Abstract
The first description of patients with clustering of various metabolic abnormalities was as early as 1923 but it was more than five decades later, in 1988, that Reaven coined the term ‘syndrome X’ for this entity. The last two decades have brought forth a number of definitions and criteria to identify this condition. Various studies have demonstrated disparities in these definitions and a few researchers have questioned the utility of these criteria and even the existence of such a syndrome. A few important definitions are reviewed in this paper and, at the end, a simplified clinical definition is given and a simple parameter – lipid accumulation product – is been described that can be used to identify this condition.
Keywords: Controversies, definition, index of central obesity, metabolic syndrome
INTRODUCTION
A clustering of various metabolic abnormalities, e.g., hypertension, hyperglycemia, and hyperuricemia, was observed in some patients as early as 1923.[1] More than five decades after this observation, Reaven coined the term ‘syndrome X’ for this conglomeration of various metabolic abnormalities, including glucose intolerence, hypertension, increased very-low-density lipoproteins (VLDL), triglycerides, and decreased high-density lipoprotein cholesterol (HDL-C), with insulin resistance being the basic underlying pathophysiologic problem.[2] Over the last two decades, various organizations have proposed different definitions, using varying terminologies. We review a few important definitions in this paper.
WHO DEFINITION
WHO, in 1999, suggested a working definition of metabolic syndrome (MS), which was to be improved in due course of time.[3] WHO defined MS as glucose intolerence, impaired glucose tolerance (IGT) or diabetes mellitus (DM), and/or insulin resistance, together with two or more of the components listed below:
Raised arterial pressure, i.e., ≥140/90 mm of Hg
Raised plasma triglyceride (≥ 150 mg/dl) and/or low HDL-C (<35 mg/dl in men and <39 mg/dl in women)
Central obesity, i.e., waist/hip ratio (WHR) >0.9 in men and >0.85 in women and/or body mass index (BMI) >30 kg/m2
Microalbuminuria, i.e., urinary albumin excretion rate ≥ 20 μgm/minute or albumin/creatine ratio ≥ 30 μgm/mg.
This definition further insisted on a need for a clear description of the essential components of the syndrome, along with data to support the relative importance of each component. These conditions seem to be highly technical and the definition is rather impracticable.
EUROPEAN GROUP FOR STUDY OF INSULIN RESISTANCE DEFINITION
The European Group for Study of Insulin Resistance (EGIR) proposed a modification of the WHO definition, using the term insulin resistance syndrome rather than MS.[4] According to the EIGR definition the diagnostic criteria included elevated plasma insulin (>75th percentile) plus two other factors from among the following:
Abdominal obesity: waist circumference (WC) ≥94 cm in men and ≥80 cm in women
Hypertension: ≥140/90 mm of Hg or on antihypertensive treatment
Elevated triglycerides (≥150 mg/dl) and/or reduced HDL-C (<39 mg/dl for both men and women)
Elevated plasma glucose: impaired fasting glucose (IFG) or IGT, but no diabetes
Notably, EGIR focused more on abdominal obesity than did WHO, but in contrast to WHO, EGIR excluded patients with type 2 DM from their syndrome because insulin resistance was viewed primarily as a risk factor for diabetes.
This definition was followed by a simpler definition released by the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III).[5]
NCEP ATP III DEFINITION
According to this definition, a subject has the MS if he or she has three or more of the following criteria:
Abdominal obesity: WC ≥102 cm in men and ≥88 cm in women
Hypertriglyceridemia: ≥150 mg/dl (1.695 mmol/l)
Low HDL-C: <40 mg/dl in men and <50 mg/dl in women
High blood pressure (BP): >130/85 mmHg
High fasting glucose: >110 mg/dl
This definition differs from the WHO definition on several fronts. The NCEP ATP III did not believe that insulin resistance is mandatory for the development of MS and hence suggested the term MS instead of the previously used term ‘insulin resistance syndrome.’ This definition recognizes central obesity as the culprit and hence body mass index (BMI,) which is a parameter for generalized obesity, has not been included in this definition. Central obesity has been quantified using WC instead of the WHR used by WHO. This definition considers low HDL and high triglycerides as separate components (both of them being individually atherogenic) rather than viewing dyslipidemia as a single component. The cutoff points used for BP and HDL are stringent as compared to those suggested in the WHO definition, but by avoiding the need for clamp techniques and measurement of microalbuminuria, the NCEP ATP III definition is much more practically applicable. The NCEP ATP III considers the proinflamatory state and prothrombotic state as components of MS though these have not been included among the criteria necessary to define MS.
AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS DEFINITION
The American Association of Clinical Endocrinologists (AACE) too preferred using the term insulin resistance syndrome over MS.[6] The major criteria they considered were IGT, elevated triglycerides, reduced HDL-C, elevated BP, and obesity. They did not specify any particular number of criteria for diagnosis, rather they left it to clinical judgment. They suggested that factors like family history of atherosclerotic cardiovascular disease or type 2 DM, polycystic ovary syndrome, and hyperuricemia be considered while exercising clinical judgement. Patients with type 2 DM were excluded from the definition of insulin resistance syndrome. The various components suggested by the AACE are as follows:
-
Some degree of glucose intolerance
- IFG/IGT
-
Abnormal uric acid metabolism
- Plasma uric acid concentration
- Renal uric acid clearance
-
Dyslipidemia
- Triglycerides
- HDL-C
- LDL particle diameter (small, dense LDL-particles)
- Postprandial accumulation of TG-rich lipoproteins
-
Hemodynamic changes
- Sympathetic nervous system activity
- Renal sodium retention
- Blood pressure (~50% of patients with hypertension are insulin resistant)
-
Prothrombotic factors
- Plasminogen activator inhibitor-1
- Fibrinogen
-
Markers of inflammation
- C-reactive protein, white blood cell count, etc.
-
Endothelial dysfunction
- Mononuclear cell adhesion
- Plasma concentration of cellular adhesion molecules
- Plasma concentration of asymmetric dimethylarginine
- Endothelial-dependent vasodilatation
ADA lowered the fasting plasma glucose threshold used to identify individuals with IFG from 110 mg/dl to 100 mg/dl. Subsequently, the NCEP ATP III has also suggested that the fasting plasma glucose concentration for diagnosing MS be lowered to 100 mg/dl.[7]
Researchers worldwide preferred using the NCEP ATP III definition because it was relatively simple and clinically applicable. Various researchers noted that the WC cutoffs suggested by this definition were not applicable in other countries.[8–11] Though the WC cutoffs suggested by various groups differ, the generally accepted cutoffs for Asians are 90 cm for men and 80 cm for women.[8,12]
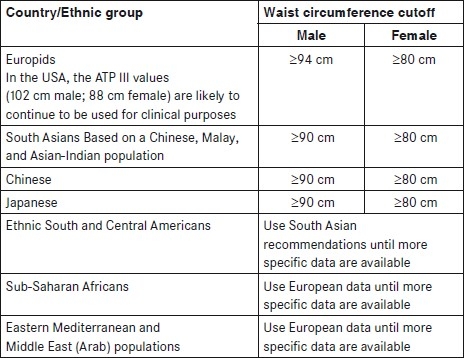
INTERNATIONAL DIABETES FEDERATION GLOBAL CONSENSUS DEFINITION
Against the backdrop of all these controversies related to diagnostic criteria and the lack of consensus regarding WC cutoffs, the International Diabetes Federation (IDF) released a global consensus definition for MS, along with race- and gender-specific WC cutoffs.[13] This definition identified central obesity as an essential component of MS and defined MS as central obesity (based on race- and gender-specific WC cutoffs) plus any two of the following four parameters:
Raised triglycerides: ≥150 mg/dl (1.7 mmol/l) or history of specific treatment for this lipid abnormality
Reduced HDL cholesterol: < 40 mg/dl (1.03 mmol/l) in males and < 50 mg/dl (1.29 mmol/l) in females or history of specific treatment for this lipid abnormality
Raised blood pressure: systolic BP ≥130 mm Hg or diastolic BP ≥85 mm Hg or on treatment for previously diagnosed hypertension
Raised FPG: ≥ 100 mg/dl or previously diagnosed type 2 DM
The race- and gender-specific WC cutoffs suggested are as follows:
This global consensus definition was immediately followed by a joint statement from the American Diabetes Association and the European Association for the Study of Diabetes questioning the use of the term ‘metabolic syndrome.’ The statement concluded that too much critically important information is missing to warrant its designation as a ‘syndrome.’[14] It was also argued that having a label of MS does not add any risk in addition to the risk contributed by the individual components.
