Abstract
Background
Prior research has found an 80% return-to-work rate in mid-income White breast cancer survivors, but little is known about the employment trajectory of low-income minorities or Whites. We set out to compare the trajectories of low-income Latina and non-Latina White survivors and to identify correlates of employment status.
Methods
Participants were low-income women who had localized breast cancer, spoke English or Spanish, and were employed at the time of diagnosis. Interviews were conducted 6, 18, and 36 months after diagnosis. Multivariate logistic regression was used to identify independent correlates of employment status at 18 months.
Results
Of 290 participants, 62% were Latina. Latinas were less likely than non-Latina Whites to be working 6 months (27% vs. 49%, p=0.0002) and 18 months (45% vs. 59%, p=0.02) after diagnosis, but at 36 months there was no significant difference (53% vs. 59%, p=0.29). Latinas were more likely to be manual laborers than were non-Latina Whites (p<0.0001). Baseline job type and receipt of axillary node dissection were associated with employment status among Latinas but not non-Latina Whites.
Conclusions
Neither low-income Latinas nor non-Latina Whites approached the 80% rate of return to work seen in wealthier White populations. Latinas followed a protracted return-to-work trajectory compared to non-Latina Whites, and differences in job type appear to have played an important role. Manual laborers may be disproportionately impacted by surgical procedures that limit physical activity. This can inform the development of rehabilitative interventions and may have important implications for the surgical and postsurgical management of patients.
Keywords: disparities, employment, breast cancer, survivorship
Introduction
Employment status after breast cancer is related to recovery from treatment, financial security, and quality of life.1,2 Although prior studies have demonstrated a return-to-work rate of approximately 80% in primarily middle- and high-income non-Latina White breast cancer survivors, little is known about the employment trajectories of low-income, ethnically diverse women in the years after diagnosis.3, 4 Research suggests that employment is a major concern for Latina survivors, and African Americans and Latinas may be more vulnerable to work absence and job loss immediately post-treatment than non-Latina Whites.2, 5 Since Latinos are the largest and fastest growing minority group in the United States and comprise approximately 14% of the labor force, any improvement in Latinas’ ability to work has the potential to meaningfully affect the country’s workforce and tax base, as well as patients’ own financial stability and quality of life.6
Ethnic disparities have been demonstrated in cancer stage at diagnosis, treatment, morbidity, mortality, and quality of life.7-10 Latinas have lower age- and stage-specific survival rates and are more likely to be diagnosed at advanced stages compared to non-Latina Whites.9, 10 Ethnic disparities also exist in the labor market with respect to income earned, job type, and unemployment rates.11 Nationwide, only 23% of Latina women are employed in managerial and professional occupations, compared to 40% of non-Latina Whites; 64% are in service occupations (e.g., food service, housekeepers) and in sales and office support.11 Latinos also have lower median household incomes compared to Non-Latino Whites and Asians.12 Low-income women may be less likely to return to work after cancer treatment and more likely to experience financial hardship.2-4 However, ethnic differences in employment outcomes and correlates of employment status among low-income women have not been characterized, and the impact of breast cancer on employment of low-income Latinas remains poorly understood.
To address this gap in knowledge, we undertook a prospective 3-year longitudinal study of low-income, medically underserved Latina and non-Latina White women treated for breast cancer. Our goal was to identify differences in the employment trajectories of these women and understand the factors that might influence this outcome.
Participants and Methods
Eligibility criteria
Eligible participants were English- and/or Spanish-speaking women enrolled in the Breast and Cervical Cancer Treatment Program (BCCTP) administered by California’s Medicaid. Program eligibility requires that a patient be uninsured/underinsured, a California resident, and have a family income ≤200% of the Federal Poverty Level. The program is open to undocumented immigrants. Participants were 6 months post-diagnosis of localized breast cancer, undergoing or had undergone treatment with curative intent, cognitively able to participate, and not undergoing treatment for another cancer. This study was approved by the University of California, Los Angeles Human Subjects Protection Committee. Informed consent was obtained from participants prior to enrollment.
Recruitment and study participants
The current study is part of a larger, longitudinal study described elsewhere.13 Of 1508 eligible women invited to participate, 921 completed a survey 6 months after diagnosis (Figure 1). Compared to those who completed a survey, nonresponders were older (52 vs. 50 years, p<0.05) and less likely to be Latina (46% vs. 56%, p<0.05). Participants lost to follow-up by 36 months were more likely to have undergone mastectomy (54% vs. 42%, p<0.05), have higher cancer stage (p<0.001), and have at least one child living at home (66% vs. 53%, p<0.005).
Figure 1.
