Abstract
South Asia is home to one of the largest population of people with metabolic syndrome (MetS). The prevalence of MetS in South Asians varies according to region, extent of urbanization, lifestyle patterns, and socioeconomic/cultural factors. Recent data show that about one-third of the urban population in large cities in India has the MetS. All classical risk factors comprising the MetS are prevalent in Asian Indians residing in India. The higher risk in this ethnic population necessitated a lowering of the cut-off values of the risk factors to identify and intervene for the MetS to prevent diabetes and cardiovascular disease. Some pharmacological and nonpharmacological interventions are underway in MetS to assess the efficacy in preventing the diabetes and cardiovascular disease in this ethnic population.
Keywords: Metabolic syndrome, South Asians, prediabetes
INTRODUCTION
Metabolic syndrome is probably one of its kind in the fact that there have been innumerable studies related to it without there being a consensus on its optimum definition yet. The concept of this syndrome with the central pathogenesis of insulin resistance gained ground to identify individuals who were at risk of developing diabetes and cardiovascular diseases (CVD) in the future. South Asians have been found to have a predilection for development of this syndrome.
DEFINITION OF SOUTH ASIA
According to the United Nations geographic region classification, South Asia comprises the countries of Afghanistan, Bangladesh, Bhutan, India, Iran, Maldives, Nepal, Pakistan, and Sri Lanka. By other definitions and interpretations, Myanmar and Tibet are also sometimes included in the region of South Asia. South Asia is home to well over one-fifth of the world's population, making it both the most populous and the most densely populated geographic region in the world.[1]
South Asia, also known as southern Asia, is the southern region of the Asian continent, which comprises the sub-Himalayan countries and, for some authorities, also includes the adjoining countries to the west and the east. Topographically, it is dominated by the Indian Plate, which rises above sea level as the Indian subcontinent south of the Himalayas and the Hindu Kush. Loosely speaking, the word South Asian would mean inhabitants of the Indian subcontinent.
POPULATION DIVERSITY
Ethnic distribution of South Asian population is complex as South Asia has been invaded and settled by many ethnic groups over the centuries – including various Dravidian, Indo-Aryan, and Iranian groups – and amalgamation of Dravidian, Indo-Aryan, and native societies has produced composite cultures. Census data from India have shown that Indo-Aryan comprise 72%, Dravidian 25%, and Austro-Asiatic, Tibeto-Burman, and others comprise 3% of the population.[2]
Archeogenetic study of South Asian population as mapped by the human Y-chromosome DNA haplogroups, however, has found that overall haplogroup diversity among Indian populations was relatively high (NRY diversity value 0.893) in contrast to other European or East Asian populations, but was closer to that of Central Asia. Multi dimentional scaling (MDS) plotting study has further documented the genetic proximity of the majority of the Indian population to the Indo-European speakers of Central Asia and Eastern Europe (Russia and Siberia), rather than with populations of Western Europe.[3]
EPIDEMIOLOGY OF METABOLIC SYNDROME
Prevalence of the metabolic syndrome
Nationally representative studies regarding the prevalence of the metabolic syndrome (MetS) are generally not available from any South Asian country. Available data indicate that the prevalence of the MetS in Asian Indians varies according to region, extent of urbanization, lifestyle patterns, and socioeconomic/cultural factors.[4] Recent data show that about one-third of the urban population in large cities in India have MetS.[5,6]
A study conducted in urban areas of Karachi, Pakistan, showed a high prevalence of the MetS – 34.8 and 49% according to the International Diabetes Federation (IDF) definition and modified National Cholesterol Education Program, Adult Treatment Panel III (NCEP ATP III) criteria, respectively.[7] While obesity in urban Pakistani population ranged between 46 and 68%, hypertriglyceridemia ranged between 27 and 54%, and in particular, 68 and 81% of the population had low levels of high-density lipoprotein cholesterol (HDL-C).[8]
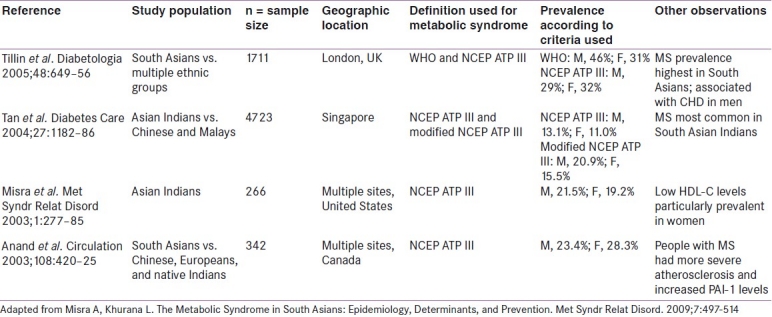
The initial astute observation of the relationship between the central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians focused the attention of the world community on the high prevalence of MetS in this particular population subgroup.[9,10] The observation was replicated in various other South Asian migrant populations from different regions of the globe. Overall, the prevalence of the MetS in migrant Asian Indians varies from 20 to 32% [Table 1]. Most UK investigators have studied South Asians consisting of Bangladeshis, Pakistanis, and Asian Indians (predominantly Punjabis and Gujaratis). Abdominal obesity, hyperinsulinemia, and dyslipidemia in migrant South Asians were significantly higher than in British Caucasians.[11,12] The prevalence of the MetS in migrant Asian Indians is higher than in many other ethnic groups. For example, in Singapore, the prevalence was 28.8% in migrant Asian Indians when using the modified NCEP ATP III definition as compared with 24.2% in Malays and 14.8% in Chinese.[13]
Table 1.
Prevalence of the Metabolic Syndrome in Migrant South Asians
Surveys in large cities in different parts of the country suggest that about one-third of the urban population in large cities in India have MetS.[14–16] All classical risk factors comprising the MetS are prevalent in Asian Indians residing in India; 31.4% abdominal obesity, 45.6% hypertriglyceridemia, 65.5% low HDL, 55.4% hypertension, and 26.7% raised fasting plasma glucose have been reported from South India. Data from North India show that 66% of men and 88% of women, classified as “nonobese” on the basis of the international cut-off of body mass index (BMI), had ?1 cardiovascular risk factors.[17]
A recent community-based study from eastern India has measured a prevalence of MetS of 31.4%, with females having a much higher prevalence (48.2%) than males (16.3%).[18]
The rural prevalence of MetS is found to be reasonably low compared to the urban prevalence. A recent survey in Central India observed an overall MetS prevalence as per ATP III criteria to be 5.0% in the adult rural population. When ATP III criteria were modified using waist circumference (WC) cut-offs recommended by Asia-Pacific guidelines, MetS was seen in 9.3% (8.2% in males and 10.7% in females).[19]
The prevalence landscape of the MetS in semi-urban area was found to be at an intermediate level between the rural and the urban prevalence levels. A recent population survey conducted in a semi-urban area in South India showed that the prevalence of MetS is 29.7% (26.5% in men and 31.2% in women).[20]
MetS in pediatric and adolescent population is also not lagging far behind. As obesity has permeated into all strata of society and age groups, it is little wonder that the pediatric age groups are not immune from it, especially so because the pediatric population is advancing rapidly in the BMI. The prevalence of overweight/obesity in urban children in Delhi has shown an increase from 16% in 2002 and 24% in 2006 to about 29% in 2007.[21] The studies conducted in developed countries have reported the overall prevalence of pediatric MetS varying between 3.1% and 12.7%, utilizing the criteria of hypertension, impaired fasting glucose (IFG), hypertriglyceridemia, reduced HDL, and central obesity as measured by WC. A survey in North India found an overall prevalence of MetS in adolescents to be 4.2%. However, there was no gender difference in the distribution of MetS. While only 1.9% of the normal weight adolescent population had MetS, 36.6% of overweight adolescents met the criteria for MetS.[22] A recent survey in another location in North India showed that the prevalence of MetS in pediatric age group is 6.5% (males 6.9% and females 5.9%). The pediatric MetS is known to be a precursor of adult MetS in a population. Hence, with the burgeoning wave of obesity in the pediatric population, the seed of MetS is sown quite early.[23]
The central obesity is associated with changes in many biochemical variables, especially with the various adipokines like leptin and adiponectin. In a study on Iranian subjects, leptin level has been found to be associated with insulin resistance and components of MetS, after adjustment of age, sex, and BMI. After adjustment of WC, this association does not hold true anymore, therefore signifying the association of leptin with central obesity.[24] In fact, in a recent study in the same population, the diagnostic accuracy of the leptin cut-off values in identifying MetS was similar to that of insulin resistance in identifying MetS.[25] In another study in a migrant South Asian population in the USA, leptin was strongly associated with all measures of adiposity, including BMI, total body fat, visceral fat, and hepatic fat. Adiponectin level showed an insignificant trend toward an inverse association with body fat composition in both women and men. Adiponectin's inverse association with adiposity was significantly attenuated by low HDL, increased triglycerides (TG), and insulin resistance.[26]
COMPONENTS OF METS IN SOUTH ASIANS
In 2005, the International Diabetes Federation (IDF) also introduced an ethnicity-specific definition of this syndrome [Table 2].[27] In a South Indian study, the prevalence of MetS was estimated to be 25.8%, 23.2%, and 18.3% according to the IDF, World Health Organization (WHO), and NCEP ATP III definitions, respectively, implicating a discord between the same.[28] Pattern recognition and identification of risk factors by cluster analysis for the development of diabetes and cardiovascular disease (CVD) have consistently implicated four key components – increased adiposity, disturbed glucose metabolism, dyslipidemia, and hypertension. However, each component has multiple methods of assessment, cut-offs, and varying predictive role, which even today are hotly debated topics.[16]
Table 2.
