Abstract
Metabolic syndrome is a clustering of several cardiovascular risk factors. Contrary to earlier thoughts, metabolic syndrome is no longer rare in Africa. The prevalence is increasing, and it tends to increase with age. This increase in the prevalence of metabolic syndrome in the continent is thought to be due to departure from traditional African to western lifestyles. In Africa, it is not limited to adults but is also becoming common among the young ones. Obesity and dyslipidemia seem to be the most common occurring components. While obesity appears more common in females, hypertension tends to be more predominant in males. Insulin resistance has remained the key underlying pathophysiology. Though pharmacologic agents are available to treat the different components of the syndrome, prevention is still possible by reverting back to the traditional African way of life.
Keywords: Africa, insulin resistance, metabolic syndrome
INTRODUCTION
The term “metabolic syndrome” is a subject that has received much attention in the recent times, due to increasing awareness of its association with cardiovascular morbidity and mortality. However, it is a concept that dates back to over 5 decades now. Its existence was first observed as clustering of hypertension, hyperglycemia, and gout as described by Kylin in the 1920s. Later, r, Jean Vague in 1947 noted its association with android obesity.[1–3] The effect of hypocaloric, low-carbohydrate diet on obese patients with diabetes, hypercholesterolemia, and hypertriglyceridaemia was later reported by Avogadro, Crepaldi, and co-workers.[1,4] Other important historical developments include the use of the term “metabolic syndrome” by H. Haller in 1977 to describe the associations of obesity, diabetes mellitus, hyperlipoproteinemia, hyperuricemia, and hepatic steatosis when highlighting the additive effects of risk factors on atherosclerosis.[5] Singer also in 1977 used the term for associations of obesity, gout, diabetes mellitus, and hypertension with hyperlipoproteinemia.[6] In 1977 and 1978, Phillips developed the concept that risk factors for myocardial infarction form a “constellation of abnormalities” that is associated not only with heart disease but also with aging, obesity, and other clinical states. These abnormalities included glucose intolerance, hyperinsulinemia, hypercholesterolemia, hypertriglyceridemia, and hypertension.[7,8] In 1988, in his Banting lecture, Reaven proposed insulin resistance as the underlying factor and named the constellation of abnormalities, Syndrome X.[9] This however did not include abdominal obesity. The syndrome has been variously called “The Deadly Quartet” by Kaplan and “The Insulin Resistance Syndrome.”[10,11] Notwithstanding the various aforementioned evolutionary nomenclatures, the term “metabolic syndrome” has remained widely accepted, and currently is the term that is in use globally.
DEFINITION OF METABOLIC SYNDROME
Metabolic syndrome is a constellation of interrelated risk factors of metabolic origin (metabolic risk factors) that appear to directly promote the development of atherosclerotic cardiovascular disease. The primary components of metabolic syndrome included insulin resistance, obesity, dyslipidemia, and hypertension but with continuing emergence of new facts, the list tends to be growing. The components therefore now include insulin resistance, hyperinsulinemia, central obesity, hypertension, dyslipidemia (increase in plasma triglycerides (TG)), decrease in high density lipoprotein cholesterol (HDL-C), an LDL particle pattern shifted to small dense particles (type B pattern)), procoagulant state (increased plasma fibrinogen, increased plasminogen activator inhibitor-1 (PAI-1)), vascular abnormalities (increase in urinary albumin excretion, endothelial dysfunction), inflammatory markers, and hyperuricemia.[12,13]
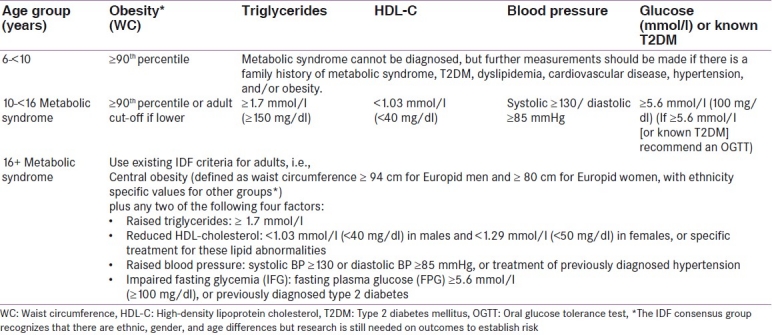
The wide interest generated by this subject has resulted in several definitions being put forward by different expert groups [Table 1].[14–16] These definitions indicate attempts that have been made to describe the syndrome from various perspectives of the expert groups but despite all these no unified definition has been adopted. The quest to fill this gap for a unified worldwide definition resulted in the definition proposed by the International Diabetes Federation (IDF). This was the outcome of a consensus workshop held from May 12 to 14 2004 in London, UK.[1] The IDF also realized that there are still some unanswered questions; hence areas for future research to help describe the syndrome better were identified. These areas for future research can be grouped into epidemiologic, clinical, and biochemical characterization.[15] Due to its continued evolution and other reasons, debate is still ongoing in some quarters about the usefulness of the syndrome.[16]
Table 1.
Summary of the diagnostic criteria for the metabolic syndrome as proposed by different expert groups[17]
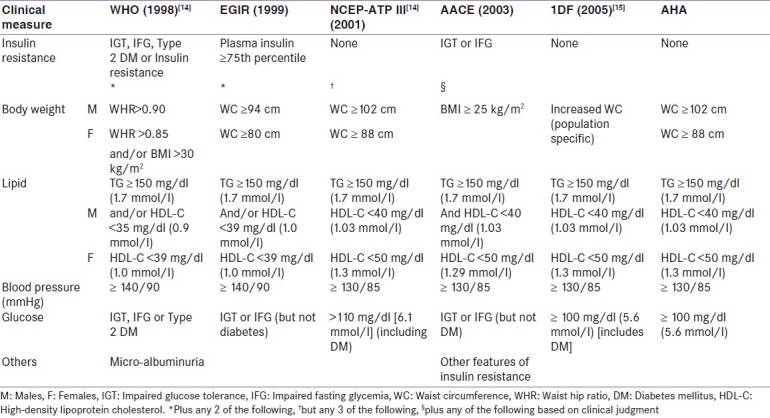
These definitions can be broadly grouped into those which require the measurement of insulin resistance and those which do not. For those which require measurement of insulin resistance, a major drawback is that measurement of insulin resistance by the gold standard method cannot be routinely done. Definitions which can easily be applied in a routine clinic setting and do not require measurement of insulin resistance (NCEP, ACE, and IDF) were shown by Can and Bersot[18] to be more useful than those requiring measurement of insulin levels (WHO and EGIR) as they identified twice more patients with insulin resistance and increased Framingham risk scores. Recently in conjunction with representatives from the World Heart Federation, International Atherosclerosis Society, and International Association for the Study of Obesity, a revised set of criteria harmonizing the definition of the metabolic syndrome were published.[19] These “consensus criteria” again included the same five components, but did not designate any component as required. It however still recommended the use of ethnic or country-specific cutoff points for central obesity.
