Abstract
Hypertriglyceridemia is a rare, but well-known cause of acute pancreatitis. A serum triglyceride level of more than 1000 to 2000 mg / dl is the identifiable risk factor. It typically presents as an episode of acute pancreatitis or recurrent acute pancreatitis. The clinical course and routine management of Hypertriglyceridemia-induced pancreatitis is similar to other causes. A thorough family history is important, as is the identification of secondary causes of hypertriglyceridemia. The mainstay of therapy includes dietary restriction of fatty meal and fibric acid derivatives. We hereby report the case of a 37-year-old lady with a family history of dyslipidemia presenting with recurrent episodes of acute pancreatitis. We also review the literature for pathogenesis and management of hyperlipidemia.
Keywords: Acute pancreatitis, fibric acid derivatives, hypertriglyceridemia, hyperlipidemia
INTRODUCTION
Acute pancreatitis is a common condition with various possible etiologies, gall stones and alcohol being the most common.[1] Metabolic, structural, and iatrogenic causes account for 20 – 25% of the cases.[2] Hyperlipidemia in the form of hypertriglyceridemia or chylomicronemia, although less frequent, is one of the well-accepted underlying causes of acute pancreatitis in 7% of the cases — the most common after gall stones and alcohol.[3] Typically hypertriglyceridemia-induced pancreatitis occurs in a patient with a pre-existing lipid abnormality, along with the presence of a secondary precipitating factor (e.g., poorly controlled diabetes, alcohol or medication). The triglyceride levels of more than 1000 to 2000 mg / dl in patients with type I, III, IV, and V hyperlipoproteinemia (Friedrickson's classification) is the identifiable risk factor.[4] Genetic factors determine over 60% of the variability in serum lipids.[5] The secondary causes of hypertriglyceridemia have to be ruled out. Most patients can be effectively treated with the existing drug therapy. Heparin and insulin have a role to play in the treatment.[6] Other novel modalities include plasma exchange and lipid aphaeresis.[7] Here we report a lady presenting with recurrent pancreatitis, with features of hyperlipidemia, and review the literature for pathogenesis and management of hyperlipidemia.
CASE REPORT
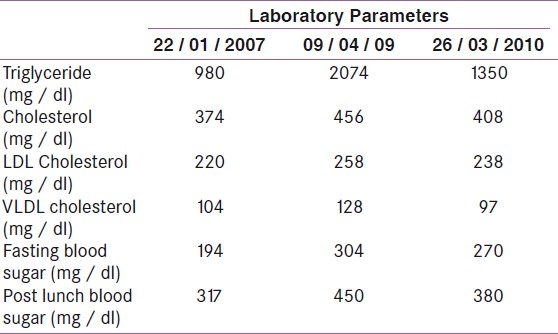
A 37-year-old female presented with a chief complaint of epigastric pain for three days. The pain was continuous, radiating to the back, and associated with two episodes of bilious vomiting. She was not receiving hypolipidemic agents for last three months against physician's advice. Four years back she presented with similar complaints and was diagnosed as having acute pancreatitis with type 2 diabetes, hypertension, and combined dyslipidemia. Treatment was started with insulin, telmisartan, atrorvastatin, fenofibrate, and a low-fat diet. In between, after stopping treatment on her own, she ended up with two episodes of acute pancreatitis. Laboratory parameters during the previous three presentations are depicted in Table 1. Two of her elder brothers died at the age of 40 to 45 years, because of coronary artery disease and combined dyslipidemias. One younger sister was also a known case of combined dyslipidemia, on treatment.
Table 1.
Laboratory parameters of the patient during the previous three presentations with acute pancreatitis
On examination, her pulse rate was 120 / minute, blood pressure 150 / 100 mm Hg, respiratory rate 26 / minute, and temperature 101.4°F. She was somnolent and dehydrated. There was a markedly tender and rigid epigastrium, with diminished bowel sounds and hepatosplenomegaly. She had arcussenilis and lipemiaretinalis, but no eruptive xanthoma. Initial laboratory findings were a total leukocyte count of 16000 / cmm with 86% neutrophils, platelets 220000 / cmm, and c-reactive protein 17.2 gm / dl. Serum electrolytes, calcium, liver, and renal function tests, and lactate dehydrogenase and coagulation tests were normal. Serum was lipemic. Other investigations were as follows, total cholesterol 741 mg / dl, Low-density lipoprotein (LDL) cholesterol 249 mg / 74 mg / dl, very-low-density lipoprotein (VLDL) cholesterol 416 mg / dl, and triglycerides 2080 mg / dl. Fasting blood sugar (FBS) was 174 mg / dl and post-lunch blood sugar (PLBS) was 286 mg / dl. Ultrasonography of the abdomen showed a grade 1 fatty liver, hepetosplenomegaly with a bulky body, and the tail of the pancreas. Enlarged and edematous pancreas with smooth, ill-defined margins, a non-visualized pancreatic duct, and peripancreatic fat stranding were seen in a computed tomogram of the abdomen [Figure 1]. The patient was conservatively managed with intravenous fluids and narcotics for pain control. On the basis of high triglycerides, cholesterol, and VLDL cholesterol, a diagnosis of type IIb hyperlipoproteinemia (Familial Combined Hyperlipidemia / FCHL) was established. Treatment with fenofibrate 160 mg, atorvastatin 20 mg, and omega-3 fatty acids 2 g, twice daily, with antioxidants was started. After stabilization endoscopic retrograde cholangiopancreatography found no anatomic abnormality. The patient was discharged with insulin, antihypertensive, and hypolipidemic agents.