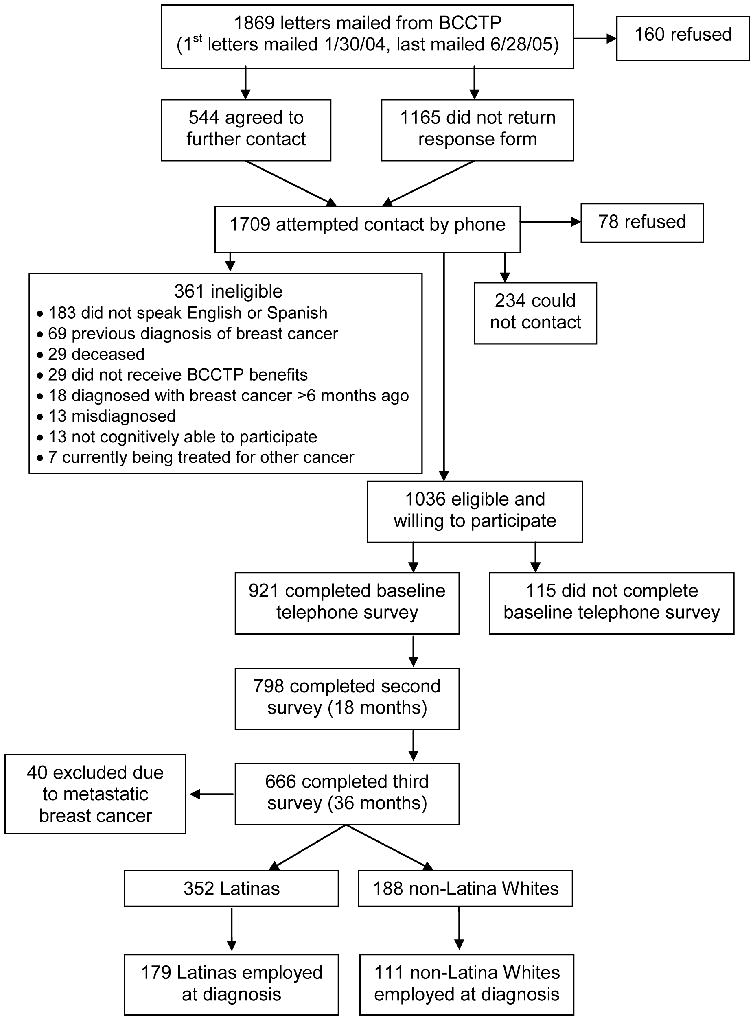
Study recruitment flow
Of 666 women who remained in the study at 36 months, 540 were either Latina or non-Latina White (352 and 188, respectively) and were free of cancer recurrence. Because we were interested in the proportion of women remaining in or returning to the workforce after treatment, this analysis includes only the 179 Latinas and 111 non-Latina Whites who reported working at diagnosis. There was no difference in the baseline employment rate of Latinas and non-Latina Whites (51% and 59%, respectively, p=0.08).
Interviews
One-hour telephone surveys were administered in English or Spanish 6, 18, and 36 months after diagnosis. The study instrument was translated using standard methods.14
Variables
The main outcome in this study was self-reported employment status after 6, 18, and 36 months. We defined the primary outcome as employment that was either part time or full time, but we performed secondary analyses of changes in hours worked. Unless otherwise stated, all independent variables were measured 6 months post-diagnosis.
Education was classified as no high school diploma, completed high school and/or some college, and completed college and/or a post-graduate degree. Family structure was evaluated along 3 parameters: married/partnered versus not married/partnered, children ≤17 years old living at home (0/1/2+), and seniors ≥65 years old living at home (0/1+).
Participants self-identified their ethnic group and place of birth. Acculturation among Latina participants was evaluated using an index based on language use and preference.15
Quality of life was assessed at 18 months using the Medical Outcomes Study 36-Item Short-Form (SF-36) Health Survey.16 Clinical cancer and treatment variables were abstracted from medical records. Comorbid medical conditions were evaluated using the Charlson Comorbidity Index as modified for patient report by Katz et al.17,18 Social support was assessed by asking the participant if she had anyone to provide emotional support, help with daily tasks, and accompany her to medical appointments.19
Job type was classified according to the U.S. Census Bureau Index of Occupations,20 collapsed into 4 categories (operator/fabricator, professional/manager, service, and technical/sales/administrative) based on previously used methods.3, 21-24 Examples of operators/fabricators include farm and factory workers; professionals/managers include teachers and financial workers; service jobs include housekeepers, food servers, and nannies; and technical/sales/administrative jobs include clerks, administrative assistants, and skilled technical workers such as information technology personnel.
Analysis
Initial analyses compared survey and clinical variables by ethnicity, using t-tests for continuous variables and chi-square (or Fisher’s exact) tests for categorical variables. To identify correlates of employment status within each ethnic group, a second set of analyses compared the same variables by employment status at 18 months, stratified by ethnicity. We focused on correlates at 18 months because it is well after the time at which all treatment (except endocrine therapy) should have been completed. Because quality of life in cancer survivors is known to improve with time after treatment, we analyzed quality of life at 18 months as both a correlate of employment status at 18 months and as a predictor of employment status at 36 months.25 A multivariate logistic regression including variables that were statistically significant in the univariate analysis (i.e., two-sided alpha levels with p-values <0.05) was then conducted to identify independent predictors of employment status at 18 months. In an exploratory analysis, we analyzed trends in job-type shifts between baseline and 36 months descriptively only, due to the exploratory nature of this analysis and small numbers in each subgroup.
Fifteen participants completed 6- and 36-month surveys but did not complete an 18-month survey. The employment rates calculated for the 6- and 36-month surveys were not sensitive to the inclusion or exclusion of these participants.
Results
Table 1 lists the baseline characteristics of the participants by ethnic group. Latinas were younger, more likely to be married/partnered, and more likely to have children living at home, whereas non-Latina Whites were significantly more educated than Latinas and had greater diversity in job type. More than half (56%) of Latinas were employed in service jobs, and 24% were employed as operators/fabricators. Treatment differences included more reconstructive surgery among non-Latina Whites, and a higher likelihood of radiotherapy among Latinas.
Table 1.
