Abstract
Background:
We present the outcomes of a survey conducted in Nandurbar, a tribal district of Maharashtra, India. It was based on “Rapid Assessment for Avoidable Blindness” methodology and conducted in 2009 in Nandurbar, a tribal district of Maharashtra, India.
Materials and Methods:
We examined persons of 50 years and older ages. Ophthalmic assistants noted the distant vision [best corrected vision (BCV) and as presented]. Ophthalmologist examined eyes of persons with vision less than 6/18. The principal cause of impairment in each eye and the most “preventable” or “treatable” cause were assigned. We calculated the prevalence rates of bilateral blindness, severe visual impairment (SVI), and moderate visual impairment (MVI).
Result:
We examined 2,005/2,300 persons (response rate 87.2%). The prevalence of blindness, SVI, and MVI for the BCV was 1.63% (95% CI 1.11–2.15), 5.93% (95% CI 4.96–6.90), and 14.6% (95% CI 13.2–16.1), respectively. The prevalence of blindness, SVI, and MVI for the presented vision was 1.87% (1.32–2.42), 6.72% (95% CI 5.70–7.74), and 19% (95% CI 17.4–20.6), respectively. Unoperated cataract was responsible for 77% of different visual disabilities. The coverage of existing cataract surgery service was 9.4%. Lack of knowledge about cataract surgery was the main cause of unoperated cataract among 41% of interviewed participants with cataract and SVI.
Conclusion:
Unoperated cataract was the main curable cause of visual disabilities in tribal population of India. Increasing awareness and offering cataract surgeries at affordable cost in the district would reduce visual disabilities.
Keywords: Blindness, cataract, low vision, prevalence, VISION 2020, visual disability
Introduction
Tribal people are the most marginalized sections of the Indian society. Eight to ten percent population of India (80–100 million) stay in tribal areas. Barriers such as accessibility, awareness, affordability, and accountability affect eye care services in such areas.[1] The magnitude of visual disabilities and unattended curable eye conditions are therefore high among the tribal population. To reach the goals of VISION 2020, this underprivileged population should be given due care.[2] Information on the magnitude and determinants of visual disabilities in tribal areas will therefore be crucial for better and effective planning and monitoring of VISION 2020—India. As Rapid Assessment for Avoidable Blindness (RAAB) was carried out in 16 states in the country in 2006–2007, it is not a new tool and could safely be used for reviewing the magnitude of visual disabilities among tribal population.[3] Epidemiologically community-based survey would be more acceptable method of generating information on the prevalence of visual disabilities at district levels. To our knowledge, no such information is available in Nadurbar district of Maharashtra. Interestingly, experts of World Health Organization had concluded that there seems to be a 25% decline in the prevalence of blindness in India between 1971 and 2000.[4] But the trends in district levels in these surveys showed wide variations. It was as low as 1.6% in Kodagu district and as high as 7.24% in Tumkur district of Karnataka.[5]
Nandurbar district has a large tribal population. It is at the intersection of Gujarat, Maharashtra, and Madhya Pradesh states. Due to difficult terrain, people are unable to easily access the static units of all three states. The cataract surgery rate (CSR) of less than 400 in this district during a survey in 2006–2007 in contrast to 24,000 per million Indian population of 50 years and older ages in 2001 India confirms presence of these barriers.[4,6]
We conducted a cross-sectional survey to determine the magnitude and causes of blindness and low vision in the Nandurbar district. This would help estimating cataract blind and suggest public health measures to address avoidable blindness.
Materials and Methods
The ethical and research committee of H V Desai Eye Hospital and Nandurbar District Health Administration approved this study. We offer eye care services at “no profit no loss” motto in this eye hospital and it is also a training center for the postgraduate ophthalmology and mid-level eye care professionals. It also has a community ophthalmology wing to serve the rural Maharashtra. Informed verbal consent was obtained from all eligible individuals, in the presence of a local witness. This survey was conducted between July and September 2009.
