Abstract
This study is a secondary analysis of data for 107 home health care heart failure patients. The authors investigate the impact of patient characteristics and nursing visit intensity on change in activities of daily living (ADL) status and instrumental activities of daily living (IADL) status and improvement/stabilization of dyspnea. Prior hospital stay (β = .38, p = .001) and nursing visit intensity (β = −.39, p = .001) predict improvement in ADL status. The model for change in IADL status is not significant. Patients with more than two comorbidities (OR = 6.5, p = .04) and patients who received higher nursing visit intensity (OR = 7.0, p = .04) are more likely to have improved/stabilized dyspnea at home care discharge.
Keywords: home health care, heart failure, nursing intensity, patient outcomes
Introduction
Demand for home health care services is increasing due in part to aging of the population and advances in medicine and technology that support provision of many health care services in patients’ homes (Bureau of Labor Statistics, 2006; Centers for Medicare & Medicaid Services [CMS], 2008). Skilled home health care is physician-directed health care services provided by licensed health care providers and supervised paraprofessionals to patients in their homes. Medicare is the payer for the majority of skilled home health care (National Association for Home Care & Hospice [NAHC], 2008); thus, skilled home health care is sometimes called Medicare home (health) care. Private insurance, governmental insurance plans and programs, and Medicaid may also be payers for skilled home health care services for enrollees who do not have Medicare insurance or who do not meet eligibility requirements for Medicare reimbursement of home health services. The Medicare home health benefit (CMS, 2005) requires that patients have a reasonable and necessary need for intermittent skilled nursing, physical therapy, or speech-language pathology services (or a continuing need for occupational therapy services). Patients must be under the care of a physician who establishes and approves a plan of care and patients must be homebound (unable to leave home without a considerable and taxing effort). Typically, eligibility requirements for skilled home health care services offered by other insurance providers are modeled on Medicare requirements, though there may be differences in terms of the type, scope, and duration of services offered.
Skilled home health care services are generally intended to fill a short-term patient need, for example, following acute illness or injury or exacerbation of an existing condition. Although some patients may remain continuously eligible for skilled home health care services over a long period of time, duration of care for the majority is 2 months or less (Madigan, 2008). Thus, skilled home health care services are distinct from the system of community-based long-term care services (CBLTCs) available to individuals and families in the community. Medicaid is the principal payer for CBLTCs that includes assistance provided by aides or attendants with activities of daily living (ADL), such as bathing, dressing, and toileting, or with instrumental activities of daily living (IADL), such as shopping, housework, or meal preparation. Services are aimed at keeping patients in their homes to avoid nursing home placement.
The majority (75%) of skilled home health care patients receive nursing services (National Center for Health Statistics [NCHS], 2004). Nursing services are delivered to patients in home visits. Nursing visit intensity is a measure of nursing service use, calculated as a ratio of total nursing visits to length of stay that accounts for large variations in duration of the home care stay among patients. Little research evidence exists about the relationship between skilled home care nursing visits, patient characteristics, and patient outcomes. Thus, home health care nurses and managers make decisions about the frequency and pattern of skilled nursing visits to provide on the basis of tradition and anecdote. Empirical evidence is needed to guide clinical practice and inform policy.
Heart failure (HF) is a high-cost, high-volume diagnosis in home health care where approximately 70% of current patients are elders (NCHS, 2004). Heart failure is a significant public health problem, affecting more than 5 million people with more than 550,000 new cases diagnosed each year at an estimated total health care system cost of US$33.2 billion (Rosamond et al., 2007). There is substantial research on hospitalized or community dwelling patients with HF (e.g., see reviews by Holland et al., 2005; McAlister, Stewart, Ferrua, & McMurray, 2004). Knowledge developed from this body of research provides little guidance for home health care nursing, however, since the management programs and interventions do not include skilled home health care services. As well, there is relatively little research on the processes of care within home health care for patients with HF. There are clinical recommendations and general practices within home health care focused on assessment of symptoms of HF exacerbation, extensive patient teaching on medication regimens, diet, and symptom recognition (Visiting Nurse Associations of America [VNAA], 2010). but these have not been evaluated with research. The most evidence on effective processes of care within home health care has been found with telehealth (Bensink, Hailey, & Wootton, 2007) and frontloading of visits (providing most home visits earlier in the episode of home health care; Rogers, Perlic, & Madigan, 2007).