The different definitions were evaluated in a cross-sectional, methodological study of 1568 Turkish nondiabetic subjects and it was found that the agreement between WHO and EGIR definitions was very good (kappa: 0.83) while that between NCEP, ACE, and IDF definitions was substantial to very good (kappa: 0.77-0.84). The agreement between NCEP or ACE or IDF and WHO or EGIR definitions was fair (kappa: 0.32-0.37).[18]
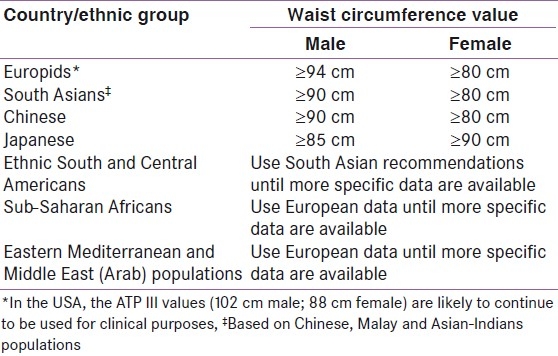
Several of these definitions have been used by people working among Africans and people of African descent who live among other populations, but none of the expert groups is of African origin. As the awareness of the syndrome and its consequences is fast growing among healthcare professionals, especially at the tertiary healthcare level, there is a great need for large scale research in order to characterize the syndrome further, as IDF proposed, especially in Africans.[15] Consequently, it may be difficult at this point for consensus opinion to be developed on the definition of metabolic syndrome in Africans. Lack of data applicable to Africans and some other ethnic populations of the world is reflected, for instance, in the nonavailability of ethnic-specific waist circumference cutoff threshold as proposed by the IDF in her definition of metabolic syndrome [Table 2].[15] Studies carried out among African populations still utilize the available definitions based on thresholds derived from western populations. The need for research on epidemiology of metabolic syndrome and other cardiometabolic disorders among Africans therefore cannot be overemphasized. Longo-Mbenza et al.,[20] for instance, suggested the inclusion of low birth weight, coronary heart disease, malnutrition, elevated fibrinogen, total cholesterol, and urea nitrogen as additional components of metabolic syndrome in the African patients born between 1930 and 1945.
Table 2.
Ethnic-specific values for waist circumference according to International Diabetes Federation[15]
PREVALENCE OF METABOLIC SYNDROME - EMERGING DATA FROM AFRICA
Africa is a large continent occupied by several nations or ethnic groups. Patterns of diseases in many nations understandably vary by ethnicity because of possible cultural differences.[21] Several decades ago, the burden of diseases among African populations was from infectious diseases. Cardiovascular disorders were then seen as rare among these populations but today, these nations are witnessing epidemiological transition which has placed on them a double burden of disease. This implies that while infections and infestations are still a major health burden in these countries, noncommunicable diseases have also become a problem.. Early in the century, the point prevalence rate of diabetes mellitus in Africa was 0-1% but today available data show that this is no longer the position.[22,23] Prevalence trend of diabetes as an example is on the rise when early reports are compared to the IDF estimates (2-5%) and other reported prevalence rates from African countries such as Benin (3%), Mauritania (6%), Cameroon (6.1%), Congo (7.1%), Zimbabwe (10.2%), Democratic Republic of Congo (14.5%), Nigeria (2.2%).[24–26] In most of these studies, diagnosis is based on fasting blood glucose concentration measured using capillary, whole blood, or venous plasma.
Metabolic syndrome is becoming common in Africans too, contrary to the earlier trend of being considered rare.[27–32] The prevalence of metabolic syndrome among a group of hypertensive Nigerians was found to be 34.3% (ATP III), 35% (WHO), and 42.9% (IDF).[27] These values generally were similar to that which emerged from nondiabetic Turkish adults where the prevalence rates were as follows: 38% (NCEP-ATP III), 42% (ACE and IDF), 20% (EGIR), and 19% (WHO).[18] These rates favorably compared to those observed in Canada.[33]
The prevalence of the metabolic syndrome varies between different populations. It is known to be high in developed nations because of increased physical inactivity and consumption of energy-laden foods, which thus lead to high rates of obesity. In the general population, the prevalence of metabolic syndrome is estimated to be between 17% and 25%.When cohorts of subjects already having cardiovascular risk such as hypertension or diabetes are evaluated, it becomes higher as was demonstrated in Caucasians with type 2 diabetes mellitus where the prevalence was 75.6%.[28–30] The increase in the number of people suffering from diabetes and its inclusion in the definition of metabolic syndrome by some expert groups may be responsible for the very high rate seen in diabetic subjects.
The prevalence of metabolic syndrome in African populations ranges from as low as 0% to as high as about 50% or even higher depending on the population setting.[31,30] The trend is similar to that obtained in developed nations. Some data on characterization of metabolic syndrome among Africans as reported in various literatures are shown in Table 3.[27,29–31,34–40]
Table 3.
