frame of individuals. A sample of 1,266 individuals aged 20 years and above was selected by systematic random sampling. The minimum sample size required was calculated using the formula N = (1.96)2 pq/L2 wherein P = 12% and allowable error L = 15% of P based on pilot study findings. The study subjects were interviewed face-to-face using a semi-structured questionnaire for baseline demographic data and details related to diabetes and complications. This was followed by anthropometric, clinical and biochemical assessment.
DM was diagnosed by American Diabetes Association (ADA) criteria(9) as fasting plasma glucose ≥7mmol/l, done on two separate occasions or when the patients were on anti-diabetics proven as per medical records. Blood glucose estimation was done using the Folin-Wu method.
Minnesota criterion was used to define coronary heart disease (CHD).(10) Peripheral vascular disease (PVD)(11) was defined as presence of definite history of intermittent claudication or/if one or more of the peripheral pulses were absent on both the feet or/presence of an ulcer or amputation. Cerebrovascular accident (CVA) was defined as cases proven by medical and CT scan records. Diabetic neuropathy(12) was defined as a bilateral absence of ankle jerks and/or bilateral distal sensory loss or any other severe neurological deficit. Diabetic retinopathy(13) was defined based on fundoscopy findings.
Data was analyzed using SPSS version 14.0 and Chi-square test, χ2 - Trend used for analyzing the associations. Approval for the study was obtained from the institutional ethics committee and written informed consent was received from all study subjects.
Results
The present study selected an overall of 1,266 individuals aged 20 years and above to participate in the study. Among them 609 were males and 657 were females respectively. Among the total participants, 130 (10.3%) subjects had DM with females (12%) showing a significantly higher prevalence compared to males (8.4%) (P = 0.032). Around 60% (79/130) were old cases while, 39.2% (51/130) were newly detected in the study area.
The prevalence of associated diabetic complications is shown in Table 1. Among the diabetics, the prevalence of CHD, peripheral vascular disease, CVA, retinopathy, cataract and neuropathy were 32.3%, 11.5%, 6.9%, 15.4%, 20% and 60% respectively. The various complications were found to be significantly associated with DM. The prevalence of CHD (32.3%] was higher among the diabetics compared to non-diabetics (3.3%). Diabetics were fourteen times [P= 0.0001, OR= 14.18; 95% CI: 8.42-23.89) more likely to have CHD than the non-diabetics. The difference was found to be statistically significant.
Table 1.
Prevalence of associated complications among diabetics and non-diabetics
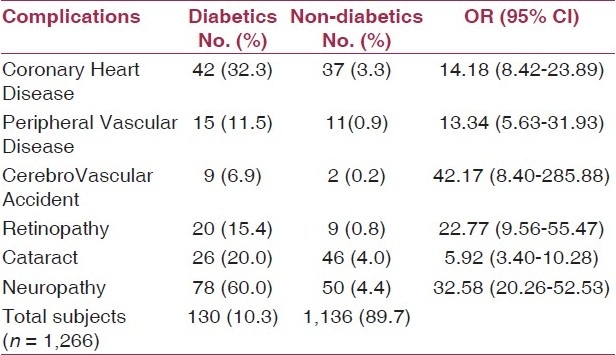
PVD prevalence was significantly higher [15/130] (11.5%) among diabetics and among these about two (2/15) (13.3%) were amputated and four (26.7%) were having an ulcer. Diabetics carried a 13 times more risk of suffering from PVD than non-diabetics (OR= 13.34; 95% CI: 5.63-31.93). CVA prevalence was 6.9% and diabetics were 42 times more likely to acquire strokes and TIA's than non-diabetics (OR = 42.17; 95% CI: 8.40-285.88).
Diabetic retinopathy and cataract prevalence was 15.4% and 20% respectively. Diabetic incurred a 22 times higher chance of having retinopathy (OR = 22.77; 95% CI: 9.56-55.47) and were six times more likely to have cataract [OR= 5.92; 95% CI: 3.40-10.28] compared to non-diabetics. Sixty percent of diabetics showed peripheral neuropathy compared to non-diabetics (4.4%) and the occurrence of neuropathy was 32 times more among diabetics (OR = 32.58; 95% CI: 20.26-52.53).
