Abstract
Coronary artery disease (CAD) is the leading cause of morbidity and mortality in patients with diabetes. CAD is often asymptomatic in these patients, until the onset of myocardial infarction or sudden cardiac death. Consequently, proper screening and diagnosis of CAD is crucial for the prevention and early treatment of coronary events. This review deals with selection of the sub group of patients who have type 2 diabetes, who are at high risk for developing CAD and need to be screened for the same. The various diagnostic modalities which can be used in the screening process for enhancing risk stratification and management are also discussed.
Keywords: Coronary artery disease, screening, type 2 diabetes mellitus
INTRODUCTION
The current epidemic of Type 2 diabetes and its complications are on a dramatic rise both in the developed and the developing world. Coronary artery disease (CAD) is often asymptomatic in these patients until the onset of myocardial infarction (MI) or sudden cardiac death.[1] The American College of Cardiology (ACC) / American Diabetes Association (ADA) recommends that cardiac testing be done irrespective of the presence of CAD symptoms in diabetics, with two or more atherogenic risk factors.[2]
Diabetes is classified as type 1 and type 2 diabetes, the former associated with insufficient insulin secretion from the beta cells in the pancreas, and the latter characterized by the phenomenon of insulin resistance with relative insulin deficiency. The diagnostic criteria for type 2 diabetes as defined by the ADA is mentioned in Figure 1.[3]
Figure 1.
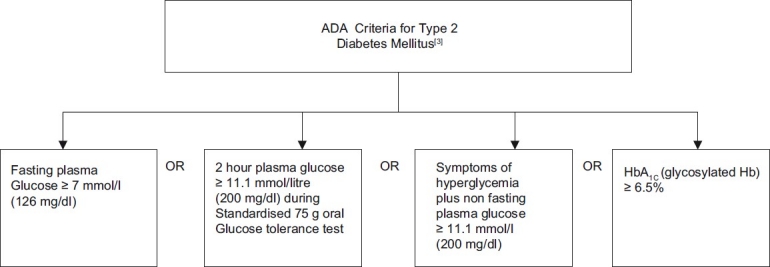
American Diabetes Association criteria for diagnosis of Type 2 diabetes mellitus
Leading cause of mortality in diabetes is cardiovascular diseases (CVD). CVD in diabetic patients is more severe, more complex, and results in higher complication rates than in patients without diabetes.[4]
Diabetes causes microvascular complications (retinopathy, nephropathy, neuropathy) and macrovascular complications (CAD, myocardial ischemia, acute coronary syndrome, cerebrovascular disease and peripheral vascular disease).
The U.S. Preventive Services Task Force (USPSTF) recommends lower blood pressure targets for persons with diabetes and high blood pressure, to reduce the risk of CVD events. In persons with blood pressure of 135/80 mmHg or lower, screening may be considered on an individual basis, if knowledge of diabetes status would help inform decisions about coronary heart disease prevention strategies, including assessment of coronary heart disease risk and subsequent consideration of lipid-lowering agents or aspirin.[5]
Diabetes is considered a CAD risk equivalent according to the Adult Treatment Panel of the National Cholesterol Education Program guidelines. This means that patients with diabetes have a risk for coronary events similar to that of patients without diabetes who have already had an event.[6]
The aim of this review is to provide practitioners with information on the risk factors for CAD in asymptomatic diabetics, the criteria on selection of patients to screen and the various investigation modalities available.
PATHOGENESIS
The microvascular and macrovascular complications of diabetes is mediated primarily by atherosclerosis. Hyperglycemia causes vascular disturbances, especially endothelial dysfunction, contributed by abnormal nitric oxide biology, increased endothelin and angiotensin 2, and reduced prostacyclin activity.[7]
Diabetic dyslipidemia further contributes to the increased atherosclerotic risk. Diabetic dyslipidemia is mainly due to increased low density lipoproteins (LDL), increased apolipoprotein B concentration, increased triglycerides and decreased high density lipoproteins (HDL).[8] The vascular effects of Advanced Glycosylation End Products (AGE s), circulating free fatty acids aggravate the systemic inflammation due to oxidative stress.[9]
Hypoglycemia can contribute to the atherosclerotic risk by the sympathovagal imbalance due to diabetic autonomic neuropathy.
Diabetes leads to a prothrombotic milieu[10] with disturbances in platelet activation and aggregation, thus accelerating atherosclerosis.
Metabolic syndrome has increased in children and adults, reflecting the increased prevalence of obesity, prediabetes and type 2 diabetes.[11,12] Metabolic syndrome is associated with increased risk of fatty streaks and fibrous plaques in the aorta and coronary arteries.[13]
CANDIDATES FOR SCREENING
Increasing age, obesity, increasing longevity of patients with diabetes and sedentary lifestyle has added to the burden of development of CVD in this population. Diabetic patients have a high risk for development of CAD as compared to nondiabetics. CAD increases with advancing age but often occurs at a younger age in patients with diabetes. Occult CAD among asymptomatic diabetics is common, ranging from 20 to more than 50%.[14,15] Hence, screening of diabetics for CAD is of great value.
In type 2 diabetics who are asymptomatic for CAD, the increased risk for MI or cardiac death can be identified by the associated clinical evaluation. The major risk factors identified by the Framingham Risk Score include sex, total cholesterol, HDL cholesterol, blood pressure (or treatment thereof), cigarette smoking, and age.[16]
The appropriate candidates eligible for screening according to the ADA[17] consensus statement on CAD are tabulated in Figure 2.
Figure 2.