Purpose
The purpose of this study was to investigate the relationship between patient characteristics, nursing visit intensity, and outcomes for skilled home health care patients with HF. The following research questions were asked:
Research Question 1
For skilled home health care patients with a primary diagnosis of HF, to what extent do patient predisposing, enabling and need characteristics predict change in ADL or IADL status, or improvement/stabilization of dyspnea?
Research Question 2
For these same patients, how is nursing visit intensity associated with change in ADL or IADL status, or improvement/stabilization of dyspnea, after accounting for patient predisposing, enabling, and need characteristics?
Theoretical Framework
Andersen’s (1995) behavioral model of utilization was the theoretical framework for the study, explaining patient outcomes in terms of patient characteristics and health service utilization (Figure 1). Variables for this study were selected from the existing literature to be consistent with the conceptual model and based on availability in the existing data set. Predisposing patient characteristics were age, gender, and race/ethnicity. The enabling resource was having Medicaid insurance in addition to Medicare. Need factors were severity of HF, number of comorbidities, and having a hospital stay in the 14 days prior to home care admission (prior hospital stay). The variable for health service use was skilled home health care nursing visit intensity. Patient outcome variables were change in ADL status, change in IADL status, and improvement or stabilization of dyspnea. Stabilization is defined as no change in status from admission to discharge.
Figure 1.
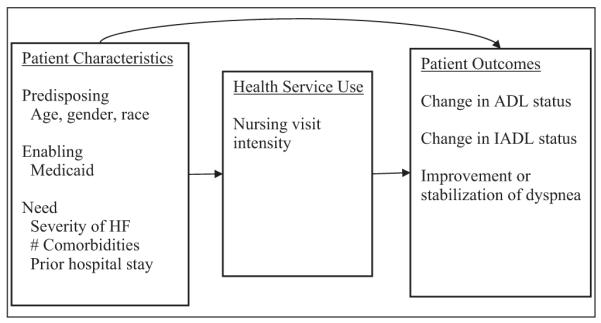
Andersen’s (1995) Behavioral Model of Utilization
Literature Review
Few studies have been conducted in the home health care setting to investigate the relationship between nursing service utilization and outcomes of patients with heart failure (HF). In early home care research more nursing visits were associated with fewer hospitalizations for one sample of home health care patients with HF (Dennis, Blue, Stahl, Benge, & Shaw, 1996), and more nursing time was associated with increased likelihood of home care HF patients achieving the clinical outcome of pacing activity to manage dyspnea (Adams & Short, 1997). Other studies examined home health care resource use more broadly. Fortinsky and Madigan (1997) identified similar amounts of home health care resource use for patients whether they were discharged from home care to the hospital or to self-care at home, whereas the length of home care stay for patients discharged to the hospital was about half as long. Using a different approach Fortinsky and colleagues (Fortinsky, Fenster, & Judge 2004) examined state data between 1995 and 1997 to identify risk factors associated with Medicare (skilled) and Medicaid home health care and Medicaid waiver service use. In this study patients with more ADL dependencies were more likely to have used Medicare home care versus Medicaid home care or Medicaid waiver services.
These studies provided preliminary knowledge about the relationships between skilled home health care service use and patient outcomes. The home health care industry, however, has always been sensitive to changes in the interpretation of eligibility and coverage guidelines for the Medicare home health benefit. These changes in interpretation have resulted in increases and decreases in home care service use in the 1980s and 1990s (Fishman, Penrod, & Vladeck, 2003; Liu, Gage, Harvell, Stevenson, & Brennan, 1999). More recently, the implementation in 2000 of the Prospective Payment System (PPS) for home care, a provision of the Balanced Budget Act of 1997, resulted in a reduction in the number of Medicare-certified home health agencies and also a decline in skilled home health care service use (Fishman et al., 2003; McCall, Petersons, Moore, & Korb, 2003). Research studies conducted prior to implementation of the PPS for home care cannot realistically be compared to studies conducted after PPS because the context of the industry is so different.