Prevalence of metabolic syndrome from some African studies
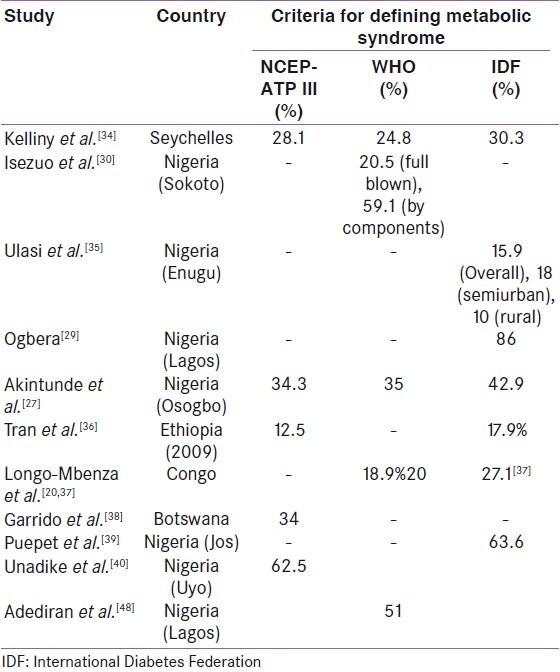
These studies focused mainly on the prevalence of metabolic syndrome and analyses of its components in different African populations using different criteria. Though the use of different criteria is a limitation on comparison of these findings, they are still informative about the burden of metabolic syndrome in Africans. Reports from Lagos, Nigeria, for instance, showed the prevalence rate of metabolic syndrome as high as over 80% among diabetic patients, similar to rates in Caucasians.[28,29] The current trend of increase in the prevalence of metabolic syndrome is largely and generally attributed to adoption of western lifestyle which is characterized by reduced physical activity, substitution of the traditional African diet rich in fruits, and vegetables for the more energy-laden foods.[32]
Prevalence based on settings
Comparatively, metabolic syndrome appears to be more common in the presence of diabetes mellitus than hypertension.[30,41,42] Among diabetic subjects, the prevalence was as high as 80% whereas it was 21.2% among hypertensive subjects but varying with place of domicile (rural or semiurban).[28,29,34,35] This is likely to be due to the close association of diabetes with insulin resistance, which still remains the pathogenic hallmark of metabolic syndrome.[9,43] In Africa, metabolic syndrome was found to be more common in females and to increase with age, and urban dwelling.[32,35,44]
Components of metabolic syndrome
The prevalence of metabolic syndrome varies with the number of components present in an individual. In Nigeria, using the WHO criteria, full blown metabolic syndrome (i.e., presence of all the major components) was found in 25.1% of type 2 diabetic subjects whereas using different combinations of the components the prevalence rate rose to 56%.[30] No clear trend has been demonstrated in Africans on the pattern and frequency of the metabolic syndrome components. In Cameroon, 1573 adults (638 rural, 935 urban dwellers) aged 24–74 years were studied.[31] The clustering of the components was assessed using the NCEP-ATP III definition. For two components, the most frequent combinations were central obesity and high blood pressure (81% in women and 52% in men), high blood pressure and hypercholesterolemia (6% in women and 24% in men), high blood pressure and hyperglycemia (6% in women and 12% in men). Two combinations of three components were found, namely central obesity, high blood pressure, high cholesterol, and high blood pressure (100% in women), high blood glucose, high triglycerides. No subject had four components. Central obesity being the most common component in the study was reported to be the key determinant, becoming detected most often in rural and urban dwellers using WHR (WHO) and WC (NCEP/IDF) respectively. Similarly, obesity was also the most common component in Benin where diabetes mellitus and hypertriglyceridemia were noted to be uncommon.[45]
Dyslipidemia
Dyslipidemia has been commonly demonstrated in subjects with metabolic syndrome.[30,38,46] Reduced HDL-C and hypertriglyceridemia are the two main types of dyslipidemia associated with metabolic syndrome. Dyslipidemia manifesting as reduced HDL-C was extremely common as demonstrated in Nigeria (72.4%, 70%, 88%) and Botswana (80%).[30,38,46] Hypertriglyceridemia has also been demonstrated to contribute to dyslipidemia in Africans with metabolic syndrome but its contribution seems to be less frequent than reduced HDL-C as demonstrated in Botswana (14%) and Nigeria (Uyo: 17.3%, Lagos: 25%).[38,40,46] In Cameroon and Cotonou, hypertriglyceridemia was described also as being low or uncommon.[31,45] This pattern of dyslipidemia varied from the findings in north central Nigeria where a relatively high rate (62%) of raised TG was found.[39] Though not used in the definition of metabolic syndrome, LDL-C was found to be the most common lipid abnormality followed by reduced HDL-C which occurred in about 60% of the subjects as reported by Ogbera.[29] There is a great need for dyslipidemia to be addressed because it is becoming common in apparently healthy populations.[47]
Obesity
Obesity is another major component that characterizes metabolic syndrome. Obesity is the accumulation of excess body fat, which manifests as increased weight or waist circumference. It is commonly associated with insulin resistance. The contribution of obesity (generalized or central) to the definition of the metabolic is emphasized by its inclusion by all the expert groups in the definition of metabolic syndrome. The central role of obesity in metabolic syndrome in Africans was demonstrated in the study by Fezeu et al. in Cameroon, thus bringing to the fore again, the need for ethnic-specific cutoff values for waist circumference in the people of African descent as suggested by IDF.[31]
In Cameroon, central obesity determined using WHR (WHR > 0.9 and 0.85 for males and females respectively) was more common in rural dwellers while that determined using WC (as defined by both NCEP and IDF) was more common in urban dwellers.[31] In Africans, obesity seems to be more common when WHR is used but in a comparative study of apparently healthy individuals, WC was shown to have a better performance as an index of central obesity.[48–50] Central obesity (32%) defined according WHO classification as WC ≥ 102 cm and ≥ 88 cm for males and females, respectively, was demonstrated to be more common than generalized obesity (18%) (BMI ≥ 30 kg/m2) in Cotonou, Benin, while in Gambia using BMI (≥30 kg/m2), obesity was also reported to be higher in females with a prevalence rate of 32.8%.[45,51] Studies from Nigeria, which involved semiurban and rural communities, demonstrated high rates of obesity ranging from about 40% (rural/semiurban communities) to 80% (urban communities).[35,30,39] These studies defined overweight and obesity using BMI of ≥25 to 29.9 kg/m2 and ≥ 30 kg/m2, respectively. Central obesity was defined based on IDF criteria[35,39] and NCEP criteria.[30]
In Africa it has been observed that unhealthy weight gain (obesity and overweight) and metabolic syndrome are not limited to the adult population. Adolescents and young people are also affected. Metabolic syndrome was found in 7.4% of Egyptian adolescents, with about 25% of them who have different combinations of metabolic syndrome components having full blown (≥3 components) metabolic syndrome.[52] Obesity in young people is not new in the western world but its presence in the young Africans is a trend that should be a major public health concern. This is because if unchecked the consequences may be grave in the face of inadequate facilities and poverty which many African nations still face today. About 10% of South African women aged between 15 years and 24 years, in the South African Demographic Health Survey (SADHS), were already considered obese.[53] Similarly, in the Youth Risk Behaviour Survey (n=9 054), conducted in 2002, over 17% of adolescents were overweight while 4.2% were obese.[54] In Nigeria, a low prevalence of obesity in males at the age of 16 years (0.9-2.7%) and females (0 and 1.9%) was reported by Akinpelu et al.[55] This observation was however low compared with previous report in Nigeria where Akesode and Ajibode[56] reported a prevalence of 3.2% and 5.1% in males and females respectively while Owa and Adejuyigbe[57] reported 18% for all children between ages 5 and 15 years. Obesity therefore is becoming a problem of the young in developing nations of Africa.