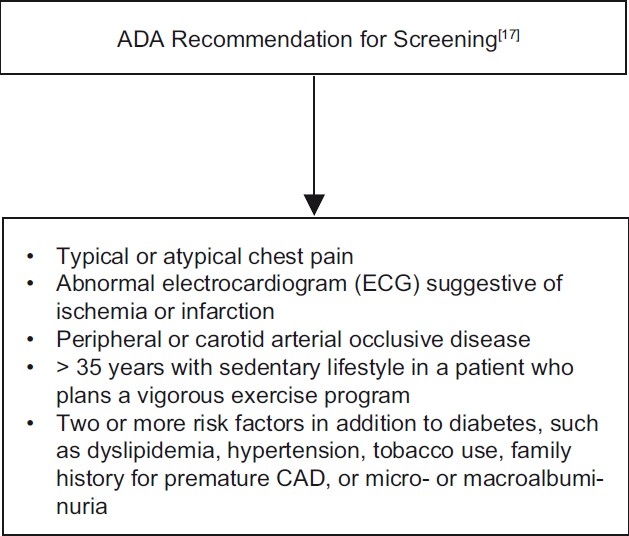
American Diabetes Association recommendations for screening of CAD in diabetics
If the resting ECG shows previously unrecognized MI (i.e., abnormal Q waves or deep T wave inversions, Left Bundle Branch Block, nonspecific ST-T changes), this triggers an evaluation for CAD and inducible ischemia.[18]
The evidence of atherosclerotic vascular disease involving the lower extremities, cerebral, renal or mesenteric arteries, can predict the future chance of a cardiac event.[19] In patients with claudication or asymptomatic peripheral arterial disease, 90% of death are attributable to CAD.[20] A diminished ankle brachial index (ABI) is a sensitive indicator of increased risk for future cardiovascular events.[21]
Patients with type 2 diabetes with chronic kidney disease (CKD) due to diabetic nephropathy have a very high risk for MI and cardiac death , with 40% experiencing a cardiac complication over a 5-year period.[20] Microalbuminuria, defined as urinary albumin excretion from 30 to 300 mg in 24 hours, has been shown to be a harbinger of many of the serious complications in type 2 diabetes, particularly CAD, along with retinopathy, neuropathy and nephropathy.[22,23] Since medical intervention including control of blood glucose, cholesterol and hypertension at the onset of microalbuminuria has been shown to be critical in reducing adverse outcomes , current guidelines recommend that type 2 diabetic patients should be screened annually for microalbuminuria.[24]
Cardiovascular autonomic neuropathy in diabetics , mediated by impairment of ischemia awareness or hemodynamic lability secondary to blunted parasympathetic activation, is associated with a poor overall prognosis.[25] In the Detection of Ischemia in Asymptomatic Diabetics (DIAD) study, cardiac autonomic function testing was found to have an important association with CAD risk assessment of patients with type 2 diabetes. Previous studies have demonstrated the same association between autonomic neuropathy and risk for adverse cardio vascular events.[26] The ADA has recently recommended screening for cardiac autonomic neuropathy, beginning at diagnosis of type 2 diabetes or 5 years after the diagnosis of type 1 diabetes.[27]
Hyperglycemia, evidenced by uncontrolled fasting blood sugar and elevated HbA1c, is a strong predictor of microvascular disease than atherosclerotic macrovascular disease in people with diabetes.[28] Retinopathy, a microvascular complication of diabetes is similarly, a risk factor for CAD in diabetics.[29]
Women with diabetes are considered to be having optimal risk if they have a healthy lifestyle and no CAD risk factors. If there are one or more cardiovascular risk factors, they are considered as at risk, and those having high risk are the ones who already have diabetes with CAD, peripheral arterial disease or CKD.[30] Although diabetes increases relative cardiovascular risk more in females than in males, the absolute risk of cardiovascular events is still higher in men than women.[31] Prevalence of inducible ischemia is significantly higher in patients with type 2 diabetes over the age of 65 years.[32]
Regular monitoring of blood pressure is essential as hypertension predisposes to adverse cardiovascular outcomes. The blood pressure target for these patients is less than 130/80 mm of Hg.[33,34]
Diabetic dyslipidemia is another crucial indicator of adverse cardiovascular outcome in these patients. Hence lipid levels should be monitored, keeping a target to maintain LDL levels below 100 mg/dl or attain a 35-40 % reduction from baseline levels.[33]
The incidence of inducible ischemia is increased in diabetic patients who have unexplained dyspnea or those who are unable to exercise due to dyspnea. This portends a very poor prognosis with adverse cardiovascular complications.[35] Multiple risk factors (Hypertension, dyslipidemia ,inactivity, smoking and abdominal obesity) in the same patient having type 2 diabetes substantially increase the overall cardiovascular risk.[36]
SCREENING TESTS
The technology and the clinical usefulness of screening modalities for cardiovascular diseases have continuously advanced over the past few years. They range from invasive procedures like coronary arteriography to noninvasive tests like electrocardiogram, echocardiography, treadmill testing, coronary computed tomography (CT) angiography and radionuclide studies. These screening tests are vital in diabetics for determining the presence and severity of CAD, and assessing therapeutic options.
Advancements in screening techniques, as discussed later in this review, have expanded the possibilities of extracting more information about the heart's anatomy and physiology, that will extend these clinical applications further.
