Abstract
A plethora of studies have examined the efficacy and effectiveness of cognitive-behavioral therapy (CBT) for adult anxiety disorders. In recent years, several meta-analyses have been conducted to quantitatively review the evidence of CBT for anxiety disorders, each using different inclusion criteria for studies, such as use of control conditions or type of study environment. This review aims to summarize and to discuss the current state of the evidence regarding CBT treatment for panic disorder, generalized anxiety disorder, social anxiety disorder, obsessive-compulsive disorder, and post-traumatic stress disorder. Overall, CBT demonstrates both efficacy in randomized controlled trials and effectiveness in naturalistic settings in the treatment of adult anxiety disorders. However, due to methodological issues, the magnitude of effect is currently difficult to estimate. In conclusion, CBT appears to be both efficacious and effective in the treatment of anxiety disorders, but more high-quality studies are needed to better estimate the magnitude of the effect.
Keywords: cognitive-behavioral therapy, psychotherapy, meta-analysis, anxiety disorder, panic disorder, generalized anxiety disorder, obsessive-compulsive disorder, acute stress disorder, post-traumatic stress disorder
Abstract
Existen numerosos estudios que ban examinado la eficacia y efectividad de la terapia cognitivo conductual (TCC) para los trastornos ansiosos del adulto. En los ultimos anos se han efeciuado varios meta-anâiisis para revisar cuantitativamenie la evidencia de la TCC para los trastornos ansiosos, los que han empleado diferentes criterios de inclusion para los estudios, como el uso de condiciones control o el tipo de ambiente del estudio. El objetivo de esta revisión es resumir y discutir la situación actual de la evidencia en relación con el tratamienio de la TCC para el trastorno de pánico, el trastorno de ansiedad generalizada, el trastorno de ansiedad social, el trastorno obsesivo compulsivo y el trastorno por estrés postraumático. La TCC ha demostrado globalmente eficacia en ensayos controlados randomizados y efectividad en estudios naturalísticos en el tratamiento de los trastornos ansiosos del adulto. Sin embargo, debido a aspectos metodológicos, la magnitud del efecto actualmente resulta dificil de estimar. En conclusion, la TCC aparece como un tratamiento eficaz y efectivo para los trastornos ansiosos, pero se requiere de más estudios de alta calidad para una mejor estimación de la magnitud del efecto.
Abstract
Une pléthore d'études a examiné l'efficacité de la thérapie cognitivo-comportementale (TCC) dans les troubles anxieux de l'adulte. Ces dernières années, plusieurs metaanalyses ont été menées pour examiner quantitativement la preuve de l'efficacité des TCC dans les troubles anxieux, chacune utilisant des critères d'inclusion différents pour les études, comme l'utilisation des conditions de contrôle ou le type d'environnement de l'étude. Cet article a pour but de résumer et analyser l'état actuel des connaissances sur la TCC des troubles paniques, des troubles anxieux généralisés, des troubles anxieux sociaux, des troubles obsessionnels compulsifs et de l'état de stress post-traumatique. Globalement, la TCC démontre une efficacité à la fois dans les études contrôlées randomisées ainsi qu'en conditions naturelles dans le traitement des troubles anxieux de l'adulte. Cependant, l'amplitude de l'effet est actuellement difficile à évaluer du fait de problèmes méthodologiques. Pour conclure, la TCC semble être efficiente et efficace pour traiter les troubles anxieux, mais il faut des études de meilleure qualité afin de mieux estimer l'importance de son effet
Introduction
Anxiety disorders are characterized by excessive fear and subsequent avoidance, typically in response to a specified object or situation and in the absence of true danger. Anxiety disorders have a high prevalence, with a 12-month rate of about 18% and lifetime rates of about 29%.1-2 Cognitive behavioral therapy (CBT) is considered the gold standard in the psychotherapeutic treatment of anxiety disorders and several meta-analyses and reviews of these meta-analytic findings regarding the efficacy and effectiveness of CBT have been published in recent years. 3-9
CBT is defined as:
An amalgam of behavioral and cognitive interventions guided by principles of applied science. The behavioral interventions aim to decrease maladaptive behaviors and increase adaptive ones by modifying their antecedents and consequences and by behavioral practices that result in new learning. The cognitive interventions aim to modify maladaptive cognitions, self-statements or beliefs. The hallmark features of CBT are problem-focused intervention strategies that are derived from learning theory [as well as] cognitive theory principles.8 , 10
While it is beyond the scope of this article to review specific treatment components of CBT, they generally include various combinations of the following: psychoeducation about the nature of fear and anxiety, self-monitoring of symptoms, somatic exercises, cognitive restructuring (eg, logical empiricism and disconfirmation), imaginal and in vivo exposure to feared stimuli while weaning from safety signals, and relapse prevention.8 Depending on the specific anxiety disorder, these CBT techniques are weighted differentially during therapy.
