Abstract
Purpose
Research suggests stereotype endorsement or self-stigma serves as a barrier to functioning and well-being among persons with schizophrenia. Little is known about how stable self-stigma is and whether it is linked over time with related constructs such as discrimination experiences and psychological distress.
Methods
Stereotype endorsement and discrimination experiences were assessed using the Internalized Stigma of Mental Illness Scale and psychological distress was assessed using the Emotional Discomfort component of the Positive and Negative Syndrome Scale, at three points in time across 1 year.
Results
Path analyses indicated that the constructs of stereotype endorsement and discrimination experiences are stable over periods of 5–7 months and may fluctuate over 12 months. Further, the constructs of stereotype endorsement and discrimination experiences were related to one another concurrently, but analyses failed to detect a relationship over time. Neither construct was related to psychological distress over time.
Conclusions
Self-stigma is a stable construct in the short term, and is distinct from related constructs such as discrimination experiences and psychological distress.
Keywords: Schizophrenia, Stigma, Symptoms, Discrimination, Recovery, Rehabilitation
Introduction
Despite increased awareness of the nature of schizophrenia spectrum disorders, many among the general public hold stereotyped beliefs about persons with these conditions [1, 2]. Categorically referred to as stigma, these beliefs include heightened expectations of violent and disorderly behavior, lack of personal competence, as well as an inability to sustain gainful employment or make informed decisions [3–5]. Link and Phelan [6] have described three mechanisms by which stigma may affect individuals with mental illness. At the broadest level, structural/institutional mechanisms and legal restrictions can restrict opportunities for stigmatized individuals. At the level of individual interactions, overt and subtle discriminatory behaviors can negatively affect stigmatized individuals. For example, community members may reject or seek social distance from persons with schizophrenia [7, 8], which can negatively affect social relationships and mood [9]. Finally, awareness of stigma can directly affect stigmatized individuals’ self-perceptions.
Two main mechanisms are proposed for how stigma can affect individuals’ self-perceptions. Link’s modified labeling perspective posits that generally held stereotypical attitudes about people with mental illness take on personal relevance among diagnosed individuals, who then incorporate them into self-conceptions [10]. Research examining the modified labeling perspective tends to use the Devaluation-Discrimination scale [11], which examines degree of endorsement of negative attitudes that “most people” might hold about persons with mental illness. A second manner in which stigma can impact self-conceptions concerns the more overt process of internalization of stigmatizing views. Individuals who internalize stigma come to directly agree with stigmatizing views about mental illness and agree that they apply to them (e.g., that one is incapable of working as a result of having a mental illness) and incorporate these views into their identity [12].
The internalization of stigma (also referred to as stereotype endorsement or self-stigma) may represent a potent barrier to functioning because it may incline persons to believe that they are not equal members of their communities and to entertain self-fulfilling prophecies of failure [13–15]. The levels of distress that self-stigma produces may further exacerbate symptoms or other underlying neurobiological factors associated with illness [16], increase risk for suicide [17] and possibly lead some with mental illness to reject that they are ill or at least to reject treatment [18–22], creating a vicious cycle of dysfunction. Internalized stigma has been found to predict more severe levels of symptoms when assessed concurrently and prospectively [23–25] and is also linked with lower levels of self-esteem [26].
Despite the considerable number of studies that have been conducted regarding self-stigma, several unaddressed issues remain. One area that remains unclear is the extent to which the internalization of stigmatizing views is related to the experience of stigmatizing interactions. Studies have linked the experience of rejection and other negative social interactions to poorer life satisfaction and self-esteem [15, 27–29], and research has observed a relationship between report of rejection experiences and endorsement of awareness of stigmatizing community attitudes as reflected in the Devaluation-Discrimination scale [30]. However, research has yet to explicitly examine the extent to which the experience of stigmatizing interactions, such as social rejection, is directly related to the explicit internalization of stigmatizing views.
Another understudied issue concerns the stability of self-stigma over time. The extent to which negative beliefs about the self and one’s mental illness persist over time has not been studied. Furthermore, the degree to which stereotyped beliefs about one’s mental illness overlap with the experience of discrimination and distress has not been studied. It is not known whether stereotype endorsement, discrimination experiences, and distress represent distinct constructs that meaningfully persist over time, influencing one another in the moment but following their own course over time, or if they are simply reflective of a general underlying state of dysfunction. An understanding of these issues would have several important implications. For one, it would illuminate the issue of whether a person’s level of stereotype endorsement is more a function of a stable belief or of current or previous discrimination experiences. It would also address whether helping to reduce discrimination experiences would necessarily reduce previously existing self-stigma.