Echocardiography
Echocardiography remains the most frequently used and usually the initial imaging test to evaluate all cardiovascular diseases related to structural, functional, or hemodynamic abnormality of the heart or great vessels. Echocardiography uses ultrasound beams reflected by cardiovascular structures to produce characteristic lines or shapes caused by normal or altered cardiac anatomy in one, two, or three dimensions by M (motion)–mode, two-dimensional, or three-dimensional echocardiography, respectively. It gives the anatomical and physiological information about the heart without the risk of ionizing radiation or patient discomfort and is well suited for the initial assessment of cardiac diseases. The evolving capabilities of Doppler, 3D echocardiography continue to extend its use. Appreciation of cardiac anatomy and hemodynamics by bedside echocardiography makes a physician's clinical evaluation, including physical examination, more relevant to the care of patients. Thus, echocardiography with its reliable noninvasive hemodynamic evaluation and confident delineation of cardiovascular structures has become an important tool for both risk stratification and assessment of cardiac function.
Stress echocardiography
The advent of stress echocardiography has dramatically reduced the clinical necessity for hemodynamic cardiac catheterization. Stress echocardiography incorporates same techniques used to assess cardiac function at rest (e.g., ejection fraction, cardiac output, segmental wall motion analysis) with stressors such as exercise or a pharmacological agent such as dobutamine infusion (Dobutamine stress echocardiogram or DSE). DSE provides information about Left ventricular (LV) systolic and diastolic function, wall motion abnormalities and assesses for evidence of exercise-induced ischemia. Some studies have also shown exercise echocardiography to be the most cost-effective strategy followed by exercise electrocardiography.[37]
Exercise treadmill test
Exercise electrocardiography is one of the most frequent noninvasive modalities used to assess patients with suspected or proven cardiovascular disease. This test is well-established, inexpensive, and easily available. It is based on standard Bruce protocol, and is mainly used to estimate prognosis, determine functional capacity, the likelihood and extent of coronary artery disease, and the effects of therapy. Dynamic protocols are most frequently used to assess cardiovascular reserve, and those suitable for clinical testing should include a low-intensity warm-up phase. In general, approximately 8-12 minutes of continuous progressive exercise, during which the myocardial oxygen demand is elevated to the patient's maximal level, is optimal for diagnostic and prognostic purposes.[38]
An adequately performed Exercise treadmill test (TMT) can help in deciding the prognosis of the patient. The factors that indicate poor outcome include poor exercise capacity <5 metabolic equivalents (METS), exercise induced angina, low peak blood pressure or fall in systolic blood pressure, chrono-tropic incompetence, low heart rate recovery (HRR) at 1-2 minutes after exercise, and ventricu-lar arrhythmias, especially during the recovery phase.[39–41]
Cardiac catheterization with coronary arteriography
Identification of coronary artery disease and assessment of its extent and severity are the most common indications for cardiac catheterization with coronary arteriography in adults. It is performed by direct injection of radiopaque contrast material into the coronary arteries and recording of digital radiographic images. Coronary arteriography establishes the presence or absence of coronary stenoses, defines therapeutic options, and determines the prognosis of patients with symptoms or signs of ischemic CAD.[42]
Although coronary arteriography is considered the gold standard for identifying obstructive lesions, it is never used as an initial screening test. It is indicated in patients who show evidence of ischemia on a stress test or for those who continue to be symptomatic in spite of a negative stress test (suspected false negative results).[43] Cardiac catheterization with coronary arteriography aids in the adequate assessment of coronary anatomy in these patients.
Coronary computed tomography angiogram
The basic principle of computed tomography (CT) technology is the use of ionizing radiation within a gantry rotating around the patient in which X-rays are detected on a detector array and converted through reconstruction algorithms to images. It is these images, acquired at high spatial and temporal resolution, that have enabled cardiovascular medicine to enter the CT imaging era. CT Angiography utilizes intravenous iodinated contrast injection in order to visualize the contrast-filled coronary vessels.
Among the indications of coronary computed tomography angiogram (CCTA) in screening diabetics for CAD, detection of coronary stenosis is the most important. Coronary stenosis should be ruled out in patients with low to intermediate risk for CAD. This is especially helpful in patients who are unable to undergo invasive angiography or who are at a high risk for the procedure.[44]
With the recent development of the latest models of Multislice CT (MSCT) such as 16, 64, dual source, 256 and 320 slice CT scanners, the diagnostic accuracy of MSCT angiogram in CAD has significantly improved.[45,46] The clinical application of CT angiogram is of enormous value in the evaluation of patients who have a low likelihood of CAD . No further screening test is required in those patients in whom a high-quality MSCT shows no coronary stenosis.[44] MSCT has further contributed to better image quality in cardiac imaging by the introduction of dual source CT in 2006, as the temporal resolution is shortened from 165 to 83 ms and heart rate dependence is eliminated.[47] Several meta-analysis of 64 slice CT studies have reported an impressive range of results in sensitivity and specificity (99% sensitivity and 89% specificity in 28 studies).[48,49] The development of 320 slice CT has improved the diagnostic accuracy in the detection of CAD. It allows a whole heart coverage in one gantry rotation with a slice thickness of 0.5 mm,[46,50] and a 16-cm craniocaudal coverage can be obtained in a single heart beat, with excellent image quality and demonstration of the entire coronary arteries. Patient-based analysis has proven the diagnostic accuracy of 320 slice CT angiogram upto 95%, in the detection of more than 50% coronary stenosis.[51]
Therefore MSCT, (especially with 64 slice or more CT), has developed as an effective alternative to invasive coronary angiography, for the detection of CAD. It can be used as a highly sensitive screening modality, that achieves high diagnostic accuracy for the detection of significant CAD.