A plethora of studies have examined the efficacy of CBT for adult anxiety disorders. Furthermore, several meta-analyses have been conducted to quantitatively review the evidence of CBT for anxiety disorders.4,6,9,11 In meta-analysis, treatment efficacy is quantified in terms of an effect size. An effect size indicates the magnitude of an observed effect in a standard unit of measurement. However, it is important to realize that different types of effect sizes can be used to appraise the available evidence. For instance, effect sizes are sometimes categorized as ”controlled“ versus ”uncontrolled.“4 A controlled effect size expresses the magnitude of a specific treatment effect as compared with alternative treatments or control conditions. Most often, it is calculated by subtracting the post-treatment mean of the control group from the post-treatment mean of the treatment group divided by the pooled standard deviation. This effect size is called Cohen's d. 12 An uncontrolled effect size expresses the magnitude of improvement within a group from pretreatment to post-treatment. It is calculated by subtracting a group's post-treatment mean from its pretreatment mean divided by the pooled standard deviation. Uncontrolled effect sizes are less preferable than controlled effect sizes, since they are susceptible to threats to internal validity.4
Meta-analytic reviews of CBT studies in anxiety disorders have generally found large effect sizes for the majority of treatment studies. Accordingly, recent reviews that summarized the results of these numerous meta-analyses of CBT treatment in anxiety disorders concluded that CBT is highly effective.3 - 4 - 13
However, these existing meta-analyses are not without limitations. In particular, most meta-analyses of CBT for anxiety disorders have included studies that vary greatly with respect to control procedures, which range from waitlist, alternative treatments, and placebo interventions that were evaluated with or without randomization while some studies did not include any control groups. However, it is important to determine how including a control condition and their specific nature impacts the efficacy results of CBT in anxiety disorders. Furthermore, one important question is how results derived from research studies in mostly well-controlled research designs (efficacy) generalize to real-world settings in naturalistic surroundings (effectiveness).
Therefore, this review will particularly focus on two recent meta-analyses by Hofmann6 and by Stewart11regarding CBT treatment for panic disorder, generalized anxiety disorder, social anxiety disorder, obsessive-compulsive disorder, and post-traumatic stress disorder.
The first meta-analysis6 limited the included studies to randomized placebo-controlled trials, the gold standard in clinical outcome research. For example, the Federal Drug Administration (FDA) in the United States and the European Medicines Agency (EMA) require successful randomized placebo-controlled double-blind trials in order to approve a new medication. Pharmacotherapy trials typically administer a sugar pill to individuals in the placebo condition. Instead of including a pill placebo, a number of psychotherapy trials have employed psychological placebo conditions to control for nonspecific factors. To be included in the meta-analysis,6 the psychological placebo had to involve interventions to control for nonspecific factors (eg, regular contact with a therapist, reasonable rationale for the intervention, discussions of the psychological problem). Although it is almost impossible to protect the blind in placebo-controlled psychotherapy trials, the randomized placebo-controlled design is still the most rigorous and conservative test of the effects of an active treatment. This approach assesses the overall efficacy of CBT in anxiety disorders under well-controlled research conditions. Overall, 27 studies met inclusion criteria: n=7 for social anxiety disorder, n=6 for post-traumatic stress disorder, n=5 for panic disorder, n=4 for acute stress disorder, n=3 for obsessive-compulsive disorder, and n=2 for generalized anxiety disorder. As a controlled effect size, Hedges' g was calculated, which is a variation of Cohen's d taking into account small sample sizes.