To address these issues, we used structural equation modeling to simultaneously examine the relationships among assessments of discrimination experience, stereotype endorsement (internalized stigma) and distressed mood in a sample of persons with schizophrenia-spectrum disorders assessed over three time points within the period of 1 year. Given the lack of prior studies on the topic, we considered these analyses to be largely exploratory and planned to examine whether the measurements of each construct at each time would be related to: (i) measurements of that same construct at other time points or (ii) other constructs at the same time point. We were also interested in investigating whether stereotype endorsement and discrimination experience were related to an index of psychological distress concurrently and over time.
Methods
Participants
Ninety-five males and 15 females with SCID [31] confirmed DSM-IV diagnoses of schizophrenia (n = 73) or schizoaffective disorder (n = 37) were recruited from a comprehensive day hospital at a VA Medical Center and local community mental health center for a larger survey of the effects of cognitive therapy and vocational rehabilitation in schizophrenia. All participants were receiving ongoing outpatient treatment and were in a non-acute or stable phase of their disorder, defined as no hospitalizations or changes in medication or housing in the last month. Participants with active substance dependence or those with a documented history of mental retardation were excluded. Participants had a mean age of 46.03 (SD = 10.09), a mean educational level of 12.57 (SD = 2.24) and a mean of 7.58 (SD = 9.61) lifetime psychiatric hospitalizations with the first occurring on average at the age of 27.19 (SD = 9.79). Forty-one percent of the sample was Caucasian, 58% was African American, and 1% was Latino.
Instruments
The Internalized Stigma of Mental Illness Scale (ISMIS) [13] is a 29-item questionnaire designed to assess subjective experience of stigma. It presents participants with first-person statements and asks them to rate on a 4-point Likert scale the extent to which they agree or disagree. Items are then summed to provide five subscale scores. For the purposes of this study, we were primarily interested in two of these scales: Stereotype Endorsement, which reflects agreement with negative stereotypes of mental illness and Discrimination Experience, which reflects current mistreatment attributed to the biases of others. All subscale scores are calculated as averages with higher scores suggesting graver experiences of stigma. Evidence of acceptable internal consistency, test–retest reliability, factorial and convergent validity has been reported by the authors [13].
The Positive and Negative Syndrome Scale (PANSS) [32] is a 30-item rating scale completed by clinically trained research staff at the conclusion of chart review and a semi-structured interview. It is one of the most widely used semi-structured interviews for assessing the wide range of psychopathology in schizophrenia. For the purposes of this study, we were interested in an index of psychological distress and, therefore, used the factor analytically derived Emotional Discomfort component, which includes the symptoms of depression, anxiety, guilt and active social avoidance [33]. Assessment of inter-rater reliability for this study was found to be good to excellent with intraclass correlations for blind raters.
Procedures
The research review committees of Indiana University and the Roudebush VA Medical Center approved all procedures. Following informed consent, diagnoses were determined using the Structured Clinical Interview for DSM-IV conducted by a clinical psychologist. Following the SCID, participants were administered the PANSS and ISMIS as part of an assessment battery for participants entering a vocational rehabilitation research program. A research assistant was available to assist participants if there were difficulties reading or understanding the questionnaire. PANSS ratings were performed blind to responses to the ISMIS. PANSS interviews were conducted by trained research assistants with a minimum of a B.A. degree in a field related to psychology.
Within two weeks of completing the baseline assessments, all participants were offered a 6-month part-time, paid work placement within the VA medical center. More information about placements and support services have been reported elsewhere [34]. The PANSS and ISMIS were administered a second time 5 months after baseline assessments were completed, and a third time 1 year after baseline assessments were completed (i.e., 7 months after the second assessments were completed).
Analyses
Data analysis was conducted in three phases. First, correlations were obtained among all three variables of interest at each time point. Second, if significant correlations were found between and among measurements of stereotype endorsement and discrimination experiences over three time points, we planned to explore these concurrent and prospective relationships using a measured-variable path analysis using structural equation modeling software. Third, if correlations were observed between the PANSS emotional discomfort score and stereotype endorsement and discrimination experience, we planned a second path analysis exploring these relationships in a similar manner.