Participant Characteristics
| Non-Latina Whites (n=111) No. (%) | Latinas (n=179) No. (%) | P Value | |
|---|---|---|---|
|
DEMOGRAPHICS
| |||
| AGE | |||
| Median | 53 | 49 | <0.05 |
| Range | 32-65 | 26-85 | |
| US-BORN | |||
| Yes | 100 (90) | 21 (12) | |
| No | 11 (10) | 156 (88) | < 0.0001 |
| ACCULTURATION SCORE ≥15 | |||
| Yes | N/A | 15 (9) | |
| No | N/A | 156 (91) | |
| EDUCATION | |||
| Did not complete high school | 13 (12) | 103 (58) | |
| High school diploma +/- some college | 63 (57) | 64 (36) | < 0.0001 |
| College degree +/- post-graduate | 35 (31) | 11 (6) | |
|
| |||
|
WORK RELATED (BEFORE DIAGNOSIS)
| |||
| JOB TYPE | |||
| Operator/fabricator | 5 (5) | 43 (24) | |
| Professional/manager | 37 (33) | 6 (3) | |
| Service | 36 (32) | 101 (56) | < 0.0001 |
| Technical/Sales/Admin. | 33 (30) | 29 (16) | |
| MEAN WEEKLY WORK HOURS | 38 | 39 | 0.50 |
|
| |||
|
FAMILY STRUCTURE AND SOCIAL SUPPORT
| |||
| MARITAL STATUS | |||
| Partnered/Married | 34 (31) | 96 (54) | |
| No partner | 77 (69) | 83 (46) | 0.0001 |
| PEOPLE ≤ 17 IN HOUSE | |||
| 0 | 57 (72) | 55 (36) | |
| 1 | 11 (14) | 36 (23) | < 0.0001 |
| 2 or more | 11 (14) | 63 (41) | |
| PEOPLE ≥ 65 IN HOUSE | |||
| 0 | 68 (83) | 127 (82) | |
| 1 or more | 14 (17) | 27 (18) | 0.93 |
| SOCIAL SUPPORT FOR MEDICAL VISITS | |||
| Yes | 96 (86) | 150 (84) | |
| No | 15 (14) | 28 (16) | 0.61 |
| SOCIAL SUPPORT FOR DAILY TASKS | |||
| Yes | 23 (21) | 34 (19) | |
| No | 87 (79) | 145 (81) | 0.69 |
| EMOTIONAL SUPPORT | |||
| Yes | 100 (90) | 150 (84) | |
| No | 11 (10) | 28 (16) | 0.16 |
|
| |||
|
CLINICAL VARIABLES
| |||
| CANCER STAGE | |||
| DCIS | 7 (7) | 17 (11) | |
| I | 38 (39) | 39 (25) | 0.07 |
| II | 34 (35) | 73 (47) | |
| III | 18 (19) | 25 (16) | |
| MASTECTOMY | |||
| Yes | 42 (41) | 61 (38) | |
| No | 61 (59) | 101 (62) | 0.61 |
| RECONSTRUCTION (IF MASTECTOMY) | |||
| Yes | 11 (26) | 5 (8) | |
| No | 31 (74) | 56 (92) | 0.01 |
| AXILLARY NODE DISSECTION | |||
| Yes | 71 (68) | 105 (65) | |
| No | 33 (32) | 57 (35) | 0.56 |
| CHEMOTHERAPY | |||
| Yes | 67 (64) | 119 (73) | |
| No | 37 (36) | 43 (27) | 0.12 |
| RADIATION THERAPY | |||
| Yes | 68 (66) | 128 (81) | |
| No | 35 (34) | 31 (19) | <0.01 |
| ENDOCRINE THERAPY | |||
| Yes | 73 (71) | 105 (68) | |
| No | 30 (29) | 50 (32) | 0.59 |
| COMORBIDITIES | |||
| 0 | 79 (71) | 131 (73) | |
| 1-2 | 25 (23) | 37 (21) | 0.93 |
| ≥3 | 7 (6) | 11 (6) | |
|
| |||
|
QUALITY OF LIFE
| |||
| SF 36 | Mean (SD) | Mean (SD) | |
| Physical functioning | 78 (23) | 76 (23) | 0.52 |
| Emotional well-being | 66 (24) | 63 (24) | 0.27 |
| Role function, physical | 54 (41) | 50 (43) | 0.45 |
| Role function, emotional | 69 (41) | 74 (39) | 0.39 |
| Social functioning | 72 (30) | 71 (25) | 0.92 |
| Pain | 66 (28) | 69 (25) | 0.41 |
| Energy/fatigue | 51 (26) | 54 (24) | 0.38 |
| General health perceptions | 69 (24) | 67 (21) | 0.42 |
| Physical component summary | 46 (11) | 45 (10) | 0.71 |
| Mental component summary | 46 (13) | 46 (13) | 0.91 |
Abbreviations: DCIS, ductal carcinoma in situ; SF 36, Medical Outcomes Study 36-Item Short-Form Health Survey; SD, standard deviation
Employed low-income non-Latina Whites and Latinas followed different employment trajectories after a breast cancer diagnosis, with Latinas taking a longer time to return to work than non-Latina Whites (Figure 2). Fewer Latinas were working 6 and 18 months post-diagnosis, but by 36 months this difference was no longer statistically significant. However, overall less than 60% of participants from both ethnic groups had returned to work 3 years post-diagnosis.
Figure 2.
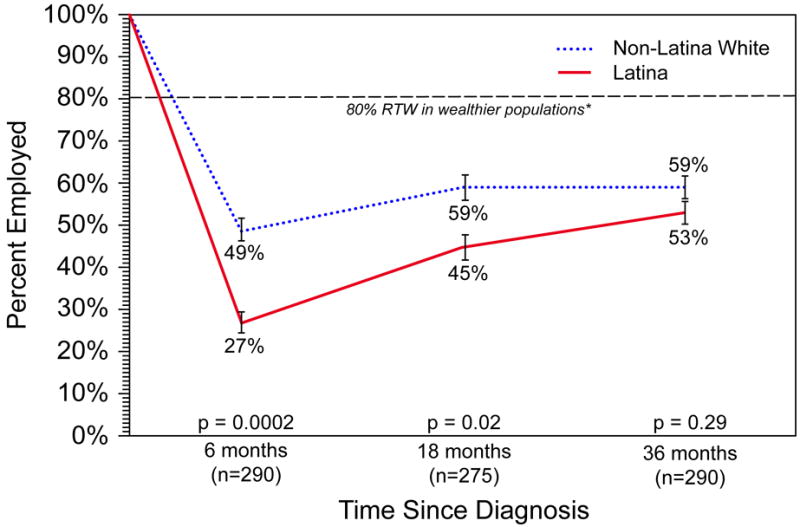
Employment trajectories of low-income Latina and non-Latina White breast cancer survivors who were employed prior to diagnosis
*The dashed line corresponds to the 80% rate of return to work (RTW) by 12 months seen in wealthier, primarily non-Latina White populations.
There were no significant differences in mean weekly work hours among employed participants at any survey time-point. Non-Latina Whites and Latinas worked, respectively, 30 versus 31 hours at 6 months, 29 hours at 18 months, and 33 versus 31 hours at 36 months.