The tribal population of the district Nandurbar was 1,311,709. Fifty years and older people were targeted for this survey. This was a cross-sectional type of study. A stratified and cluster random sampling method was used for the survey. The district sample was stratified according to the percentage proportion of population in each taluka. To calculate the sample with 95% confidence, acceptable range of the prevalence of blindness as 4.4% to 6.6%, cluster size 40, design effect 1.4, and noncompliance 10%; 2,300 persons in 46 clusters were enrolled in this study.[5]
A cluster constituted a population segment of 1,000 people of all ages. Villages with smaller populations were clubbed together. The villages with larger populations were segmented so that they get more opportunity for selection. Because 13.7% of the Indian population is aged 50 years or older, a cluster would yield 110 to 130 people*. Of the 1,312 clusters in the district, 64 clusters (50 villages and 14 urban zones) were randomly selected. We identified a random starting point in a cluster. One street was randomly picked up by the local leaders to identify the direction in which the enumeration team should proceed. The first occupied house on the right side of the street was identified as the starting point for household visit.
We enumerated and examined the first 40 people aged 50 years and more and residing in these houses. A modified “Early Treatment Diabetic Retinopathy Study” (ETDRS) chart with five “E”s corresponding to the 6/18 on one side and another 5 “Es” corresponding to the 6/60 cut-off on the reverse side was used. This chart was placed in shaded day light and at a distance of six meters the participant was seated. Ophthalmic assistants who were trained in the survey methodology conducted the vision tests. An individual who could not identify four out of five “E”s of the 6/18 optotype was sent to make shift ophthalmic clinic in the cluster. In this clinic, ophthalmologist examined persons with impaired vision. Vision of each eye was retested. If a person was using spectacles for viewing objects at distance, his/her vision was noted as presenting vision. All individuals with presenting vision less than 6/18 in any eye had their vision recorded with a pinhole to determine the best-corrected vision [BCV]. If an individual could not read the 6/60 optotype from a distance of 6 m, the vision was retested at 3 m distance. To examine the posterior segment of eye, we dilated the pupils using 10% phenylephrine eye drops. Once possible causes of visual impairment were listed, the ophthalmologist identified principal cause among them that could have lead to disability. The most “preventable” or “treatable” cause was given precedence over a nonpreventable or non-treatable cause.± The person's visual impairment was categorized into preventable, treatable, and no treatment possible. The cause of visual impairment was also labeled according to the main tissue involved: cornea, lens, posterior segment, globe, and error of refraction.
The visual disabilities were defined as per the revised International Classification of Diseases ICD10.[7] The list of diagnosis included cornea, opacity, cataract, glaucoma, globe abnormality, and uncorrected aphakia.
Ophthalmic assistants, local health workers, and ophthalmologists were the team members for the survey. Epidemiologist supervised the field activities and the training. Health workers assisted in collecting medical history and demographic information. Ophthalmic assistants examined vision of all individuals and recorded all relevant findings.
A person was defined as blind if the BCV acuity in the better eye was less than 3/60. If a person had BCV less than 6/60 to 3/60, the visual disability was considered as severe visual impairment (SVI). Moderate visual impairment (MVI) was defined as the BCV acuity between 6/18 and 6/60. These definitions were to measure prevalence with presenting vision and with the best correction. If vision improved to less than 6/18 with pin hole, the cause of visual disability was considered to be refractive error. Cataract impairing the vision in an eye was defined as having cataract as underlying cause of visual disability. In the absence of any other obvious cause, presence of significant pallor, cup: disc (C: D) ratio of more than 0.6, pigment changes, and other signs such as iridectomy/blebs and C: D asymmetry of more than 0.2 between the two eyes were used to define glaucoma. A person with sight threatening diabetic retinopathy was considered to have visual disability due to diabetes. In the presence of macular scar, drusen at macula, geographic atrophy, a person was labelled as having age-related macular degeneration.
We included the field staff with the experience of conducting blindness or eye disease survey in the past. A training workshop was also held for all the team members to standardize survey methodology. The interobserver variation assessment for visual acuity was conducted during pilot and Kappa value was more than 0.8. Guidelines for conducting survey were prepared and given to the field investigators who used it as reference material. A pilot of RAAB was held in the district but in the area other than the selected clusters.
The data were collected on a standard pretested form. The data were entered in spreadsheet of Microsoft XL. Then it was converted to Statistical Package for Social Studies (SPSS 11 IBM, Boston, USA). Univariate analysis was carried out using the parametric method. For qualitative variable frequencies, percentage proportion and their 95% confidence intervals were calculated. To compare the risk of blindness, visual impairments among variables, we calculated odds ratio (OR) and their 95% confidence intervals and P values.