We analyzed the hypothesized models using LISREL 8.8 [35]. In our path analyses, we treated the baseline measures of stereotype endorsement, discrimination, and distress as exogenous variables and all of the Time 2 and Time 3 measures of these constructs as endogenous variables. In the first model, we proposed that stereotype endorsement and discrimination would predict each other over time. In the second model, we proposed that discrimination and distress would predict each other over time but that stereotype endorsement would be independent of the other two over time. Additionally, for both models we predicted that these constructs would all be related at a single time point.
We evaluated model fit using the chi-square statistic (χ2) and the root mean square error of approximation (RMSEA). The chi-square statistic tests the difference between the observed correlation matrix and the theoretically proposed correlation matrix. A small, non-significant chi-square is desired, which indicates that the observed correlations are not significantly different from the expected correlations [36]. The RMSEA indicates how well the model would fit the hypothetical population covariance matrix. Acceptable values are 0.0–0.10, with smaller RMSEAs indicating adequate fit and values less than 0.05 indicating good fit [37]. Parameters were estimated by full information maximum likelihood, which uses all of the observed data and is superior to traditional methods of handling missing data [38].
Results
Data were checked for normality and fit assumptions for parametric statistics. The zero-order correlations, means, and standard deviations for all study measures are presented in Table 1. As expected, we found that stereotype endorsement at baseline, 5 months, and 12 months was moderately to strongly related to all three time points of discrimination. We also found that the relationship between stereotype endorsement and distress over time was inconsistent, and the two constructs were unrelated at several time points. In contrast, the relationship between discrimination and distress was much more consistent as evidenced by significant correlations across most time points (see Table 1).
Table 1.
Correlations, means, and standard deviations for measures
| SEB | DISCB | SE5 | DISC5 | SE12 | DISC12 | D5 | D21 | |
|---|---|---|---|---|---|---|---|---|
| SEB | – | |||||||
| DISCB | 0.53** | – | ||||||
| SE5 | 0.59** | 0.43** | – | |||||
| DISC5 | 0.35** | 0.65** | 0.59** | – | ||||
| SE12 | 0.29* | 0.27* | 0.62** | 0.45** | – | |||
| DISC12 | 0.32* | 0.48* | 0.54** | 0.66** | 0.76** | – | ||
| DB | 0.17 | 0.30** | 0.21 | 0.33** | 0.02 | 0.21 | – | |
| D21 | 0.17 | 0.27* | 0.26* | 0.33** | 0.13 | 0.26 | 0.51** | – |
| D52 | 0.28* | 0.47** | 0.39** | 0.52** | 0.22 | 0.33* | 0.50** | 0.79* |
N = 110
SEB stereotype endorsement at baseline, DISCB discrimination at baseline, SE5 stereotype endorsement at 5 months, DISC5 discrimination at 5 months, SE12 stereotype endorsement at 12 months, DISC12 discrimination at 12 months, DB distress at baseline, D21 distress at 21 weeks, D52 distress at 52 weeks