In contrast to well-controlled efficacy studies in research settings, effectiveness studies examine how efficacious interventions are transferred into naturalistic real-world settings. Research treatments might not work equally well in clinical practice settings because of greater disease severity, or more comorbid conditions in patients in general practice compared with patients in research settings. Another variable that might impact the outcome in naturalistic settings is the treatments themselves and the clinicians who provide them. Treatment protocols in randomized controlled trials are manualized and strictly monitored with an emphasis on treatment integrity. However, therapy manuals are less likely to be used in clinical practice. Furthermore, practitioners typically do not have access to the level of intensive training, monitoring, and supervision available to therapists in research settings. Clinicians in research settings are more likely to be expert in the administration of particular treatments and are motivated through adherence measures to stay consistent with the protocol. In summary, treatments delivered in naturalistic settings may not be as rigorous in terms of content or quality, and this may limit how well results of controlled research trials can generalize to actual clinical practice. Therefore, it is important to empirically examine how well findings from research studies (efficacy) translate into real-world settings (effectiveness). Thus, in the second meta-analysis11, 56 effectiveness studies were included to assess how CBT treatment works in less well-controlled real-life settings. CBT was defined broadly and included any treatment with cognitive, behavioral (eg, exposure), or a combination of components. In sum, a total of 56 studies were included in these analyses: 17 for panic disorder; 11 each for social anxiety disorder, OCD, and GAD; and 6 for PTSD. No study assessed effectiveness in acute stress disorder. We will present and contrast the meta-analytically derived controlled and uncontrolled effect sizes reflecting the efficacy and effectiveness results for each anxiety disorder.
Results
Panic disorder
Panic attacks are defined as sudden spells of unidentified feelings consisting of at least four out of 13 symptoms such as palpitations, chest pains, sweating, shortness of breath, feelings of choking, trembling, nausea, dizziness, paresthesias, chills or hot flushes, depersonalization or derealization, and fear of dying or losing control. In order to make a diagnosis of panic disorder, additional criteria are that these attacks at least once have been unexpected, followed by at least 1 month of fearful expectation or concern about the consequences of an attack. Panic disorder is frequently followed (or accompanied) by agoraphobia, which is defined as follows: (i) fear of being in places or situations from which escape might be difficult or help might not be available; (ii) these situations are avoided or endured with marked distress or the patient needs a companion.
CBT for panic disorder typically involves education about the nature and physiology of the panic response, cognitive therapy techniques designed to modify catastrophic misinterpretations of panic symptoms and their consequences, and graduated exposure to panic-related body sensations (ie, interoceptive exposure) and avoided situations.
Efficacy
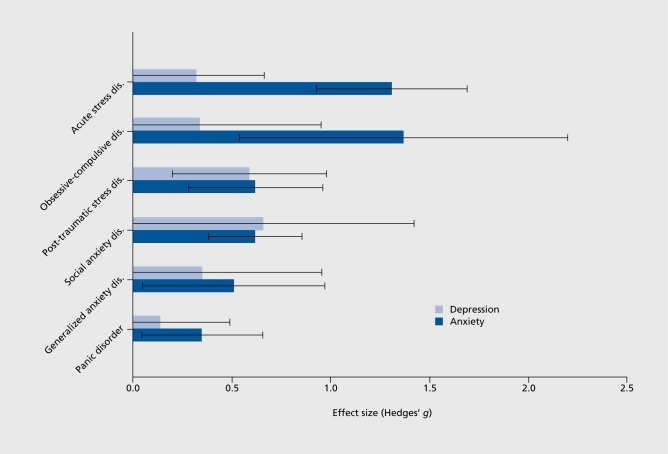
Five studies examined the efficacy of CBT in panic disorder in a randomized placebo-controlled design.6 The effect size was 0.35 (95% CI 0.04-0.65), indicating a small to medium effect ((Figure 1). How important it is to take into account the type of effect size when appraising the magnitude of effect can be seen from a different meta-analysis that calculated uncontrolled pre- to post-treatment effect sizes.9. That meta-analysis reported an effect size of 1.53 for CBT in panic disorder.