Persons with curable causes of visual impairment were treated at Nadurbar Eye Hospital. Eye medications were given free of cost. The survey outcomes and their public health implications were discussed with the district health authorities.
Results
Of the 2,300 enumerated persons of 50 years and older ages, we could examine 2,004 persons (response rate: 87.2%). Twenty-six persons refused while 249 persons were absent during the survey. The mean age of participants was 61.9 years (standard deviation 9.1 years); 951 (47.5%) participants were working to earn while 501 participants had “no work at all [Table 1].”
Table 1.
Comparison of enumerated and examined participants in Rapid Assessment of Avoidable Blindness in Nandurbar district of Maharashtra India
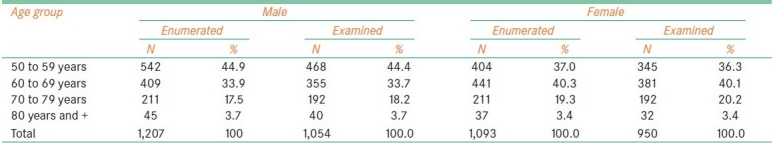
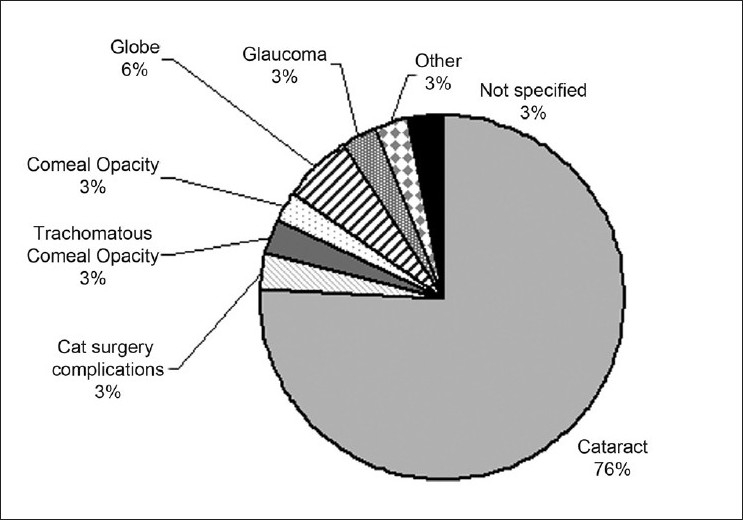
The magnitude of blindness, SVI, and MVI were calculated. The age and sex-adjusted prevalence rates with their 95% confidence interval for enumerated sample are given in Table 2. The prevalence of bilateral blindness was 1.63% (95% CI 1.11–2.15). The prevalence of SVI was 5.93% (95% CI 4.96–6.90). The prevalence of MVI was 14.6% (95% CI 13.2–16.1).
Table 2.
Blindness (vision <3/60), SVI and MVI among tribal population of Nadurbar District of Maharashtra, India
In addition to the BCV acuity, we calculated the magnitude of visual disabilities on the basis of visual acuity for distance as presented. The prevalence of blindness, SVI, and MVI for presented vision was 1.87% (1.32–2.42), 6.72% (95% CI 5.70–7.74), and 19% (95% CI 17.4–20.6), respectively.
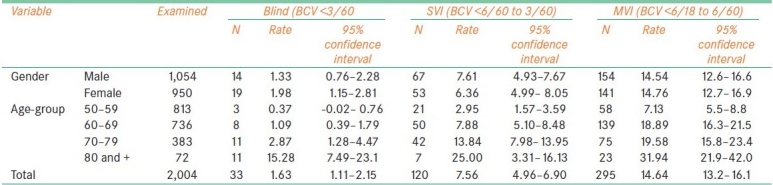
We compared the prevalence rates of blindness in different surveys [Figure 1]. We used definition of blindness as presented vision of 6/60 in better eye and accordingly the prevalence rate in this study was 7.56% (95% CI 6.48–8.64).
Figure 1.
Comparison of Rapid Assessment of Avoidable Blindness outcomes of different studies in India (blindness is defined as BCV Acuity 6/60 in better eye)
Although more females were blind than males, the gender difference of blindness was not statistically significant. (OR = 1.5, 95% CI of OR 0.75–3.75). The blindness was significantly higher in age group of “80 years and older” compared with other age groups. (χ2 = 49.3, degree of freedom = 3, P ≤ 0.0001). The blindness was significantly associated to the persons who did not have any work (χ2 = 36.6, degree of freedom = 3, p ≤ 0.0001).