p < 0.05;
p < 0.01
Path analysis
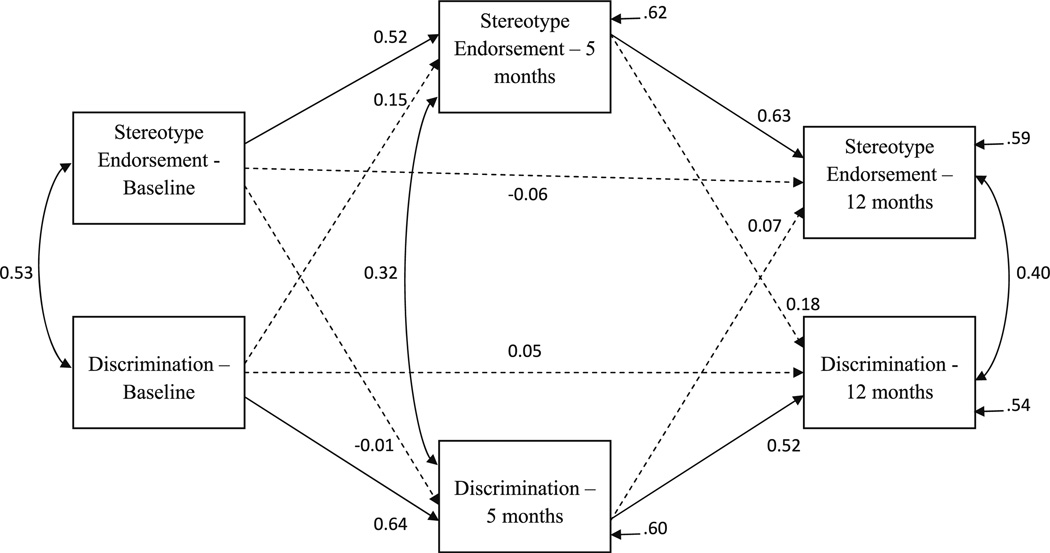
Model 1: Initially, we were interested in determining if two different aspects of stigma (i.e., stereotype endorsement and discrimination) predicted each other over time. We began with a theoretical path model based on the hypothesis that, consistent with the moderate to strong correlations among the variables, each subtype would predict the other subtype prospectively. In other words, we hypothesized that stereotype endorsement at baseline would predict discrimination at 5 months and vice versa. Additionally, we hypothesized that the cross-lagged paths from 5 to 12 months would also be significant. The basic model testing our hypotheses showed good fit to the observed data, , p = 0.85, RMSEA = 0.000, and is presented in Fig. 1.
Fig. 1.
Path model of stereotype endorsement and discrimination across three time points.
N = 110. Non-significant paths are indicated by dashed lines. All other paths are significant at the 0.05 level
The findings from the model indicate that stereotype endorsement and discrimination do not predict each other over time; none of the cross-lagged paths for all three time points were significant. Moreover, autoregressive paths for stereotype endorsement and discrimination (e.g., discrimination at baseline predicting discrimination at 5 months) were significant. We failed to find that the baseline measures of stereotype endorsement and discrimination predicted 12-month measures of these constructs. Our findings thus failed to suggest that these constructs are entirely trait-like and it is possible that they do fluctuate over time, with the best predictor of the current levels being the most proximal previous measure. The model accounted for 41% of the variance in stereotype endorsement at 12 months and 46% of the variance in discrimination at 12 months.
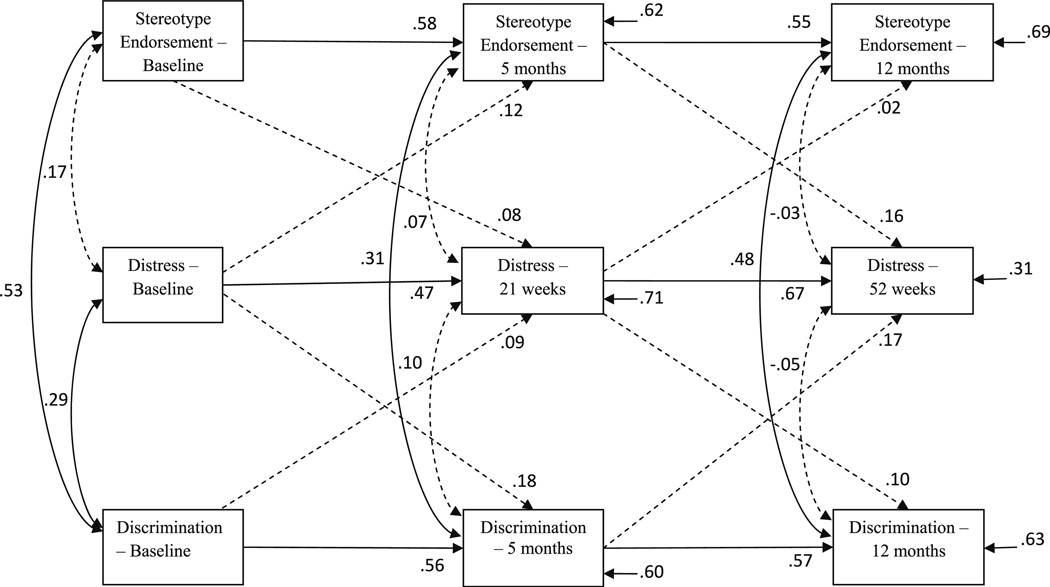
Model 2: Examining the zero-order correlations (presented in Table 1) of each of the subtypes of stigma, we became interested in their differential relationships with distress. Thus, we created a second theoretical model based on the hypothesis that discrimination and distress would predict each other over time but that stereotype endorsement would not predict anything other than itself. The number of parameters-to-sample size ratio for this model using the current sample (4.78) is slightly smaller than the recommended minimum of 5 participants per path [39]. We thought that it was worthwhile to test this model because how these constructs are related over time may have important implications for future research and interventions; however, the results from this model should be interpreted with the small parameter-to-participant ratio in mind and taken as preliminary evidence. The basic model testing our hypotheses showed good fit to the observed data, , p = 0.67, RMSEA = 0.000, and is presented in Fig. 2.
