Abstract
Context:
Current literature suggests that laparoscopic nephrectomy (LN) in patients with xanthogranulomatous pyelonephritis (XGP) is associated with high conversion and complication rate.
Aims:
To report contemporary outcome of patients with XGP, managed with either open nephrectomy (ON) or LN.
Settings and Design:
In this retrospective study, medical records of 37 patients with histopathologically confirmed XGP from January 2001 to October 2009 were reviewed.
Materials and Methods:
The clinical presentation, preoperative course, intraoperative findings, postoperative recovery and complications in ON and LN were analyzed.
Statistical Analysis:
Student's t test was used to perform statistical comparison between the LN and ON groups. Values are expressed as mean ± standard deviation.
Results:
In 37 patients, 20 underwent ON and 17 underwent LN. One patient in the LN group required conversion. He had ectopic pelvic kidney, and the vascular pedicle could not be identified because of dense adhesions. There were no intraoperative complications. The mean blood loss was 257.5 ± 156.67 ml and 141.18 ± 92.26 ml in ON and LN groups, respectively. Mean hospital stay was 15.45 ± 7.35 days and 9.71 ± 4.55 days in ON and LN groups, respectively. Postoperative complications were classified according to Clavien grading for surgical complications. Grade 2 complications were seen in 40% and 29.4% of patients in ON and LN groups, respectively. One patient in LN required secondary suturing of specimen retrieval site.
Conclusions:
LN in patients with XGP is often challenging and requires considerable experience in laparoscopy. In properly selected patients, all benefits of minimally invasive surgery can be availed with LN.
Keywords: Laparoscopy nephrectomy, open nephrectomy, xanthogranulomatous pyelonephritis
INTRODUCTION
Xanthogranulomatous pyelonephritis (XGP) is characterized by diffuse or focal, chronic, severe renal parenchymal infection leading to destruction and replacement of the renal parenchyma by lipid-laden macrophages (foamy cells) which impart yellowish tan to the tissue.[1] Nephrectomy is the treatment of choice for XGP. Inflammatory involvement of renal pelvis, hilum and adjacent structures leads to dense fibrotic reaction and obliteration of the tissue planes, which makes this procedure challenging.[2,3] The aim of this retrospective study was to analyze the feasibility of laparoscopic approach and to compare it with open approach.
MATERIALS AND METHODS
The medical records of 37 patients were reviewed. We retrospectively reviewed the surgical pathology reports from January 2001 to October 2009. XGP was diagnosed in 37 patients. Information on clinical presentation, operative detail, postoperative course and complications was reviewed and the outcome was compared in open nephrectomy (ON) and laparoscopic nephrectomy (LN) groups. Of these 37 subjects, 20 were approached by ON and 17 by LN. The selection for either approach was based on the clinical assessment (age of patients, comorbid illness, extension of lump and tenderness, features of sepsis, past history of various approaches of intervention), computed tomography findings (focal or diffuse enlargement, perinephric extension) and surgeon's discretion. Contrast-enhanced computed tomography (CECT) [Figure 1] helps in identifying the relationship with surrounding structures. This is of help particularly if the images are scrolled on the console. The surgeon can have a 3D picture of what he will expect intraoperatively. The relationship of the artery and vein with each other, number of lumbar veins, size and extent of lymph node mass, the lie of the kidney, the extent of the disease beyond the gerotas can be assessed. It helps in identifying relationship with the surrounding structures, relationship of upper pole with diaphragm and inflammatory renal parenchyma. This helps the surgeon to assess “prehand” the difficulties he might expect. Laparoscopic procedures were performed by transperitoneal route, except in one in whom retroperitoneal approach was used.
Figure 1.