Figure 1.

CT abdomen showing enlarged and edematous pancreas with smooth, ill-defined margins, non-visualized pancreatic duct, and peripancreatic fat stranding
DISCUSSION
The association between acute pancreatitis and hyperlipidemia is well known, both as a precipitant and as an epiphenomenon.[8] The coexistent medical conditions such as diabetes should prompt further workup.[9] Hypertriglyceridemia can be primary in less than 5% of the cases, due to genetic causes and more often secondary to other causes like diabetes, obesity, pregnancy, excess carbohydrate intake, hypothyroidism, alcohol, hepatitis, sepsis, renal failure, and drugs like estrogen, glucocorticoids, β blocker, bile acid binding resins, thiazide, tamoxifen cyclosporine protease inhibitors, and isotretinoin.[10]
In our patient, the presence of a family history of dyslipidemia, with laboratory values of high cholesterol, LDL cholesterol, VLDL cholesterol, and triglycerides, led us to the diagnosis of type IIb hyperlipoproteinemia.
Chylomicrons are triglyceride-rich lipoprotein particles. They are present in the circulation when triglycerides are > 10 mmol / l (900 mg / dl). These are large enough to occlude the pancreatic capillaries, leading to ischemia and subsequent acinar structural alteration, as also a release of pancreatic lipase. Enhanced lipolysis leads to an increased concentration of free fatty acids, which results in the release of inflammatory mediators and free radicals culminating in inflammation, edema, and necrosis.[11] Our patient had a total of four episodes of pancreatitis (each time triglycerides were > 900 mg / dl) after stopping the hyolipidemic agent each time.
Chylomicrons are the product of dietary fat absorption. Therefore, abstinence from eating after pancreatitis may allow rapid metabolism of the triglyceride-rich chylomicrons.[2] Other non-pharmacological measures include weight reduction, reduced calories, fat, and refined carbohydrate intake. Our patient was advised to restrict fat to 10 – 15% of total energy intake (about 15 – 20 gm / day) with reduction in saturated fats and unsaturated and trans fats.[12]
Fibrates are the mainstay of therapy, they reduce plasma triglyceride levels by up to 50% and raise the high-density lipoprotein (HDL) cholesterol by 20%.[13] They modulate peroxisome proliferator activated receptors-α (PPAR-α) in the liver, with decreased hepatic secretion of VLDL and increased lipolysis of the plasma triglyceride.[14] They also reduce small dense LDL particles and increase HDL.[15] Statins reduce the cholesterol by inhibiting hydroxylmethylglutaryl CoA reductase, thereby reducing coronary heart disease end points in type 2 diabetes.[16] Omega-3-fatty acids (eicosapentanoic and docosahexanoic acid) reduce plasma triglycerides by 20% when used in combination with other triglyceride-lowering therapies.[17] Antioxidant therapies (Selenium, β carotene, vitamin C, α-tocopherol) have been used in the reduction of recurrent pancreatitis episodes that have remained markedly hypertriglyceridemic after medical therapy, by virtue of their protection from free radical-induced acinar damage.[18] Our patient had been prescribed a combination of fenofibrate, atorvastatin, omega-3 fatty acids, and antioxidants. Other options include niacin, bile acid binding resins, and glitazar drugs. Novel modalities include the use of medium chain triglycerides (they do not require chylomicron formation for absorption), plasmapheresis,[13] insulin and heparin,[19] and lipoprotein lipase gene therapy.[20]
CONCLUSION
Hypertriglyceridemia is a common clinical problem, and if markedly elevated, can lead to pancreatitis. General and specific therapies are available to reduce triglycerides during the acute phases of pancreatitis. Nutrition, pharmacological therapy, and avoiding aggravating factors are essential for preventing further attacks.