Fig. 2.
Path model of the relationships between stereotype endorsement, discrimination, and depression over time. N = 110. Non-significant paths are indicated by dashed lines. All other paths are significant at the 0.05 level
The findings from this model indicated that all of the cross-lagged paths between discrimination and distress were non-significant. This suggests that these two variables do not predict each other over time. The cross-lagged paths between stereotype endorsement and distress were also non-significant. Additionally, each variable had significant autoregressive effects from one time point to the next. The model accounted for 31% of the variance in stereotype endorsement at 12 months, 37% of the variance in discrimination at 12 months, and 69% of the variance in distress at 52 weeks.
To check for the possibility that amount of work was related to stigma, we performed simple correlations between hours of work and indices of stigma at each time point and found no significant correlations.
Discussion
In this study, we explored the extent to which the constructs of stereotype endorsement, discrimination, and psychological distress are stable over time and related to one another, both concurrently and across time. Results suggested three different things. First, the constructs of stereotype endorsement and discrimination experience are stable over periods of 5–7 months; however, as we look out over a span of 12 months, the most proximal scores, rather than the most distant, are the best predictors. Baseline scores were related to 5-month scores, and 5-month scores were related to 12-month scores, but we failed to find that baseline scores were related to 12-month scores. Second, the constructs of stereotype endorsement and discrimination experience are related to one another concurrently but analyses failed to detect a relationship over time. Third, while there were bivariate links between an index of psychological distress and discrimination experience, path analyses failed to find any significant links between these variables over time.
One interpretation suggested by these findings is that, over periods of months, internalized sigma is a stable phenomenon, which is distinct from related constructs such as discrimination experiences and psychological distress. In other words, while stereotype beliefs may be stronger among persons with current recollections of discrimination experiences, there was no evidence that previous levels of the recollection of discrimination experiences or of distressed mood played a causal role in later levels of stereotype endorsement. It is thus possible that, consistent with emerging models that suggest impoverished narratives may represent a potent barrier to recovery in schizophrenia [40], that the internalization of stigma may persist within a person’s storied account of who they are long after exposure to stigmatizing experiences. Stereotype endorsement could similarly not be accounted for by levels of emotional distress. While a failure to find significant relationships over the course of a year could reflect measurement issues or low power, results point to the possibility that stereotype endorsement may fluctuate in response to any number of changes in life circumstances.
Of note, these interpretations should be taken at present as speculative and as fodder for future research. Alternative interpretations cannot be ruled out. For one, there are many different factors not accounted for here, which might have influenced the course of the constructs we assessed, including experiences within and outside of rehabilitation. It is also possible that a failure to detect relationships was a function of difficulties with the measures employed.
There are limitations to this study. Generalization of findings is limited by sample composition. Participants were mostly males in their 40s who were involved in treatment. It may well be that a different relationship exists between discrimination experiences, stereotyped endorsement and psychological distress among females, or younger males with schizophrenia, or persons who decline treatment. Results may also not generalize to persons in an acute phase of disorder or to persons who do not enter rehabilitation (e.g. those who decline to engage in work in the wake of having little expectation of success due to internalized stigma). It is also possible the responses to the questionnaires were influenced by participants’ expectations of what the experimenters were looking for at baseline or their experiences at work following baseline. We also measured discrimination experiences as they might be reflected in overt behaviors and thus, our measure may not have been sensitive to more subtle forms of discrimination which occur when persons detect stigma in more subtle ways (e.g. via casual comments, facial expression or gestures). Further studies are needed which include a non-rehabilitation control group along with a larger number of assessments gathered across a greater span of time in order to shed more light on whether or not such a construct is stable over the course of a lifetime rather than just a year. Further study is also needed to explore differences among persons for whom stereotyped endorsement changed versus remained the same over time points. Finally, we explored discrimination experiences as a larger construct and it may be that there are certain experiences, which are more closely linked to self-stigma than others are. Qualitative work is needed to develop more finely tuned hypotheses regarding these issues.