More recent home health care research that examines the relationship between home health care or nursing service use and patient outcomes is limited. In a retrospective record review aimed at identifying reasons for hospitalization, falls, or death occurring within 60 days of home health care referral, Taft and colleagues (Taft, Pierce, & Gallo, 2005) found no significant differences in numbers of home visits (all disciplines combined) for patients who experienced a fall compared to those who did not. Comparison of patients who were hospitalized with patients who died revealed that patients who died had significantly fewer home visits, a finding researchers concluded was associated with the shorter home care length of stay for patients who died. Rogers and colleagues (2007) found that a frontloaded nursing visit pattern was associated with fewer rehospitalizations in a sample of HF patients from one home health agency system, whereas no relationship between nursing service use and dyspnea was identified. Frontloading is providing more nursing visits early in the home care episode. The clinical pathway developed for the study was designed to provide increased frontloading and intensity for increased severity of HF. Patients who received frontloading did have significantly lower mean total visits, a lower mean length of stay, and lower mean visit intensity compared to patients who did not receive frontloading. Vanderboom and Madigan (2008) used a visits-per-patient measure derived from Medicare-cost reports dividing the total number of visits provided by all disciplines with the total number of patients seen in an analysis of the impact of home care agency characteristics and rurality on hospitalizations. For-profit agency ownership and larger agency size were positively associated with visits per patient, whereas hospital ownership and rurality had inverse associations. Visits per patient were also directly positively associated with hospitalization.
Findings of these studies have expanded our understanding of the relationship between home health care service use and patient outcomes, but approaches, measures for service use, and outcomes differ across studies, leaving gaps in our understanding. Research examining the relationship of home health care nursing service use to patient outcomes, aimed at identification of outcomes sensitive to nursing, remains very sparse. The present study begins to address this gap in the literature by examining the relationship between nursing visit intensity and patient outcomes.
Methods
Design and Sample
Data for this article were derived from a larger prospective cohort study that has been described elsewhere (Fortinsky, Madigan, Sheehan, Tullai-McGuinness, & Fenster, 2006). In the larger study, clinical data from OASIS forms were linked with visit data gathered by home health agency personnel over complete episodes of care, providing patient-level clinical assessment and utilization data. Ohio home health agency patients with a primary diagnosis of HF (ICD-9 428.0) were identified and extracted from the larger data set. This subset of patients (n = 107) comprised the sample for the present study.
Variables and Measures
The patient characteristics variables were derived from the OASIS clinical assessment data. Predisposing characteristics in the model were age, gender, and race/ethnicity. Only 11 patients in the sample were of any minority race/ethnicity; therefore, though the number is too small to analyze, a two-level (White, minority) variable was retained for descriptive purposes. The enabling variable was having Medicaid insurance, because availability of additional insurance might result in greater service utilization. However, only 4 patients in the study sample had Medicaid, too few for analysis or description. Thus, the variable for Medicaid was not retained in the analytic models. Need variables in this study were severity of HF, number of comorbidities, and whether the patient had a hospitalization in the 14 days prior to home care admission (labeled “prior hospital stay”). Severity of HF was measured with an OASIS item for diagnosis severity with responses ranging from 0 (asymptomatic, no treatment needed) to 4 (symptoms poorly controlled, history of rehospitalizations). The number of secondary diagnoses listed for each patient was summed for number of comorbidities; a maximum of five secondary conditions can be listed on the OASIS assessment. The OASIS item that identifies whether the patient had an inpatient hospital stay in the 14 days prior to home care admission was used to identify a prior hospital stay. Finally, a variable for the home health agency was included in the models as a covariate since patients in the sample were from 24 different agencies.