Definitions of metabolic syndrome
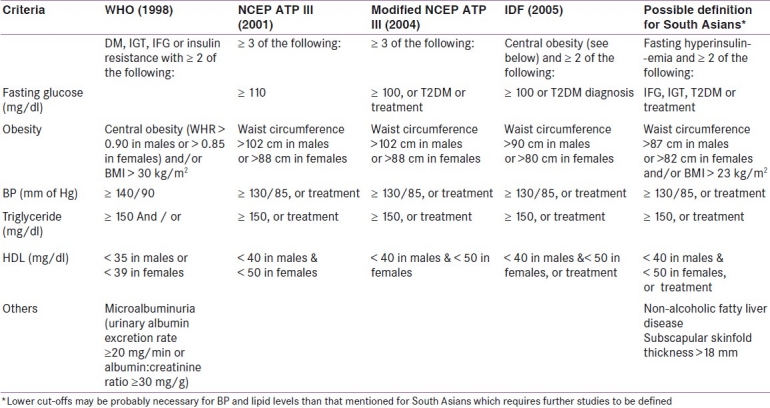
Abdominal obesity is quite prevalent in South Asians, with females outnumbering males.[14] Several studies have indicated that body fat, abdominal adiposity, and cardiovascular risk are higher in South Asians compared to Caucasians at similar BMI and lower average WC levels.[29–31] In a WHO consultation on obesity in Asia and Pacific regions in 2000, lower cut-offs for diagnosis of overweight and obesity were suggested, i.e. 23 kg/m2 and 25 kg/m2 or greater, respectively.[32] An analysis of the Chennai Urban Rural Epidemiology Study (CURES) study demonstrated that the optimal BMI cut-off point for identifying two cardiometabolic risk factors was 23 kg/m2 for Indians of both sexes and a WC of 87 cm for men and 82 cm for women.[33] A recent 2006 study of 289 South Asian migrants residing in Canada revealed BMI cut-off points of 22.5 kg/m2 for lipid metabolism and 21 kg/m2 for glucose metabolism.[34] A more recent WHO consultation in 2004 opined that the proportion of Asian people with a high risk of type 2 diabetes mellitus (T2DM) and CVD is considerable at BMI values lower than the existing WHO cut-off point for overweight (25 kg/m2) and proposed potential public health action points of BMI (23.0, 27.5, 32.5, and 37.5 kg/m2), but did not suggest a clear BMI cut-off point for overweight and obesity.[35] Intriguingly, the WHO and other international agencies have failed to define lower BMI cut-offs for Asians despite considerable evidence for the same. Contrary to BMI cut-offs, a consensus has been reached regarding lowering WC cut-offs (≥90 cm in males and ≥80 cm in females) in South Asians based on adequate evidence, which has henceforth been adopted in the modified NCEP ATP III and IDF definitions. A study has reported significantly high odds ratio (OR) for hypertension and hypertriglyceridemia even at a lower WC range (70–80 cm) in Indians.[36]
Studies have shown that the prevalence of type 2 diabetes is particularly high in South Asians, with the prevalence of insulin resistance in healthy, young lean Asian men being three to four times higher than lean men in other ethnic groups.[37,38] In a study in South African Indian individuals with MetS, elevated fasting blood glucose was found to be the most frequently occurring criterion (IDF, 87%; NCEP ATP III, 83%).[39] A study in Singapore noted that mortality risk for T2DM in Asian Indians was higher when compared with Chinese and Malays, although the latter had a higher prevalence of impaired glucose tolerance and IFG, suggesting that IFG carries a greater risk for CVD mortality in Asian Indians due to faster progression to type 2 diabetes.[40] As diabetes is the major factor underlying the progression of vascular disease, the IDF definition utilizes a fasting glucose cut-off of 100 mg/dl, a level consistent with the American Diabetes Association's revised 2003 definition of IFG which was also accepted by NCEP in 2004.[41]
Atherogenic dyslipidemia is common in South Asians who have lower HDL and higher levels of small, dense low-density lipoprotein (LDL) compared to Caucasians across all strata of the society.[42,43] Elevated serum TG is more common in affluent Indians and migrant Indians compared to the rural populace.[44–46] The NCEP ATP III criterion which is most likely to identify insulin resistance is the TG/HDL ratio, but large-scale clinical trials to determine its relative risk for development of CVD or its relationship with the MetS in different ethnicities are lacking.[47]
Hypertension is generally accepted to have the weakest association with insulin resistance compared to other factors that make up the MetS, although some studies have shown that a substantial percentage of hypertensive individuals have insulin resistance.[48,49] Interestingly, studies in the UK have shown that hypertensive South Asians have higher CVD mortality compared to individuals of African ancestry, although hypertension is more prevalent in the latter, thereby suggesting a probable requirement of ethnicity-based cut-offs in this regard.[50,51]
A number of studies using skinfold thickness have shown that subcutaneous body fat is thicker in South Asians compared to Caucasians across all age groups.[29,52–54] Studies have shown truncal subcutaneous fat to be an important determinant of insulin sensitivity in South Asians with an influence similar to that of abdominal obesity.[55–56] In an Indian study, candidate definitions using the criterion of subscapular skinfold thickness (>18 mm) have shown an increase in prevalence of MetS compared to the NCEP ATP III definition.[56] However, a candidate definition comprising only anthropometric criteria showed poor predictability for MetS in Asian Indians, implying a significant role of the laboratory in diagnosing the same.[57]
In a study in Asian Indian adolescents, inclusion of fasting hyperinsulinemia as an additional criterion to the NCEP ATP III definition resulted in an increase in the prevalence of MetS from 0.8 to 4.2%. Detection of fasting hyperinsulinemia, though resource constraining, is an early biochemical surrogate of insulin resistance and could be an additional defining criterion of MetS in young Asian Indians.[58]
Studies indicate that unlike Caucasians, intramyocellular lipid content (IMCL) is not related to insulin resistance in South Asians.[59,60] It has been shown to be related to excess body fat and abdominal obesity in this population, but the overall significance of IMCL in the pathogenesis of insulin resistance remains to be determined.[59] Obstructive sleep apnea (OSA) commonly co-occurs with obesity, hypertension, and hyperglycemia, suggesting it to be a part of the syndrome. Despite some evidence, relationship of OSA with insulin resistance independent of obesity remains to be definitely established and more investigations in South Asians are necessary in this regard.[6] Non-alcoholic fatty liver disease (NAFLD) is quite prevalent in South Asians and is an important hepatic correlate of insulin resistance and the MetS, with non-alcoholic steatohepatitis often being the first clinical indication of insulin resistance.[6,61] Both obese and non-obese Indians with NAFLD have significantly higher insulin resistance compared to those without NAFLD.