In conclusion, with replication, there may be clinical implications to our findings. If stereotype endorsement is something that is stable in the short term but fluctuates over the long-term and is unrelated to discrimination experiences and distress, it may be that interventions are warranted which focus directly upon internalized stigma [41, 42]. It may be that interventions that aim to reduce psychological distress or help persons ward off stigmatizing experiences will not immediately affect how persons come to think about their own lives.
Acknowledgment
This research was funded by a grant from the VA Rehabilitation Research and Development Service.
Footnotes
Conflict of interest The authors have no conflict of interest to declare.
Contributor Information
Paul H. Lysaker, Email: plysaker@iupui.edu, Roudebush VA Medical Center, Day Hospital 116H, 1481 West 10th St, Indianapolis, IN 46202, USA; Department of Psychiatry, Indiana University School of Medicine, Indianapolis, IN 46202, USA.
Chloe Tunze, Department of Psychology, Indiana University Purdue University at Indianapolis, Indianapolis, IN, USA.
Philip T. Yanos, Psychology Department, John Jay College of Criminal Justice, CUNY, 445 W. 59th St., New York, NY 10019, USA
David Roe, Department of Community Mental Health, Faculty of Social Welfare and Health Science, University of Haifa, Haifa, Israel.
Jamie Ringer, Roudebush VA Medical Center, Day Hospital 116H, 1481 West 10th St, Indianapolis, IN 46202, USA; Department of Psychiatry, Indiana University School of Medicine, Indianapolis, IN 46202, USA.
Kevin Rand, Department of Psychology, Indiana University Purdue University at Indianapolis, Indianapolis, IN, USA.
References
- 1.Angermeyer MC, Matschinger H. The stigma of mental illness: effects of labeling on public attitudes towards people with mental disorder. Acta Psychiatr Scand. 2003;108:304–309. doi: 10.1034/j.1600-0447.2003.00150.x. [DOI] [PubMed] [Google Scholar]
- 2.Swindle R, Heller K, Pescosolido BA, Kikuzawa S. Responses to nervous breakdowns in America over a 40-year period: mental health policy implications. Am Psychol. 2000;55(7):740–749. doi: 10.1037//0003-066x.55.7.740. [DOI] [PubMed] [Google Scholar]
- 3.Markowitz FE. The effects of stigma on the psychological well-being and life satisfaction of persons with mental illness. J Health Soc Behav. 1998;39:335–347. [PubMed] [Google Scholar]
- 4.Phelan JC, Link BG, Stueve A, Pescosolido BA. Public conceptions of mental illness in 1950 and 1996: what is mental illness and is it to be feared? J Health Soc Behav. 2000;41(2):188–207. [Google Scholar]
- 5.Magliano L, Read J, Marassi R. Metaphoric and non-metaphoric use of the term “schizophrenia” in Italian newspapers. Soc Psychiatry Psychiatr Epidemiol. doi: 10.1007/s00127-010-0274-3. (in press) [DOI] [PubMed] [Google Scholar]
- 6.Link BG, Phelan JC. Conceptualizing stigma. Ann Rev Sociol. 2001;27(1):363. [Google Scholar]
- 7.Martin JK, Pescosolido BA, Tuch SA. Of fear and loathing: the role of disturbing behavior, labels and causal attributions in shaping public attitudes toward persons with mental illness. J Health Soc Behav. 2000;41(2):208–233. [Google Scholar]
- 8.Leiderman EA, Vazquez G, Berizzo C, Bonifacio A, Bruscoli N, Capria JI, Ehrenhaus B, Guerrero M, Guerrero M, Lolich M, Milev R. Public knowledge, beliefs and attitudes towards patients with schizophrenia: Buenos Aires. Soc Psychiatry Psychiatr Epidemiol. doi: 10.1007/s00127-010-0196-0. (in press) [DOI] [PubMed] [Google Scholar]
- 9.Cechnicki A, Angermeyer MC, Bielańska A. Anticipated and experienced stigma among people with schizophrenia: its nature and correlates. Soc Psychiatry Psychiatr Epidemiol. doi: 10.1007/s00127-010-0230-2. (in press) [DOI] [PubMed] [Google Scholar]