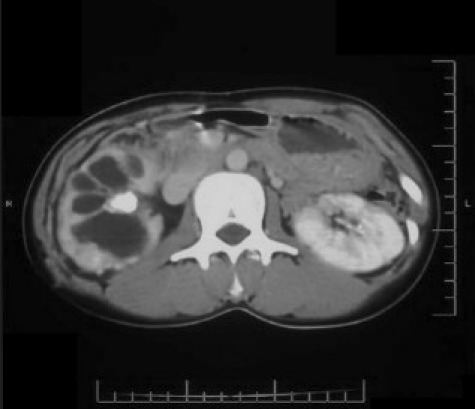
Preop CECT scan from a patient with XGP who underwent successful LN
Operative technique
Transperitoneal approach: Patient was placed in lateral decubitus position. Under anesthesia, surface marking of rectus abdominis muscle, anterior superior iliac spine and costal margin was done. Ports were placed in standard position [Figure 2]. The colon was reflected medially off the kidney. Preoperative placement of ureteric catheter on ipsilateral side facilitated the identification of ureter and the pelvis which was lifted up to assist exposure of the renal hilum. The upper pole dissection as well as hilar dissection were challenging because of intense inflammatory reaction and involvement of renal pelvis, renal vessels and the surrounding structures obscuring anatomical planes. Renal hilar dissection was done using hook and harmonic scalpel. Renal hilar vessels were taken care of separately by using Hem-o-lock™ clips. Dense adhesions when present at upper pole were dissected with harmonic scalpel. Extragerotal dissection was preferred to prevent entry into the infected renal unit, but at times subcapsular nephrectomy was required [Figure 3]. Spillage of pus or infected urine was avoided by applying clips on either side of the ureter prior to its division. Specimen was placed in indigenously made specimen retrieval bag. The specimen was extracted through extension of 11-mm port or iliac fossa incision. ON was performed by standard flank approach. Retroperitoneal procedure was performed, similar to the procedure described by Gill.[4]
Figure 2.

Port placement
Figure 3.
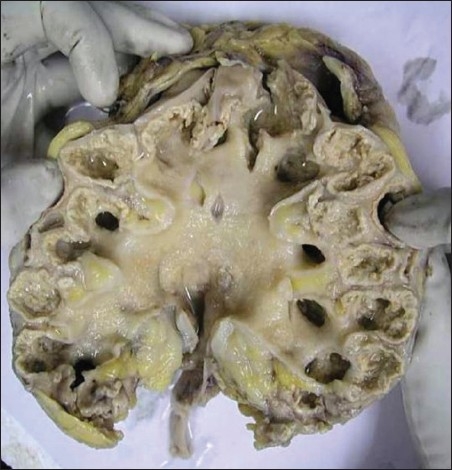
Specimen of a patient with XGP who underwent LN
Student's t test was used to perform statistical comparison between the LN and ON groups. Values are expressed as mean ± standard deviation.
RESULTS
Of the 37 patients, 20 were in ON group and 17 were in LN group. Preoperative diagnosis of XGP was suspected in 17 (46%) patients based on clinical and imaging study findings. Detailed demographic data of patients including clinical presentation, associated comorbid conditions, significant past history and physical examination findings are as shown in Table 1. Positive urine culture was present in 30% and 35.3% of patients in ON and LN groups, respectively. The most common organism was Escherichia coli.
Table 1.