ACKNOWLEDGEMENTSs
All the authors would extend their heartfelt thanks to Dr. Jagadeesh Tangudu, M Tech, MS, PhD and Sowmya Jammula, M Tech for their immense and selfless contribution towards manuscript preparation, language editing and final approval of text.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Toskes PP. Hyperlipidemic pancreatitis. Gastroenterol Clin North Am. 1990;19:783–91. [PubMed] [Google Scholar]
- 2.Dominguez-Munoz JE, Malfertheiner P, Ditschuneit HH, Blanco-Chavez J, Uhl W, Buchler M, et al. Hyperlipidemia in acute pancreatitis.Relationship with etiology, onset and severity of the disease. Int J Pancreatol. 1991;10:261–7. [PubMed] [Google Scholar]
- 3.Seales CE, Ooi TC. Underrecognition of chylomicronemia as a cause of acute pancreatitis. CMAJ. 1992;147:1806–8. [PMC free article] [PubMed] [Google Scholar]
- 4.Lithell H, Vessby B, Walldius G, Carlson LA. Hypertriglyceridemia-acute pancreatitis-ischemic heart disease. A case study in a pair of monozygotic twins. Acta Med Scand. 1987;221:311–6. [PubMed] [Google Scholar]
- 5.Fortson MR, Freedman SN, Webster PD., 3rd Clinical assessment of hyperlipidemic pancreatitis. Am J Gastroenterol. 1995;90:2134–9. [PubMed] [Google Scholar]
- 6.Monga A, Arora A, Makkar RP, Gupta AK. Hypertriglyceridemia- induced- acute pancreatitis- treatment with hepatin and insulin. Indian J Gastroenterol. 2003;22:102–3. [PubMed] [Google Scholar]
- 7.Yeh JH, Chen JH, Chiu HC. Plasmapheresis for hyperlipidemic pancreatitis. J Clin Apheresis. 2003;18:181–5. doi: 10.1002/jca.10063. [DOI] [PubMed] [Google Scholar]
- 8.Yadav D, Pitchumoni CS. Issues in hyperlipidemic pancreatitis. J Clin Gastroenterol. 2003;36:54–62. doi: 10.1097/00004836-200301000-00016. [DOI] [PubMed] [Google Scholar]
- 9.Lemieux I, Pascot A, Couillard C, Lamarche B, Tchernof A, Alméras N, et al. Hypertriglyceridemic waist: A marker of the atherogenic metabolic triad (hyperinsulinemia; hyperapolipoprotein B; small dense LDL) in men? Circulation. 2000;102:179–84. doi: 10.1161/01.cir.102.2.179. [DOI] [PubMed] [Google Scholar]
- 10.Hegele RA. Monogenic dyslipidemias: Window on determinants of plasma lipoprotein metabolism. Am J Hum Genet. 2001;69:1161–77. doi: 10.1086/324647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kimura W, Mossner J. Role of hypertriglyceridemia in the pathogenesis of experimental acute pancretitis in rats. Int J Pancreatol. 1996;20:177–84. doi: 10.1007/BF02803766. [DOI] [PubMed] [Google Scholar]
- 12.Expert panel on detection, evaluation and treatment of high blood cholesterol in adults. Executive summary of the third report of the National Cholesterol Education Programme (NCEP) Expert panel on detection, evaluation and treatment of high blood cholesterol in adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 13.Barter PJ, Rye KA. Cardioprotective properties of fibrates: Which fibrate, which patients, what mechanism? Circulation. 2006;113:1553–5. doi: 10.1161/CIRCULATIONAHA.105.620450. [DOI] [PubMed] [Google Scholar]
- 14.Rubins HB, Robins SJ, Collins D, Nelson DB, Elam MB, Schaefer EJ, et al. Diabetes, plasma insulin and cardiovascular disease: Subgroup analysis from the Department of Veterans Affairs high density lipoprotein intervention trial (VA-HIT) Arch Intern Med. 2002;162:2597–604. doi: 10.1001/archinte.162.22.2597. [DOI] [PubMed] [Google Scholar]
- 15.Frick MH, Elo O, Haapa K, Heinonen OP, Heinsalmi P, Helo P, et al. Helsinki Heart Study: Primary-prevention trial with gemfibrozil in middle aged men with dyslipidemia.Safety of treatment, changes in risk factors and incidence of coronary heart disease. N Engl J Med. 1987;317:1237–45. doi: 10.1056/NEJM198711123172001. [DOI] [PubMed] [Google Scholar]
- 16.Gami AS, Montori VM, Erwin PJ, Khan MA, Smith SA Evidence in Diabetes Enquiry System (EVIDENS) Research Group. Systematic review of lipid lowering for primary prevention of coronary heart disease in diabetes. BMJ. 2003;326:528–9. doi: 10.1136/bmj.326.7388.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hooper L, Thompson RL, Harrison RA, Summerbell CD, Ness AR, Moore HJ, et al. Risks and benefits of omega 3 fats for mortality, cardiovascular disease and cancer: Systematic review. BMJ. 2006;332:752–60. doi: 10.1136/bmj.38755.366331.2F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Topol EJ. Intensive statin therapy-A sea change in cardiovascular prevention. N Engl J Med. 2004;350:1562–4. doi: 10.1056/NEJMe048061. [DOI] [PubMed] [Google Scholar]
- 19.Tenenbaum A, Motro M, Fisman EZ, Tanne D, Boyko V, Behar S. Benzafibrate for the secondary prevention of myocardial infarction in patients with metabolic syndrome. Arch Intern Med. 2005;165:1154–60. doi: 10.1001/archinte.165.10.1154. [DOI] [PubMed] [Google Scholar]
- 20.Rip J, Nierman MC, Sierts JA, Petersen W, Van den Oever K, Van Raalte D, et al. Gene therapy for lipoprotein lipase deficiency: Working towards clinical application. Hum Gene Ther. 2005;16:1276–86. doi: 10.1089/hum.2005.16.1276. [DOI] [PubMed] [Google Scholar]