Dysglycemia
Diabetes mellitus, as already observed, increases the likelihood of developing metabolic syndrome.[29] This can be attributed to insulin resistance, which is the pathogenic hallmark. DM is no longer rare in Africa and type 2 diabetes accounts for about 90% of cases of DM seen all over Africa, as is observed globally. Though dysglycemia is becoming common, it ranked lowest in few studies in terms of contributing to the components of the syndrome. For instance, in Cameroon, using the NCEP-ATP III definition, impaired glycemia (women: rural, 1.1% and urban, 1.2%; men: rural, 1.2% and urban, 1.2%) was quite uncommon while the WHO definition gave a higher prevalence (women: rural, 6.4% and urban, 3.2%; men: rural, 11.5%, and urban, 6.0%).[31] In Botswana, 26.7% of subjects had abnormally high fasting blood glucose; being the least after low HDL-C (80%), hypertension (44%), and obesity (42%).[38] Similarly, among semiurban and rural dwelling Nigerians, hyperglycemia (≥5.6 mmol/l) was found in 13.9%, 10.4%, and 21.2% of all the subjects, nonhypertensives and hypertensive subjects respectively but it was the least frequent of all the components of the syndrome.[35] Higher occurrence of hyperglycemia among the hypertensive compared to the nonhypertensive population in both semiurban (20.7% vs. 9.6%) and rural communities (23% vs. 12.2%) was noted. This may be evidence in support of insulin resistance being behind the clustering of metabolic syndrome components.[58] Among the hypertensive subjects attending a tertiary healthcare facility in Nigeria, prediabetes was reported with equal gender proportion of 25% each.[59] Specifically, 25% and 14% had impaired fasting glycemia (IFG) and impaired glucose tolerance respectively while 6% had both IFG and IGT.[59]
Hypertension
Hypertension is another common component of the metabolic syndrome with diagnostic indications. Hypertension is one of the most common cardiovascular disorders today in Africa.[29,30,34,35,40] In Botswana, hypertension was found in 44% of the subjects being the second most common component of the syndrome.[38] The number of people suffering from hypertension is also on the rise as are other noncommunicable diseases. In Nigeria, a survey of the market population, for instance, showed that 42% of the subjects had hypertension, thus representing an about 65% increase when compared to the national survey report of 1997 which gave a national prevalence of 10-15%.[25,60] There is therefore an increase in the prevalence of hypertension both in rural and urban communities but in Cameroon, the increase was found to have occurred more in rural communities.[61] The risk of hypertension is however known to increase with long-term urbanization.[45,51]
This again brings to the fore the role being played by urbanization and epidemiologic transitions in the current upward trend in the number of people being affected by cardiometabolic disorders. As the number of affected people increases, it is worrisome that awareness of the presence of hypertension, its associated risks and compliance with recommended therapies is low in these subjects.[60,62] In many studies, hypertension was more common in males but higher prevalence in females has been reported.[63–65]
EPIDEMIOLOGY OF METABOLIC SYNDROME IN AFRICA
Metabolic syndrome and age
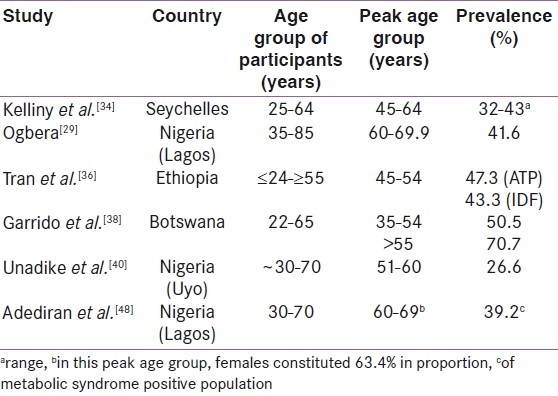
Metabolic syndrome was initially recognized as an adult disorder because its early descriptions were made in adults and its constituent components are disorders which are seen commonly in adults or are associated with aging.[1–12] The currently emerging data in Africa have mainly been from adult populations (>20 years) though some studies had involved subjects that were <20 years.[51,62] Several workers have observed that the prevalence of metabolic syndrome increases with age.[29,31,34,36,39,62] Prevalence increased from 11% in subjects aged 20-29 years to 89% in those aged 70-79 years in Nigeria.[29] Available data suggest that despite the increasing trend in prevalence as age increases, adults who may be classified as middle aged (40-60 years) are predominantly affected [Table 4]. This is also seen in the mean ages recorded in these studies (not shown).
Table 4.
Prevalence of metabolic syndrome from some African studies showing the peak age group
Metabolic syndrome today is not only seen in adults but it is now also beginning to occur in children and adolescents due to the growing obesity epidemic within this young population.[66–68] As a result, the IDF has also developed a consensus definition for identifying this syndrome in the young [Table 5].[69] The intention is “to obtain a universally accepted tool which is easy to use for the early diagnosis of metabolic syndrome, in order to take preventive measures before the child or adolescent develops diabetes or cardiovascular disease.”[69]
Table 5.
The International Diabetes Federation consensus definition of the metabolic syndrome in children and adolescents[69]
Approximately 22 million children under the age of 5 years were estimated to be overweight or obese by the World Health Organization (WHO 2004) while according to the International Obesity Task Force (IOTF), at least 10% of school-aged children between 5 and 17 years are overweight or obese.[70,71] In the United States of America for instance, the rate of overweight and obesity among children and adolescents aged 6-18 years increased from 15% in the 1970s to more than 25% in the 1990s.[72]
Such increases are not re-stricted to developed coun-tries; many low- and middle-income countries are becoming largely involved. Globally, it is estimated that 17 million of the 22 million children under 5 years live in major economically developing countries.[73] In China for example, the rate of over-weight and obesity observed in a study of urban school children increased from almost 8% in 1991 to more than 12% after 6 years while in Brazil, the rate of over-weight and obesity among children and adolescents 6-18 years old increased from 4% in the mid-1970s to over 13% in the late 1990s.[72] A survey among South African undergraduate students revealed that metabolic risk factors were evident in this much younger population (60%) than was commonly expected with gender-specific differences being observed.[74] This may not be unconnected with the epidemiologic transition being witnessed in many developing nations, with South Africa appearing to be advanced compared to other African nations.[75] Among Nigerian adolescents, overweight was more common than obesity.[55] In Egypt, metabolic syndrome was found in 7.4% of 4250 adolescents with nearly 25% having the full components of the syndrome among those with high values of the different components.[76] The odds of having the syndrome was increased by positive family history of obesity and diabetes mellitus. Similarly, proinflammatory markers were also found to be common in subjects who participated in the study.[76] In some nations of Africa as well as other developing nations, it has been shown that a high socioeconomic status may be related to positive obesity status.[77] This observation is in contrast to what is seen in developed nations where high educational status (one of the determinants of socioeconomic status) seems to be protective against metabolic syndrome; this benefit is attributed to potential mechanisms such as exposure to less psychosocial and material stress, better health knowledge, and better health behavior.[78]
Metabolic syndrome and gender
Gender-specific differences have been demonstrated by different workers. Metabolic syndrome appears to be more common in females [Table 6] like obesity whereas hypertension appears to be more common in males.[36,45,51,74,79] The prevalence of metabolic syndrome was only observed to be higher among males from the Jos plateau of Nigeria where the authors noted that the high activity profile of women may have contributed to this observation.[39] This pattern is at variance with the findings from the north-western Nigeria (Sokoto) where the religious practice of putting the women in Purdah makes them sedentary.
Table 6.