Data of 37 patients undergoing surgery for xanthogranulomatous pyelonephritis
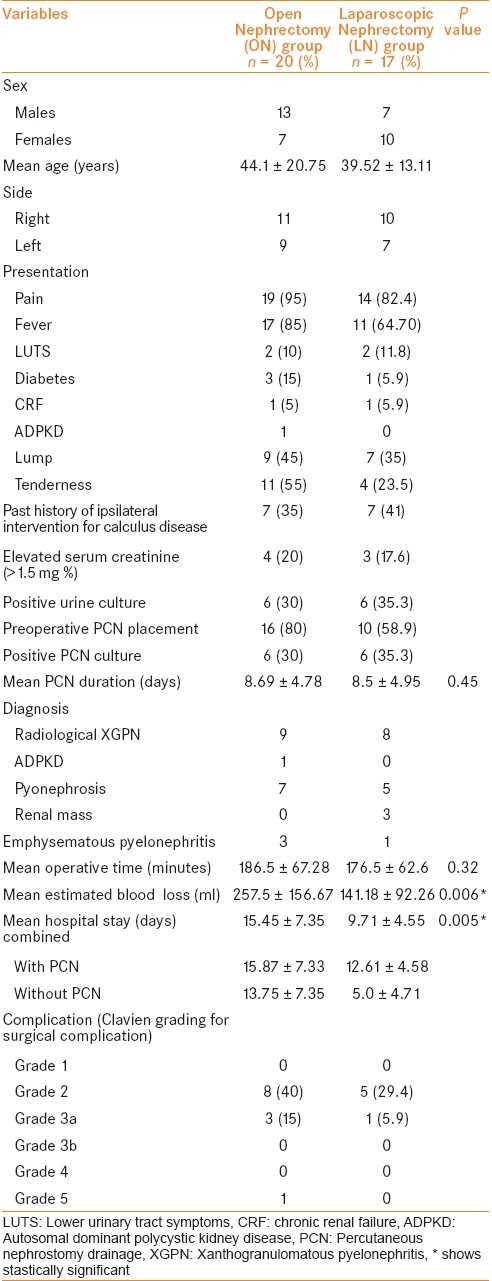
Preoperative percutaneous nephrostomy (PCN) was placed in 26 patients, 16 of ON group and 10 of LN group. Indication for PCN placement was based on clinical examination (pain, fever, and/or tenderness), laboratory results (raised counts, altered renal function, and pyuria) and ultrasonography features (hydronephrosis, internal echoes). Mean duration of PCN placement was 8.69 ± 4.78 days and 8.5 ± 4.95 days in ON and LN groups, respectively.
Of the 37 subjects, 20 were in ON group and 17 were in LN group. Mean operative time was 186.5 ± 67.28 minutes and 176.5 ± 62.6 minutes in ON and LN groups, respectively (P = 0.32). The mean blood loss was 257.5 ± 156.67 ml and 141.18 ± 92.26 ml in ON and LN groups, respectively (P = 0.006). Mean length of stay was 15.45 ± 7.35 days and 9.71 ± 4.55 days in ON and LN groups, respectively (P = 0.005). One patient in LN group, with right-side ectopic pelvic kidney had dense adhesions at hilum and thickened gerota's fascia that precluded further dissection and needed conversion.
The complications following ON and LN [Table 1] were classified according to Clavien-Dindo classification.[5]
In the ON group, eight patients had developed grade 2 complication. It included development of fever postoperatively and requirement of change of antibiotics. Three patients had grade 3 complications, one had rising serum creatinine and fever which was controlled with antibiotics. Another patient had pleura injury which required intercostal drain placement. Third patient had discharge from the wound, which required dressing and secondary suturing. While in the LN group, five patients had developed grade 2 complication. All of them had postoperative fever which was treated with antibiotics. One patient had grade 3 complication; this patient had an infected retrieval site wound which required secondary suturing.
DISCUSSION
XGP is a severe, chronic renal inflammatory condition, generally associated with urinary tract infection and obstructing renal calculi, leading to diffuse or focal kidney destruction.[3] It starts within the pelvis and calyces and subsequently spreads into renal parenchyma; if uncontrolled, it spreads to adjacent tissue and destroys it.[6] Tentative clinical diagnosis can be made based on a combination of renal mass, nonfunctioning kidney on intravenous urography, calculi and urinary tract infection.[7] Most cases of XGP are being treated surgically with nephrectomy. Traditionally, open approach is being used for nephrectomy in XGP.[2,3] Because of inflammatory nature and loss of normal tissue planes, surgery can be extremely challenging.