Coronary calcium score
Coronary calcium score (CCS) on CT can be highly correlated with total coronary atherosclerotic burden and it identifies asymptomatic diabetics at higher risk for inducible ischemia.[52] Coronary calcium score is quanti-fied by calculating the Agatston score, the volume score, and the absolute mass score. The Agatston score for each lesion in each segment of coronary artery is computed as the prod-uct of the area of each lesion with a weighting fac-tor assigned according to the maximum attenuation value of the lesion.[53] The sum of the scores for all lesions in all coronary artery segments yields the to-tal Agatston score. The volume score for each lesion is estimated as the product of the number of voxels containing calcium and the volume of one voxel.[54] The scores for all lesions in all coronary arteries is summed to obtain the total volume score.
Table 1 mentions the categories of CCS.[43]
Table 1.
Categories of coronary calcium scoring[43]
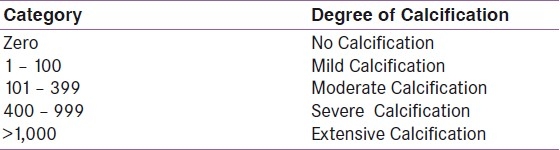
If the CCS is zero, it is associated with a high level of confidence that an individual has no obstructive CAD with a very low rate of death or MI over 3-5 years.[55,56] It is well established that the detection of coronary calcium indicates an increased risk of incident coronary artery disease above that predicted by standard risk factors, from 2-fold for scores of up to 100 and increasing to 11-fold for scores above 1000.[56]
The drawback of CCS lies in the fact that it is an anatomical study and not a functional one. Hence , it may be considered only as a second-line testing modality or for patients who are unable to exercise.[56] However, CCS can confirm or reclassify individual risk derived from the initial risk assessment[55] and hence is preferred as the initial mode of screening for CAD in patients who do not achieve therapeutic targets with medical treatment.[57]
Magnetic resonance imaging
Cardiovascular magnetic resonance imaging (MRI) is well established particularly for the assessment of cardiac function.[58] Pharmacological stress testing using dobutamine or adenosine can be applied along with cardiac magnetic resonance imaging (CMR) and is well established for assessing myocardial ischemia.[59,60] The technique is used in a similar way to stress echo, but has no limitations from restricted acoustic access and it can be combined with perfusion and viability imaging using a contrast agent.
Nuclear cardiac imaging
Nuclear cardiology is an established subspeciality that has grown significantly in recent years due to the fact that functional information provided by nuclear techniques can play a good role in clinical cardiology.
Single Photon Emission Computed Tomography
The clinical application of Single Photon Emission Computed Tomography (SPECT), as a modality to assess myocardial perfusion is growing worldwide, especially in the screening protocol for diabetics with risk of CAD. The accuracy of SPECT for myocardial perfusion is approaching that of Positron Emission Tomography (PET)[61] with the emergence of vasodilator stress SPECT myocardial perfusion imaging. This is of enormous value in patients who are unable to complete a symptom limited exercise test due to obesity, PVD or peripheral neuropathy, where therapeutic intervention may be required. Medical stress test with SPECT imaging assesses myocardial ischemia with sensitivity of 91-96% and specificity of 75-82%.[43] The information from doing a gated SPECT has incremental prognostic value over coronary angiography in patients with known or suspected ischemic heart disease.[62] This has definite advantages over clinical, electrocardiographic, lab and resting echocardiographic data, as it describes the severity and extent of stress-induced myocardial perfusion abnormality. The clinical outcome of the patient can be better predicted on the basis of ischemic abnormalities on noninvasive testing, than the presence or absence of angina.[63] The presence of reversible defects in SPECT myocardial perfusion imaging can define a silent MI in diabetics.[15,64,65]
Positron Emission Tomography
PET has several advantages over SPECT for cardiac imaging, including better spatial resolution, higher sensitivity and the ability to measure tracer distribution in absolute terms as a function of time. PET can assess myocardial perfusion and metabolism.
Other modalities of screening
Left ventricular hypertrophy
Left ventricular hypertrophy (LVH) detected by ECG or echocardiography can be used as a predictor for CAD in asymptomatic diabetics.[66]
Carotid intimal medial thickness
Carotid intimal medial thickness (CIMT), measured by B-mode ultrasonography is a noninvasive and easily applicable method of documenting the atherosclerotic process in adults.[67] Intima- media complex thickening greater than 0.8 mm is abnormal and represent the earliest marker of atherosclerotic burden in asymptomatic population. Asymptomatic patients with increased CIMT are predisposed to increased risk of MI.[68] The relation between CIMT and presence of CAD is independent of other cardiovascular risk factors.[69]
Ankle brachial index
ABI is the ratio of the blood pressure in the lower legs to the blood pressure in the arms. A diminished ABI is a sensitive indicator of increased risk for future cardiovascular events.[21] This index reclassifies a substantial proportion of patients towards the high-risk category of developing cardiovascular diseases.[70]
Cardiac autonomic neuropathy
Various studies have suggested an association between autonomic neuropathy and asymptomatic ischemia.[71–73] A decreased heart rate response to Valsalva manoeuvre is associated with moderate to large perfusion defects on radionuclide myocardial imaging.[15]
CONCLUSIONS
Although it remains controver-sial to screen asymptomatic patients with diabetes, screening patients with a limited func-tional status is probably a reasonable approach for people at moderate to high risk of underlying CAD. An exercise TMT can be a safe and effective initial screening test in patients who can exer-cise and have a normal baseline ECG. If, based on the assessment, a tread-mill stress test is not the best study for a particular patient, an imaging study may be considered. Screening should also be con-sidered in patients with an abnormal ECG tracing suggestive of ischemia or infarction. If the results of an anatomi-cal study, such as CCS or CCTA, are abnormal, a functional study, such as a nuclear stress or stress echocardiog-raphy study, is recommended to assess for the presence of ischemia. Coronary arteriography remains the gold standard for identifying obstructive lesions, though it is never used as an initial screening test.