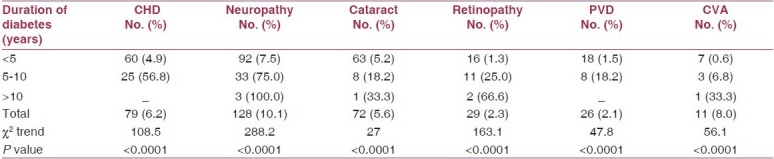
The various diabetic complications prevalence in relation to duration of DM is shown in Table 2. The prevalence of diabetic complications in relation to duration of diabetes when studied showed a rising trend. A statistically significant association was observed between the various complications and duration of DM.
Table 2.
Duration of DM and prevalence of associated complications
Discussion
A significantly higher prevalence (10.3%) was observed in rural Goa, India compared to other similar studies in India. Applying ADA criterion in rural setting of Maharashtra, Sudha et al(14) (2006) studied a similar high prevalence of 8.9% .Yet in another rural area of India in the year 2004, Yagnik CS et al(15) reported a prevalence of 6.3%. A rising prevalence rate from 11 to 17% was studied in Pakistani rural population.(16) Also in another diabetic prevalence study conducted in Malaysia over 10 years period showed a rise in prevalence rate from 3.9 to 12.2%.(17)
The present study showed a significant association between prevalence of complications and DM. The common complications among the diabetics were neuropathy (60%), CHD (32.3%) and cataract (20%) while the other significant complications included retinopathy (15.4%), PVD (11.5%) and CVA (6.9%).
In a South India, a similar high prevalence of CHD (30.3%) among the diabetics was revealed by Ramachandran et al.(18) Yet in another study Ramachandran et al(19) reported a prevalence of 0.9% and 61.9% for stroke and neuropathy respectively among the diabetes subjects while the prevalence of PVD was 4.1%. Around 17.2% of diabetics had cataract as a complication in a study (Mohan V et al) carried out in Southern India.(20) Rema M et al(21) reported a retinopathy prevalence of 34.1% among diabetics, in South India. A rising trend in the prevalence of associated diabetic complications with advancing years of DM was found in our study. Ramachandran et al(18) in their study on prevalence of vascular complications of type 2 diabetes in an urban set up also observed a similar upsurge in trend in the prevalence of diabetic complications with increasing duration of DM. Persons having diabetes for more than ten years were comparatively less in number in the study population which could be either due to ‘survivor’ bias or reflection of a lower prevalence of DM a decade earlier.
Conclusion
The prevalence of DM and its associated complications was higher among the diabetic individuals in the rural setting of Goa, India. All the diabetic complications observed need to be addressed in prevention and control strategies in the study area. Also, community awareness programmes need to be implemented to percolate the knowledge about the diabetic complications, the available screening facilities for their early detection, treatment and care in the rural population.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Lusignan S, Sismanidis C, Carey IM, DeWilde S, Richards N, Cook DG. Trends in the prevalence and management of diagnosed type 2 diabetes 1994-2001 in England and Wales. BMC Fam Pract. 2005;6:13. doi: 10.1186/1471-2296-6-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Azizi F, Guoya MM, Vazirian P, Dolatshati P, Habbibian S. Screening for type 2 diabetes in the Iranian national programme:a preliminary report. East Mediterr Health J. 2003;9:1122–7. [PubMed] [Google Scholar]
- 3.Hussain A, Vaaler S, Sayeed MA, Mahtab H, Ali SM, Khan AK. Type 2 diabetes and impaired fasting blood glucose in rural Bangladesh: a population-based study. Eur J Public Health. 2007;17:291–6. doi: 10.1093/eurpub/ckl235. [DOI] [PubMed] [Google Scholar]