The role of laparoscopic surgery in patients with XGP has been controversial in earlier laparoscopic series, with higher open conversion and complication rates.[8–10] Reported open conversion rate is 16-33% and complication rate is 20-50% in a contemporary series.[11–15] With increase in advanced laparoscopic experience and skills, LN can be offered in selected patients with acceptable morbidity, decreased blood loss and shorter convalescence.[16]
Our data suggest that the laparoscopic approach in properly selected and prepared patients is associated with reduced hospital stay, blood transfusion rate, shorter convalescence and better cosmesis in comparison with the open approach. Laparoscopic approach requires proper placement of ports for meticulous surgical dissection. Preoperative plain and CECT help in identifying renal hilar anatomy as well as the relationship with the surrounding structures. Placement of PCN in preoperative period helps in identifying the kidney and facilitating hilar dissection by anchoring the kidney at lateral abdominal wall. Eight of the 17 patients in the LN group who had densely adherent upper pole of kidney with diaphragm needed careful dissection with laparoscopic vessel sealing devices like Ligasure (Valleylab, Boulder, CO, USA) and Harmonic scalpel which could facilitate the dissection of dense tissue planes and minimize bleeding. Preoperatively placed PCN and ureteric catheter help in identifying the landmarks of laparoscopic dissection and facilitate subsequent LN. All the patients who had past history of intervention (open surgery or minimally invasive surgery, i.e. Percutaneous Nephrolithotripsy (PCNL), Shockwave lithotripsy (SWL) had dense adhesion surrounding the kidney. Patients with past history of ureterolithotomy had thickened and adherent ureter. In all these patients, placement of ureteric catheter facilitates identification of ureter and helps in identifying the landmarks of laparoscopic dissection. In all these cases, extragerota dissection was preferred. In all our patients, the specimen retrieval bag was used to avoid spillage of the content in the peritoneal cavity as well as for avoiding contamination of wound retrieval site. Preoperative CECT predicts the level of difficulty which might be encountered.
XGP as a disease presents with wide spectrum, ranging from incidentally detected to morbidly ill patients. Laparoscopic approach should be considered, but patient selection is critical. Our data suggest that LN in selected patients of XGP is feasible and should be undertaken only after gaining adequate experience in laparoscopy.
Considerations of following points can provide better outcome during laparoscopic approach:
Placement of PCN in selected patients,
Preoperative CECT in identifying anatomy of renal hilum as well as relationship with the surrounding structures.
Preoperative placement of ureteric catheter in patients with past history of intervention, especially open surgery.
Intraoperative identification of landmarks to maintain adequate tissue plane and to avoid major complications.
Extragerotal dissection.
Adrenal sparing subcapsular upper pole dissection.
Avoid spillage by doubly clipping ureter prior to division.
Retrieving specimen in specimen retrieval bag to avoid spillage and contamination of peritoneal cavity as well as specimen retrieval site.
LIMITATIONS
This was a retrospective study and relatively low number of patients in each group is a limitation of this study. As selection of surgical approach was based on clinical findings also, which may have influenced the results.
To conclude, in XGP, preoperative CECT helps in planning laparoscopic technique and in proper case selection. LN in carefully selected patients with XGP has the benefit of minimally invasive surgery such as reduced intraoperative blood loss, shorter hospital stay and minimal postoperative pain, leading to early and faster convalescence period compared with the open approach.