Results of an 18-month univariate analysis are shown in Table 2. Quality of life was positively associated with employment status in both ethnic groups (with the exception of the pain scale among Latinas). Treatment with chemotherapy and higher comorbidity burden both were inversely associated with being employed 18 months after diagnosis among non-Latina Whites but not among Latinas. Conversely, axillary lymph node dissection (ALND), which is known to be associated with impaired upper body mobility, was inversely associated with employment status among Latinas but not among non-Latina Whites.26, 27 Additional factors associated with employment status among Latinas included education and baseline job type, which was associated with employment status at all survey time-points among Latinas but not non-Latina Whites. Latinas employed as operators or fabricators were least likely to be working at each time-point compared to Latinas working in other jobs (Table 3).
Table 2.
Univariate analysis of characteristics associated with employment status at 18 months
| Non-Latina Whites (n=106)* | Latinas (n=169)* | |||||
|---|---|---|---|---|---|---|
| Not Working No. (%) | Working No. (%) | P Value | Not Working No. (%) | Working No. (%) | P Value | |
|
DEMOGRAPHICS
| ||||||
| AGE | ||||||
| Median | 53 | 53 | 49 | 48 | ||
| Range | 34-65 | 33-65 | 0.54 | 31-85 | 26-74 | 0.23 |
| US-BORN | ||||||
| Yes | 39 (41) | 56 (59) | 7 (39) | 11 (61) | ||
| No | 4 (36) | 7 (64) | 1.00 | 85 (57) | 65 (43) | 0.15 |
| ACCULTURATION SCORE ≥15 | ||||||
| Yes | 6 (46) | 7 (54) | ||||
| No | 84 (56) | 66 (44) | 0.49 | |||
| EDUCATION | ||||||
| Did not complete high school | 7 (54) | 6 (46) | 65 (65) | 35 (35) | ||
| High school diploma +/- some college | 23 (38) | 37 (62) | 0.58 | 23 (40) | 35 (60) | 0.005 |
| College degree +/- post-graduate | 13 (39) | 20 (61) | 4 (40) | 6 (60) | ||
|
| ||||||
|
WORK RELATED (BEFORE DIAGNOSIS)
| ||||||
| JOB TYPE | ||||||
| Operator/Fabricator | 2 (40) | 3 (60) | 24 (73) | 11 (27) | ||
| Professional/Manager | 14 (39) | 22 (61) | 3 (50) | 3 (50) | ||
| Service | 14 (40) | 21 (60) | 0.99 | 54 (55) | 45 (45) | 0.01 |
| Technical/Sales/Admin. | 13 (43) | 17 (57) | 7 (32) | 17 (68) | ||
| MEAN WEEKLY WORK HOURS | 38 | 38 | 0.96 | 39 | 38 | 0.63 |
|
| ||||||
|
FAMILY STRUCTURE AND SOCIAL SUPPORT
| ||||||
| MARITAL STATUS | ||||||
| Partner/Married | 10 (29) | 24 (71) | 56 (59) | 39 (41) | ||
| No partner | 33 (46) | 39 (54) | 0.11 | 37 (50) | 37 (50) | 0.25 |
| PEOPLE ≤ 17 IN HOUSE | ||||||
| 0 | 22 (41) | 32 (59) | 30 (56) | 24 (44) | ||
| 1 | 4 (36) | 7 (64) | 0.81 | 17 (50) | 17 (50) | 0.70 |
| 2 or more | 5 (50) | 5 (50) | 36 (59) | 25 (41) | ||
| PEOPLE ≥ 65 IN HOUSE | ||||||
| 0 | 26 (41) | 38 (59) | 73 (59) | 51 (41) | ||
| 1 or more | 7 (50) | 7 (50) | 0.52 | 10 (40) | 14 (60) | 0.08 |
| SOCIAL SUPPORT FOR MEDICAL VISITS | ||||||
| Yes | 38 (41) | 54 (59) | 77 (55) | 64 (45) | ||
| No | 5 (36) | 9 (64) | 0.69 | 15 (56) | 12 (44) | 0.93 |
| SOCIAL SUPPORT FOR DAILY TASKS | ||||||
| Yes | 36 (42) | 50 (58) | 78 (56) | 61 (44) | ||
| No | 6 (32) | 13 (68) | 0.41 | 15 (50) | 15 (50) | 0.54 |
| EMOTIONAL SUPPORT | ||||||
| Yes | 37 (39) | 59 (61) | 77 (54) | 65 (46) | ||
| No | 6 (60) | 4 (40) | 0.31 | 15 (58) | 11 (42) | 0.74 |
|
| ||||||
|
CLINICAL VARIABLES
| ||||||
| CANCER STAGE | ||||||
| DCIS | 3 (43) | 4 (57) | 8 (47) | 9 (53) | ||
| I | 12 (32) | 25 (68) | 0.54 | 16 (48) | 17 (52) | 0.06 |
| II | 15 (47) | 17 (53) | 33 (52) | 30 (48) | ||
| III | 9 (50) | 9 (50) | 18 (82) | 4 (18) | ||
| MASTECTOMY | ||||||
| Yes | 17 (40) | 25 (60) | 36 (60) | 24 (40) | ||
| No | 24 (41) | 34 (59) | 0.93 | 51 (52) | 47 (48) | 0.33 |
| RECONSTRUCTION (IF MASTECTOMY) | ||||||
| Yes | 4 (36) | 7 (64) | 3 (60) | 2 (40) | ||
| No | 13 (42) | 18 (58) | 0.75 | 33 (60) | 22 (40) | 1.00 |
| AXILLARY NODE DISSECTION | ||||||
| Yes | 31 (45) | 38 (55) | 66 (64) | 37 (34) | ||
| No | 10 (31) | 22 (69) | 0.19 | 21 (38) | 34 (62) | <0.005 |
| CHEMOTHERAPY | ||||||
| Yes | 32 (48) | 34 (52) | 67 (58) | 48 (42) | ||
| No | 9 (26) | 26 (74) | <0.05 | 20 (47) | 23 (53) | 0.19 |
| RADIATION THERAPY, No. (%) | ||||||
| Yes | 31 (46) | 36 (54) | 67 (54) | 58 (46) | ||