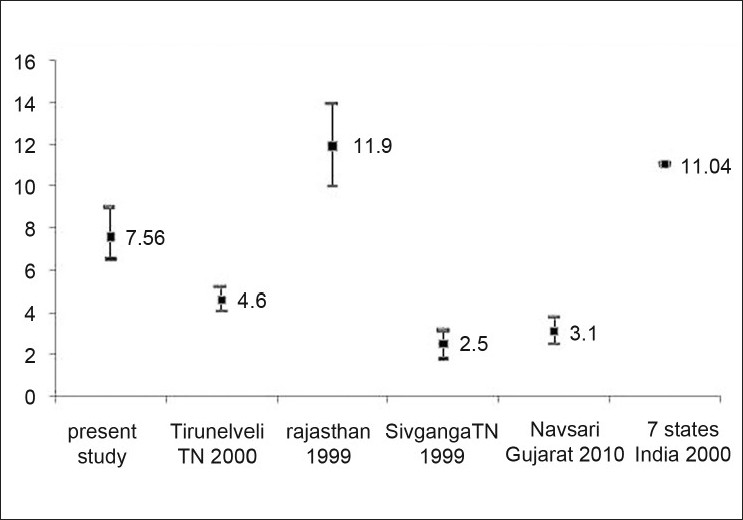
The proportion of principal causes responsible for bilateral blindness is shown in Figure 2. Unoperated cataract contributed three-forth of visual disabilities.
Figure 2.
Causes of bilateral blindness (BCVA <3/60), in tribal population of Nandurbar district of India
Of the 306 eyes of 153 persons with SVI, significant lens opacity was present in 135 (89.4%) eyes. Only 14 (9.1%) eyes had undergone cataract surgery in the past. Thus, the coverage of the existing cataract surgery service was 14/(14 + 135) × 100 = 9.4%. Nine (64.3%) of 14 eyes had undergone lens implantation during cataract surgery. The rural population in Nandurbar district is 1,110,000 (560,000 males and 550,000 females). Thus, there could be 13,750 (5,560 males and 8,290 females) persons with blinding cataract in rural areas of Nandurbar district.
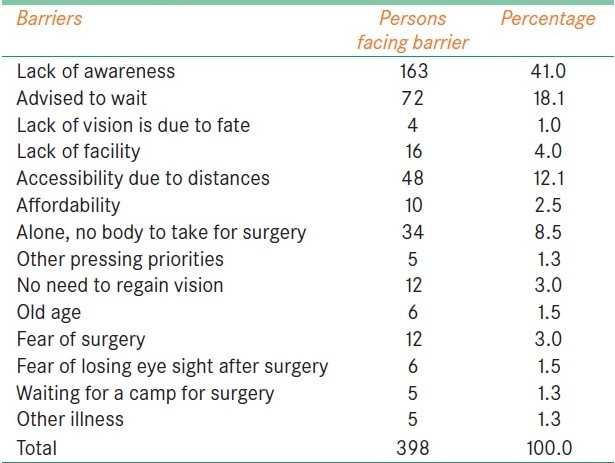
The questions related to the barriers for cataract surgery were answered by 398 persons having vision less than 6/18 due to cataract. The main causes of “not getting operating for cataract in the past” were analyzed [Table 3]. Lack of knowledge about role of cataract surgery to restore eyesight was the main cause of unoperated cataract among study participants.
Table 3.
Barriers for cataract surgeries in the tribal population of Nandurbar District of Maharashtra, India
Discussion
The health care in general and eye health care in particular have improved in India in the last two decades. However, marked variation is reported in cataract surgery rates and resources for eye care in different states.[8,9] Tribal belts of different states are inaccessible and hence are likely to have a huge backlog of preventable/curable causes of visual disabilities. If further inroads are to be made in the elimination of avoidable blindness, services should reach them. Our survey outcomes will help in better planning of eye care in Nandurbar district of Maharashtra. It also gave information of blinding eye diseases and barriers to cataract services in the tribal areas.
The prevalence of bilateral blindness among tribal population of 50 years and older ages was 1.63%. Three-forth of them were blind due to unoperated cataract. Lack of awareness, distance for eye clinic, cost, and wrong advice to wait were the main causes for cataract-related blindness.