- 4.Gan D, editor. 2nd ed. Brussels belgium: International Diabetes Federation; 2003. International Diabetes Federation: Diabetes Atlas. [Google Scholar]
- 5.King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes care. 1998;21:1414–31. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 6.Fall CH. Non-industrialised countries and affluence. Br Med Bull. 2001;60:33–50. doi: 10.1093/bmb/60.1.33. [DOI] [PubMed] [Google Scholar]
- 7.Wild S, Roglic Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 8.Pradeepa R, Mohan V. The changing scenario of the diabetes epidemic: implications for India. Indian J Med Res. 2002;116:121–32. [PubMed] [Google Scholar]
- 9.American Diabetes Association. Standards of medical care in diabetes--2006. Diabetes care. 2006;29(Suppl 1):S4–42. [PubMed] [Google Scholar]
- 10.Prineas RJ, Crow RS, Blackburn H. Bristol: John Wright; 1982. The Minnesota manual of electrographic findings. John Wright. [Google Scholar]
- 11.Fernandez BB., Jr A rational approach to diagnosis and treatment of intermittent claudication. Am J Med Sci. 2002;323:244–51. doi: 10.1097/00000441-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Dyck PJ. Severity and staging of Diabetic neuropathy. In: Gries F A, Cameron N E, Low P A, Ziegler D, editors. Textbook of Diabetic neuropathy. New York: Thieme; 2003. pp. 170–75. [Google Scholar]
- 13.Diabetic retinopathy study. Report Number 6. Design, methods, and baseline results. Report Number 7. A modification of the Airlie House classification of diabetic retinopathy. Prepared by the Diabetic Retinopathy. Invest Ophthalmol Vis Sci. 1981;21:1–226. [PubMed] [Google Scholar]
- 14.Deo SS, Zantye A, Mokal R, Mithbawkar S, Rane S, Thakur K. To identify the risk factors for high prevalence of diabetes and impaired glucose tolerance in Indian rural population. Int J Diabetes Dev Ctries. 2006;26:19–23. [Google Scholar]
- 15.Yagnik CS. Early life origin of insulin resistance and type 2 diabetes in India and other Asian countries. Nutrition. 2004;134:205–10. doi: 10.1093/jn/134.1.205. [DOI] [PubMed] [Google Scholar]
- 16.Shera AS, Rafique G, Khwaja IA, Ara J, Bagai S, King H. Pakistan national diabetes survey: prevalence of glucose intolerance and associated factors in Shikarpur, Sindh Province. Diabetes Med. 1995;12:1116–21. doi: 10.1111/j.1464-5491.1995.tb00430.x. [DOI] [PubMed] [Google Scholar]
- 17.Ali O, Tan TT, Sakinah O, Khalid BA, Wu LL, Ng ML. Prevalence of NIDDM and impaired glucose tolerance in aborigines and Malays in Malaysia and their relationship to sociodemographic, health, and nutritional factors. Diabetes Care. 1993;16:68–75. doi: 10.2337/diacare.16.1.68. [DOI] [PubMed] [Google Scholar]
- 18.Ramachandran A, Snehalatha C, Vijay V, King H. Impact of poverty on the prevalence of diabetes and its complications in urban southern India. Diabet Med. 2002;19:130–5. doi: 10.1046/j.1464-5491.2002.00656.x. [DOI] [PubMed] [Google Scholar]
- 19.Ramachandran A, Snehalatha C. Burden of type 2 diabetes and its complications-Indian scenario. Diab Research. 2002;83:1471–6. [Google Scholar]
- 20.Mohan V, Premlatha G, Sastry NG. Peripheral vascular disease in non-insulin-dependent diabetes mellitus in south India. Diabetes Res Clin Pract. 1995;27:235–40. doi: 10.1016/0168-8227(95)01048-i. [DOI] [PubMed] [Google Scholar]
- 21.Rema M, Ponnaiya M, Mohan V. Prevalence of retinopathy in non insulin dependent diabetes mellitus at a diabetes centre in southern India. Diabetes Res Clin Pract. 1996;34:29–36. doi: 10.1016/s0168-8227(96)01327-7. [DOI] [PubMed] [Google Scholar]