Key messages
Laparoscopic nephrectomy in patients with Xanthogranulomatous pyelonephritis is often challenging and requires considerable experience. In properly selected patients, laparoscopic approach offers all benefits of minimally invasive surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Petronic V, Buturovic J, Isvaneski M. Xanthogranulomatous Pyelonephritis. Br J Urol. 1989;64:336–8. doi: 10.1111/j.1464-410x.1989.tb06036.x. [DOI] [PubMed] [Google Scholar]
- 2.Rosi P, Selli C, Carini M, Rosi MF, Mottola A. Xanthogranulomatous Pyelonephritis: Clinical experience with 62 cases. Eur Urol. 1986;12:96–100. doi: 10.1159/000472589. [DOI] [PubMed] [Google Scholar]
- 3.Easthan J, Ahlering T, Skinner E. Xanthogranulomatous Pyelonephritis: Clinical findings and surgical considerations. Urology. 1994;43:295–9. doi: 10.1016/0090-4295(94)90069-8. [DOI] [PubMed] [Google Scholar]
- 4.Gill IS. Retroperitoneal laparoscopic nephrectomy. Urol Clin North Am. 1998;25:343–60. doi: 10.1016/s0094-0143(05)70023-9. [DOI] [PubMed] [Google Scholar]
- 5.Clavien PA, Barkun J, de Oliveria ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical Complications: Five year experience. Ann Surg. 2009;250:187–96. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 6.Anthony JS, Edward MS. Infection of the urinary tract. In: Wein, Kavoussi, Novick, Partin, Peters, editors. Campbell-Walsh Urology. 9th ed. Philadelphia: Saunders; 2007. pp. 280–3. [Google Scholar]
- 7.Tolia BM, Iloreta A, Freed SZ, Fruchtman B, Bennett B, Newman HR. Xanthogranulomatous Pyelonephritis: Detailed analysis of 29 cases and brief discussion of atypical presentation. J Urol. 1981;126:437–42. doi: 10.1016/s0022-5347(17)54566-8. [DOI] [PubMed] [Google Scholar]
- 8.Keeley FX, Tolley DA. A review of our first 100 cases of laparoscopic nephrectomy defining risk factors for complications. Br J Urol. 1998;82:615–8. doi: 10.1046/j.1464-410x.1998.00847.x. [DOI] [PubMed] [Google Scholar]
- 9.Rassweiler J, Fornara P, Weber M, Janetschek G, Fahlenkamp D, Henkel T, et al. Laparoscopic nephrectomy the experience of the laparoscopy working group of the German Urologic Association. J Urol. 1998;160:18–21. doi: 10.1016/s0022-5347(01)63015-5. [DOI] [PubMed] [Google Scholar]
- 10.Bercowsky E, Shalhav AL, Portis A, Elbahnasy AM, McDougall EM, Clayman RV, et al. Is the laparoscopic approach justified in patients with Xanthogranulomatous Pyelonephritis? Urology. 1999;54:437–42. doi: 10.1016/s0090-4295(99)00261-7. [DOI] [PubMed] [Google Scholar]
- 11.Kapoor R, Vijjan V, Singh K, Goyal R, Mandhani A, Dubey D, et al. Is laparoscopic nephrectomy the preferred approach in Xanthogranulomatous Pyelonephritis? Urology. 2006;68:952–5. doi: 10.1016/j.urology.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 12.Vanderbrink BA, Ost MC, Rastinehad A, Anderson A, Badlani G, Smith A, et al. Laparoscopic versus open radical nephrectomy for Xanthogranulomatous Pyelonephritis: Contemporary outcomes analysis. J Endourol. 2007;21:65–70. doi: 10.1089/end.2006.0188. [DOI] [PubMed] [Google Scholar]
- 13.Rosoff J, Raman JD, Del Pizzo JJ. Feasibility of laparoscopic approach in management of Xanthogranulomatous Pyelonephritis. Urology. 2006;68:711–4. doi: 10.1016/j.urology.2006.04.031. [DOI] [PubMed] [Google Scholar]
- 14.Manohar T, Desai M, Desai M. Laparoscopic nephrectomy for benign and inflammatory condition. J Endourol. 2007;21:1323–8. doi: 10.1089/end.2007.9883. [DOI] [PubMed] [Google Scholar]
- 15.Khaira HS, Shah RB, Wolf JS. Laparoscopic and open surgical nephrectomy for Xanthogranulomatous Pyelonephritis. J Endourol. 2005;19:813–7. doi: 10.1089/end.2005.19.813. [DOI] [PubMed] [Google Scholar]
- 16.Guzzo TJ, Bivalacqua TJ, Pierorazio PM, Varkarakis J, Schaeffer EM, Allaf ME. Xanthogranulomatous Pyelonephritis: Presentation and management in the era of laparoscopy. BJU international. 2009;104:1265–8. doi: 10.1111/j.1464-410X.2009.08547.x. [DOI] [PubMed] [Google Scholar]