Figure 1. Average effect size estimates and corresponding 95% confidence intervals of the acute treatment efficacy of cognitive-behavioral therapy as compared with placebo on the various anxiety disorders for the primary continuous anxiety measure (dark blue bars) and depression measures (light blue bars) Adapted from ref 6: Hofmann SG, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69:621-632. Copyright© Physicians' Postgraduate Press, 2008 .
Effectiveness
Several studies examined the effectiveness of CBT in panic disorder.11 The calculated uncontrolled pre- to post-treatment effect size was 1.01 (95% CI 0.77-1.25) for panic attacks and 0.83 (95% CI 0.60-1.06) for avoidance.
Generalized anxiety disorder
Generalized anxiety disorder is marked by excessive and uncontrollable worry. It is believed to be maintained by cognitive (attention and judgment) biases toward threat-relevant stimuli and the use of worry (and associated tension) and overly cautious behaviors as a means to avoid catastrophic images and associated autonomic arousal.8 CBT of generalized anxiety disorder involves cognitive therapy to address worry and cognitive biases and relaxation to address tension, as well as imaginal exposure to catastrophic images and exposure to stressful situations while response preventing overly cautious behaviors.
Efficacy
The controlled effect size for CBT in generalized anxiety disorder was 0.51 (95% CI 0.05-0.97), indicating a medium effect (Figure 1) although only two studies using a randomized controlled design to examine CBT treatment in patients with generalized anxiety disorder were available. Nevertheless, these results were recently corroborated by a Cochrane meta-analysis examining psychological treatments of generalized anxiety disorder.14 Based on thirteen studies, the authors concluded that psychological therapies, all using a CBT approach, were more effective than treatment as usual or wait list control in achieving clinical response at post-treatment (RR 0.64, 95% CI 0.55-0.74). However, those studies examining CBT against supportive therapy (nondirective therapy and attention-placebo conditions) did not find a significant difference in clinical response between CBT and supportive therapy at post-treatment (RR 0.86, 95%CI 0.70 to 1.06).
Again, the meta-analysis calculating uncontrolled pre- to post-treatment effect sizes found much a larger overall effect size of 1.80. 9
Effectiveness
In eleven effectiveness studies, the pre- to post-treatment effect size for CBT in generalized anxiety disorder was 0.92 (95% CI 0.77-1.07).
Social anxiety disorder
Social anxiety disorder (or social phobia) is characterized by marked fear of performance, excessive fear of scrutiny, and fear of acting in a way that may be embarrassing. Most patients are oversensitive to the assumed opinion of others and have a low self-esteem, although they feel their fears are exaggerated and out of proportion. Going through the feared situations, or even anticipating them, most people suffer from physical symptoms like sweating, trembling, or blushing, and these symptoms can become a trigger on their own to worry about social consequences. CBT for social phobia typically emphasizes cognitive restructuring and in vivo exposure to feared social situations. Patients are instructed in identifying and challenging their beliefs about their social competence and the probability of experiencing negative social evaluation and consequences. In vivo exposures provide opportunities to confront feared and avoided social encounters and to practice social skills. ((Figure 2).