FUTURE
Further research is needed for identification of diabetics at high risk of developing acute coronary events that are precipitated by plaque rupture and thrombosis. Future studies in this field should aim on use of biomarkers and genetic testing along with the present imaging techniques.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Jouven X, Lemaitre RN, Rea TD, Sotoodehnia N, Empana JP, Siscovick DS. Diabetes, glucose level, and risk of sudden cardiac death. Eur Heart J. 2005;26:2142–7. doi: 10.1093/eurheartj/ehi376. [DOI] [PubMed] [Google Scholar]
- 2.Consensus development conference on the diagnosis of coronary heart disease in people with diabetes: 10-11 February 1998, Miami, Florida. American Diabetes Association. Diabetes Care. 1998;21:1551–9. doi: 10.2337/diacare.21.9.1551. [DOI] [PubMed] [Google Scholar]
- 3.American Diabetes Association: Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Albers AR, Krichavsky MZ, Balady GJ. Stress testing in patients with diabetes mel-litus. Circulation. 2006;113:583–92. doi: 10.1161/CIRCULATIONAHA.105.584524. [DOI] [PubMed] [Google Scholar]
- 5.The Guide to Clinical Preventive Services 2010-2011. Recommendations of the U.S Preventive Services Task Force (USPSTF) [PubMed] [Google Scholar]
- 6.Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Mortality from coronary heart disease in sub-jects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339:229–34. doi: 10.1056/NEJM199807233390404. [DOI] [PubMed] [Google Scholar]
- 7.Rask-Madsen C, King GL. Mechanisms of disease: Endothelial dysfunction in insulin resistance and diabetes. Nat Clin Pract Endocrinol Metab. 2007;3:46–56. doi: 10.1038/ncpendmet0366. [DOI] [PubMed] [Google Scholar]
- 8.Khera A, McGuire DK. Management of diabetic dyslipidemia: Need for reappraisal of the goals. Am J Cardiovasc Drugs. 2005;5:83. doi: 10.2165/00129784-200505020-00002. [DOI] [PubMed] [Google Scholar]
- 9.Libby P, Plutzky J. Inflammation in diabetes mellitus: Role of peroxisome proliferator–activated receptor-alpha and peroxisome proliferator–activated receptor-gamma agonists. Am J Cardiol. 2007;99:27B–40. doi: 10.1016/j.amjcard.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Mathewkutty S, McGuire DK. Platelet perturbations in diabetes: Implications for cardiovascular disease risk and treatment. Expert Rev Cardiovasc Ther. 2009;7:541–9. doi: 10.1586/erc.09.30. [DOI] [PubMed] [Google Scholar]
- 11.Pinhas-Hamiel O, Zeitler P. The global spread of type 2 diabetes mellitus in children and adolescents. J Pediatr. 2005;146:693–700. doi: 10.1016/j.jpeds.2004.12.042. [DOI] [PubMed] [Google Scholar]
- 12.Pinhas-Hamiel O, Dolan LM, Daniels SR, Standiford D, Khoury PR, Zeitler P. Increased incidence of non-insulin dependent diabetes mellitus among adolescents. J Pediatr. 1996;128:608–15. doi: 10.1016/s0022-3476(96)80124-7. [DOI] [PubMed] [Google Scholar]
- 13.Berenson GS, Srinivasan SR, Bao W, Newman WP, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and the early development of atherosclerosis.Bogalusa Heart Study. N Engl J Med. 1998;338:1650–6. doi: 10.1056/NEJM199806043382302. [DOI] [PubMed] [Google Scholar]
- 14.Di Carli MF, Hachamovitch R. Should we screen for occult coronary artery disease among asymptomatic patients with diabetes? J Am Coll Cardiol. 2005;45:50–3. doi: 10.1016/j.jacc.2004.09.055. [DOI] [PubMed] [Google Scholar]
- 15.Wackers FJ, Young LH, Inzucchi SE, Chyun DA, Davey JA, Barrett EJ, et al. Detection of silent myocardial ischemia in asymptomatic diabetic subjects: The DIAD study. Diabetes Care. 2004;27:1954–61. doi: 10.2337/diacare.27.8.1954. [DOI] [PubMed] [Google Scholar]
- 16.Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 17.American Diabetes Association: Standards of medical care in diabetes. Diabetes Care. 2007;30:S4–41. doi: 10.2337/dc07-S004. [DOI] [PubMed] [Google Scholar]
- 18.Rajagopalan N, Miller TD, Hodge DO, Frye RL, Gibbons RJ. Identifying high risk asymptomatic diabetic patients who are candidates for screening stress singlephoton emission computed tomography imaging. J Am Coll Cardiol. 2005;45:43–9. doi: 10.1016/j.jacc.2004.06.078. [DOI] [PubMed] [Google Scholar]
- 19.Golomb BA, Dang TT, Criqui MH. Peripheral arterial disease: Morbidity and mortality implications. Circulation. 2006;114:688–99. doi: 10.1161/CIRCULATIONAHA.105.593442. [DOI] [PubMed] [Google Scholar]
- 20.Mann JF, Gerstein HC, Pogue J, Bosch J, Yusuf S. Renal insufficiency as a predictor of cardiovascular outcomes and the impact of ramipril: The HOPE randomized trial. Ann Intern Med. 2001;134:629–36. doi: 10.7326/0003-4819-134-8-200104170-00007. [DOI] [PubMed] [Google Scholar]