- 10.Link BG, Cullen F, Struening EL, Shrout PE, Dohrenwend BP. A modified labeling theory approach to mental disorders: an empirical assessment. Am Sociol Rev. 1989;54:400–423. [Google Scholar]
- 11.Link BG, Struening EL, Neese-Todd S, Asmussen S, Phelan JC. The consequences of stigma for the self-esteem of people with mental illness. Psychiatr Serv. 2001;52:1621–1626. doi: 10.1176/appi.ps.52.12.1621. [DOI] [PubMed] [Google Scholar]
- 12.Lally SJ. Does being in here mean there is something wrong with me? Schizophr Bull. 1989;15:253–265. doi: 10.1093/schbul/15.2.253. [DOI] [PubMed] [Google Scholar]
- 13.Ritsher JB, Otilingam PG, Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatr Res. 2003;121:31–49. doi: 10.1016/j.psychres.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 14.Warner R, Taylor D, Powers M, Hyman R. Acceptance of the mental illness label by psychotic patients: effects on functioning. Am J Orthopsychiat. 1989;59:389–409. doi: 10.1111/j.1939-0025.1989.tb01675.x. [DOI] [PubMed] [Google Scholar]
- 15.Wright ER, Gronfein WP, Owens TJ. Deinstitutionalization, social rejection and the self esteem of former mental patients. J Health Soc Behav. 2000;41:68–90. [PubMed] [Google Scholar]
- 16.Yanos PT, Roe D, Lysaker PH. The impact of illness identity on recovery from severe mental illness. Am J Psychiatric Rehabil. doi: 10.1080/15487761003756860. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Siris SG. Suicide and schizophrenia. J Psychopharmacol. 2001;15:127–135. doi: 10.1177/026988110101500209. [DOI] [PubMed] [Google Scholar]
- 18.Freudenreich O, Cather C, Evins AE, Henderson DC, Goff DC. Attitudes of schizophrenia outpatients towards psychiatric medications: relationship to clinical variables and insight. J Clin Psychiat. 2004;65(10):1372–1376. doi: 10.4088/jcp.v65n1012. [DOI] [PubMed] [Google Scholar]
- 19.Katschnig H. Schizophrenia and quality of life. Acta Psychiatr Scand. 2000;102:33–37. doi: 10.1034/j.1600-0447.2000.00006.x. [DOI] [PubMed] [Google Scholar]
- 20.Lloyd C, Sullivan PL, Williams D. Perceptions of social stigma and its effect on interpersonal relationships of young males who experience a psychotic disorder. Aust Occup Ther J. 2005;52(3):243–250. [Google Scholar]
- 21.Lysaker PH, Roe D, Yanos PT. Toward understanding the insight paradox: internalized stigma moderates the association between insight and social functioning, hope and self-Esteem among people with schizophrenia spectrum disorders. Schizophr Bull. 2007;33:192–199. doi: 10.1093/schbul/sbl016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rüsch N, Corrigan PW, Wassel A, et al. Self-stigma, group identification, perceived legitimacy of discrimination and mental health service use. Br J Psychiatry. 2009;195(6):551–552. doi: 10.1192/bjp.bp.109.067157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ertugrul A, Ulug B. Perception of stigma among patients with schizophrenia. Soc Psych Psych Epid. 2004;39(1):73–77. doi: 10.1007/s00127-004-0697-9. [DOI] [PubMed] [Google Scholar]
- 24.Lysaker PH, Davis LW, Warman DM, Strasburger A, Beattie N. Stigma, social function and symptoms in schizophrenia and schizoaffective disorder: associations across six months. Psychiatr Res. 2007;149:89–95. doi: 10.1016/j.psychres.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 25.Yanos PT, Roe D, Markus K, Lysaker PH. Pathways between internalized stigma and outcomes related to recovery in schizophrenia-spectrum disorders. Psychiatr Serv. 2008;59:1437–1442. doi: 10.1176/appi.ps.59.12.1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lysaker PH, Tsai J, Yanos P, Roe D. Associations of multiple domains of self-esteem with four dimensions of stigma in schizophrenia. Schizophr Res. 2008;98:194–200. doi: 10.1016/j.schres.2007.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yanos PT, Rosenfield S, Horwitz A. Negative and supportive social interactions and quality of life among persons diagnosed with severe mental illness. Community Mental Health J. 2001;37:405–419. doi: 10.1023/a:1017528029127. [DOI] [PubMed] [Google Scholar]