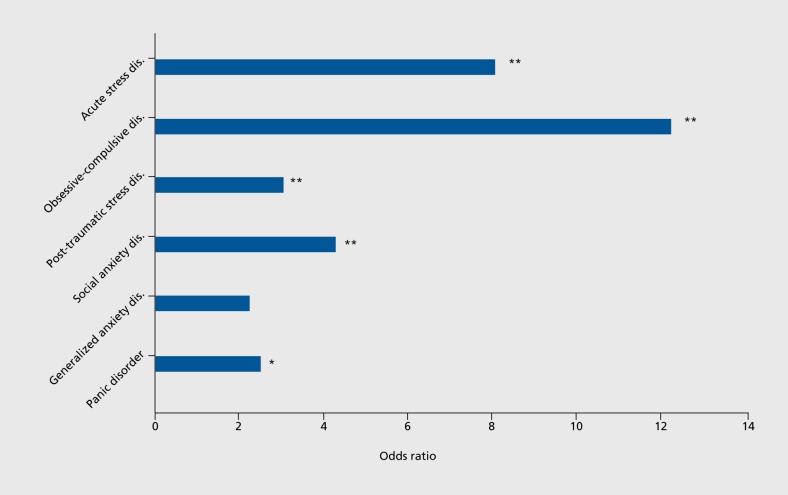
Figure 2. Average odds ratios of acute treatment response to cognitive-behavioral therapy as compared with placebo. *, P<0.05; **, P<0.01 Adapted from ref 6: Hofmann SG, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69:621-632. Copyright© Physicians' Postgraduate Press, 2008.
Efficacy
In seven randomized placebo-controlled treatment studies, the effect of CBT in social anxiety disorder was 0.62 (95% CI 0.39-0.86, Figure 1) indicating a medium effect. In a separate meta-analysis, the uncontrolled pre- to post-treatment acute treatment effect size was 1.27.9
Effectiveness
In eleven effectiveness studies, the uncontrolled pre- to post-treatment effect size was 1.04 (95% 0.79-1.29).5
Post-traumatic stress disorder
The DSM-IV definition for post-traumatic stress disorder (PTSD) contains criteria for: (i) the traumatic experience; (ii) re-experiencing; (iii) avoidance of associated stimuli and numbing; and (iv) increased arousal. CBT for PTSD typically includes three components: (i) psychoeducation about the nature of fear, anxiety, and PTSD; (ii) controlled, prolonged exposure to stimuli related to the traumatic event; and (iii) cognitive restructuring, processing, or challenging of maladaptive beliefs/appraisals.
Efficacy
In six randomized placebo-controlled efficacy trials of CBT in PTSD, the controlled effect size was 0.62 (95% CI 0.28-0.96), indicating a medium effect. A recent Cochrane analysis of psychological treatment in PTSD15 supported these findings and found that trauma-focused CBT was more effective than treatment as usual or wait list control. The uncontrolled effect size derived from a separate meta-analysis was 1.86. 9
Effectiveness
Six studies examined the effectiveness of CBT in the treatment of PTSD5 and found an uncontrolled pre- to post-treatment effect size of 2.59 (95% CI 2.06-3.13).
Acute stress disorder
Acute stress disorder is an anxiety disorder characterized by a cluster of dissociative and anxiety symptoms that occur within a month of a traumatic stressor. Acute stress disorder may be diagnosed in patients who (i) lived through or witnessed a traumatic event to which they (ii) responded with intense fear, horror, or helplessness, and are (iii) currently experiencing three or more of the following dissociative symptoms: psychic numbing, being dazed or less aware of surroundings, derealization, depersonalization, or dissociative amnesia.