[6] An Indian study reported the presence of early abnormalities in hepatic gluconeogenesis pathway in nondiabetic obese and non-obese Asian Indians with NAFLD, indicating increased future risk for development of type 2 diabetes.[14] Presence of excess dorsocervical fat (mild buffalo hump) and excess fat deposition under the skin (double chin) may also signify heightened risk for the MetS in urban Asian Indians and may be used as phenotypic markers.[62] A study in obese children and adolescents showed significant correlation of uric acid to lipids, BMI, and blood pressure, and that uric acid was a reliable indicator for the “pre-metabolic syndrome.”[63] Some studies have implicated hyperuricemia as a component of the MetS, but it is presently believed to have a weak association with the same.[64] Polycystic ovarian syndrome is more prevalent in South Asians compared to Caucasians and is associated with younger age of presentation, more severe symptoms, and greater degree of insulin resistance and could well be a significant correlate of MetS in this population.[65]
The link between subclinical inflammation and the MetS is yet to be conclusively established in South Asians. Although a few studies have shown increased C-reactive protein to correlate with adiposity in South Asians, the link between C-reactive protein and insulin resistance is far from clear in Asian Indians on the basis of available evidence.[66–68] A number of additional metabolic criteria have been proposed for research (apoB100/apoA-I ratio, lipoprotein(a), interleukin 6, fibrinogen, plasminogen activator inhibitor-1, vascular cell adhesion molecule 1, homocysteine, and endothelium-dependent dilatation), some of which are already under intense investigation.[41]
Recent evidence suggests that the MetS and its components are associated with T2DM but have weak or no association with vascular risk in elderly populations, and so the predictive value of any definition of the MetS for CVD will be required to be investigated further in different age groups in the developing countries.[69]
PECULIARITIES OF METS IN SOUTH ASIANS
South Asians with MetS are phenotypically distinct from Caucasians. Investigators have shown that compared to Caucasians, Asian Indians have lower BMI, WC, and muscle mass.[30] Studies in South Asian adults as well as children have shown that hyperglycemia, hypertension, and hypertriglyceridemia occur at lower levels of BMI and WC.[36,70,71] This is beautifully epitomized by the Y-Y hypothesis whereby the researchers Yajnik (Indian) and Yudkin (British) were found to have a similar BMI of 22.3 kg/m2, but the body fat percentages in the two differ widely at 21.2% in Yagnik and 9.1% in Yudkin.[35] Higher body fat seen in South Asians than Caucasians at similar BMI was clearly demonstrable in Asian Indians based in Singapore, who showed a BMI of 3 kg/m2 lower than Caucasians at any given percentage of body fat.[72] Multiple studies have shown that truncal subcutaneous tissue (measured by suprascapular and suprailiac skinfolds) is thicker in South Asians across all ages and correlates more closely with insulin resistance than intrabdominal adipose tissue.[52–56] It has also been noted that morbidities related to excess adiposity (diabetes, hypertension, dyslipidemia) occur at lower BMI levels more frequently in Asians than in Caucasians.[56] CVD rate is higher among South Asians and despite falling CVD-related mortality in Whites, CVD mortality among South Asians is decreasing at a significantly lower pace.[73,74] Studies also indicate that South Asians have a younger age of onset of CVD and also increased mortality risk from the same.[75,76] Although both WC and hip circumference are lower in Asian Indians compared to Caucasians, the former have a higher waist–hip ratio (WHR). In a study in Asian Indians, BMI showed correlation with WC but not with WHR, which indicates that WC and BMI may be better predictors of MetS when compared with WHR in Asian Indians.[16] Another study found similar correlation between WC and BMI and suggested that WC is a better marker of abdominal obesity than WHR.[77] Studies show that South Asians carry an increased risk and prevalence of hyperglycemia, dyslipidemia, and procoagulant tendency and have larger adipocytes (more insulin resistant).[14,30,78]
Other differences between South Asians and Caucasians include lower disease awareness and health-seeking behavior, delayed diagnosis due to atypical presentation, language barriers, religious and sociocultural factors. All these factors result in poorer prevention, less aggressive therapy, poorer response to medical and surgical interventions, and higher morbidity and mortality in the South Asians. Probably, differences in response to pharmacological agents may exist between South Asians and Caucasians, although these have been inadequately studied. In view of these data, prevention and management strategies should be more aggressive for South Asians for more positive health outcomes. Hence, lower cut-offs of obesity and abdominal obesity for South Asians are expected to help physicians in better and more effective prevention for MetS and its associated ills, especially diabetes and coronary artery diseases.[79]
VAILIDITY OF THE RISK ESTIMATORS OF METS IN SOUTH ASIANS
Although it is well known that conventional risk factors (many of which are included as components of MetS) can predict type 2 diabetes and coronary heart disease (CHD) on their own, there are evidences to suggest that the MetS may add to the prediction of type 2 diabetes and CHD beyond that provided by individual components. Subjects with the MetS from western countries face a twofold greater risk of all-cause mortality and a two- to three-fold increased risk of cardiovascular mortality compared with those without the syndrome.[80] MetS also predicts diabetes independently of other factors.[4]
Though the clinical validity of MetS to predict type 2 diabetes and, in particular, CHD has been debated by several authors, studies show that ORs for predicting incident CHD using different definitions of the MetS [NCEP ATP III (OR 2.00), IDF (1.69), and the WHO (1.73)] were almost similar, independent of age, sex, ethnic origin, history of CHD and T2DM, non–HDL-C, smoking status, and family history of myocardial infarction.[81] Subjects free from CHD and/or CHD risk equivalents, when evaluated with NCEP ATP III, IDF, and WHO definitions, were also shown to have similar ORs for predicting CHD.