| No | 10 (29) | 24 (71) | 0.10 | 17 (57) | 13 (43) | 0.76 |
| ENDOCRINE THERAPY | ||||||
| Yes | 30 (42) | 41 (58) | 54 (53) | 48 (47) | ||
| No | 10 (34) | 19 (66) | 0.47 | 27 (55) | 22 (45) | 0.80 |
| COMORBIDITIES | ||||||
| 0 | 27 (36) | 48 (64) | 67 (54) | 57 (46) | ||
| 1-2 | 10 (40) | 15 (60) | 0.01 | 18 (53) | 16 (47) | 0.47 |
| ≥3 | 6 (100) | 0 | 8 (73) | 3 (27) | ||
|
| ||||||
|
QUALITY OF LIFE
| ||||||
| SF 36 | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
| Physical functioning | 71 (29) | 82 (16) | <0.05 | 72 (25) | 80 (20) | <0.05 |
| Emotional well-being | 56 (25) | 73 (21) | <0.0005 | 56 (25) | 71 (20) | <0.0001 |
| Role function, physical | 33 (40) | 67 (36) | <0.0001 | 37 (43) | 66 (38) | <0.0001 |
| Role function, emotional | 48 (44) | 84 (32) | <0.0001 | 62 (44) | 88 (28) | <0.0001 |
| Social functioning | 56 (32) | 82 (22) | <0.0001 | 67 (27) | 77 (22) | 0.01 |
| Pain | 58 (30) | 71 (25) | <0.05 | 66 (26) | 72 (24) | 0.14 |
| Energy/fatigue | 42 (26) | 57 (24) | <0.005 | 49 (24) | 60 (23) | <0.005 |
| General health perceptions | 60 (26) | 74 (20) | <0.005 | 62 (22) | 73 (18) | <0.0005 |
| Physical component summary | 43 (12) | 47 (9) | <0.05 | 44 (10) | 47 (9) | <0.05 |
| Mental component summary | 39 (14) | 50 (11) | <0.0001 | 42 (13) | 50 (10) | <0.0001 |
Abbreviations: DCIS, ductal carcinoma in situ; SF 36, Medical Outcomes Study 36-Item Short-Form Health Survey; SD, standard deviation
Fifteen participants did not complete an 18-month survey.
Table 3.
Employment status by baseline job type at each survey time point
| EMPLOYMENT STATUS AT 6 MONTHS | EMPLOYMENT STATUS AT 18 MONTHS | EMPLOYMENT STATUS AT 36 MONTHS | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-Latina Whites (n=111) | Latinas (n=179) | Non-Latina Whites (n=106) | Latinas (n=169) | Non-Latina Whites (n=111) | Latinas (n=179) | |||||||||||||
| Not Working |
Working | P Value | Not Working |
Working | P Value | Not Working |
Working | P Value | Not Working |
Working | P Value | Not Working |
Working | P Value | Not Working |
Working | P Value | |
| JOB TYPE AT BASELINE, No. (%) | ||||||||||||||||||
| Operator/Fabricator | 3 (60) | 2 (40) | 37 (86) | 6(14) | 2 (40) | 3 (60) | 29 (72) | 11 (28) | 1 (20) | 4 (80) | 28 (65) | 15 (35) | ||||||
| Professional/Manager | 18(49) | 19 (51) | 3 (50) | 3 (50) | 14 (39) | 22 (61) | 3 (50) | 3 (50) | 15 (41) | 22 (59) | 3 (50) | 3 (50) | ||||||
| Service | 18 (50) | 18 (50) | 75 (74) | 26 (26) | 14 (40) | 21 (60) | 54 (55) | 45 (45) | 14 (39) | 22 (61) | 47 (47) | 54 (53) | ||||||
| Tech/Sales/Admin | 18 (55) | 15 (45) | 0.94 | 16 (55) | 13 (45) | <0.05 | 13 (43) | 17 (57) | 0.99 | 7 (29) | 17 (71) | <0.05 | 15 (45) | 18 (55) | 0.74 | 6 (21) | 23 (79) | <0.005 |
In a multivariate analysis stratified by ethnicity, only the SF-36 Mental Component Summary score was significantly associated with employment status at 18 months for non-Latina Whites (Table 4). Among Latinas, however, job type (operator/fabricator), ALND, and both the Physical and Mental Component Summary scores were significant correlates.
Table 4.
Multivariate analysis of characteristics associated with being employed 18 months after diagnosis
| Non-Latina Whites (n=101)* | Latinas (n=157)* | |
|---|---|---|
| Odds Ratio (95% CI) | Odds Ratio (95% CI) | |
| JOB TYPE | ||
| Operator/Fabricator | 0.25 (0.03-2.31) | 0.19 (0.05-0.75) |
| Professional/Manager | 1.46 (0.45-4.81) | 0.33 (0.04-3.02) |
| Service | 1.11 (0.34-3.64) | 0.45 (0.14-1.45) |
| Technical/Sales/Administrative** | 1.00 | 1.00 |
|
| ||
| EDUCATION | ||
| Did not complete high school | 0.53 (0.12-2.27) | 0.47 (0.22-1.02) |
| High school diploma (or higher) ** | 1.00 | 1.00 |
|
| ||
| CHEMOTHERAPY | ||
| Yes | 0.67 (0.22-2.02) | 0.87 (0.35-2.16) |
| No** | 1.00 | 1.00 |
|
| ||
| AXILLARY NODE DISSECTION | ||
| Yes | 0.67 (0.23-1.90) | 0.35 (0.15-0.82) |
| No** | 1.00 | 1.00 |
|
| ||
| COMORBIDITIES | ||
| 0 | 1.54 (0.51-4.67) | 0.60 (0.24-1.47) |
| 1 or more** | 1.00 | 1.00 |
|
| ||
| QUALITY OF LIFE | ||
| SF 36 Physical component summary | 1.015 (0.96-1.07) | 1.05 (1.009-1.10) |
| SF 36 Mental component summary | 1.07 (1.03-1.12) | 1.07 (1.03-1.10) |
Number of participants included in multivariate analysis limited by missing data.