Efficacy
In four randomized placebo-controlled efficacy trials of CBT in acute stress disorder, the controlled effect size was 1.31 (95% CI 0.93-1.69) indicating a large effect. Consistent with these results, a recent Cochrane metaanalysis concluded that there was evidence that individual trauma-focused CBT was effective for individuals with acute traumatic stress symptoms compared with both waiting list and supportive counseling interventions.16
Effectiveness
No effectiveness data were available/included in the meta-analysis of CBT treatment in acute stress disorder.5
Obsessive-compulsive disorder
Obsessive-compulsive disorder (OCD) is defined as the presence of recurrent obsessions (persistent thoughts, impulses, or images) or compulsions (repetitive behavior or thought patterns induced in an attempt to prevent anxiety) that are excessively time-consuming (taking more than an hour a day) or cause marked distress or significant impairment. The subject recognizes that these patterns are excessive. Components of CBT in the treatment of OCD include exposure and response prevention as well as cognitive interventions.3
Efficacy
Three studies examined CBT treatment in OCD in a randomized placebo-controlled design. The controlled effect size was 1.37 (95% CI 0.64-2.20) indicating a large effect, in fact the largest effect size for CBT in any of the anxiety disorders (Figure 1). However, the 95% confidence interval was large due to the small numbers of included studies (n=3). Interestingly, the uncontrolled pre- to post-treatment effect size of 1.50 that was calculated in a separate meta-analysis' was only marginally larger than the controlled effect size.
These results were corroborated by a Cochrane analysis of eight studies, all of which compared cognitive and/or behavioral treatments versus treatment as usual control groups.17 These studies demonstrated that patients receiving any variant of cognitive behavioral treatment exhibited significantly fewer symptoms post-treatment than those receiving treatment as usual.
Effectiveness
Consistent with the acute efficacy effects of CBT in OCD, eleven effectiveness studies found an uncontrolled effect size of 1.32 (95% CI 1.19-1.45) in real-world settings.5
Summary
According to recent meta-analyses examining CBT in anxiety disorders in randomized placebo-controlled trials6 and in naturalistic real-life settings,5 both the efficacy and effectiveness of CBT for anxiety in adults appears to be well established. These favorable effects of CBT are further corroborated by several Cochrane analyses of psychological treatments for several anxiety disorders.14-16
The controlled effect sizes from 27 randomized placebo-controlled trials involving 1496 patients ranged from 0.35 in panic disorder (small effect) to 1.37 in obsessive-compulsive disorder (large effect) indicating that CBT compared favorably to placebo conditions in all anxiety disorders. In post-hoc comparisons, the only significant difference among the different anxiety disorders regarding the efficacy of CBT was between panic disorder and obsessive-compulsive disorder. Furthermore, the effect size for ASD was significantly greater relative to those observed for all other anxiety disorders except OCD. However, these results should be interpreted with caution given the small numbers of included studies for each anxiety disorder (n of studies ranging from 2 to 7 for each specific disorder).
Although this meta-analysis circumvented many methodological problems of other meta-analyses of psychotherapy studies by including only randomized, placebo-controlled trials, there still remained methodological issues that need to be taken into account when appraising these results. As indicated by the authors, a concerning issue is the lack of intention-to-treat (ITT) analyses in most studies included. An ITT analysis is based on the initial treatment intent, not on the treatment eventually administered. ITT analysis is intended to avoid various misleading arti-facts that can arise in intervention research. For example, if people who have a more refractory or serious problem tend to drop out at a higher rate, even a completely ineffective treatment may appear to be providing benefits if one merely compares the condition before and after the treatment for only those who finish the treatment (ignoring those who were enrolled originally, but have since been excluded or dropped out). For the purposes of ITT analysis, everyone who begins the treatment is considered to be part of the trial, whether he or she finishes it or not. This is different from the completer or per-protocol analysis, which only includes those patients finishing the trial. Thus, the ITT analysis is a much more conservative measure and is generally used in pharmacotherapy studies.