- 21.Doobay AV, Anand SS. Sensitivity and specificity of the ankle-brachial index to predict future cardiovascular outcomes: A systematic review. Arterioscler Thromb Vasc Biol. 2005;25:1463–9. doi: 10.1161/01.ATV.0000168911.78624.b7. [DOI] [PubMed] [Google Scholar]
- 22.Berrut G, Bouhanick B, Fabbri P. Microalbuminuria as a predictor of a drop in glomerular filtration rate in subjects with non Insulin dependant Diabetes Mellitus and Hypertension. Clin Nephrol. 1997;48:92–7. [PubMed] [Google Scholar]
- 23.Savage S, Estacio RO, Jeffers BW, Shrier RW. Urinary albumin excretion as a predictor of diabetic retinopathy, neuropathy and cardiovascular diseases in NIDDM. Diabetes Care. 1996;19:1243–8. doi: 10.2337/diacare.19.11.1243. [DOI] [PubMed] [Google Scholar]
- 24.Bennett PH, Haffner S, Kasiske BL, Keane WF, Mogensen CE, Parving HH, et al. Screening and management of microalbuminuria in patients with diabetes mellitus: Recommendations to the Scientific Advisory Board of the National Kidney Foundation from an ad hoc committee of the Council on Diabetes Mellitus of the National Kidney Foundation. Am J Kidney Dis. 1995;25:107–12. doi: 10.1016/0272-6386(95)90636-3. [DOI] [PubMed] [Google Scholar]
- 25.Vinik AI, Maser RE, Mitchell BD, Freeman R. Diabetic autonomic neuropathy. Diabetes Care. 2003;26:1553–79. doi: 10.2337/diacare.26.5.1553. [DOI] [PubMed] [Google Scholar]
- 26.Gerritsen J, Heine RJ, Dekker JM, Bouter LM, TenVoorde BJ, Heethaar RM, et al. Impaired autonomic function is associated with increased mortality, especially in subjects with diabetes, hypertension, or a history of cardiovascular disease. Diabetes Care. 2001;24:1793–8. doi: 10.2337/diacare.24.10.1793. [DOI] [PubMed] [Google Scholar]
- 27.Boulton AJ, Vinik AI, Arezzo JC, Bril V, Feldman EL, Freeman R, et al. Diabetic neuropathies: A statement by the American Diabetes Association (ADA Statement) Diabetes Care. 2005;28:956–62. doi: 10.2337/diacare.28.4.956. [DOI] [PubMed] [Google Scholar]
- 28.Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33): UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352:837–53. [PubMed] [Google Scholar]
- 29.Klein BE, Klein R, McBride PE, Cruickshanks KJ, Palta M, Knudtson MD, et al. Cardiovascular disease, mortality, and retinal microvascular characteristics in type 1 diabetes: Wisconsin epidemiologic study of diabetic retinopathy. Arch Intern Med. 2004;164:1917–24. doi: 10.1001/archinte.164.17.1917. [DOI] [PubMed] [Google Scholar]
- 30.Mosca L, Banka CL, Benjamin EJ, Berra K, Bushnell C, Dolor RJ, et al. Evidence-based guidelines for cardiovascular disease preven-tion in women: 2007 update. J Am Coll Cardiol. 2007;49:1230–50. doi: 10.1016/j.jacc.2007.02.020. [DOI] [PubMed] [Google Scholar]
- 31.Abbott RD, Donahue RP, Kannel WB, Wilson PW. The impact of diabetes on survival following myocardial infarction in men vs women: The Framingham Study. JAMA. 1988;260:3456–60. [PubMed] [Google Scholar]
- 32.Chaowalit N, Arruda AL, McCully RB, Bailey KR, Pellikka PA. Dobutamine stress echocardiography in patients with diabetes mellitus: Enhanced prognostic prediction using a simple risk score. J Am Coll Cardiol. 2006;47:1029–36. doi: 10.1016/j.jacc.2005.10.048. [DOI] [PubMed] [Google Scholar]
- 33.American Diabetes Association: Standards of medical care in diabetes-2010. Diabetes Care. 2010;33(Suppl 1):S11. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pignone M, Alberts MJ, Colwell JA, Cushman M, Inzucchi SE, Mukherjee D, et al. Aspirin for primary prevention of cardiovascular events in people with diabetes: A position statement of the American Diabetes Association, a scientific statement of the American Heart Association, and an expert consensus document of the American College of Cardiology Foundation. Circulation. 2010;121:2694–701. doi: 10.1161/CIR.0b013e3181e3b133. [DOI] [PubMed] [Google Scholar]
- 35.Vanzetto G, Halimi S, Hammoud T, Fagret D, Benhamou PY, Cordonnier D, et al. Prediction of cardiovascular events in clinically selected high-risk NIDDM patients: Prognostic value of exercise stress test and thallium- 201 single-photon emission computed tomography. Diabetes Care. 1999;22:19–26. doi: 10.2337/diacare.22.1.19. [DOI] [PubMed] [Google Scholar]
- 36.Mortality after 16 years for participants randomized to the Multiple Risk Factor Intervention Trial. Circulation. 1996;94:946–51. doi: 10.1161/01.cir.94.5.946. [DOI] [PubMed] [Google Scholar]
- 37.Hayashino Y, Kobayashi SN, Morimoto T, Maeda K, Shimbo T, Fukui T, et al. Cost-effectiveness of Screening for Coronary Artery Disease in Asymptomatic Patients with Type 2 Diabetes and Additional Atherogenic Risk Factors. J Gen Intern Med. 2004;19:1181–91. doi: 10.1111/j.1525-1497.2004.40012.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Froelicher VF, Myers J. 5th ed. Philadelphia: WB Saunders; 2006. Exercise and the Heart. [Google Scholar]