This joint statement did not discourage researchers working in the field of MS and number of papers supporting the use of MS as screening tool to identify subjects at high risk of cardiovascualr disease were published.[15–18] Disparities in the data generated due to the use of various definitions still remained a major issue.[19–23] For example, from the subanalysis of the Chennai Urban Rural Epidemiology Study, MS was identified in 546 subjects (23.2%) by the WHO definition, in 430 subjects (18.3%) by the NCEP ATPIII definition, and in 607 subjects (25.8%) by the IDF definition. It is worthy of note that only 224 of these subjects were identified as MS by all the three criteria.[6]
A joint interim statement of the IDF Task Force on Epidemiology and Prevention; the National Heart, Lung, and Blood Institute; the American Heart Association; the World Heart Federation; the International Atherosclerosis Society; and the International Association for the Study of Obesity suggested using the IDF global consensus definition, but without having central obesity as an obligatory parameter. It was suggested that the presence of three or more of the five parameters could be considered as diagnostic of MS.[24] This joint statement suggested that the IDF-recommended race- and gender-specific cutoffs be used until WC cutoffs could be further evaluated based on data from various regions. The WC cutoffs suggested by various researchers from Japan,[25,26] Korea,[27,28] Iran,[29] Iraq,[30] and other regions[31] has further confused the definition of MS as there are now numerous race- and gender-specific WC cutoffs.
Looking at the various race- and gender-specific cutoffs of WC suggested by the IDF and the corresponding average heights of the different population groups, it was postulated that the need for various race- and gender-specific cutoffs can be largely attributed to differences in the average heights (32). A novel parameter, the index of central obesity (ICO), defined as the ratio of the WC to the height, was suggested as an alternative.[32] The utility of ICO for defining MS among diabetic[33] as well as nondiabetic subjects[34] has been evaluated.
The ICO has been widely studied and has been shown to have a good correlation with central adipocity[35] and tissue glucose utilization;[36] it was found to be a good predictor of type 2 DM.[37] ICO has also been shown to have a strong correlation with leptin levels and atherogenic lipid profile,[38] oxidative stress,[39] and increased cardiovascular risk.[40] Besides, it has been shown to be useful in identifying childhood central obesity[41] and insulin resistance in children.[42]
SIMPLIFIED DEFINITION OF METABOLIC SYNDROME
In view of all the above evidence, we have proposed that WC be replaced by ICO in all definitions of MS.[43] With the use of ICO, the need for various race- and gender-specific cutoffs for WC can be obviated. Although a number of studies have proposed ICO cutoffs ranging between 0.45 and 0.55, we propose the use of a simple cutoff of 0.5 across both genders and all races. MS is a screening tool, and we believe that it should be used to identify people at high risk of metabolic complications and cardiovascular disease so that further detailed investigations can be performed. This definition translates into a very simple message to the community ‘If your waist size is more than half of your height, you should consult your doctor.’ Thus, all patients with ICO >0.5 should be evaluated for high blood pressure, prediabetes, and dyslipidemia.
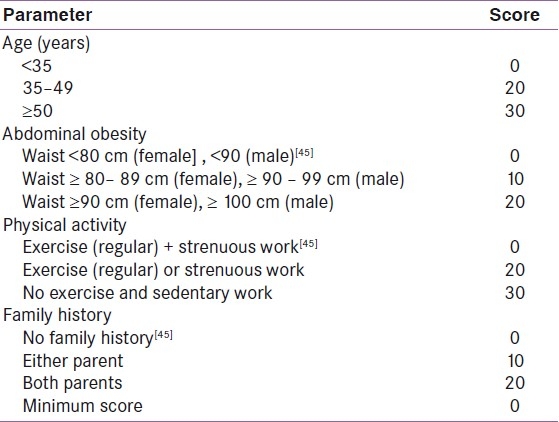
INDIAN DIABETES RISK SCORE
Identification of MS can be made more clinical by including clinical parameters like age, family history, personal history, etc., as parameters to define MS. Indian diabetes risk score (IDRS) is one such parameter comprising simple clinical information like age, WC, family history of diabetes, and physical activity.[44] IDRS ≥ 60 been found to be useful In predicting MS and cardiovascular disease [Table 1].[45]
Table 1.