- 28.Dickerson FB, Sommerville J, Origoni AE, Ringel NB, Parente F. Experiences of stigma among outpatients with schizophrenia. Schizophr Bull. 2002;28:143–155. doi: 10.1093/oxfordjournals.schbul.a006917. [DOI] [PubMed] [Google Scholar]
- 29.Lundberg B, Hansson L, Wentz E, Björkman T. Are stigma experiences among persons with mental illness, related to perceptions of self-esteem, empowerment and sense of coherence? J Psychiatr Mental Health Nurs. 2009;16(6):516–522. doi: 10.1111/j.1365-2850.2009.01418.x. [DOI] [PubMed] [Google Scholar]
- 30.Lundberg B, Hansson L, Wentz E, Björkman T. Sociodemographic and clinical factors related to devaluation/discrimination and rejection experiences among users of mental health services. Soc Psychiatry Psychiatr Epidemiol. 2007;42(4):295–300. doi: 10.1007/s00127-007-0160-9. [DOI] [PubMed] [Google Scholar]
- 31.Spitzer R, Williams J, Gibbon M, First M. Biometrics Research. New York: 1994. Structured clinical interview for DSM IV. [Google Scholar]
- 32.Kay SR, Fizsbein A, Opler LA. The positive and negative syndrome scale for schizophrenia. Schizophr Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 33.Bell MD, Lysaker PH, Goulet JB, Milstein RM, Lindenmayer JP. Five-component model of schizophrenia: assessing the factorial invariance of the PANSS. Psychiatr Res. 1994;52:295–303. doi: 10.1016/0165-1781(94)90075-2. [DOI] [PubMed] [Google Scholar]
- 34.Davis L, Lysaker PH, Lancaster RS, Bryson GJ, Bell MD. The Indianapolis Vocational Intervention Program: a cognitive behavioral approach to addressing rehabilitation issues in schizophrenia. J Rehabil Res Dev. 2005;42:35–46. doi: 10.1682/jrrd.2003.05.0083. [DOI] [PubMed] [Google Scholar]
- 35.Jöreskog KG, Sörbom D. LISREL (Version 8.8) [Computer software] Chicago: Scientific Software International; 2006. [Google Scholar]
- 36.Keith TZ. Multiple regression and beyond. Boston: Allyn & Bacon; 2006. [Google Scholar]
- 37.Byrne BM. Structural equation modeling with LISREL, PRELIS, and SIMPLIS: Basic concepts, applications, and programming. Mahwah: Lawrence Erlbaum Associates; 1998. [Google Scholar]
- 38.Enders CK. The performance of the full information maximum likelihood estimator in multiple regression models with missing data. Educ Psychol Meas. 2001;61:713. [Google Scholar]
- 39.Kline RB. Principles and practice of structural equation modeling. 2nd edn. New York: Guilford Press; 1998. [Google Scholar]
- 40.Lysaker PH, Glynn SM, Wilkness SM, Silverstein SM. Psychotherapy and recovery from schizophrenia: a review of potential application and need for future study. Psychol Serv. 2010;7(2):75–91. doi: 10.1037/a0019115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roe D, Hasson-Ohayon I, Derhy O, Yanos PT, Lysaker PH. Talking about life and finding solutions to different hardships: a qualitative study on the impact of Narrative Enhancement and Cognitive Therapy on persons with serious mental illness. J Nerv Ment Dis. 2010;198(11):807–812. doi: 10.1097/NMD.0b013e3181f97c50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yanos PT, Roe D, Lysaker PH. Narrative enhancement and cognitive therapy: a new group-based treatment for internalized stigma among persons with severe mental illness. Group Psychother. doi: 10.1521/ijgp.2011.61.4.576. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]