Reference category (odds ratio = 1.00)
Abbreviations: CI, confidence interval; N/A, not applicable; SF 36, Medical Outcomes Study 36-Item Short-Form Health Survey
Quality of life was positively correlated with employment status 18 months post-diagnosis and also predicted employment status 36 months post-diagnosis. Both the Physical and Mental Component Summary scores at 18 months were correlated with employment status at 36 months in both ethnic groups. (Data not shown.)
Results of an exploratory analysis of trends in job-type shifts are reported in Table 5. Every Latina who worked in a service job at baseline was either unemployed or working in a service job 36 months after diagnosis. Latinas who worked as operators/fabricators at baseline were either unemployed, working as operators/fabricators, or working in service jobs 36 months later. Conversely, non-Latina Whites working as operators/fabricators or in service jobs appeared to have somewhat more job-type flexibility than their Latina counterparts.
Table 5.
Job type at 36 months by job type at baseline (exploratory analysis)
| Non-Latina Whites (n=111) | |||||
|---|---|---|---|---|---|
| JOB TYPE AT 36 MONTHS
| |||||
| Not working | Operator/Fabricator | Professional/Manager | Service | Tech/Sales/Admin | |
| No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | |
| JOB TYPE AT BASELINE | |||||
|
| |||||
| Operator/Fabricator; n=5 | 1 (20) | 1 (20) | 1 (20) | 0 | 2 (40) |
| Professional/Manager; n=37 | 15 (41) | 0 | 20 (54) | 1 (3) | 1 (3) |
| Service; n=36 | 14 (39) | 1 (3) | 2 (6) | 18 (50) | 1 (3) |
| Tech/Sales/Admin; n=33 | 16 (49) | 0 | 5 (15) | 0 | 12 (36) |
|
| |||||
| Latinas (n=179) | |||||
|
JOB TYPE AT 36 MONTHS
| |||||
| Not working | Operator/Fabricator | Professional/Manager | Service | Tech/Sales/Admin | |
|
| |||||
| No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | |
| JOB TYPE AT BASELINE | |||||
|
| |||||
| Operator/Fabricator (n=43) | 27 (63) | 13 (30) | 0 | 3 (7) | 0 |
| Professional/Manager (n=6) | 3 (50) | 1 (17) | 1 (17) | 1 (17) | 0 |
| Service (n=101) | 47 (47) | 0 | 0 | 54 (53) | 0 |
| Tech/Sales/Admin (n=29) | 6 (21) | 0 | 5 (17) | 1 (3) | 17 (59) |
Discussion
In this study, low-income, medically underserved Latina and non-Latina White women who were employed prior to a breast cancer diagnosis followed different employment trajectories over the 3 years following their diagnosis. At 6 and 18 months, fewer Latinas than non-Latina Whites were working, but 36 months after diagnosis there was no significant difference in employment rate. Job type was associated with employment status throughout the study among Latina but not non-Latina White participants, and significant differences in job-type distribution were noted between the groups. This suggests that job type is an important driver of the disparity in return to work. For example, fewer than 5% of non-Latina Whites worked as operators/fabricators, whereas 24% of Latinas had such jobs at the time of diagnosis, and participants in this job category consistently had the lowest employment rate. Interestingly, family structure and social support factors that might facilitate or hinder return to work, such as number of children at home or help with daily tasks, made no difference in employment after diagnosis for either ethnic group.
Prior research has demonstrated that breast cancer survivors whose jobs involve heavy lifting and those with upper-body strength limitations are less likely to return to work within a year of diagnosis.3, 23, 28 These findings are consistent with our own with respect to both job type and ALND among Latinas. Although similar proportions of Latina and non-Latina White participants underwent ALND, the procedure was associated with employment status only among Latinas in our sample. Manual laborers may be disproportionately impacted by surgical procedures, such as ALND, which are known to limit mobility and physical activity.26, 27 Since the association between ALND and employment status persisted when controlling for job type, additional factors may also be important, such as differences in knowledge about lymphedema or in utilization of lymphedema therapy. These results have implications for the postsurgical management of patients and can inform the development of job retraining and rehabilitative interventions. Our results are also relevant in the context of surgical decision-making. The American College of Surgeons Oncology Group (ACOSOG) recently reported the results of the Z0011 trial, which demonstrated a lack of survival benefit associated with ALND in women with clinically node-negative breast cancer (preoperatively) and two or fewer involved lymph nodes on sentinel lymph node biopsy.29 The findings of that study call into question the tenet that ALND improves overall survival in all patients with axillary lymph node metastases and, if accepted into practice, could have an impact on employment outcomes among low-income women in particular. Certainly, given our findings, there is a need for a more complex assessment of the risk/benefit trade-off associated with ALND in low-income patients with clinically node-negative disease.
Our study findings indicate that existing labor-market disparities may be exacerbated by a breast cancer diagnosis.11, 30 The association between job type and employment status is not surprising, as physical activity at work, schedule flexibility, and employer accommodation are known correlates of employment status.3, 23, 31 Low-income Latinas may have less job-type flexibility than their non-Latina White counterparts, as suggested by the results of our exploratory analysis of job-type shifts. Research by the Pew Hispanic Center has shown that job-type disparities between Latinas and non-Latina Whites are most pronounced in Latinas who, like the majority of those in our study sample, are foreign-born and have relatively low levels of education.32 Job reorientation may be an important intervention to promote return to work in this group of women.
Less than 60% of participants in our study returned to work, in contrast to prior studies, in which approximately 80% of middle- and high-income breast cancer survivors were working by 1-3 years after diagnosis.3, 4 In these other studies, higher income was associated with increased return to work.3, 4 Based on these data and on our results, it appears that low-income women, regardless of ethnic background, may take longer to return to work and do so at a lower rate than middle- and high-income women. In a uniformly low-income sample it is reasonable to suppose that few participants would have significant sources of unearned income, making them directly dependent on income earned (and employment) for financial security. Low-income women, therefore, may be both more vulnerable to delayed return to work and more likely to bear a greater financial burden as a result of a breast cancer diagnosis.