Indian diabetes risk score
LIPID ACCUMULATION PRODUCT
In view of the role of central obesity and dyslipidemia in atherosclerotic process, an alternative continuous index of lipid overaccumulation, the lipid accumulation product (LAP), has been proposed. LAP is computed using WC and fasting triglycerides level (in mmol/l): (WC – 65) × TG (men) and (WC – 58) × TG (women).[46] This parameter has been found to be better than BMI for predicting diabetes[47] and has also been suggested for use in the identification MS.[48] It has been shown to be a good predictor of cardiovascular disease[49] though one study has shown that it may not be better than ICO or WHR for predicting cardiovascular disease.
CONCLUSION
In spite of the large number of controversies regarding the existence of MS as an entity and the nomenclature to be used, this conglomeration of various metabolic abnormalities has been widely accepted as a screening tool for identifying subjects at high risk of cardiovascular disease. While the various definitions proposed by different organizations have provided us with remarkable scientific insights into this syndrome, it has also complicated what was supposed to a simple screening tool. With the ongoing research in the area, we might soon have a very simple clinical definition to identify subjects at high risk of metabolic complications and cardiovascular disease.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Kylin E. Studies of the hypertension hyperglycemia hyperuricemia syndrome. Zentralbl Innere Med. 1923;44:105–27. [Google Scholar]
- 2.Reaven GM. Banting Lecture 1988: Role of insulin resistance in human disease. Diabetes. 1988;37:1595–607. doi: 10.2337/diab.37.12.1595. [DOI] [PubMed] [Google Scholar]
- 3.Part 1: diagnosis and classification of diabetes mellitus. World Health Organization: Geneva, Switzerland; 1999. [Last accessed on 2011 Jun 03]. World Health Organization. Definition, diagnosis and classification of diabetes mellitus and its complications: Report of a WHO Consultation. Available from: http:// www.whqlibdoc.who.int/hq/1999/WHO_NCD_NCS_99.2.pdf . [Google Scholar]
- 4.Balkau B, Charles MA. Comment on the provisional report from the WHO consultation. European Group for the Study of Insulin Resistance (EGIR) Diabet Med. 1999;16:442–3. doi: 10.1046/j.1464-5491.1999.00059.x. [DOI] [PubMed] [Google Scholar]
- 5.National Institutes of Health: Third Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Executive Summary. Bethesda, MD, National Institutes of Health, National Heart, Lung and Blood Institute. 2001 (NIH publ. no. 01-3670) [Google Scholar]
- 6.Einhorn D, Reaven GM, Cobin RH, Ford E, Ganda OP, Handelsman Y, et al. American College of Endocrinology position statement on the insulin resistance syndrome. Endocr Pract. 2003;9:237–52. [PubMed] [Google Scholar]
- 7.Grundy SM, Brewer HB, Jr, Cleeman JI, Smith SC, Jr, Lenfant C. American Heart Association; National Heart, Lung, and Blood Institute. Definition of Metabolic Syndrome. Report of the National Heart, Lung and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109:433–8. doi: 10.1161/01.CIR.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 8.Tan CE, Ma S, Wai D, Chew SK, Tai ES. Can we apply the National Cholesterol Education Program Adult Treatment Panel definition of the metabolic syndrome to Asians? Diabetes Care. 2004;27:1182–6. doi: 10.2337/diacare.27.5.1182. [DOI] [PubMed] [Google Scholar]
- 9.Zhou BF, Wu YF, Li Y, Zhang LF. The cut-off point of waist circumference for identifying metabolic syndrome in Chinese adults. Zhonghua Xin Xue Guan Bing Za Zhi. 2005;33:81–5. [PubMed] [Google Scholar]
- 10.Matsuzawa Y. Metabolic syndrome-definition and diagnostic criteria in Japan. J Atheroscler Thromb. 2005;12:301. doi: 10.5551/jat.12.301. [DOI] [PubMed] [Google Scholar]
- 11.Barbosa PJ, Lessa I, de Almeida Filho N, Magalhães LB, Araújo J. Criteria for central obesity in a Brazilian Population: Impact on the metabolic syndrome. Arq Bras Cardiol. 2006;87:366–73. doi: 10.1590/s0066-782x2006001700003. [DOI] [PubMed] [Google Scholar]
- 12.Misra A, Wasir JS, Pandey RM. An Evaluation of candidate definitions of the metabolic syndrome in adult Asian Indians. Diabetes Care. 2005;28:398–403. doi: 10.2337/diacare.28.2.398. [DOI] [PubMed] [Google Scholar]
- 13.The IDF consensus worldwide definition of the metabolic syndrome. [Last accessed on 2011 June 11]. Available from: http://www.idf.org/webdata/docs/IDF_Meta_def_final.pdf .