Prevalence of metabolic syndrome from Africa showing some gender patterns and differences
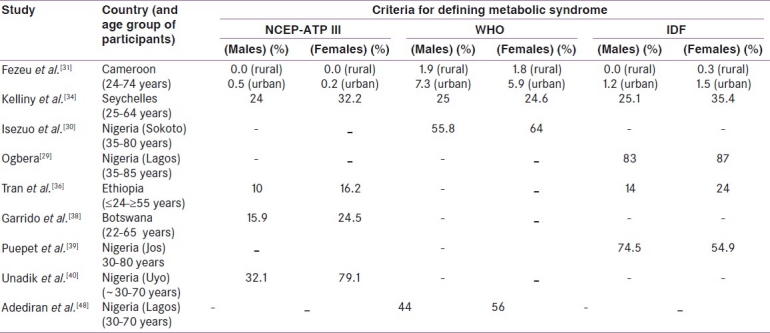
Age-adjusted prevalence of central obesity (using NCEP-ATP III and IDF definitions, based on waist circumference) was found to be higher in women compared to men and were lower in the rural than the urban areas.[31] Among Cameroonians, considering those with two components of metabolic syndrome, the most frequent combination was central obesity and high blood pressure, which was more predominant in women than men (81% vs. 52%). Combination of high blood pressure and hypercholesterolemia (24% vs. 6%) and high blood pressure and hyperglycemia (12% vs. 6%) demonstrated male predominance.[29] In South Africa, greater incidence of risk factors for the metabolic syndrome occurred in males but obesity was more common in females (25% vs. 14%). Both genders had abnormally high mean TG but male predominance appeared to be observed for dyslipidemia.[29,42,45] Metabolic syndrome was seen to be more common in males in Jos, Nigeria.[39]
Pathogenesis of metabolic syndrome
Till date, the pathogenesis of metabolic syndrome is yet to be clearly defined. Insulin resistance, which clinically is defined as requiring higher amounts of insulin to maintain euglycemia, is the key mechanism thought to underlie metabolic syndrome.[43,58] Insulin resistance is believed to be determined not only by environmental factors but also by genetic factors as anchored in the “thrifty gene hypothesis” proposed by Neel.[80] Other genetic hypothetical models have also been suggested in Africans such as the fetal origins of chronic disease.[81] The thrifty genotype theory suggests that genes derived from times of deprivation may result in adaptive processes that have adverse effects in times of plenty while the fetal origins of chronic disease hypothesis ascribes the epidemic, in part, to an adverse intrauterine environment. There is compelling evidence that small size at birth in full-term pregnancies is linked with the subsequent development of the major features of the metabolic syndrome, namely glucose intolerance, increased blood pressure, dyslipidemia, and increased mortality from cardiovascular disease.[82] The resultant hyperinsulinemia has been associated with lots of the abnormalities or components associated with insulin resistance.[58] Three mechanisms of insulin resistance as highlighted by Adediran et al.[43] include an abnormal B-cell secretory product, circulating insulin antagonists, and target tissue defect in insulin action. The target tissues predominantly involved are the skeletal muscle, liver, and adipose tissue.
Insulin resistance is thought to affect about 25% of an apparently healthy population.[12] Prevalence estimates of insulin resistance in the general population vary depending on the criteria used for its definition. The prevalence increases with worsening of glucose tolerance status, being about 60-75% in those with impaired glucose tolerance (IGT) and about 85% in those with type 2 diabetes.[12] Ferrannini et al. using the euglycemic insulin clamp technique demonstrated a prevalence rate of 26% in 1146 normotensive, nondiabetic obese Caucasian subjects aged 18-85 years recruited from the database of the EGIR (European Group for the study of Insulin Resistance).[83] Studies on insulin resistance in indigenous African populations are quite few. In south-western Nigeria, a prevalence of 35% was reported among 500 healthy elderly subjects.[84] Among Ghanaians, Amoah et al.[85] evaluated 200 randomly selected subjects who were urban residents with no previous history of hypertension or diabetes mellitus and reported that mean homeostasis model assessment for insulin resistance (HOMA-IR) index was significantly higher in 26.5% of the subjects who were found to be hypertensive.
Management of metabolic syndrome
The successful management of metabolic syndrome hinges basically on lifestyle modification and pharmacological intervention. While attempts are ongoing in search for an approach that can simultaneously affect all the components, the current approach remains to treat each component as it becomes manifest. Since it is believed that a major driving force in Africa is epidemiologic transition, reverting back to African traditional lifestyles is a potential point of action to prevent the development of metabolic syndrome in Africans. This will involve paying attention to our local cardio-protective diets once again and improving on our level of physical activity structured into the activities of daily living of the individuals.[86–89] This however calls for plans to increase awareness among African subjects and for those already on treatment to adhere strictly to their medications.[60,62,90] These actions constitute significant primary and secondary prevention strategies.
Pharmacologically, several classes of drugs which include antihypertensive agents, oral glucose lowering agents, insulin sensitizers, and lipid-lowering agents are available to treat metabolic syndrome. Due to the clustering of the components of the syndrome, an individual with full-blown syndrome is exposed to high pill burden and in turn increased cost. These can contribute to poor adherence or compliance. The earlier the components are addressed the better, however prevention still remains the watchword.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Alberti KG, Zimmet P, Shaw J. Metabolic syndrome: A new world-wide definition: A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006;23:469–80. doi: 10.1111/j.1464-5491.2006.01858.x. [DOI] [PubMed] [Google Scholar]
- 2.Kylin E. Studies of the hypertension-hyperglycemia-hyperuricemia syndrome (German) Zentralbl Inn Med. 1923;44:105–27. [Google Scholar]
- 3.Vague J. Sexual differentiation: A factor affecting the forms of obesity. Presse Med. 1947;30:339–40. [PubMed] [Google Scholar]
- 4.Avogadro A, Crepaldi G, Enzi G, Tiengo A. Associazione di iperlipidemia, diabete mellito e obesità di medio grado. Acta Diabetol Lat. 1967;4:572–90. [Google Scholar]
- 5.Haller H. Epidermiology and associated risk factors of hyperlipoproteinemia. Zeitschrift fur die gesamte innere Medizin und ihre Grenzgebiete. 1977;32:124–8. [PubMed] [Google Scholar]
- 6.Singer P. Diagnosis of primary hyperlipoproteinemias. Zeitschrift fur die gesamte innere Medizin und ihre Grenzgebiete. 1977;32:129–33. [PubMed] [Google Scholar]
- 7.Phillips GB. Relationship between serum sex hormones and glucose, insulin and lipid abnormalities in men with myocardial infarction. Proc Natl Acad Sci USA. 1977;74:1729–33. doi: 10.1073/pnas.74.4.1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Phillips GB. Sex hormones, risk factors and cardiovascular disease. Am J Med. 1978;65:7–11. doi: 10.1016/0002-9343(78)90685-x. [DOI] [PubMed] [Google Scholar]
- 9.Reaven GM. Banting lecture 1988: Role of insulin resistance in human disease. Diabetes. 1988;37:1595–607. doi: 10.2337/diab.37.12.1595. [DOI] [PubMed] [Google Scholar]
- 10.Kaplan NM. The deadly quartet: Upper-body obesity, glucose intolerance, hypertriglyceridemia, and hypertension. Arch Intern Med. 1989;149:1514–20. doi: 10.1001/archinte.149.7.1514. [DOI] [PubMed] [Google Scholar]
- 11.Haffner SM, Valdez RA, Hazuda HP, Mitchell BD, Morales PA, Stern MP. Prospective analysis of the insulin-resistance syndrome (syndrome X) Diabetes. 1992;41:715–22. doi: 10.2337/diab.41.6.715. [DOI] [PubMed] [Google Scholar]
- 12.Lebovitz HE. Insulin resistance and the insulin resistance syndrome. In: Wheatcroft C, editor. Clinician's Manual on Insulin Resistance. London: Science Press Ltd; 2002. pp. 1–15. [Google Scholar]
- 13.Pedrinelli R, Dell’Omo G, Di Bello V, Pontremoli R, Mariani M. Microalbuminuria: An integrated marker of cardiovascular risk in essential hypertension. J Hum Hypertens. 2002;16:79–89. doi: 10.1038/sj.jhh.1001316. [DOI] [PubMed] [Google Scholar]
- 14.Grundy SM, Bryan Brewer H, Cleeman JI, Smith SC, Jr, Lenfant C. (for conference participants). Definition of Metabolic Syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association Conference on Scientific Issues Related to Definition. Circulation. 2004;109:433–8. doi: 10.1161/01.CIR.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 15.The IDF consensus worldwide definition of the metabolic syndrome. [cited in 2011]. Available from: http://www.idf.org/webdata/docs/IDF_Metasyndrome_definition.pdf .