- 39.Lauer MS. What is the best test for a patient with classic angina? Cleveland Clin J Med. 2007;74:123–6. doi: 10.3949/ccjm.74.2.123. [DOI] [PubMed] [Google Scholar]
- 40.Dewey FE, Kapoor JR, Williams RS, Lipinski MJ, Ashley EA, Hadley D, et al. Ventricular arrhythmias during clinical treadmill testing and prognosis. Arch Intern Med. 2008;168:225–34. doi: 10.1001/archinte.168.2.225. [DOI] [PubMed] [Google Scholar]
- 41.Curfman GD, Hillis LD. A new look at cardiac exercise testing. N Engl J Med. 2003;348:775–6. doi: 10.1056/NEJMp030004. [DOI] [PubMed] [Google Scholar]
- 42.Conti R. The continuing value of invasive coronary arteriography. Clin Cardiol. 2008;31:345. doi: 10.1002/clc.20408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Roelker E. Screening for Coronary artery disease in patients with Diabetes. Diabetes Spectr. 2008;21:166–71. [Google Scholar]
- 44.Achenbach S. Top 10 indications for coronary CTA. Ruling out stenosis in patients at low-to-intermediate risk for coronary artery disease tops the list, but coronary CT angiography has a much broader role to play. Supplement to Applied Radiology. 2006:22–8. [Google Scholar]
- 45.Nieman K, Oudkerk M, Rensing BJ, van Ooijen P, Munne A, van Geuns RJ, et al. Coronary angiography with multi-slice computed tomography. Lancet. 2001;357:599–603. doi: 10.1016/S0140-6736(00)04058-7. [DOI] [PubMed] [Google Scholar]
- 46.Dewey M, Zimmermann E, Deissenrieder F, Laule M, Dübel HP, Schlattmann P, et al. Noninvasive coronary angiography by 320-row computed tomography with lower radiation exposure and maintained diagnostic accuracy: comparison of results with cardiac catheterization in a head-to-head pilot investigation. Circulation. 2009;120:867–75. doi: 10.1161/CIRCULATIONAHA.109.859280. [DOI] [PubMed] [Google Scholar]
- 47.Flohr TG, McCollough CH, Bruder H, Petersilka M, Gruber K, Suss C, et al. First performance evaluation of a dual-source CT (DSCT) system. Eur Radiol. 2006;16:256–68. doi: 10.1007/s00330-005-2919-2. [DOI] [PubMed] [Google Scholar]
- 48.Vanhoenacker PK, Heijenbrok-Kal MH, Van Heste R, Decramer I, Van Hoe LR, Wijns W, et al. Diagnostic performance of multidetector CT angiography for assessment of coronary artery disease: Meta-analysis. Radiology. 2007;244:419–28. doi: 10.1148/radiol.2442061218. [DOI] [PubMed] [Google Scholar]
- 49.Mowatt G, Cook JA, Hillis GS, Walker S, Fraser C, Jia X, et al. 64-Slice computed tomography angiography in the diagnosis and assessment of coronary artery disease: Systematic review and meta-analysis. Heart. 2008;94:1386–93. doi: 10.1136/hrt.2008.145292. [DOI] [PubMed] [Google Scholar]
- 50.Rybicki FJ, Otero HJ, Steigner ML, Vorobiof G, Nallamshetty L, Mitsouras D, et al. Initial evaluation of coronary images from 320-detector row computed tomography. Int J Cardiovasc Imaging. 2008;24:535–46. doi: 10.1007/s10554-008-9308-2. [DOI] [PubMed] [Google Scholar]
- 51.Graaf FR, Schuijf JD, Velzen JE, Kroft LJ, Roos A, Reiber JH, et al. Diagnostic accuracy of 320-row multidetector computed tomography coronary angiography in the non-invasive evaluation of significant coronary artery disease. Eur Heart J. 2010;31:1908–15. doi: 10.1093/eurheartj/ehp571. [DOI] [PubMed] [Google Scholar]
- 52.Anand DV, Lim E, Hopkins D, Corder R, Shaw LJ, Sharp P, et al. Risk stratification in uncomplicated type 2 diabetes: Prospective evaluation of the combined use of coronary artery calcium imaging and selective myocardial perfusion scintigraphy. Eur Heart J. 2006;27:713–21. doi: 10.1093/eurheartj/ehi808. [DOI] [PubMed] [Google Scholar]
- 53.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–32. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 54.Callister TQ, Cooil B, Raya SP, Lippolis NJ, Russo DJ, Raggi P. Coronary artery disease: Improved reproducibility of calcium scoring with an electron-beam CT volumetric method. Radiology. 1998;208:807–14. doi: 10.1148/radiology.208.3.9722864. [DOI] [PubMed] [Google Scholar]
- 55.Erbel R, Mohlenkamp S, Kerkhoff G, Budde T, Schmermund A. Non-invasive screening for coronary artery disease: Calcium scoring. Heart. 2007;93:1620–9. doi: 10.1136/hrt.2005.071258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Greenland P, Bonow RO, Brundage BH, Budoff MJ, Eisenberg MJ, Grundy SM, et al. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardio-vascular risk assessment and in evaluation of patients with chest pain. J Am Coll Cardiol. 2007;49:378–402. doi: 10.1016/j.jacc.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 57.Bax JJ, Young LH, Frye RL, Bonow RO, Steinberg HO, Barrett EJ. Screening for coro-nary artery disease in patients with diabetes. Diabetes Care. 2007;30:2729–36. doi: 10.2337/dc07-9927. [DOI] [PubMed] [Google Scholar]