Despite the fact that all these information are based on western data, they are likely to be true for other populations as well. The data in this regard are limited from South Asia. In South Asians, Sattar et al. showed strong association of the MetS with diabetes [relative risk (RR) 7.47], however, that with CHD was less strong (RR 1.27).[69] Forouhi et al. also showed higher cardiovascular risk in South Asians as compared to Caucasians, which could not be explained by presence of conventional risk factors.[82]
GENETIC STUDIES IN METS IN SOUTH ASIANS
Genetic studies in Indians have largely failed to show any exclusive genetic correlates of the MetS, with the exceptions of hepatic glucokinase promoter gene, fatty acid binding protein 2 (FABP2) gene, and apoplipoprotein C-III gene (APOC3).[83] In another study in migrant South Asian patients in South Africa with myocardial infarction and MetS, no relationship was found between any obesity-associated genetic polymorphism and the MetS compared to a control population. The melanocortin-4-receptor (MC4R) gene associated TT genotype occurred more frequently in patients with lower TG levels, while the adiponectin 45 TT genotype occurred more commonly in patients with normal fasting glucose levels. The leptin receptor (LEPR) gene Q223R TT genotype was associated with low HDL-C levels.[84] In the same population, a significant relationship was noted with the LPL –93 T/G polymorphism, with the minor G allele occurring more frequently in patients defined by the NCEP ATP III criteria (OR 2.72). The X allele of the LPL S447X polymorphism was observed less frequently in MetS patients (OR 0.52). Several genotypes, including the LPL S447X, APO E3/E3, and the CETP Taq1 B2B2, were associated with favorable lipid profiles.[85]
In a migrant South Asian population study, three of the six novel APOA1 single nucleotide polymorphisms (SNPs) were significantly associated with MetS, substantiating the CAD risk for APOA1 gene variants in South Asians. Though larger cohort studies are required to establish the etiologic role of SNPs in MetS as well as of reduced HDL, their identification can be obtained at an earlier age and aggressive measures, especially targeting HDL therapies, may prevent the future risk of CAD and clustering of risk factors.[86]
Genome-wide association (GWA) studies have become overwhelmingly popular in the last few years as a means to elucidate the association between particular alleles in one's DNA and predisposition to a disease, using genetic data from unrelated individuals randomly sampled from a population. MetS consists of a number of phenotypic traits that tend to co-occur and are highly heritable in Indian Asians (h2 between 0.27and 0.53).[87] The co-occurrence raised the question of whether or not they have common genetic mechanisms.[88,89] Most published associations for the MetS are only with individual component phenotypes, or in some cases with multiple phenotypes, but not matching any of the classic definitions of MetS. A recent study with a GWA approach was undertaken to look into the association of the composite MetS phenotype with common SNPs in a large population of Asian Indian diaspora. The results from the study suggest that the primary genetic determinants of MetS are the same in Asian Indians as in other populations, despite the higher prevalence. Scant evidence was found of a common genetic basis for MetS traits in the Asian Indian population.[90]
DETERMINANTS AND CAUSATIVE FACTORS OF METS IN SOUTH ASIANS
The South Asians are physically less active compared to other ethnic groups. Increasing usage of computers and mechanization in workplaces and at household work is leading to a sedentary lifestyle. Leisure-time activities have also shifted from outdoor games to indoor entertainment like television and computer games. Importantly, girls and women have been found to be more sedentary than men.[14,91] Energy dense imbalanced foods (high calories, carbohydrates, saturated fats, and low fiber) are being consumed increasingly in the Indian subcontinent.[92] Asian Indians consume higher carbohydrates as compared with Europeans, and this may lead to hyperinsulinemia, postprandial hyperglycemia, high serum TG, and low HDL levels associated with insulin resistance.[93] South Asians also have significantly lower intakes of ω-3 polyunsaturated fatty acids (PUFAs), monounsaturated fatty acids (MUFAs), and higher intakes of ω-6 PUFAs than British Caucasians.[94] Overall, increasing carbohydrate and fat intake, along with decreased fiber intake is likely to contribute to obesity, the MetS, and type 2 diabetes in Asian Indians.[95]
Rapid demographic, nutritional, and economic changes are occurring in South Asians. The life expectancy and the percentage of elderly population have increased. Most importantly, globalization of diets and consumption of nontraditional fast foods have occurred at a rapid pace in urban areas. Moreover, migration from villages to cities is increasing. These intra-country migrants become urbanized and mechanized, resulting in nutritional imbalance, physical inactivity, stress, and increased consumption of alcohol and tobacco. There is a high prevalence rate of cardiovascular risk factors, including insulin resistance, obesity, atherogenic dyslipidemia, and type 2 diabetes, in these intra-country rural-to-urban migrant populations settled in urban areas.[96,97]
Although highly prevalent, vitamin D insufficient status was not associated with MetS or insulin resistance in Asian Indians of either sex.[98]
PREVENTION OF METS IN SOUTH ASIANS
“Prevention is better than cure.” The old adage holds good particularly for MetS. However, there are not many population-based interventional studies for prevention of MetS in South Asians. In order to prevent MetS, a multipronged approach is essential, which should include behavior modification, dietary modifications, increase in physical activities, prevention of smoking and alcohol excess. It has to be appreciated that though an individual-based approach may be beneficial at an individual level, we would actually need population-based community intervention programs to successfully prevent MetS.
Behavioral modification
It is essential to identify maladaptive behavior related to eating habits and rewards, especially in children and younger adults. Habits are difficult to change in older individuals. It is essential that corrective measures continue even after the achievement of a healthy lifestyle.[99]
Dietary modifications
Dietary modifications, including a reduction in intake of saturated fat and refined carbohydrates and sweetened beverages, help in modifying childhood obesity. In countries in nutritional transition, including India, it is seen that adolescents tend to favor high carbohydrate and saturated fat intake. Dietary strategies should highlight the need to stick to traditional diets and restriction of sweetened beverages, high saturated and trans fat containing food stuffs. Snacking between major meals should be discouraged. Low-fat dairy food should be encouraged. Avoidance of salted and processed food is essential to prevent hypertension.[100] Increased dietary fiber and including green leafy vegetables and fruits need to be encouraged to help prevent obesity. It is now also appreciated that nutrition during perinatal period and early childhood may influence insulin resistance and MetS in later life. Hence, maternal undernutrition and excess nutrition in children both have deleterious effects and need to be avoided.
Physical activity
Regular exercise should be promoted to increase energy expenditure and achieve weight loss and increase insulin sensitivity. Exercise is also known to reduce blood pressure, increase HDL-C and lower TG levels. Institution of physical activity needs to be gradual and graded.
Community-based interventions
Several programs have been launched to prevent obesity and MetS at a community level. These include CHETNA and MARG. The objectives of the programs are to make children aware of obesity and diabetes and educate them regarding the beneficial effects of a healthy diet and increased physical activity. The effect of these programs remains to be evaluated.[101]
Schools offer an ideal medium for lifestyle interventions because the obesogenic lifestyle behaviors are less well developed in children and are therefore amenable to change.[102] Moreover, it is important to identify the adolescents at risk for T2DM and CHD at an early age and use appropriate prevention strategies while the pathological processes are still reversible.[103,104]
A school-based program has been launched which aims to impart health education on the prevention of obesity, diabetes, and heart disease in school children, code named CHETNA (Childrens’ Health Education Through Nutrition and Health Awareness).[21] A large prospective, school-based behavioral intervention study, code named MARG (Medical education for children/Adolescents for Realistic prevention of obesity and diabetes and for healthy aGing) is being carried out in 14 cities in North India. At 6 months follow-up, significantly improved β-cell function as well as decrease in the markers of inflammation like hs-CRP were observed in the intervention group compared to the control group. The Pearson's coefficient of correlation in the intervention group showed that the decrease in the mean WC was significantly correlated with the decrease in homeostasis model assessment of insulin resistance.[104]
Behavioral intervention in migrant Asian Indian population in New Zealand showed a decrease in obesity parameters in men and blood pressure reduction in women with lifestyle changes.[105]
In another nonpharmacological community-based intervention study, reduction of fasting blood glucose levels and improved obesity measures of prediabetic and diabetic subjects from South India were seen with improvement of the dietary patterns.[106]
Pharmacological interventions
According to the current international guidelines, none of the pharmacological agents are approved for use for prevention of obesity or MetS in children. However, metformin is found to be beneficial in obese children and has effects on body composition and insulin sensitivity. Pharmacological therapy of dyslipidemia is not recommended in children less than 10 years of age.[107] As far as hypertension is concerned, a thorough search for secondary causes of hypertension in children is the need of the hour.
Community intervention programs amongst Asian Indians in South India demonstrated a relative risk reduction of 28.5% in cumulative incidence of diabetes through interventional lifestyle modification, which was higher than that achieved by metformin alone (24%).[108]
Recently, a study has been undertaken in multi-ethnic subjects with MetS for prevention of CVD and diabetes, which is called as The Reversal Intervention for Metabolic Syndrome (TRIMS) study, a double-blind placebo-controlled study on 82 participants with lifestyle intervention. The results of the study will be published in a few years, giving us an insight on the role of self-management educational programs on lifestyle intervention and their impact on the incidence of CVD and diabetes.[109]
The present definitions of the MetS bear analogy to the folklore of the six blind men and the elephant whereby each correctly describes only a part of the whole. The perfect definition of MetS would be the one which would not only be resource demanding, detect abnormalities at the earliest and in a graded manner, but would also encompasses all the clinically relevant aspects of the aforesaid syndrome. The varying relationships of the components of the MetS with CVD risk in different ethnic groups (mostly in developing countries) necessitate further studies.[110] Combating the metabolic syndrome— either as it is commonly understood or through the various components of the syndrome at the population level— is complex and requires multisectoral policy approaches. Policy changes should focus on providing balanced nutrition and an enabling environment for improving physical activity. For physicians treating individuals at high risk, aggressive lifestyle modification will remain the mainstay, until such individuals reach thresholds for drug therapy.[111]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1. [Last Accessed on 2011 Nov 25]. Available from: http://millenniumindicators.un.org/unsd/methods/m49/m49regin.htm#asia .
- 2. [Last Accessed on 2011 Nov 25]. Available from: https://www.cia.gov/library/publications/the-worldfactbook/geos/in.html .