- 16.Sattar N. The metabolic syndrome: Setting the scene: The cons. Diabetes Vasc Dis Res. 2007;4(suppl 2):S4–6. [Google Scholar]
- 17.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: An American Heart Association/ National Heart, Lung, and Blood Institute scientific statement. Circulation. 2005;112:2735–52. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 18.Can AS, Bersot TP. Analysis of agreement among definitions of metabolic syndrome in nondiabetic Turkish adults: A methodological study. BMC Public Health. 2007;7:353. doi: 10.1186/1471-2458-7-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: A Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 20.Longo-Mbenza B, Vangu Ngoma D, Mbungu Fuele S. Low birth weight, metabolic syndrome and their associations with the global crisis of 1930 - 1945, rapidly growing economy and coronary heart disease in Central Africa. Int J Nutr Metab. 2010;2:1–10. [Google Scholar]
- 21.Oldroyd J, Banerjee M, Heald A, Cruickshank K. Diabetes and ethnic minorities. Postgrad Med J. 2005;81:486–90. doi: 10.1136/pgmj.2004.029124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mclarty D, Pollitt C, Swai A, Alberti KG. Epidemiology of diabetes in Africa. In: Gill G, Mbanya J, Alberti G, editors. Diabetes in Africa. Cambridge: FSG Communications Ltd; 1997. pp. 1–17. [Google Scholar]
- 23.McLarty DG, Pollitt C, Swai AB. Diabetes in Africa. Diabet Med. 1990;7:670–84. doi: 10.1111/j.1464-5491.1990.tb01470.x. [DOI] [PubMed] [Google Scholar]
- 24.Mbanya JC, Motala AA, Sobngwi E, Assah FK, Enoru ST. Diabetes in sub-Saharan Africa. Lancet. 2010;375:2254–66. doi: 10.1016/S0140-6736(10)60550-8. [DOI] [PubMed] [Google Scholar]
- 25.Akinkugbe OO. Final report of national survey on non-communicable diseases in Nigeria. Federal Ministry of Health and Social Services. 1997 [Google Scholar]
- 26.International Diabetes Federation. Diabetes Atlas. 2nd ed. 2003. [accessed on 2006 Mar 31]. pp. 7–13. Available from: http//www.idf.org/e-atlas .
- 27.Akintunde AA, Ayodele OE, Akinwusi PO, Opadijo GO. Metabolic syndrome: Comparison of occurrence using three definitions in hypertensive patients. Clin Med Res. 2011;9:26–31. doi: 10.3121/cmr.2010.902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bruno G, Merletti F, Biggeri A, Bargero G, Ferrero S, Runzo C. Metabolic syndrome as a predictor of all-cause and cardiovascular mortality in type 2 diabetes: The Casale Monferrato study. Diabetes Care. 2004;27:2689–94. doi: 10.2337/diacare.27.11.2689. [DOI] [PubMed] [Google Scholar]
- 29.Ogbera A. Prevalence and gender distribution of the metabolic syndrome. Diabetol Metab Syndrome. 2010;2:1. doi: 10.1186/1758-5996-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Isezuo SA, Ezunu E. Demographic and clinical correlates of metabolic syndrome in native African type 2 diabetic patients. J Natl Med Assoc. 2005;97:557–63. [PMC free article] [PubMed] [Google Scholar]
- 31.Fezeu L, Balkau B, Kengne A, Sobngwi E, Mbanya JC. Metabolic syndrome in a Sub-Saharan African setting: Central obesity may be the key determinant. Atherosclerosis. 2007;193:70–6. doi: 10.1016/j.atherosclerosis.2006.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vorster HH. The emergence of cardiovascular disease during urbanization of Africans. Public Health Nutr. 2002;5:239–43. doi: 10.1079/phn2001299. [DOI] [PubMed] [Google Scholar]
- 33.van den Hooven C, Ploemacher J, Godwin M. Metabolic syndrome in a family practice population: Prevalence and clinical characteristics. Can Fam Physician. 2006;52:982–3. [PMC free article] [PubMed] [Google Scholar]
- 34.Kelliny C, William J, Riesen W, Paccaud F, Bovet P. Metabolic syndrome according to different definitions in a rapidly developing country of the African region. Cardiovasc Diabetol. 2008;7:27. doi: 10.1186/1475-2840-7-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ulasi II, Ijoma CK, Onodugo OD. A community-based study of hypertension and cardio-metabolic syndrome in semi-urban and rural communities in Nigeria. BMC Health Serv Res. 2010;10:71. doi: 10.1186/1472-6963-10-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tran A, Gelaye B, Girma B, Lemma S, Berhane Y, Bekele T, et al. Prevalence of metabolic syndrome among working adults in ethiopia. Int J Hypertens. 2011;2011:193719. doi: 10.4061/2011/193719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Longo-Mbenza B, Kasiam Lasi On’kin JB, Nge Okwe A, Kangola Kabangu N. The metabolic syndrome in a Congolese population and its implications for metabolic syndrome definitions. Diabet Metab Syndrome Clin Res Rev. 2011;5:17–24. doi: 10.1016/j.dsx.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 38.Garrido RA, Semeraro MB, Temesgen SM, Simi MR. Metabolic syndrome and obesity among workers at Kanye Seventh-day Adventist Hospital, Botswana. S Afr Med J. 2009;99:331–4. [PubMed] [Google Scholar]
- 39.Puepet FH, Uloko A, Akogu IY, Aniekwensi E. Prevalence of the metabolic syndrome among patients with type 2 diabetes mellitus in urban North-Central Nigeria. Afr J Endocrinol Metab. 2009;8:10–2. [Google Scholar]
- 40.Unadike BC, Akpan NA, Peters EJ, Essien IO, Essien OE. Prevalence of the metabolic syndrome among patients with type 2 diabetes mellitus in Uyo, Nigeria. Afr J Endocrinol Metab. 2009;8:7–9. [Google Scholar]
- 41.AlSaraj F, McDermott JH, Cawood T, McAteer S, Ali M, Tormey W, et al. Prevalence of the metabolic syndrome in patients diabetes mellitus. Ir J Med Sc. 2009;178:309–13. doi: 10.1007/s11845-009-0302-z. [DOI] [PubMed] [Google Scholar]
- 42.Wahab KW, Sani M, Gbadamosi M, Yandutse M. Frequency and determinants of the metabolic syndrome in apparently healthy adult Nigerians. Trop Doct. 2008;38:224–6. doi: 10.1258/td.2007.070335. [DOI] [PubMed] [Google Scholar]
- 43.Adediran OS, Jimoh AK, Ogbera AO. Metabolic syndrome: The pathogenesis of its predictors. Postgrad Doctor Caribbean. 2006;22:35–45. [Google Scholar]