- 14.Kahn R, Buse J, Ferrannini E, Stern M American Diabetes Association; European Association for the Study of Diabetes. The metabolic syndrome: Time for a critical appraisal: joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2005;28:2289–304. doi: 10.2337/diacare.28.9.2289. [DOI] [PubMed] [Google Scholar]
- 15.Lau DC, Yan H, Dhillon B. Metabolic syndrome: A marker of patients at high cardiovascular risk. Can J Cardiol. 2006;22(Suppl B):85B–90B. doi: 10.1016/s0828-282x(06)70992-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tong PC, Kong AP, So WY, Yang X, Ho CS, Ma RC, et al. The usefulness of the International Diabetes Federation and the National Cholesterol Education Program's Adult Treatment Panel III definitions of the metabolic syndrome in predicting coronary heart disease in subjects with type 2 diabetes. Diabetes Care. 2007;30:1206–11. doi: 10.2337/dc06-1484. [DOI] [PubMed] [Google Scholar]
- 17.Koutsovasilis A, Protopsaltis J, Triposkiadis F, Kokkoris S, Milionis HJ, Zairis MN, et al. Comparative performance of three metabolic syndrome definitions in the prediction of acute coronary syndrome. Intern Med. 2009;48:179–87. doi: 10.2169/internalmedicine.48.1654. [DOI] [PubMed] [Google Scholar]
- 18.Jayasinghe SR, Jayasinghe SH. Variant metabolic risk factor profile leading to premature coronary disease: time to define the syndrome of accelerated atherocoronary metabolic syndrome in Asian Indians. Singapore Med J. 2009;50:949–55. [PubMed] [Google Scholar]
- 19.Hunt KJ, Resendez RG, Williams K, Haffner SM, Stern MP; San Antonio Heart Study. National Cholesterol Education Program versus World Health Organization metabolic syndrome in relation to all-cause and cardiovascular mortality in the San Antonio Heart Study. Circulation. 2004;110:1251–7. doi: 10.1161/01.CIR.0000140762.04598.F9. [DOI] [PubMed] [Google Scholar]
- 20.Oda E, Abe M, Veeraveedu PT, Watanabe K. Considerable disagreement among definitions of metabolic syndrome for Japanese. Circ J. 2007;71:1239–43. doi: 10.1253/circj.71.1239. [DOI] [PubMed] [Google Scholar]
- 21.Moebus S, Hanisch JU, Aidelsburger P, Bramlage P, Wasem J, Jöckel KH. Impact of 4 different definitions used for the assessment of the prevalence of the Metabolic Syndrome in primary healthcare: The German Metabolic and Cardiovascular Risk Project (GEMCAS) Cardiovasc Diabetol. 2007;6:22. doi: 10.1186/1475-2840-6-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hwu CM, Hsiung CA, Wu KD, Lee WJ, Shih KC, Grove J, et al. Diagnosis of insulin resistance in hypertensive patients by the metabolic syndrome: AHA vs. IDF definitions. Int J Clin Pract. 2008;62:1441–6. doi: 10.1111/j.1742-1241.2008.01818.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Deepa M, Farooq S, Datta M, Deepa R, Mohan V. Prevalence of metabolic syndrome using WHO, ATPIII and IDF definitions in Asian Indians: the Chennai Urban Rural Epidemiology Study (CURES-34) Diabetes Metab Res Rev. 2007;23:127–34. doi: 10.1002/dmrr.658. [DOI] [PubMed] [Google Scholar]
- 24.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the Metabolic Syndrome. A Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 25.Oizumi T, Daimon M, Wada K, Jimbu Y, Kameda W, Susa S, et al. A proposal for the cutoff point of waist circumference for the diagnosis of metabolic syndrome in the Japanese population. Circ J. 2006;70:1663. doi: 10.1253/circj.70.1663. [DOI] [PubMed] [Google Scholar]