Not surprisingly therefore, in the meta-analysis of randomized, placebo-controlled trials, pooled analyses using data from ITT samples yielded much smaller effect sizes than those derived from completer samples. In the completer sample, the overall Hedges' g for anxiety disorder severity was 0.73 (95% CI: 0.56-0.90 and the pooled odds ratio for treatment response was 4.06 (95% CI: 2.78-5.92). However, in ITT analyses that were only provided for the minority of included studies, the Hedges' g for anxiety disorder severity was 0.33 (95% CI: 0.110.54), and the odds ratio for treatment response was 1.84 (95% CI: 1.17-2.91). The authors of the meta-analysis6 concluded the following:
Given the status of CBT as the gold-standard psychosocial intervention for treating anxiety disorders, it is very surprising and concerning that after more than 20 years of CBT treatment research, we were only able to identify 6 high-quality randomized placebo controlled CBT trials that provided ITT analyses for continuous measures and only 8 trials for ITT response rate analyses. In our opinion, this is an unacceptable situation that will have to change for psychosocial intervention to become a viable alternative to pharmacotherapy in the medical community.
In 56 effectiveness studies of CBT in anxiety disorders in naturalistic real-life settings, the (uncontrolled) effect sizes ranged from 0.92 in generalized anxiety disorder to 2.59 in post-traumatic stress disorder. It is important to keep in mind that these uncontrolled pre-to post-treatment effect sizes cannot be readily compared with the controlled effect sizes. Nevertheless, these effect sizes seem to indicate that CBT also works in real-world settings in the treatment of anxiety disorders. Again, in that meta-analysis only 4 out of 56 included reports of intention-to-treat data, prohibiting a meaningful ITT-analysis. Newer therapies for anxiety disorders include mindfulness-based therapies. These therapies propose different approaches for dealing with anxiety-related cognition, including cognitive defusion (eg, distancing from the content of fear-based thinking) and mindfulness and acceptance, and are more contextually based. They are sometime called the “third wave” of CBT. A recent meta-analysis found that mindfulness-based therapy in patients with anxiety disorders was associated with a large effect size (Hedges' g) of 0.97 (95% CI: 0.72-1.22) for improving anxiety.18 Thus, mindfulness-based therapy is a promising newapproach in the treatment of anxiety disorders.
Furthermore, pharmacological augmentation strategies designed to enhance the learning that occurs with CBT approaches for anxiety disorders may hold particular promise. For example, recent studies demonstrated that glucocorticoids administered 1 hour prior to therapy sessions enhance extinction-based psychotherapy in anxiety disorders.19,20 Furthermore, d-cycloserine, a drug used in the treatment of tuberculosis, has been shown to enhance fear extinction in several preclinical studies21 but also in clinical trials in patients with different anxiety disorders:22 Thus, combining exposure therapy with pharmacological agents holds significant promise for improving the efficacy of CBT.
Conclusion
Despite some weaknesses of the original studies, the quantitative literature review of randomized placebo-controlled trials and of trials in naturalistic treatment settings provides strong support for both the efficacy and effectiveness of CBT as an acute intervention for adult anxiety disorders. At the same time, the results also suggest that there is still considerable room for further improvement of study and analysis methods. Thus, the exact magnitude of effect is currently difficult to estimate. Nevertheless, the meta-analyses confirm that CBT is by far the most consistently empirically supported psychotherapeutic option in the treatment of anxiety disorders. Thus, CBT can be recommended as a gold standard in the psychotherapeutic treatment of patients with anxiety disorders.