- 44.Njelekela MA, Mpembeni R, Muhihi A, Mligiliche NL, Spiegelman D, Hertzmark E, et al. Gender-related differences in the prevalence of cardiovascular disease risk factors and their correlates in urban Tanzania. BMC Cardiovasc Disord. 2009;9:30. doi: 10.1186/1471-2261-9-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sodjinou R, Agueh V, Fayomi B, Delisle H. Obesity and cardiometabolic risk factors in urban adults of Benin: Relationship with socio-economic status, urbanisation, and lifestyle Patterns. BMC Public Health. 2008;8:84. doi: 10.1186/1471-2458-8-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Okafor CI, Fasanmade OA, Oke DA. Pattern of dyslipidaemia among Nigerians with type 2 diabetes mellitus. Niger J Clin Pract. 2008;11:25–31. [PubMed] [Google Scholar]
- 47.Akpa MR, Agomuoh DI, Alasia DD. Lipid profile of healthy adult nigerians in port Harcourt, Nigeria. Niger J Med. 2006;15:137–40. doi: 10.4314/njm.v15i2.37097. [DOI] [PubMed] [Google Scholar]
- 48.Adediran OS, Edo AE, Jimoh AK, Ohwovoriole AE. Prevalence of the metabolic syndrome among Nigerians with type 2 diabetes. Diabetes Int. 2007;15:13–4. [Google Scholar]
- 49.Bakari AG, Onyemelukwe GC. Indices of obesity among type 2 diabetic Hausa-Fulani Nigerians. Int J Diabetes Metab. 2005;13:28–9. [Google Scholar]
- 50.Okafor CI, Ofoegbu EN, Fasanmade OA. Comparison of the performance of two measures of central adiposity among apparently healthy Nigerians using the Receiver Operating Characteristic (ROC) analysis. Indian J Endoc Metab. 2011;15:320–6. doi: 10.4103/2230-8210.85588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.van der Sande MA, Ceesay SM, Milligan PJ, Nyan OA, Banya WA, Prentice A, et al. Obesity and under nutrition and cardiovascular risk factors in rural and urban gambian communities. Am J Public Health. 2001;91:1641–4. doi: 10.2105/ajph.91.10.1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Aboul Ella NA, Shehab DI, Ismail MA, Maksoud AA. Prevalence of metabolic syndrome and insulin resistance among Egyptian adolescents 10 to 18 years of age. J Clin Lipidol. 2010;4:185–95. doi: 10.1016/j.jacl.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 53.Puoane T, Steyn K, Bradshaw D, Laubscher R, Fourie J, Lambert V, et al. Obesity in South Africa: The South African demographic and health survey. Obes Res. 2002;10:1038–48. doi: 10.1038/oby.2002.141. [DOI] [PubMed] [Google Scholar]
- 54.Reddy SP, Panday S, Swart D, Jinabhai CC, Amosun SL, James S, et al. Cape Town: South African Medical Research Council; 2003. [cited on 2011 Jul 2]. Umthenthe Uhlaba Usamila - The South African Youth Risk Behaviour Survey 2002. Available from: http://www.mrc.ac.za/healthpromotion/reports.htm . [Google Scholar]
- 55.Akinpelu AO, Oyewole OO, Oritogun KS. Overweight and obesity: Does it occur in Nigerian adolescents in an urban community? Int J Biomed Hlth Sci. 2008;4:11–7. [Google Scholar]
- 56.Akesode FA, Ajibode HA. Prevalence of obesity among Nigerian school children. Soc Sci Med. 1983;17:107–11. doi: 10.1016/0277-9536(83)90361-1. [DOI] [PubMed] [Google Scholar]
- 57.Owa JA, Adejuyigbe O. Fat mass percentage, body mass index and upper arm circumference in a healthy population of Nigerian children. J Trop Pediatr. 1997;43:13–9. doi: 10.1093/tropej/43.1.13. [DOI] [PubMed] [Google Scholar]
- 58.Mufunda J, Sigola LB, Chifamba J, Vengesa PM. Hyperinsulinemia: Possible cause of high blood pressure in unemployed urban black women. High Blood Pressure. 1995;4:137–40. [Google Scholar]
- 59.Ogbu ISI, Neboh CI. The prevalence of Pre diabetes among Hypertensive patients in Enugu, Southeast Nigeria. Niger Med J. 2009;50:14–7. [Google Scholar]
- 60.Ulasi II, Ijoma CK, Onwubere BJ, Arodiwe E, Onodugo O, Okafor C. High prevalence and low awareness of hypertension in a market population in Enugu, Nigeria. Int J Hypertens. 2011;2011:869675. doi: 10.4061/2011/869675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fezeu L, Kengne AP, Balkau B, Awah PK, Mbanya JC. Ten-year change in blood pressure levels and prevalence of hypertension in urban and rural Cameroon. J Epidemiol Commun Health. 2010;64:360–5. doi: 10.1136/jech.2008.086355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.van der Sande MA, Milligan PJ, Nyan OA, Rowley JT, Banya WA, Ceesay SM, et al. Blood pressure patterns and cardiovascular risk factors in rural and urban Gambian communities. J Hum Hypertens. 2000;14:489–96. doi: 10.1038/sj.jhh.1001050. [DOI] [PubMed] [Google Scholar]
- 63.Tesfaye F, Byass P, Wall S. Population based prevalence of high blood pressure among adults in Addis Ababa: Uncovering a silent epidemic. BMC Cardiovasc Disord. 2009;9:39. doi: 10.1186/1471-2261-9-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Edwards R, Unwin N, Mugusi F, Whiting D, Rashid S, Kissima J, et al. Hypertension prevalence and care in an urban and rural area of Tanzania. J Hypertens. 2000;18:145–52. doi: 10.1097/00004872-200018020-00003. [DOI] [PubMed] [Google Scholar]
- 65.Opie LH, Yackoob K, Seedat YK. Hypertension in Sub-Saharan African populations. Circulation. 2005;112:3562–8. doi: 10.1161/CIRCULATIONAHA.105.539569. [DOI] [PubMed] [Google Scholar]
- 66.Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350:2362–74. doi: 10.1056/NEJMoa031049. [DOI] [PubMed] [Google Scholar]
- 67.Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: Findings from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med. 2003;157:821–7. doi: 10.1001/archpedi.157.8.821. [DOI] [PubMed] [Google Scholar]
- 68.Cruz ML, Weigensberg MJ, Huang TT, Ball G, Shaibi GQ, Goran MI. The metabolic syndrome in overweight Hispanic youth and the role of insulin sensitivity. J Clin Endocrinol Metab. 2004;89:108–13. doi: 10.1210/jc.2003-031188. [DOI] [PubMed] [Google Scholar]
- 69.The IDF consensus definition of the metabolic syndrome in children and adolescents. [accessed on 2011 Jul 9]. Available from: http://www.idf.org/webdata/docs/Mets_definition_children.pdf .