In view of sound method of sampling and proper planning, systematic error and bias are less likely to affect the outcomes of our study. We assumed that the rate of visual disabilities among 275 nonparticipants and those who were examined was same. If all persons who did not participate were blind, the blindness rate could be as high as 2.9%. In contrast, if all nonparticipants were with normal eye sight, the blindness rate could be as low as 1.6%. The study area was remote and the population had limited exposure to the urban visitors. If investigators are city dwellers, the participation rate and cooperation for eye examination during the survey would be less. To overcome this problem, we used health staff who were involved in camps in the area and even local volunteers were recruited to assist us.
Comparison of our study results with that of other studies was challenging as there was wide variation in definitions of visual disabilities, and different age groups were focussed in different studies. The prevalence of bilateral blindness in countries of African continent (Tanzania 2.4%, Rawanda 1.8%, and Kenya 2%) was higher than 1.63% that was noted in our study.[10–12] In the neighboring countries; Bangladesh, Nepal, and Pakistan, the prevalence of blindness in the same age group was 2.9%, 4.6%, and 1.9%, respectively.[13–15] In the surveys conducted in 90s and early part of this decade in India, the surveys documented 4.6%, 6.1%, and 6.6% blindness rates in “50 years and old” age group.[16–20] The access to the eye care services in the past seems to be worse in the tribal areas compared with the rural India and this could have resulted in a high backlog of curable/preventable causes of blindness.
Gender variation in visual disabilities and cataract surgery was not statistically significant in our study. This is in contrast to outcomes of other studies where researchers found that the female gender was a barrier for the uptake of eye care services.[21,22] Tribal females seem to get equal importance as male for getting health services. More working females among tribal population would need of better vision and this could be the reason for this observation.
In our study, “70 years and more” age group had high rates of different visual disabilities. With 75% of visual disabilities due to cataract, the age-related eye problem and lack of adequate eye services in the study area to operate them could have resulted in this backlog of unoperated cataract cases in last two decades. This could explain the higher rates of visual disabilities in older age group. Such high prevalence in older age group was also observed in other community-based studies mainly targeting rural populations.[3,19,23]
The World Health Organization has recommended that the member countries should use CSR, cataract surgical coverage (CSC), and cataract surgery outcomes as indicators to monitor the progress of public health approach to address cataract blindness.[24] Less than 10% CSC in our study area is alarmingly low. This will continue increasing the backlog of avoidable blindness if coverage is not improved soon. In rural Rajasthan and Tirunelveli district of Tamilnadu states of India also, the CSC in 1999 was 12.8% and 11.8%, respectively.[16,17] However, it was 14.7% in another district of Tamilnadu state.[18] Interestingly, the Gujarat state which has the highest CSR (More than 10,000 per million population in 2009) had cataract as leading cause of blindness.[19] Thus, it seems that CSR could paint a false picture of “need for cataract services.” Many blinding cataract might not be undergoing surgeries and the cataract with severe and MVI especially in urban areas might be undergoing surgeries in large proportion. It could also be possible that in the absence of detailed fundus examination and field of vision testing, the cataract blindness might have been overestimated and when we calculate CSC, we might get low rates.[25] Further studies are recommended to review relationship of CSR and CSC.
The barrier for cataract surgery in our study did not differ from other studies conducted in India.[26–28] Lack of awareness, nonaffordability, fear for surgery, and lack of access to the eye care services were also reported to be the main barriers among population with blinding cataract. Proper counselling before surgery by using success story could be strategies to address these barriers in our study area.
Evidence-based information makes the health program management more effective. The eye care services in this district should be geared up to operate 27,000 eyes with blinding cataract that are estimated in our survey. The estimates of visual disabilities also should be used as baseline and for preparing an action plan. In absence of sufficient resources, diagnostic and surgical camps could be planned as short-term solutions.
Acknowledgments
We thank the Ethical and Research Committee of HV Desai eye hospital for their approval and support to this survey. Dr. Andurkar's encouragement and help in logistics was enormous. Dr. Parikshit Gogate had provided guidance and support. Mr. Pawar, Mr. Jagdale, and all ophthalmic officers of Nandurbar co-operated in conducting and planning surveys in their respected areas. Mr. Jitesh Ratnakar Kharat and Mr. Sanjay Kulkarni had co-coordinated camps and dedicatedly contributed in the survey. Mr Mohsin (optometrist) also helped during the survey. Mr Ramdas and Mr Vishnu did the data entry. We thank all of them.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
Distribution of population by age group and sex Census India. http://gov.bih.nic.in/Depts/PlanningDevelopment/Statistics/table_7.pdf last accessed on 24 October 2011.