- 26.Hara K, Matsushita Y, Horikoshi M, Yoshiike N, Yokoyama T, Tanaka H, et al. A proposal for the cutoff point of waist circumference for the diagnosis of metabolic syndrome in the Japanese population. Diabetes Care. 2006;29:1123–4. doi: 10.2337/diacare.2951123. [DOI] [PubMed] [Google Scholar]
- 27.Oh JY, Sung YA, Lee HJ, Oh JY, Chung HW, Park H. Optimal waist circumference for prediction of metabolic syndrome in young Korean women with polycystic ovary syndrome. Obesity (Silver Spring) 2010;18:593–7. doi: 10.1038/oby.2009.297. [DOI] [PubMed] [Google Scholar]
- 28.Koh JH, Koh SB, Lee MY, Jung PM, Kim BH, Shin JY, et al. Optimal waist circumference cutoff values for metabolic syndrome diagnostic criteria in a Korean rural population. J Korean Med Sci. 2010;25:734–7. doi: 10.3346/jkms.2010.25.5.734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Azizi F, Hadaegh F, Khalili D, Esteghamati A, Hosseinpanah F, Delavari A, et al. Appropriate definition of metabolic syndrome among Iranian adults: Report of the Iranian National Committee of Obesity. Arch Iran Med. 2010;13:426–8. [PubMed] [Google Scholar]
- 30.Mansour AA, Al-Hassan AA, Al-Jazairi MI. Cut-off values for waist circumference in rural Iraqi adults for the diagnosis of metabolic syndrome. Rural Remote Health. 2007;7:765. [PubMed] [Google Scholar]
- 31.Medina-Lezama J, Pastorius CA, Zea-Diaz H, Bernabe-Ortiz A, Corrales-Medina F, Morey-Vargas OL, et al. Optimal definitions for abdominal obesity and the metabolic syndrome in Andean Hispanics: The PREVENCION study. Diabetes Care. 2010;33:1385–8. doi: 10.2337/dc09-2353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Parikh RM, Joshi SR, Menon PS, Shah NS. Index of central obesity – A novel parameter. Med Hypotheses. 2007;68:1272–5. doi: 10.1016/j.mehy.2006.10.038. [DOI] [PubMed] [Google Scholar]
- 33.Parikh RM, Joshi SR, Menon PS, Shah NS. Metabolic Syndrome Among Indian Type 2 Diabetic Patients. J Gen Med. 2009;(21):16–9. [Google Scholar]
- 34.Parikh RM, Joshi SR, Pandia K. Index of central obesity is better than waist circumference in defining metabolic syndrome. Metab Syndr Relat Disord. 2009;7:525–7. doi: 10.1089/met.2008.0102. [DOI] [PubMed] [Google Scholar]
- 35.Kagawa M, Byrne NM, Hills AP. Comparison of body fat estimation using waist: Height ratio using different ‘waist’ measurements in Australian adults. Br J Nutr. 2008;100:1135–41. doi: 10.1017/S0007114508966095. [DOI] [PubMed] [Google Scholar]
- 36.Niebisz-Cieślak AB, Karnafel W. Insulin sensitivity in chronic pancreatitis and features of insulin resistance syndrome. Pol Arch Med Wewn. 2010;120:255–63. [PubMed] [Google Scholar]
- 37.MacKay, Meredith F. Evaluating alternate anthropometric measures as predictors of incident type 2 diabetes mellitus (T2DM): The Insulin Resistance Atherosclerosis Study (IRAS) UNIVERSITY OF TORONTO. 2008. [Last accessed online on 14th Jun 2011]. p. 158. MR58808. Available from: http://www.gateway.proquest.com/openurl%3furl_ver=Z39.88-2004%26res_dat=xri:pqdiss%26rft_val_fmt=info:ofi/fmt:kev:mtx:dissertation%26rft_dat=xri:pqdiss:MR58808 .