- 70.World Health Organization. Global strategy on diet, physical activity and health: Obesity and overweight. 2004. [accessed on 2007 Aug 24]. Available from: http://www.who.int/dietphysicalactivity/publications/facts/obesity/en/
- 71.Lobstein T, Baur L, Uauy R. IASO International Obesity Task Force. Obesity in children and young people: A crisis in public health. Obes Rev. 2004;5(Suppl 1):4–104. doi: 10.1111/j.1467-789X.2004.00133.x. [DOI] [PubMed] [Google Scholar]
- 72.Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1:11–25. doi: 10.1080/17477160600586747. [DOI] [PubMed] [Google Scholar]
- 73.World Health Organization, Fight Childhood Obesity to prevent diabetes, say WHO and IDF. [accessed on 2011 Jul 9]. Available from: http://www.who.int/mediacentre/news/releases/2004/pr81/en/index.html .
- 74.Smith C, Faadiel Essop M. Gender differences in metabolic risk factor prevalence in a South African student population. Cardiovasc J Afr. 2009;20:178–82. [PMC free article] [PubMed] [Google Scholar]
- 75.Vorster HH, Wissing MP, Venter CS, Kruger HS, Kruger A, Malan NT, et al. The impact of urbanization on physical, physiological and mental health of Africans in the North West Province of South Africa: the THUSA study. S Afr J Sci. 2000;96:505–14. [Google Scholar]
- 76.Aboul Ella NA, Shehab DI, Ismail MA, Maksoud AA. Prevalence of metabolic syndrome and insulin resistance among Egyptian adolescents 10 to 18 years of age. J Clin Lipidol. 2010;4:185–95. doi: 10.1016/j.jacl.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 77.Fezeu L, Minkoulou E, Balkau B, Kengne AP, Awah P, Unwin N, et al. Association between socioeconomic status and adiposity in urban Cameroon. Int J Epidemiol. 2006;35:105–11. doi: 10.1093/ije/dyi214. [DOI] [PubMed] [Google Scholar]
- 78.Lucove JC, Kaufman JS, James SA. Association between adult and childhood socioeconomic status and prevalence of the metabolic syndrome in African Americans: The pitt county study. Am J Public Health. 2007;97:234–6. doi: 10.2105/AJPH.2006.087429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.BeLue R, Okoror TA, Iwelunmor J, Taylor KD, Degboe AN, Agyemang C, et al. An overview of cardiovascular risk factor burden in sub-Saharan African countries: A socio-cultural perspective. Global Health. 2009;5:10. doi: 10.1186/1744-8603-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Neel JV. Diabetes mellitus: A ‘thrifty’ genotype rendered detrimental by ‘progress’? Am J Hum Genet. 1962;14:353–62. [PMC free article] [PubMed] [Google Scholar]
- 81.Levitt NS, Lambert EV. The foetal origins of the metabolic syndrome: A South African perspective. Cardiovasc J S Afr. 2002;13:179–80. [PubMed] [Google Scholar]
- 82.Levitt NS, Lambert EV, Woods D, Hales CN, Andrew R, Seckl JR. Impaired glucose tolerance and elevated blood pressure in low birth weight, nonobese, young south African adults: Early programming of cortisol axis. J Clin Endocrinol Metab. 2000;85:4611–8. doi: 10.1210/jcem.85.12.7039. [DOI] [PubMed] [Google Scholar]
- 83.Ferrannini E, Natali A, Bell P, Cavallo-Perin P, Lalic N, Mingrone G. on behalf of the European Group for the Study of Insulin Resistance (EGIR). Insulin resistance and hypersecretion in obesity. J Clin Invest. 1997;100:1166–73. doi: 10.1172/JCI119628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ezenwaka CE, Akanji AO, Akanji BO, Unwin NC, Adejuwon CA. The prevalence of insulin resistance and cardiovascular risk factors in healthy elderly southwestern Nigerians. Atherosclerosis. 1997;128:201–11. doi: 10.1016/s0021-9150(96)05991-6. [DOI] [PubMed] [Google Scholar]
- 85.Amoah AG, Schuster DP, Gaillard T, Osei K. Insulin sensitivity and cardiovascular risk factors in hypertensive and normotensive native Ghanaians. Diabetologia. 2003;46:949–55. doi: 10.1007/s00125-003-1130-8. [DOI] [PubMed] [Google Scholar]
- 86.Sonnenberg L, Pencina M, Kimokoti R, Quatromoni P, Nam B, D’agostino R, et al. Dietary patterns and the metabolic syndrome in obese and non-obese Framingham women. Obes Res. 2005;13:153–62. doi: 10.1038/oby.2005.20. [DOI] [PubMed] [Google Scholar]
- 87.Weigensberg MC, Ball GD, Shaibi GQ, Cruz ML, Gower BA, Goran MI. Dietary fatintake and insulin resistance in black and white children. Obes Res. 2005;13:1630–7. doi: 10.1038/oby.2005.200. [DOI] [PubMed] [Google Scholar]
- 88.Sivasankaran S. The cardio-protective diet. Indian J Med Res. 2010;132:608–16. [PMC free article] [PubMed] [Google Scholar]
- 89.Wu T, Gao X, Chen M, van Dam RM. Long-term effectiveness of diet-plus-exercise interventions vs.diet-only interventions for weight loss: A meta-analysis. Obes Rev. 2009;10:313–23. doi: 10.1111/j.1467-789X.2008.00547.x. [DOI] [PubMed] [Google Scholar]
- 90.Lewis SJ, Rodbard HW, Fox KM, Grandy S for the SHIELD Study Group. Self-reported prevalence and awareness of metabolic syndrome: Findings from SHIELD. Int J Clin Pract. 2008;62:1168–76. doi: 10.1111/j.1742-1241.2008.01770.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