Limburg H, Kooper H, RAAB Instruction manual http://www.cehjournal.org/files/raab/RAABManualVFPV4.02.pdf
References
- 1.Taylor HR, Xie J, Fox S, Dunn RA, Arnold AL, Keeffe JE. The prevalence and causes of vision loss in Indigenous Australians: The National Indigenous Eye Health Survey. Med J. 2010;192:312–8. doi: 10.5694/j.1326-5377.2010.tb03529.x. [DOI] [PubMed] [Google Scholar]
- 2.Abdul Kalam AP. Removal of avoidable blindness, our mission. Indian J Ophthalmol. 2007;55:91–3. doi: 10.4103/0301-4738.30700. [DOI] [PubMed] [Google Scholar]
- 3.Neena J, Rachel J, Praveen V, Murthy GV Rapid Assessment of Avoidable Blindness India Study Group. Rapid Assessment of Avoidable Blindness in India. PLoS One. 2008;3:e2867. doi: 10.1371/journal.pone.0002867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murthy G, Gupta SK, John N, Vashist P. Current status of cataract blindness and Vision 2020: The right to sight initiative in India. Indian J Ophthalmol. 2008;56:489–94. doi: 10.4103/0301-4738.42774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Limburg H, Kumar R, Indrayan A, Sundaram KR. Rapid assessment of prevalence of cataract blindness at district level. Int J Epidemiol. 1997;26:1049–54. doi: 10.1093/ije/26.5.1049. [DOI] [PubMed] [Google Scholar]
- 6.Bachani D, Murthy GV, Gupta KS. Rapid assessment of cataract blindness in India. Indian J Public Health. 2000;44:82–9. [PubMed] [Google Scholar]
- 7.Geneva, 4-5 September 2003. Geneva: WHO; 2003. Prevention of Blindness and Deafness. Consultation on development of standards for characterization of vision loss and visual functioning. (WHO/PBL/03.91) [Google Scholar]
- 8.Bachani D, Murthy GV, Gupta KS. Rapid assessment of cataract blindness in India. Indian J Public Health. 2000;44:82–9. [PubMed] [Google Scholar]
- 9.Murthy GV, Gupta SK, Bachani D, Tewari HK, John N. Human resources and infrastructure for eye care in India: Current status. Natl Med J India. 2004;17:128–34. [PubMed] [Google Scholar]
- 10.Habiyakire C, Kabona G, Courtright P, Lewallen S. Rapid assessment of avoidable blindness and cataract surgical services in Kilimanjaro region, Tanzania. Ophthalmic Epidemiol. 2010;17:90–4. doi: 10.3109/09286580903453514. [DOI] [PubMed] [Google Scholar]
- 11.Mathenge W, Nkurikiye J, Limburg H, Kuper H. Rapid assessment of avoidable blindness in Western Rwanda: Blindness in a postconflict setting. PLoS Med. 2007;4:e217. doi: 10.1371/journal.pmed.0040217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mathenge W, Kuper H, Limburg H, Polack S, Onyango O, Nyaga G, et al. Rapid assessment of avoidable blindness in Nakuru district, Kenya. Ophthalmology. 2007;114:599–605. doi: 10.1016/j.ophtha.2006.06.057. [DOI] [PubMed] [Google Scholar]
- 13.Wadud Z, Kuper H, Polack S, Lindfield R, Akm MR, Choudhury KA, et al. Rapid assessment of avoidable blindness and needs assessment of cataract surgical services in Satkhira District, Bangladesh. Br J Ophthalmol. 2006;90:1225–9. doi: 10.1136/bjo.2006.101287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sherchan A, Kandel RP, Sharma MK, Sapkota YD, Aghajanian J, Bassett KL. Blindness prevalence and cataract surgical coverage in Lumbini Zone and Chetwan District of Nepal. Br J Ophthalmol. 2010;94:161–6. doi: 10.1136/bjo.2008.155408. [DOI] [PubMed] [Google Scholar]
- 15.Ahmad K, Khan MD, Qureshi MB, Munami S, Shah RA, Rasheed H, et al. Prevalence and causes of blindness and low vision in a rural setting in Pakistan. Ophthalmic Epidemiol. 2005;12:19–23. doi: 10.1080/09286580490921304. [DOI] [PubMed] [Google Scholar]