- 3.Trivedi R, Sahoo S, Singh A, Hima Bindu G, Banerjee J, Tandon M, et al. High Resolution Phylogeographic Map of Y-Chromosomes Reveal the Genetic Signatures of Pleistocene Origin of Indian Populations. In: Bhasin V, Bhasin MK, editors. Anthropology Today: Trends, Scope and Applications. Vol. 3. New Delhi: 2007. pp. 393–414. [Google Scholar]
- 4.Misra A, Khurana L. The metabolic syndrome in South Asians: Epidemiology, determinants, and prevention. Metab Syndr Relat Disord. 2009;7:497–514. doi: 10.1089/met.2009.0024. [DOI] [PubMed] [Google Scholar]
- 5.Ramachandran A, Snehalatha C, Satyavani K, Sivasankari S, Vijay V. Metabolic syndrome in urban Asian Indian adults—A population study using modified ATP III criteria. Diabetes Res Clin Pract. 2003;60:199–204. doi: 10.1016/s0168-8227(03)00060-3. [DOI] [PubMed] [Google Scholar]
- 6.Misra A, Misra R, Wijesuriya M, Banerjee D. The metabolic syndrome in South Asians: Continuing escalation and possible solutions. Indian J Med Res. 2007;125:345–54. [PubMed] [Google Scholar]
- 7.Hydrie MZ, Shera AS, Fawwad A, Basit A, Hussain A. Prevalence of metabolic syndrome in urban Pakistan (Karachi): Comparison of newly proposed International Diabetes Federation and Modified Adult Treatment Panel III criteria. Metab Syndr Relat Disord. 2009;7:119–24. doi: 10.1089/met.2008.0055. [DOI] [PubMed] [Google Scholar]
- 8.Basit A, Shera AS. Prevalence of metabolic syndrome in Pakistan. Metab Syndr Relat Disord. 2008;6:171–5. doi: 10.1089/met.2008.0005. [DOI] [PubMed] [Google Scholar]
- 9.McKeigue PM, Shah B, Marmot MG. Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet. 1991;337:382–6. doi: 10.1016/0140-6736(91)91164-p. [DOI] [PubMed] [Google Scholar]
- 10.McKeigue PM. Metabolic consequences of obesity and body fat pattern: Lessons from migrant studies. Ciba Found Symp. 1996;201:54–64. doi: 10.1002/9780470514962.ch4. [DOI] [PubMed] [Google Scholar]
- 11.McKeigue PM, Pierpoint T, Ferrie JE, Marmot MG. Relationship of glucose intolerance and hyperinsulinaemia to body fat pattern in south Asians and Europeans. Diabetologia. 1992;35:785–91. doi: 10.1007/BF00429101. [DOI] [PubMed] [Google Scholar]
- 12.McKeigue PM, Marmot MG, Syndercombe Court YD, Cottier DE, Rahman S, Riemersma RA. Diabetes, hyperinsulinaemia, and coronary risk factors in Bangladeshis in east London. Br Heart J. 1988;60:390–6. doi: 10.1136/hrt.60.5.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tan CE, Ma S, Wai D, Chew SK, Tai ES. Can we apply the national cholesterol education program adult treatment panel definition of the metabolic syndrome to Asians? Diabetes Care. 2004;27:1182–6. doi: 10.2337/diacare.27.5.1182. [DOI] [PubMed] [Google Scholar]
- 14.Misra A, Khurana L. Obesity and the Metabolic Syndrome in developing countries. J Clin Endocrinol Metab. 2008;93:S9–30. doi: 10.1210/jc.2008-1595. [DOI] [PubMed] [Google Scholar]
- 15.Das M, Pal S, Ghosh A. Prevalence of cardiovascular disease risk factors by habitat: A study on adult Asian Indians in West Bengal, India. Anthropol Anz. 2011;68:253–64. doi: 10.1127/0003-5548/2011/0099. [DOI] [PubMed] [Google Scholar]
- 16.Kanjilal S, Shanker J, Rao VS, Khadrinarasimhaih NB, Mukherjee M, Iyengar SS, et al. Prevalence and component analysis of metabolic syndrome: An Indian atherosclerosis research study perspective. Vasc Health Risk Manag. 2008;4:189–97. doi: 10.2147/vhrm.2008.04.01.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vikram NK, Pandey RM, Misra A, Sharma R, Devi JR, Khanna N. Non-obese (body mass index < 25 kg/m2) Asian Indians with normal waist circumference have high cardiovascular risk. Nutrition. 2003;19:503–9. doi: 10.1016/s0899-9007(02)01083-3. [DOI] [PubMed] [Google Scholar]
- 18.Das M, Pal S, Ghosh A. Association of metabolic syndrome with obesity measures, metabolic profiles, and intake of dietary fatty acids in people of Asian Indian origin. J Cardiovasc Dis Res. 2010;1:130–5. doi: 10.4103/0975-3583.70911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kamble P, Deshmukh PR, Garg N. Metabolic syndrome in adult population of rural Wardha, central India. Indian J Med Res. 2010;132:701–5. [PMC free article] [PubMed] [Google Scholar]
- 20.Pemminati S, Prabha Adhikari MR, Pathak R, Pai MR. Prevalence of metabolic syndrome (METS) using IDF 2005 guidelines in a semi urban south Indian (Boloor Diabetes Study) population of Mangalore. J Assoc Physicians India. 2010;58:674–7. [PubMed] [Google Scholar]
- 21.Bhardwaj S, Misra A, Khurana L, Gulati S, Shah P, Vikram NK. Childhood obesity in Asian Indians: A burgeoning cause of insulin resistance, diabetes and sub-clinical inflammation. Asia Pac J Clin Nutr. 2008;17(Suppl 1):172–5. [PubMed] [Google Scholar]
- 22.Singh R, Bhansali A, Sialy R, Aggarwal A. Prevalence of metabolic syndrome in adolescents from a north Indian population. Diabet Med. 2007;24:195–9. doi: 10.1111/j.1464-5491.2007.02066.x. [DOI] [PubMed] [Google Scholar]
- 23.Kapil U, Kaur S. Prevalence of Pediatrics Metabolic Syndrome (PMS) amongst children in the age group of 6–18 years belonging to high income group residing in National Capital Territory (NCT) of Delhi. Indian J Pediatr. 2010;77:1041. doi: 10.1007/s12098-010-0195-x. [DOI] [PubMed] [Google Scholar]
- 24.Esteghamati A, Khalilzadeh O, Anvari M, Rashidi A, Mokhtari M, Nakhjavani M. Association of serum leptin levels with homeostasis model assessment-estimated insulin resistance and metabolic syndrome: The key role of central obesity. Metab Syndr Relat Disord. 2009;7:447–52. doi: 10.1089/met.2008.0100. [DOI] [PubMed] [Google Scholar]
- 25.Esteghamati A, Zandieh A, Zandieh B, Khalilzadeh O, Meysamie A, Nakhjavani M, et al. Leptin cut-off values for determination of metabolic syndrome: Third national surveillance of risk factors of non-communicable diseases in Iran (SuRFNCD-2007) Endocrine. 2011;40:117–23. doi: 10.1007/s12020-011-9447-4. [DOI] [PubMed] [Google Scholar]
- 26.Shah A, Hernandez A, Mathur D, Budoff MJ, Kanaya AM. Adipokines and body fat composition in South Asians: Results of the Metabolic Syndrome and Atherosclerosis in South Asians Living in America (MASALA) study. Int J Obes (Lond) 2011 doi: 10.1038/ijo.2011.167. [In press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alberti KG, Zimmet P, Shaw J. The metabolic syndrome—A new worldwide definition. Lancet. 2005;366:1059–62. doi: 10.1016/S0140-6736(05)67402-8. [DOI] [PubMed] [Google Scholar]
- 28.Deepa M, Farooq S, Datta M, Deepa R, Mohan V. Prevalence of metabolic syndrome using WHO, ATPIII and IDF definitions in Asian Indians: The Chennai Urban Rural Epidemiology Study (CURES-34) Diabetes Metab Res Rev. 2007;23:127–34. doi: 10.1002/dmrr.658. [DOI] [PubMed] [Google Scholar]
- 29.Banerji MA, Faridi N, Alturi R, Chaiken RL, Lebovitz HE. Body composition, visceral fat, leptin and insulin resistance in Asian Indian men. J Clin Endocrinol Metab. 1999;84:137–44. doi: 10.1210/jcem.84.1.5371. [DOI] [PubMed] [Google Scholar]