Home health agency staff provided visit-specific data used to construct the nursing intensity variable. The total number of visits was divided by the length of stay in days; the result was multiplied by 7 to produce a nursing visit intensity rate per week. Frequently, home health care research studies use the number of nursing visits as the measure for nursing services. However, as visits occur over varying time periods, this measure does not take into account the intensity of visits. Constructing a measure for intensity, therefore, adjusts for the wide variation in the home health length of stay. For multiple regression (change in ADL status, change in IADL status), a log transformation of the nursing intensity variable was performed to correct for nonnormality of the distribution, and the log of the nursing intensity was used in the analysis. For logistic regression (improvement/stabilization of dyspnea), there was no need to do a log transformation of the nursing intensity variable as normal distributions of independent variables are not an assumption of the statistical technique (Mertler & Vannatta, 2005). Because of the small increments of change for this independent variable the decision was made to dichotomize the variable so that the odds ratios would better reflect the differences in the probability of the outcome. The rationale for the split at 1.5 visits per week is based on the distribution of visits (where 62% were higher intensity) as well as clinical practice where 1.5 or fewer visits per week represents a lower intensity of service. There is, however, no existing research that indicates this cutpoint as better or worse than other cutpoints, and it is possible that other approaches (e.g., using quartiles) may be worthwhile to consider in future research.
Patient outcome variables were change in ADL status, change in IADL status, and improvement/stabilization of dyspnea. The OASIS assessment is conducted at admission to home care. A discharge assessment including the same items that were assessed at admission is conducted if the patient is discharged from home health care services to self-care (stays at home in the community). If a patient is discharged from home health care services because she or he has been admitted to a hospital or nursing home, or has died at home, an abbreviated discharge form is completed. Therefore, change scores can be constructed as outcome variables only for patients with a complete OASIS discharge assessment. Of the 107 patients in this sample, 77 had complete OASIS discharge assessments.
The OASIS assessment includes 14 items assessing functional status; 8 items were used to construct the measure for ADL status (grooming, bathing, toileting, dressing upper and lower body, transferring, ambulating, and eating), and 6 items were used to construct the measure for IADL status (preparing meals, doing housework, laundry, shopping, ability to use transportation, and the telephone). Scores for each item were summed to create a single ADL and IADL score, for both the admission and discharge OASIS assessments. Possible ranges were 0 to 28 for the ADL score and 0 to 23 for the IADL score, where zero is defined as completely independent with ADLs or IADLs and higher scores reflect increasing impairment. Change in ADL and IADL scores were constructed as continuous variables, calculated by subtracting the discharge from the admission score for each.
The outcome variable for dyspnea was derived from the OASIS item assessing severity of dyspnea on a scale from 0 (never short of breath) to 4 (short of breath at rest). The discharge assessment score was subtracted from the admission score to construct a change score for this outcome. Unlike the ADL and IADL outcomes, however, the dyspnea outcome could not be constructed as a continuous variable. The data distributions were sufficiently discrete to require creation of a dichotomous variable. Patients whose dyspnea improved or stayed the same from admission to discharge formed one group; patients whose dyspnea worsened from admission to discharge formed the second group.
Analysis
Data were explored with descriptive statistics, and bivariate correlations were used to examine the relationships between independent and outcome variables. Multiple regression was used to analyze the impact of patient characteristics and nursing intensity on the ADL and IADL outcomes, whereas logistic regression was used to analyze the dyspnea outcome.
Results
The skilled home health care patients with HF in this study sample were mostly White (87.9%) and female (62.6%) with an average age of 79 years (Table 1). More than three fourths (78.8%) had a prior hospital stay. Most (n = 94) scored a 2 or 3 on the 0 to 4 scale for severity of HF. Although 25% of the participants (n = 27) had dyspnea only when walking more than 20 feet or climbing stairs, more than 50% (n = 62) were assessed as having moderately severe dyspnea on admission to home care. The mean score for ADL status on admission was 5, however (possible range 0-28), and the mean IADL score on admission was 10 (possible range 0-23), indicating that these patients on admission to home care required more assistance with IADLs (e.g., laundry, housework, shopping) than with ADLs such as dressing, bathing, and toileting.
Table 1.