- 58.Boxt LM. Cardiac MR imaging: A guide for the beginner. Radio Graphics. 1999;19:1009–25. doi: 10.1148/radiographics.19.4.g99jl161009. [DOI] [PubMed] [Google Scholar]
- 59.Hundley WG, Hamilton CA, Rerkpattanapipat P. Magnetic Resonance imaging assessment of cardiac function. Curr Cardiol Rep. 2003;5:69–74. doi: 10.1007/s11886-003-0040-1. [DOI] [PubMed] [Google Scholar]
- 60.Paetsch I, Jahnke C, Wahl A, Gebker R, Neuss M, Fleck E, et al. Comparison of dobutamine stress magnetic resonance, adenosine stress magnetic resonance and adenosine stress magnetic resonance perfusion. Circulation. 2004;110:835–42. doi: 10.1161/01.CIR.0000138927.00357.FB. [DOI] [PubMed] [Google Scholar]
- 61.Chen EQ, Maclntyre WJ, Go RT, Brunken RC, Saha GB, Wong CO, et al. Myocardial viability studies using fluorine – 18- FDG SPECT: A comparison with fluorine – 18– FDG PET. J Nucl Med. 1997;38:582–6. [PubMed] [Google Scholar]
- 62.Gimelli A, Rossi G, Landi P, Marzullo P, Iervasi G, Abbate AC, et al. Stress/rest myocardial perfusion abnormalities by gated SPECT: Still the best predictor of cardiac events in stable ischemic heart disease. J Nucl Med. 2009;50:546–53. doi: 10.2967/jnumed.108.055954. [DOI] [PubMed] [Google Scholar]
- 63.Giri S, Shaw LJ, Murthy DR, Travin MI, Miller DD, Hachamovitch R, et al. Impact of diabetes on the risk stratification using stress single-photon emission computed tomography myocardial perfusion imaging in patients with symptoms suggestive of coronary artery disease. Circulation. 2002;105:32–40. doi: 10.1161/hc5001.100528. [DOI] [PubMed] [Google Scholar]
- 64.Scholte A, Schuijf J, Kharagjitsingh A, Dibbets-Schneider P, Stokkel M, van der Wall E, et al. Prevalence and predictors of an abnormal l stress myocardial perfusion study in asymptomatic patients with type 2 diabetes mellitus. Eur J Nucl Med Mol Imaging. 2009;36:567–75. doi: 10.1007/s00259-008-0967-y. [DOI] [PubMed] [Google Scholar]
- 65.Bax J, Bonow R, Tscho¨pe M, Inzuchi S, Barrett E. On behalf of the Global Dialogue Group for the Evaluation of Cardiovascular Risk in Patients with Diabetes. The potential of myocardial perfusion scintigraphy for risk stratification of asymptomatic patients with type 2 diabetes. J Am Coll Cardiol. 2006;48:754–60. doi: 10.1016/j.jacc.2006.04.077. [DOI] [PubMed] [Google Scholar]
- 66.Somaratne JB, Whalley GA, Poppe KK, Balls MM, Wadams G, Pearl A, et al. Screening for left ventricular hypertrophy in patients with type 2 diabetes mellitus in the community. Cardiovasc Diabetol. 2011;10:29. doi: 10.1186/1475-2840-10-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Davis PH, Dawson JD, Riley WA, Lauer RM. Carotid intimal medial thickness is related to cardiovascular risk factors measured from childhood through middle age: The Muscatine Study. Circulation. 2001;104:2815–9. doi: 10.1161/hc4601.099486. [DOI] [PubMed] [Google Scholar]
- 68.Greenland P, Abrams J, Aurigemma GP, Bond MG, Clark LT, Criqui MH, et al. Prevention Conference V: Non invasive tests of atherosclerotic burden. Circulation. 2000;101:111–6. doi: 10.1161/01.cir.101.1.e16. [DOI] [PubMed] [Google Scholar]
- 69.Hansa G, Bhargava K, Bansal M, Tandon S, Kasliwal RA. Carotid Intima-Media Thickness and Coronary Artery Disease: An Indian Perspective. Asian Cardiovasc Thorac Ann. 2003;11:217–21. doi: 10.1177/021849230301100308. [DOI] [PubMed] [Google Scholar]
- 70.Baena-Diez JM, Alzamora MT, Fores R, Pera G, Toran P, Sorribes M. Ankle-brachial index improves the classification of cardiovascular risk PERART/ARTPER Study. Rev Esp Cardiol. 2011;64:186–92. doi: 10.1016/j.recesp.2010.10.024. [DOI] [PubMed] [Google Scholar]
- 71.Milan Study on Atherosclerosis and Diabetes Group. Prevalence of unrecognized silent myocardial ischemia and its association with atherosclerotic factors in noninsulin- dependent diabetes mellitus. Am J Cardiol. 1997;79:134–9. doi: 10.1016/s0002-9149(96)00699-6. [DOI] [PubMed] [Google Scholar]
- 72.Langer A, Freeman MR, Josse RG, Steiner G, Armstrong PW. Detection of silent myocardial ischemia in diabetes mellitus. Am J Cardiol. 1991;67:1073–8. doi: 10.1016/0002-9149(91)90868-l. [DOI] [PubMed] [Google Scholar]
- 73.Lee K, Jang H, Kim Y, Lee EJ, Choe YS, Choi Y, et al. Prognostic value of cardiac autonomic neuropathy independent and incremental to perfusion defects in patients with diabetes and suspected coronary artery disease. Am J Cardiol. 2003;92:1458–61. doi: 10.1016/j.amjcard.2003.08.060. [DOI] [PubMed] [Google Scholar]