- 30.Chandalia M, Abate N, Garg A, Stray-Gundersen J, Grundy SM. Relationship between generalized and upper body obesity to insulin resistance in Asian Indian men. J Clin Endocrinol Metab. 1999;84:2329–35. doi: 10.1210/jcem.84.7.5817. [DOI] [PubMed] [Google Scholar]
- 31.Chowdhury B, Lantz H, Sjostrom L. Computed tomography-determined body composition in relation to cardiovascular risk factors in Indian and matched Swedish males. Metabolism. 1996;45:634–44. doi: 10.1016/s0026-0495(96)90036-0. [DOI] [PubMed] [Google Scholar]
- 32.The Asia-Pacific Perspective: Redefining Obesity and Its Treatment. Melbourne: Health Communications Australia; 2000. WHO/IASO/IOTF. [Google Scholar]
- 33.Mohan V, Deepa M, Farooq S, Narayan KM, Datta M, Deepa R. Anthropometric cut points for identification of cardiometabolic risk factors in an urban Asian Indian population. Metabolism. 2007;56:961–8. doi: 10.1016/j.metabol.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 34.Razak F, Anand SS, Shannon H, Vuksan V, Davis B, Jacobs R, et al. Defining obesity cut points in a multiethnic population. Circulation. 2007;115:2111–8. doi: 10.1161/CIRCULATIONAHA.106.635011. [DOI] [PubMed] [Google Scholar]
- 35.WHO Expert Consultation 2004. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 36.Vikram NK, Pandey RM, Misra A, Sharma R, Devi JR, Khanna N. Non-obese (body mass index <25 kg/m2) Asian Indians with normal waist circumference have high cardiovascular risk. Nutrition. 2003;19:503–9. doi: 10.1016/s0899-9007(02)01083-3. [DOI] [PubMed] [Google Scholar]
- 37.Venkataraman R, Nanda NC, Baweja G, Parikh N, Bhatia V. Prevalence of diabetes mellitus and related conditions in Asian Indians living in the United Status. Am J Cardiol. 2004;94:977–80. doi: 10.1016/j.amjcard.2004.06.048. [DOI] [PubMed] [Google Scholar]
- 38.Mohan V, Mathur P, Deepa R, Deepa M, Shukla DK, Menon GR, et al. Urban rural differences in prevalence of self-reported diabetes in India – The WHO-ICMR Indian NCD risk factor surveillance. Diabetes Res Clin Pract. 2008;80:159–68. doi: 10.1016/j.diabres.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 39.Ranjith N, Pegoraro RJ, Naidoo DP, Shanmugam R, Rom L. Genetic variants associated with insulin resistance and metabolic syndrome in young Asian Indians with myocardial infarction. Metab Syndr Relat Disord. 2008;6:209–14. doi: 10.1089/met.2008.0023. [DOI] [PubMed] [Google Scholar]
- 40.Ma S, Cutter J, Tan CE, Chew SK, Tai ES. Associations of diabetes mellitus and ethnicity with mortality in a multiethnic Asian population: Data from the1992 Singapore National Health Survey. Am J Epidemiol. 2003;158:543–52. doi: 10.1093/aje/kwg199. [DOI] [PubMed] [Google Scholar]
- 41.Eapen D, Kalra GL, Merchant N, Arora A, Khan BV. Metabolic syndrome and cardiovascular disease in South Asians. Vasc Health Risk Manag. 2009;5:731–43. doi: 10.2147/vhrm.s5172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gupta R, Prakash H, Kaul V. Cholesterol lipoproteins, triglycerides, rural-urban differences and prevalence of dyslipidaemia among males in Rajasthan. J Assoc Physicians India. 1997;45:275–9. [PubMed] [Google Scholar]
- 43.Gama R, Elfatih AB, Anderson NR. Ethnic differences in total and HDL cholesterol concentrations: Caucasians compared with predominantly Punjabi Sikh Indo-Asians. Ann Clin Biochem. 2002;39:609–11. doi: 10.1177/000456320203900612. [DOI] [PubMed] [Google Scholar]
- 44.Hodge AM, Dowse GK, Collins VR, Alberti KG, Gareeboo H, Tuomilehto J, et al. Abdominal fat distribution and insulin levels only partially explain adverse cardiovascular risk profile in Asian Indians. J Cardiovasc Risk. 1996;3:263–70. [PubMed] [Google Scholar]
- 45.Reddy KS. Primordial prevention of coronary heart disease in India: Challenges and opportunities. Prev Med. 1999;29:S119–23. doi: 10.1006/pmed.1998.0437. [DOI] [PubMed] [Google Scholar]
- 46.Reddy KK, Ramachandraiah T, Reddanna P, Thyagaraju K. Serum lipid peroxides and lipids in urban and rural Indian men. Arch Environ Health. 1994;49:123–7. doi: 10.1080/00039896.1994.9937465. [DOI] [PubMed] [Google Scholar]
- 47.McLaughlin T, Reaven G, Abbasi F, Lamendola C, Saad M, Waters D, et al. Is there a simple way to identify insulin resistant individuals at increased risk of cardiovascular disease? Am J Cardiol. 2005;96:399–404. doi: 10.1016/j.amjcard.2005.03.085. [DOI] [PubMed] [Google Scholar]
- 48.Diabetes Prevention Program Research Group. Hypertension, insulin, and proinsulin in participants with impaired glucose tolerance. Hypertension. 2002;40:679–86. doi: 10.1161/01.hyp.0000035706.28494.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Garcia-Puig J, Ruilope LM, Luque M, Fernandez J, Ortega R, Dal-Re R. Glucose metabolism in patients with essential hypertension. Am J Med. 2006;119:318–26. doi: 10.1016/j.amjmed.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 50.Cappuccio FP. Ethnicity and cardiovascular risk: Variations in people of African ancestry and South Asian origin. J Hum Hypertens. 1997;11:571–6. doi: 10.1038/sj.jhh.1000516. [DOI] [PubMed] [Google Scholar]
- 51.Khattar RS, Swales JD, Senior R, Lahiri A. Racial variation in cardiovascular morbidity and mortality in essential hypertension. Heart. 2000;83:267–71. doi: 10.1136/heart.83.3.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Misra A. Impact of ethnicity on body fat patterning in Asian Indians and Blacks: Relationship with insulin resistance. Nutrition. 2003;19:815–6. doi: 10.1016/s0899-9007(03)00141-2. [DOI] [PubMed] [Google Scholar]
- 53.Misra A, Vikram NK, Arya S, Pandey RM, Dhingra V, Chatterjee A, et al. High prevalence of insulin resistance in postpubertal Asian Indian children is associated with adverse truncal body fat patterning, abdominal adiposity and excess body fat. Int J Obes Relat Metab Disord. 2004;28:1217–26. doi: 10.1038/sj.ijo.0802704. [DOI] [PubMed] [Google Scholar]
- 54.Yajnik CS, Lubree HG, Rege SS, Naik SS, Deshpande JA, Deshpande SS, et al. Adiposity and hyperinsulinemia in Indians are present at birth. J Clin Endocrinol Metab. 2002;87:5575–80. doi: 10.1210/jc.2002-020434. [DOI] [PubMed] [Google Scholar]
- 55.Misra A, Athiko D, Sharma R, Pandey RM, Khanna N. Non-obese hyperlipidemic Asian northern Indian males have adverse anthropometric profile. Nutr Metab Cardiovasc Dis. 2002;12:178–83. [PubMed] [Google Scholar]
- 56.Kamath SK, Hussain EA, Amin D, Mortillaro E, West B, Peterson CT, et al. Cardiovascular disease risk factors in 2 distinct ethnic groups: Indian and Pakistani compared with American premenopausal women. Am J Clin Nutr. 1999;69:621–31. doi: 10.1093/ajcn/69.4.621. [DOI] [PubMed] [Google Scholar]