Income-related disparities in quality of life may help explain the difference in employment outcomes between our low-income sample and previously published findings in higher-income survivors. Prior research has demonstrated that quality of life and employment status have a complex, bidirectional relationship. Higher quality of life is correlated with the ability to work, and working improves psychosocial quality of life.1 Moreover, higher income is associated with improved quality of life among cancer survivors, and this is not entirely due to the effect of health on earnings.33 A limitation of our study is that we did not assess quality of life at baseline and were, therefore, unable to evaluate quality of life as a predictor of employment status at 18 months. We were, however, able to assess quality of life as both a correlate of employment status at 18 months and a predictor of employment status at 36 months. Despite the difference in the employment rate of the two groups at 18 months, we found no significant differences in quality of life, which was associated with employment status at 18 months and predicted employment status at 36 months in both ethnic groups. It is possible, therefore, that the lower rate of return to work demonstrated in our low-income sample (compared to higher-income samples in other studies) is due to income-related disparities in quality of life.
Our results indicate that low-income Latina and non-Latina White breast cancer survivors may differ in the factors influencing their return to work. Our findings do not tell us, however, whether each factor exerts a unique effect on employment status depending on ethnic group membership. This would require a larger sample size to test for an interaction between ethnicity and each correlate. Instead, our findings lay the groundwork for additional investigation aimed at understanding how each factor influences employment.
Our study may underestimate the impact of breast cancer on employment status as participants who were lost to follow-up were more likely to have presented with more advanced disease, to have undergone a mastectomy rather than a lumpectomy, and to have at least one child at home. All three variables could reasonably be considered theoretical risk factors for impaired return to work, but none was found to be associated with employment status at 18 months.
This study is one of few that examine employment after a cancer diagnosis in Latinos, the largest and fastest growing ethnic minority group in the United States.2, 34 To our knowledge, it is the first study to examine employment trajectories in Latinos with cancer. The strengths of this study include the high response and retention rates, which were similar to those reported in prior studies of wealthier and more educated populations, as well as the homogeneity of our study sample with respect to income and health insurance.3, 4, 23 By holding income and insurance constant, we were able to isolate ethnic differences which may otherwise be confounded. However, homogeneity in health insurance limits the generalizability of our findings to survivors with employment-contingent insurance.
To date, most studies of employment after breast cancer have focused on middle- and high-income non-Latina White populations; with few exceptions, data are lacking with respect to potential ethnic and socioeconomic differences in employment after breast cancer. Our study contributes to our understanding of these differences, by demonstrating a disparity in return to work between Latina and non-Latina White survivors and suggesting a disparity between our low-income sample and higher-income samples studied previously. Future research should focus on understanding the specific conditions that hinder return to work in low-income women and on developing ethnically-sensitive interventions to facilitate return to work.
Acknowledgments
The authors gratefully acknowledge Heather Gold, Ph.D., for assistance with manuscript preparation.
Funding sources: American Cancer Society (# TURSG-02-081); California Breast Cancer Research Program (# 7PB-0070); National Cancer Institute (# 1R01CA119197-01A1); American Society of Clinical Oncology (Young Investigator Award to VB); Anne Moore Breast Cancer Research Fund.
Footnotes
Disclosures: There are no financial disclosures from any manuscript authors.
References
- 1.Engel J, Kerr J, Schlesinger-Raab A, Eckel R, Sauer H, Holzel D. Predictors of quality of life of breast cancer patients. Acta Oncologica. 2003;42(7):710–8. doi: 10.1080/02841860310017658. [DOI] [PubMed] [Google Scholar]
- 2.Mujahid MS, Janz NK, Hawley ST, et al. Racial/ethnic differences in job loss for women with breast cancer. J Cancer Surviv. 2011;5(1):102–11. doi: 10.1007/s11764-010-0152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bouknight RR, Bradley CJ, Luo Z. Correlates of return to work for breast cancer survivors. Journal of Clinical Oncology. 2006;24(3):345–53. doi: 10.1200/JCO.2004.00.4929. [DOI] [PubMed] [Google Scholar]
- 4.Drolet M, Maunsell E, Brisson J, Brisson C, Masse B, Deschenes L. Not working 3 years after breast cancer: Predictors in a population-based study. Journal of Clinical Oncology. 2005;23(33):8305–12. doi: 10.1200/JCO.2005.09.500. [DOI] [PubMed] [Google Scholar]
- 5.Ashing-Giwa KT, Padilla G, Tejero J, et al. Understanding the breast cancer experience of women: a qualitative study of African American, Asian American, Latina and Caucasian cancer survivors. Psycho-Oncology. 2004;13(6):408–28. doi: 10.1002/pon.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.United States Department of Labor, Bureau of Labor Statistics. Employment by detailed occupation, sex, race, and Hispanic ethnicity, 2008 annual averages. [April 19, 2009]; Available from URL: http://www.bls.gov/cps/cps_aa2008.htm.