REFERENCES
- 1.Kessler RC., Berglund P., Dernier O., Jin R., Merikangas KR., Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC., Ruscio AM., Shear K., Wittchen HU. Epidemiology of anxiety disorders. Curr Top Behav Neurosci. 2010;2:21–35. [PubMed] [Google Scholar]
- 3.Olatunji BO., Cisler JM., Deacon BJ. Efficacy of cognitive behavioral therapy for anxiety disorders: a review of meta-analytic findings. Psychiatr Clin N Am. 2010;33:557–577. doi: 10.1016/j.psc.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 4.Butler AC., Chapman JE., Forman EM., Beck AT. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev. 2006;26:17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Stewart RE., Chambless DL. Cognitive-behavioral therapy for adult anxiety disorders in clinical practice: a meta-analysis of effectiveness studies. J Consult Clin Psychol. 2009;77:595–606. doi: 10.1037/a0016032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hofmann SG., Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008;69:621–632. doi: 10.4088/jcp.v69n0415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klein DF. Flawed meta-analyses comparing psychotherapy with pharmacotherapy. Am J Psychiatry. 2000;157:1204–1211. doi: 10.1176/appi.ajp.157.8.1204. [DOI] [PubMed] [Google Scholar]
- 8.Arch JJ., Craske MG. First-line treatment: a critical appraisal of cognitive behavioral therapy developments and alternatives. Psychiatr Clin North Am. 2009;32:525–547. doi: 10.1016/j.psc.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 9.Norton PJ., Price EC. A meta-analytic review of adult cognitive-behavioral treatment outcome across the anxiety disorders. J Nerv Ment Dis. 2007;195:521–531. doi: 10.1097/01.nmd.0000253843.70149.9a. [DOI] [PubMed] [Google Scholar]
- 10.Craske M. Cognitive-Behavioral Therapy. New York, NY: APA Books. 2010 [Google Scholar]
- 11.Stewart RE., Chambless DL. Cognitive-behavioral therapy for adult anxiety disorders in clinical practice: a meta-analysis of effectiveness studies. J Consult Clin Psychol. 2009;77:595–606. doi: 10.1037/a0016032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Erlbaum. 1988 [Google Scholar]
- 13.Deacon BJ., Abramowitz JS. Cognitive and behavioral treatments for anxiety disorders: a review of meta-analytic findings. J Clin Psychol. 2004;60:429–441. doi: 10.1002/jclp.10255. [DOI] [PubMed] [Google Scholar]
- 14.Hunot V., Churchill R., Silva de Lima M., Teixeira V. Psychological therapies for generalised anxiety disorder. Cochrane Database Syst Rev. 2007:CD001848. doi: 10.1002/14651858.CD001848.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bisson J., Andrew M. Psychological treatment of post-traumatic stress disorder (PTSD). Cochrane Database Syst Rev. 2007:CD003388. doi: 10.1002/14651858.CD003388.pub3. [DOI] [PubMed] [Google Scholar]
- 16.Roberts NP., Kitchiner NJ., Kenardy J., Bisson Jl. Early psychological interventions to treat acute traumatic stress symptoms. Cochrane Database Syst Rev. 2010:CD007944. doi: 10.1002/14651858.CD007944.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gava I., Barbui C., Aguglia E., et al. Psychological treatments versus treatment as usual for obsessive compulsive disorder (OCD). Cochrane Database Syst Rev. 2007:CD005333. doi: 10.1002/14651858.CD005333.pub2. [DOI] [PubMed] [Google Scholar]
- 18.Hofmann SG., Sawyer AT., Witt AA., Oh D. The effect of mindfulnessbased therapy on anxiety and depression: a meta-analytic review. J Consult Clin Psychol. 2010;78:169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bentz D., Michael T., de Quervain DJF., Wilhelm FH. Enhancing exposure therapy for anxiety disorders with glucocorticoids: From basic mechanisms of emotional learning to clinical applications. J Anxiety Disord. 2010;24:223–230. doi: 10.1016/j.janxdis.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 20.de Quervain DJ-F., Bentz De., Michael T., et al. Glucocorticoids enhance extinction-based psychotherapy. Proc Natl Acad Sci USA. 2011;108:6621–6625. doi: 10.1073/pnas.1018214108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davis M., Ressler K., Rothbaum BO., Richardson R. Effects of D-cycloserine on extinction: translation from preclinical to clinical work. Biological Psychiatry. 2006;60:369–375. doi: 10.1016/j.biopsych.2006.03.084. [DOI] [PubMed] [Google Scholar]
- 22.Ganasen KA., Ipser JC., Stein DJ. Augmentation of cognitive behavioral therapy with Pharmacotherapy. Psychiatr Clin N America. 2010;33:687–699. doi: 10.1016/j.psc.2010.04.008. [DOI] [PubMed] [Google Scholar]