- 16.Nirmalan PK, Thulasiraj RD, Maneksha V, Rahmathullah R, Ramakrishnan R, Padmavathi A, et al. A population based eye survey of older adults in Tirunelveli district of south India: Blindness, cataract surgery, and visual outcomes. Br J Ophthalmol. 2002;86:505–12. doi: 10.1136/bjo.86.5.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murthy GV, Gupta S, Ellwein LB, Munoz SR, Bachani D, Dada VK. A population-based eye survey of older adults in a rural district of Rajasthan: I. Central vision impairment, blindness, and cataract surgery. Ophthalmology. 2001;108:679–85. doi: 10.1016/s0161-6420(00)00579-0. [DOI] [PubMed] [Google Scholar]
- 18.Thulasiraj RD, Rahamathulla R, Saraswati A, Selvaraj S, Ellwein LB. The Sivaganga eye survey: I.Blindness and cataract surgery. Ophthalmic Epidemiol. 2002;9:299–312. doi: 10.1076/opep.9.5.299.10334. [DOI] [PubMed] [Google Scholar]
- 19.Murthy GV, Vashist P, John N, Pokharel G, Ellwein LB. Prevalence and causes of visual impairment and blindness in older adults in an area of India with a high cataract surgical rate. Ophthalmic Epidemiol. 2010;17:185–95. doi: 10.3109/09286586.2010.483751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chandrashekhar TS, Bhat HV, Pai RP, Nair SK. Prevalence of blindness and its causes among those aged 50 years and above in rural Karnataka, South India. Trop Doct. 2007;37:18–21. doi: 10.1258/004947507779952113. [DOI] [PubMed] [Google Scholar]
- 21.Marseille E, Brand R. The distribution of cataract surgery services in a public health eye care program in Nepal. Health Policy. 1997;42:117–33. doi: 10.1016/s0168-8510(97)00063-8. [DOI] [PubMed] [Google Scholar]
- 22.Limburg H, Keunen JE. Blindness and low vision in The Netherlands from 2000 to 2020-modeling as a tool for focused intervention. Ophthalmic Epidemiol. 2009;16:362–9. doi: 10.3109/09286580903312251. [DOI] [PubMed] [Google Scholar]
- 23.Li Z, Cui H, Liu P, Zhang L, Yang H, Zhang L. Prevalence and causes of blindness and visual impairment among the elderly in rural southern Harbin, China. Ophthalmic Epidemiol. 2008;15:334–8. doi: 10.1080/09286580802227386. [DOI] [PubMed] [Google Scholar]
- 24.Approaches to prevention to prevention of visual impairment in Global Initiative for the Elimination of Avoidable Blindness: Action plan 2006-2011. France: 2007. World Health Organization; pp. 9–14. [Google Scholar]
- 25.Dandona L, Dandona R, Naduvilath TJ, McCarty CA, Nanda A, Srinivas M, et al. Is current eye-care-policy focus almost exclusively on cataract adequate to deal with blindness in India? Lancet. 1998;351:1312–6. doi: 10.1016/S0140-6736(97)09509-3. [DOI] [PubMed] [Google Scholar]
- 26.Kovai V, Krishnaiah S, Shamanna BR, Thomas R, Rao GN. Barriers to accessing eye care services among visually impaired populations in rural Andhra Pradesh, South India. Indian J Ophthalmol. 2007;55:365–71. doi: 10.4103/0301-4738.33823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khanna R, Raman U, Rao GN. Blindness and poverty in India: The way forward. Clin Exp Optom. 2007;90:406–14. doi: 10.1111/j.1444-0938.2007.00199.x. [DOI] [PubMed] [Google Scholar]
- 28.Finger RP, Ali M, Earnest J, Nirmalan PK. Cataract surgery in Andhra Pradesh state, India: An investigation into uptake following outreach screening camps. Ophthalmic Epidemiol. 2007;14:327–32. doi: 10.1080/01658100701486814. [DOI] [PubMed] [Google Scholar]