- 57.Misra A, Wasir JS, Pandey RM. An evaluation of candidate definitions of the metabolic syndrome in adult Asian Indians. Diabetes Care. 2005;28:398–403. doi: 10.2337/diacare.28.2.398. [DOI] [PubMed] [Google Scholar]
- 58.Vikram NK, Misra A, Pandey RM, Luthra K, Wasir JS, Dhingra V. Heterogeneous phenotypes of insulin resistance and its implications for defining metabolic syndrome in Asian Indian adolescents. Atherosclerosis. 2006;186:193–9. doi: 10.1016/j.atherosclerosis.2005.07.015. [DOI] [PubMed] [Google Scholar]
- 59.Misra A, Sinha S, Kumar M, Jagannathan NR, Pandey RM. Proton magnetic resonance spectroscopy study of soleus muscle in non-obese healthy and type 2 diabetic Asian Northern Indian males: High intramyocellular lipid content correlates with excess body fat and abdominal obesity. Diabet Med. 2003;20:361–7. doi: 10.1046/j.1464-5491.2003.00932.x. [DOI] [PubMed] [Google Scholar]
- 60.Forouhi NG, Jenkinson G, Thomas EL, Mullick S, Mierisova S, Bhonsle U, et al. Relation of triglyceride stores in skeletal muscle cells to central obesity and insulin sensitivity in European and South Asian men. Diabetologia. 1999;42:932–5. doi: 10.1007/s001250051250. [DOI] [PubMed] [Google Scholar]
- 61.Farrell GC. Non-alcoholic steatohepatitis: What is it, and why is it important in the Asia-Pacific region? J Gastroenterol Hepatol. 2003;18:124–38. doi: 10.1046/j.1440-1746.2003.02989.x. [DOI] [PubMed] [Google Scholar]
- 62.Misra A, Jaiswal A, Shakti D, Wasir J, Vikram NK, Pandey RM, et al. Novel phenotypic markers and screening score for the metabolic syndrome in adult Asian Indians. Diabetes Res Clin Pract. 2008;79:e1–5. doi: 10.1016/j.diabres.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 63.Denzer C, Muche R, Mayer H, Heinze E, Debatin KM, Wabitsch M. Serum uric acid levels in obese children and adolescents: Linkage to testosterone levels and pre-metabolic syndrome. J Pediatr Endocrinol Metab. 2003;16:1225–32. doi: 10.1515/jpem.2003.16.9.1225. [DOI] [PubMed] [Google Scholar]
- 64.Abate N, Chandalia M, Cabo-Chan AV, Jr, Moe OW, Sakhaee K. The metabolic syndrome and uric acid nephrolithiasis: Novel features of renal manifestation of insulin resistance. Kidney Int. 2004;65:386–92. doi: 10.1111/j.1523-1755.2004.00386.x. [DOI] [PubMed] [Google Scholar]
- 65.Wijeyaratne CN, Balen AH, Barth JH, Belchetz PE. Clinical manifestations and insulin resistance (IR) in polycystic ovary syndrome (PCOS) among South Asians and Caucasians: Is there a difference? Clin Endocrinol (Oxf) 2002;57:343–50. doi: 10.1046/j.1365-2265.2002.01603.x. [DOI] [PubMed] [Google Scholar]
- 66.Forouhi NG, Sattar N, McKeigue PM. Relation of C-reactive protein to body fat distribution and features of the metabolic syndrome in Europeans and South Asians. Int J Obes Relat Metab Disord. 2001;25:1327–31. doi: 10.1038/sj.ijo.0801723. [DOI] [PubMed] [Google Scholar]
- 67.Vikram NK, Misra A, Dwivedi M, Sharma R, Pandey RM, Luthra K, et al. Correlations of C-reactive protein levels with anthropometric profile, percentage of body fat and lipids in healthy adolescents and young adults in urban North India. Atherosclerosis. 2003;168:305–13. doi: 10.1016/s0021-9150(03)00096-0. [DOI] [PubMed] [Google Scholar]
- 68.Vikram NK. Adiponectin, insulin resistance, and C-reactive protein in postpubertal Asian Indian adolescents. Metabolism. 2004;53:1336–41. doi: 10.1016/j.metabol.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 69.Sattar N, McConnachie A, Shaper AG, Blauw GJ, Buckley BM, de Craen AJ, et al. Can metabolic syndrome usefully predict cardiovascular disease and diabetes? Outcome data from two prospective studies. Lancet. 2008;371:1927–35. doi: 10.1016/S0140-6736(08)60602-9. [DOI] [PubMed] [Google Scholar]
- 70.Misra A, Wasir JS, Vikram NK. Waist circumference criteria for the diagnosis of abdominal obesity are not applicable uniformly to all populations and ethnic groups. Nutrition. 2005;21:969–76. doi: 10.1016/j.nut.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 71.Mehta S. Relationship between measures of fatness, lipids and ethnicity in a cohort of adolescent boys. Ann Nutr Metab. 2002;46:192–9. doi: 10.1159/000065406. [DOI] [PubMed] [Google Scholar]
- 72.Deurenberg-Yap M, Chew SK, Deurenberg P. Elevated body fat percentage and cardiovascular risks at low body mass index levels among Singaporean Chinese, Malays and Indians. Obes Rev. 2002;3:209–15. doi: 10.1046/j.1467-789x.2002.00069.x. [DOI] [PubMed] [Google Scholar]
- 73.Yeolekar ME. Coronary artery disease in Asian Indians. J Postgrad Med. 1998;44:26–8. [PubMed] [Google Scholar]
- 74.Bhopal R, Unwin N, White M, Yallop J, Walker L, Alberti KG, et al. Heterogeneity of coronary heart disease risk factors in Indian, Pakistani, Bangladeshi, and European origin populations: Cross sectional study. BMJ. 1999;319:215–20. doi: 10.1136/bmj.319.7204.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Murray CJ, Lopez AD. Evidence-based health policy – Lessons from the Global Burden of Disease Study. Science. 1996;274:740–3. doi: 10.1126/science.274.5288.740. [DOI] [PubMed] [Google Scholar]
- 76.Sheth T, Nair C, Nargundkar M, Anand S, Yusuf S. Cardiovascular and cancer mortality among Canadians of European, south Asian and Chinese origin from 1979 to 1993: An analysis of 1.2 million deaths. CMAJ. 1999;161:132–8. [PMC free article] [PubMed] [Google Scholar]
- 77.Kurpad SS, Tandon H, Srinivasan K. Waist circumference correlates better with Body Mass Index than Waist to Hip ratio in Asian Indians. Natl Med J India. 2003;16:89–92. [PubMed] [Google Scholar]
- 78.Raji A, Seely EW, Arky RA, Simonson DC. Body fat distribution and insulin resistance in healthy Asian Indians and Caucasians. J Clin Endocrinol Metab. 2001;86:5366–71. doi: 10.1210/jcem.86.11.7992. [DOI] [PubMed] [Google Scholar]
- 79.Misra A, Khurana L. Obesity-related non-communicable diseases: South Asians vs Caucasians. Int J Obes (Lond) 2011;35:167–87. doi: 10.1038/ijo.2010.135. [DOI] [PubMed] [Google Scholar]
- 80.Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288:2709–16. doi: 10.1001/jama.288.21.2709. [DOI] [PubMed] [Google Scholar]
- 81.Lorenzo C, Williams K, Hunt KJ, Haffner SM. The National Cholesterol Education Program–Adult treatment Panel III, International Diabetes Federation, and World Health Organization definitions of the metabolic syndrome as predictors of incident cardiovascular disease and diabetes. Diabetes Care. 2007;30:8–13. doi: 10.2337/dc06-1414. [DOI] [PubMed] [Google Scholar]
- 82.Forouhi NG, Sattar N, Tillin T, McKeigue PM, Chaturvedi N. Do known risk factors explain the higher coronary heart disease mortality in South Asian compared with European men? Prospective follow-up of the Southall and Brent studies, UK. Diabetologia. 2006;49:2580–8. doi: 10.1007/s00125-006-0393-2. [DOI] [PubMed] [Google Scholar]