Sample Demographic and Clinical Characteristics at Home Care Admission
| Variable | Mean (SD) | Range (actual) | Frequency (%) |
|---|---|---|---|
| Patient age | 79 (9) | 45-97 | — |
| Gender (female) | — | — | 67 (62.6) |
| Race/ethnicity | — | — | |
| White | 94 (87.9) | ||
| Non-White | 11 (10.3) | ||
| Medicaid | — | — | 4 (3.7) |
| Prior hospital stay | — | 79 (78.8) | |
| Severity of heart failure (summary) | 2 (1) | 1-4 | |
| Severity of heart failure (detail) | — | — | |
| Symptoms well controlled | — | — | 5 (4.7) |
| Symptoms controlled with difficulty | — | — | 62 (57.9) |
| Needs frequent treatment adjustment | — | — | 32 (29.9) |
| Poorly controlled; history of rehospitalization | — | — | 8 (7.5) |
| Number of comorbidities (summary) | 2.7 (1.4) | 0-5 | |
| Number of comorbidities (detail) | |||
| 0 | — | — | 5 (4.7) |
| 1 | — | — | 22 (20.6) |
| 2 | — | — | 26 (24.3) |
| 3 | — | — | 20 (18.7) |
| 4 | — | — | 17 (15.9) |
| 5 | — | — | 17 (15.9) |
| Severity of dyspnea | |||
| Patient has no dyspnea | — | — | 10 (9.3) |
| When walking more than 20 feet, climbing stairs | — | — | 27 (25.2) |
| With moderate exertion (e.g., dressing, bathing) | — | — | 34 (31.8) |
| With minimal exertion (e.g., eating, conversing) | — | — | 28 (26.2) |
| At rest (day or night) | — | — | 8 (7.5) |
| Unadjusted ADL status score | 5 (4) | 0-21 | |
| Unadjusted IADL status score | 10 (4) | 2-19 |
Note: ADL = activities of daily living; IADL = instrumental activities of daily living.
Details of the sample’s service utilization are provided in Table 2. Mean duration of home care episode (length of home care stay) was 41 days (SD = 29.18, range = 2-135). Mean nursing intensity was 1.97 visits per week (median = 1.75, SD = 1.15), and the mean log of nursing intensity was 0.56 (SD = 0.5). When nursing intensity was dichotomized, more than half (62.6%, n = 67) of the patients received higher nursing intensity, whereas 37.4% (n = 40) received lower nursing intensity. The outcome variables change in ADL status and change in IADL status are illustrated in Table 3. The mean change in ADL was 1.3 (SD = 3.46). Only 18.2% of the sample had no change in ADL status between admission and discharge. The mean change in IADL status score was 2.01 (SD = 3.7). No change in IADL status between admission and discharge occurred for 16.9% of this sample. Dyspnea improved for 33 patients (42.9%) from admission to discharge (Table 4) and stayed the same for the same number, whereas it worsened for only 11 patients (13%).
Table 2.
Home Health Care Service Utilization of the Participants
| Variable | Mean (SD) | Range |
|---|---|---|
| Number of skilled nursing visits | 10 (7.07) | 0-35 |
| Length of stay (days) | 41 (29.18) | 2-135 |
| Nursing visit intensity | 1.96 (1.15) | 0-8.17 |
| Log of nursing visit intensity | 0.56 (.5) | −1.4-2.1 |
| Dichotomous nursing visit intensity variable | ||
| Lower nursing intensity = visits/week | — | 0-1.5 |
| Higher nursing intensity = visits/week | — | 1.51-8.17 |
Table 3.
Summary and Details of Change in ADL and IADL Status Outcome Variables
| Variable | Mean (SD) | Range | Frequency (%) |
|---|---|---|---|
| Change in ADL status | 1.3 (3.46) | −9.0-10 | — |
| Patients who improved |
— | — | 44 (57.1) |
| worsened | — | — | 19 (24.7) |
| stayed the same | — | — | 14 (18.2) |
| Change in IADL status |
2.0 (3.72) | −5.0-10 | — |
| Patients who improved |
— | — | 43 (55.8) |
| worsened | — | — | 21 (27.3) |
| stayed the same | — | — | 13 (16.9) |
Note: ADL = activities of daily living; IADL = instrumental activities of daily living.