- 38.Abdullah A, Abd El-Baky A, Bakry S, Abd-El Hay E. Adiponectin and liptin levels and their risk in coronary artery diseases in obese Egyptian men. Res J Med Med Sci. 2009;4:526–32. [Google Scholar]
- 39.Veigas NM, Dharmalingam M, Marcus SR. Oxidative stress in obesity and metabolic syndrome in Asian Indians. J Med Biochem. 2011;30:115–20. [Google Scholar]
- 40.Hsieh SD, Yoshinaga H. Waist/height ratio as a simple and useful predictor of coronary heart disease risk factors in women. Intern Med. 1995;34:1147–52. doi: 10.2169/internalmedicine.34.1147. [DOI] [PubMed] [Google Scholar]
- 41.Sant’anna MS, Tinôco AL, Rosado LE, Sant’ana LF, Brito IS, Araújo LF, et al. Effectiveness of the conicity index and waist to height ratio to predict the percentage of body fat in children. J Braz Soc Food Nutr. 2010;35:67–80. [Google Scholar]
- 42.Manios Y, Kourlaba G, Kafatos A, Cook TL, Spyridaki A, Fragiadakis GA. Associations of several anthropometric indices with insulin resistance in children: The Children Study. Acta Paediatr. 2008;97:494–9. doi: 10.1111/j.1651-2227.2008.00729.x. [DOI] [PubMed] [Google Scholar]
- 43.Parikh R, Mohan V, Joshi S. Should Waist Circumference (WC) be replaced by Index of Central Obesity (ICO) in definition of metabolic syndrome? Diabetes Metab Res Rev. 2011 Jun 22; doi: 10.1002/dmrr.1227. doi: 10.1002/dmrr.1227. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 44.Mohan V, Deepa R, Deepa M, Somannavar S, Datta M. A simplified Indian diabetes risk score for screening for undiagnosed diabetic subjects. J Assoc Physicians India. 2005;53:759–63. [PubMed] [Google Scholar]
- 45.Mohan V, Sandeep S, Deepa M, Gokulakrishnan K, Datta M, Deepa R. A diabetes risk score helps identify metabolic syndrome and cardiovascular risk in Indians – the Chennai Urban Rural Epidemiology Study (CURES-38) Diabetes Obes Metab. 2007;9:337–43. doi: 10.1111/j.1463-1326.2006.00612.x. [DOI] [PubMed] [Google Scholar]
- 46.Ioachimescu AG, Brennan DM, Hoar BM, Hoogwerf BJ. The lipid accumulation product and all-cause mortality in patients at high cardiovascular risk: A PreCIS database study. Obesity (Silver Spring) 2010;18:1836–44. doi: 10.1038/oby.2009.453. [DOI] [PubMed] [Google Scholar]
- 47.Kahn HS. The lipid accumulation product is better than BMI for identifying diabetes: A population-based comparison. Diabetes Care. 2006;29:151–3. doi: 10.2337/diacare.29.1.151. [DOI] [PubMed] [Google Scholar]
- 48.Tellechea ML, Aranguren F, Martínez-Larrad MT, Serrano-Ríos M, Taverna MJ, Frechtel GD. Ability of lipid accumulation product to identify metabolic syndrome in healthy men from Buenos Aires. Diabetes Care. 2009;32:e85. doi: 10.2337/dc08-2284. [DOI] [PubMed] [Google Scholar]
- 49.Bozorgmanesh M, Hadaegh F, Azizi F. Predictive performances of lipid accumulation product vs. adiposity measures for cardiovascular diseases and all-cause mortality, 8.6-year follow-up: Tehran lipid and glucose study. Lipids Health Dis. 2010;9:45. doi: 10.1186/1476-511X-9-100. [DOI] [PMC free article] [PubMed] [Google Scholar]