- 83.Guettier JM, Georgopoulos A, Tsai MY, Radha V, Shanthirani S, Deepa R, et al. Polymorphisms in the fatty acid-binding protein 2 and apolipoprotein C-III genes are associated with the metabolic syndromeand dyslipidemia in a South Indian population. J Clin Endocrinol Metab. 2005;90:1705–11. doi: 10.1210/jc.2004-1338. [DOI] [PubMed] [Google Scholar]
- 84.Ranjith N, Pegoraro RJ, Shanmugam R. Obesity-associated genetic variants in young Asian Indians with the metabolic syndrome and myocardial infarction. Cardiovasc J Afr. 2011;22:25–30. doi: 10.5830/CVJA-2010-036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ranjith N, Pegoraro RJ, Rom L. Lipid profiles and associated gene polymorphisms in young Asian Indian patients with acute myocardial infarction and the metabolic syndrome. Metab Syndr Relat Disord. 2009;7:571–8. doi: 10.1089/met.2009.0015. [DOI] [PubMed] [Google Scholar]
- 86.Dodani S, Henkhaus R, Wick J, Vacek J, Gupta K, Dong L, et al. Metabolic syndrome in South Asian immigrants: More than low HDL requiring aggressive management. Lipids Health Dis. 2011;10:45. doi: 10.1186/1476-511X-10-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zabaneh D, Chambers JC, Elliott P, Scott J, Balding DJ, Kooner JS. Heritability and genetic correlations of insulin resistance and component phenotypes in Asian Indian families using a multivariate analysis. Diabetologia. 2009;52:2585–9. doi: 10.1007/s00125-009-1504-7. [DOI] [PubMed] [Google Scholar]
- 88.Benyamin B, Sorensen TI, Schousboe K, Fenger M, Visscher PM, Kwik KO. Are there common genetic and environmental factors behind the endophenotypes associated with the Metabolic syndrome? Diabetologia. 2007;50:1880–8. doi: 10.1007/s00125-007-0758-1. [DOI] [PubMed] [Google Scholar]
- 89.Sjogren M, Lyssenko V, Jonsson A, Berglund G, Nilsson P, Groop L, et al. The search for putative unifying genetic factors for components of the metabolic syndrome. Diabetologia. 2008;51:2242–51. doi: 10.1007/s00125-008-1151-4. [DOI] [PubMed] [Google Scholar]
- 90.Zabaneh D, Balding DJ. A Genome-Wide Association study of the metabolic syndrome in Indian Asian Men. PLoS ONE. 2010;5:e11961. doi: 10.1371/journal.pone.0011961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Misra A, Vikram NK. Insulin resistance syndrome (metabolic syndrome) and obesity in Asian Indians. Evidence and implications. Nutrition. 2004;20:482–91. doi: 10.1016/j.nut.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 92.Wasir JS, Misra A. The metabolic syndrome in Asian Indians: The impact of nutritional and socio-economic transition in India. Metab Syndr Relat Disord. 2004;2:14–23. doi: 10.1089/met.2004.2.14. [DOI] [PubMed] [Google Scholar]
- 93.Burden ML, Samanta A, Spalding D, Burden AC. A comparison of the glycaemic and insulinaemic effects of an Asian and a European meal. Pract Diabetes Int. 1994;11:208–11. [Google Scholar]
- 94.Sevak L, McKeigue PM, Marmot MG. Relationship of hyperinsulinemia to dietary intake in south Asian and European men. Am J Clin Nutr. 1994;59:1069–74. doi: 10.1093/ajcn/59.5.1069. [DOI] [PubMed] [Google Scholar]
- 95.Misra A, Khurana L, Isharwal S, Bhardwaj S. South Asian diets and insulin resistance. Br J Nutr. 2009;10:465–73. doi: 10.1017/S0007114508073649. [DOI] [PubMed] [Google Scholar]
- 96.Misra A, Pandey RM, Devi JR, Sharma R, Vikram NK, Khanna N. High prevalence of diabetes, obesity and dyslipidaemia in urban slum population in northern India. Int J Obes Relat Metab Disord. 2001;25:1722–9. doi: 10.1038/sj.ijo.0801748. [DOI] [PubMed] [Google Scholar]
- 97.Misra A, Pandey RM, Sharma R. Non-communicable diseases (diabetes, obesity and hyperlipidaemia) in urban slums. Natl Med J India. 2002;15:242–4. [PubMed] [Google Scholar]
- 98.Majumdar V, Nagaraja D, Christopher R. Vitamin D status and Metabolic Syndrome in Asian Indians. Int J Obes (Lond) 2011;35:1131–4. doi: 10.1038/ijo.2010.232. [DOI] [PubMed] [Google Scholar]
- 99.Misra A, Khurana L, Vikram NK, Goel A, Wasir JS. Metabolic syndrome in children: Current issues and South Asian perspective. Nutrition. 2007;23:895–910. doi: 10.1016/j.nut.2007.08.018. [DOI] [PubMed] [Google Scholar]
- 100.Misra A, Singhal N, Sivakumar B, Bhagat N, Jaiswal A, Khurana L. Nutrition transition in India: Secular trends in dietary intake and their relationship to diet-related non-communicable diseases. J Diabetes. 2011;3:278–92. doi: 10.1111/j.1753-0407.2011.00139.x. [DOI] [PubMed] [Google Scholar]
- 101.World Diabetes Foundation. Primary prevention in Indian schools. [Last Accessed on 2011 Nov 25]. Available from: http://www.worlddiabetesfoundation.org/composite-1279.htm .
- 102.Bhatia V. IAP National Task Force for Childhood Prevention of Adult Diseases: Insulin resistance and type 2 diabetes mellitus in childhood. Indian Pediatr. 2004;41:443–57. [PubMed] [Google Scholar]
- 103.Warnberg J, Marcos A. Low-grade inflammation and the metabolic syndrome in children and adolescents. Curr Opin Lipidol. 2008;19:11–5. doi: 10.1097/MOL.0b013e3282f4096b. [DOI] [PubMed] [Google Scholar]
- 104.Singhal N, Misra A, Shah P, Gulati S, Bhatt S, Sharma S, et al. Impact of intensive school-based nutrition education and lifestyle interventions on insulin resistance, β-cell function, disposition index, and subclinical inflammation among Asian Indian adolescents: A controlled intervention study. Metab Syndr Relat Disord. 2011;9:143–50. doi: 10.1089/met.2010.0094. [DOI] [PubMed] [Google Scholar]
- 105.Rush EC, Chandu V, Plank LD. Reduction of abdominal fat and chronic disease factors by lifestyle change in migrant Asian Indians older than 50 years. Asia Pac J Clin Nutr. 2007;16:671–6. [PubMed] [Google Scholar]
- 106.Balagopal P, Kamalamma N, Patel TG, Misra R. A community based diabetes prevention and management education program in a rural village in India. Diabetes Care. 2008;31:1097–104. doi: 10.2337/dc07-1680. [DOI] [PubMed] [Google Scholar]
- 107.Tuomilehto J. Cardiovascular risk: Prevention and treatment of metabolic syndrome. Diabetes Res Clin Pract. 2005;68(Suppl 2):S28–35. doi: 10.1016/j.diabres.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 108.Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1) Diabetologia. 2006;49:289–97. doi: 10.1007/s00125-005-0097-z. [DOI] [PubMed] [Google Scholar]
- 109.Dunkley AJ, Davies MJ, Stone MA, Taub NA, Troughton J, Yates T, et al. The Reversal Intervention for Metabolic Syndrome (TRIMS) study: Rationale, design, and baseline data. Trials. 2011;12:107. doi: 10.1186/1745-6215-12-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gale EA. The myth of the metabolic syndrome. Diabetologia. 2005;48:1679–83. doi: 10.1007/s00125-005-1873-5. [DOI] [PubMed] [Google Scholar]
- 111.Prabhakaran D, Reddy KS. The metabolic syndrome: Looking beyond the debates. Clin Pharmacol Ther. 2011;90:19–21. doi: 10.1038/clpt.2011.116. [DOI] [PubMed] [Google Scholar]