- 7.Albain KS, Unger JM, Crowley JJ, Coltman CA, Hershman DL. Racial Disparities in Cancer Survival Among Randomized Clinical Trials Patients of the Southwest Oncology Group. Journal of the National Cancer Institute. 2009;101(14):984–92. doi: 10.1093/jnci/djp175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Janz NK, Mujahid MS, Hawley ST, et al. Racial/ethnic differences in quality of life after diagnosis of breast cancer. J Cancer Surviv. 2009;3(4):212–22. doi: 10.1007/s11764-009-0097-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jemal A, Clegg LX, Ward E, et al. Annual report to the nation on the status of cancer, 1975-2001, with a special feature regarding survival. Cancer. 2004;101(1):3–27. doi: 10.1002/cncr.20288. [DOI] [PubMed] [Google Scholar]
- 10.Miller BA, Hankey BF, Thomas TL. Impact of sociodemographic factors, hormone receptor status, and tumor grade on ethnic differences in tumor stage and size for breast cancer in US women. American Journal of Epidemiology. 2002;155(6):534–45. doi: 10.1093/aje/155.6.534. [DOI] [PubMed] [Google Scholar]
- 11.Gabor M. Labor Force Characteristics by Race and Ethnicity: U.S. Department of Labor. 2007 [Google Scholar]
- 12.DeNavas-Walt C, Proctor B, Smith J U.S. Census Bureau, Current Population Reports. Income, Poverty, and Health Insurance Coverage in the United States: 2008. Washington, D.C.: U.S. Government Printing Office; 2009. pp. 60–236. [Google Scholar]
- 13.Chen J, Diamant A, Thind A, Maly R. Determinants of breast cancer knowledge among newly diagnosed, low-income, medically underserved women with breast cancer. Cancer. 2008;112(5):1153–61. doi: 10.1002/cncr.23262. [DOI] [PubMed] [Google Scholar]
- 14.Eremenco SL, Cella D, Arnold BJ. A comprehensive method for the translation and cross-cultural validation of health status questionnaires. Evaluation & the Health Professions. 2005;28(2):212–32. doi: 10.1177/0163278705275342. [DOI] [PubMed] [Google Scholar]
- 15.Marin G, Sabogal F, Marin B, Otero-Sabogal R, Perez-Stable E. Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Sciences. 1987;9(2):183–205. [Google Scholar]
- 16.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care. 1992;30(6):473–83. [PubMed] [Google Scholar]
- 17.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 18.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Medical Care. 1996;34(1):73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Seeman TE, Berkman LF. Structural characteristics of social networks and their relationship with social support in the elderly: who provides support. Social Science and Medicine. 1988;26(7):737–49. doi: 10.1016/0277-9536(88)90065-2. [DOI] [PubMed] [Google Scholar]
- 20.United States Census Bureau Index of Occupations. [April 17, 2009]; Available from URL: http://www.census.gov/hhes/www/ioindex/ioindex02/occ02_a.html.
- 21.Health and Retirement Study. [April 17, 2009];AHEAD Core, Final, Version 2.0, May 2002, Revised August 2007, Master Codes. 1995 Available from URL: http://hrsonline.isr.umich.edu/modules/meta/1995/core/codebook/a95_mastercode.htm.
- 22.Chirikos TN, Russell-Jacobs A, Cantor AB. Indirect economic effects of long-term breast cancer survival. Cancer Practice. 2002;10(5):248–55. doi: 10.1046/j.1523-5394.2002.105004.x. [DOI] [PubMed] [Google Scholar]
- 23.Satariano WA, DeLorenze GN. The likelihood of returning to work after breast cancer. Public Health Reports. 1996;111(3):236–41. [PMC free article] [PubMed] [Google Scholar]
- 24.Ashing-Giwa KT, Tejero JS, Kim J, Padilla GV, Hellemann G. Examining predictive models of HRQOL in a population-based, multiethnic sample of women with breast carcinoma. Quality of Life Research. 2007;16(3):413–28. doi: 10.1007/s11136-006-9138-4. [DOI] [PubMed] [Google Scholar]
- 25.Ganz PA, Desmond KA, Leedham B, Rowland JH, Meyerowitz BE, Belin TR. Quality of life in long-term, disease-free survivors of breast cancer: a follow-up study. Journal of the National Cancer Institute. 2002;94(1):39–49. doi: 10.1093/jnci/94.1.39. [DOI] [PubMed] [Google Scholar]
- 26.Burak WE, Hollenbeck ST, Zervos EE, Hock KL, Kemp LC, Young DC. Sentinel lymph node biopsy results in less postoperative morbidity compared with axillary lymph node dissection for breast cancer. American Journal of Surgery. 2002;183(1):23–7. doi: 10.1016/s0002-9610(01)00848-0. see comment. [DOI] [PubMed] [Google Scholar]
- 27.Husted Madsen A, Haugaard K, Soerensen J, et al. Arm morbidity following sentinel lymph node biopsy or axillary lymph node dissection: a study from the Danish Breast Cancer Cooperative Group. Breast. 2008;17(2):138–47. doi: 10.1016/j.breast.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 28.Satariano WA, Ragland DR, DeLorenze GN. Limitations in upper-body strength associated with breast cancer: a comparison of black and white women. J Clin Epidemiol. 1996;49(5):535–44. doi: 10.1016/0895-4356(95)00565-x. [DOI] [PubMed] [Google Scholar]
- 29.Giuliano AE, Hunt KK, Ballman KV, et al. Axillary Dissection vs No Axillary Dissection in Women With Invasive Breast Cancer and Sentinel Node Metastasis: A Randomized Clinical Trial. JAMA. 2011;305(6):569–75. doi: 10.1001/jama.2011.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dockterman D, Velasco G. Statistical Portrait of Hispanics in the United States, 2008. Washington, D.C.: Pew Hispanic Center; Jan 21, 2010. [Google Scholar]
- 31.Mujahid MS, Janz NK, Hawley ST, Griggs JJ, Hamilton AS, Katz SJ. The impact of sociodemographic, treatment, and work support on missed work after breast cancer diagnosis. Breast Cancer Res Treat. 2010;119(1):213–20. doi: 10.1007/s10549-009-0389-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kochhar R. The Occupational Status and Mobility of Hispanics. Washington, D.C.: Pew Hispanic Center; Dec 15, 2005. [Google Scholar]
- 33.Short PF, Mallonee EL. Income disparities in the quality of life of cancer survivors. Medical Care. 2006;44(1):16–23. doi: 10.1097/01.mlr.0000188986.84819.3a. [DOI] [PubMed] [Google Scholar]
- 34.Bradley CJ, Bednarek HL, Neumark D. Breast cancer and women’s labor supply. Health Services Research. 2002;37(5):1309–28. doi: 10.1111/1475-6773.01041. [DOI] [PMC free article] [PubMed] [Google Scholar]