Table 4.
Summary and Details of Improvement/Stabilization in Dyspnea Outcome Variable
| Variable | Mean (SD) | Range | Frequency (%) |
|---|---|---|---|
| Admission dyspnea score | 1.97 (1.1) | 0-4 | — |
| Discharge dyspnea score | 1.42 (1.1) | 0-4 | — |
| Patients who | — | — | |
| improved/stabilized | 66 (86%) | ||
| worsened | — | — | 11 (14%) |
Results
Bivariate Model
The bivariate correlations were examined between the independent variables (patient characteristics and nursing intensity) and change in ADL status. Only one of the patient characteristics variables—having a prior hospital stay—was significantly associated with change in ADL status (r = .31, p < .01). The nursing intensity variable was significantly correlated with change in ADL status (r = −.27, p = .01). Examination of bivariate correlations between the patient characteristics, nursing intensity variables, and improvement/stabilization in dyspnea revealed no significant associations. Of note, for both outcomes, there was an inverse correlation between age and having a prior hospital stay (r = −.21 and −.26, respectively).
Multivariate Model
Patient characteristics and nursing intensity explain 16.3% of the variance in change in ADL status (F = 2.81, p = .01, adj. R2 = .16). Patients who had a prior hospital stay are more likely to have improvement in ADL status (β = .38, p = .001), and patients who received lower nursing intensity are more likely to have improvement in ADL status (β = −.39, p = .001). The model analyzing impact of patient characteristics and nursing intensity on change in IADL status is not significant (p = .09). The model analyzing the impact of patient characteristics and nursing intensity on improvement/stabilization of dyspnea is significant (overall model χ2 = 0.03), and the model is a good fit for the data (Hosmer Lemeshow χ2 = .568; results not shown). Comorbidities, categorized as 2 or fewer and more than 2, is the only significant patient characteristic. Patients with more than two comorbidities are more likely than patients with two or fewer to have improved/stabilized dyspnea on discharge from home care (OR = 6.5, p = .04, 95% confidence interval [CI] = 1.04-40.6). Nursing intensity is also significant in this model. Patients who receive higher nursing intensity are more likely than patients who received lower nursing intensity to have improved/stabilized dyspnea on discharge (OR = 7.0, p = .04, 95% CI = 1.1-45.9). The model correctly classified patients whose dyspnea improved or stabilized 98.5% of the time, but correctly classified patients whose dyspnea worsened only 9.1% of the time.
Discussion
Findings of this study provide additional empirical support for Andersen’s behavioral model of utilization. Skilled home health care HF patient outcomes are influenced by nursing service use as well as patient characteristics. One of the challenges of using the Andersen model in research is its scope. Many studies, including the present study, test only a portion of the model rather than the entire framework. In the present study the relationship between patient characteristics and patient outcomes was tested (Figure 1), and the relationship between nursing visit intensity and patient outcomes was tested. The impact of each variable on the outcome was tested while controlling for all the other variables. This approach is one way to begin to explore the relationships that exist between patient characteristics, health service use, and outcomes. However, reciprocal relationships between patient characteristics and outcomes depicted in the model were not tested in this study. As acknowledged by Andersen in a review and update of the model (Andersen, 1995) more advanced analytic methods are necessary to test the complexity of the relationships suggested by the model, including potential interactions and endogeneity.
The multivariate results for change in ADL status were counterintuitive. A prior hospital stay was associated with more improvement in ADL status. Lower nursing intensity was also associated with more improvement in ADL status. There are several plausible explanations for these findings. First, functional status of older adults often declines during the course of hospitalization (Covinsky et al., 2003). Thus, those patients who had a prior hospital stay may have been more functionally impaired at the time of home health care admission but, consequently, gain more ability by home health care discharge. Alternatively, those patients without a hospital stay prior to home health care may have been functioning near or at their best, limiting the amount of improvement that was possible for them.
The lack of statistical significance for other independent variables in the model for change in ADL status was also surprising, particularly for age, severity of HF, and comorbidities. In other research, older age is associated with poorer functional status (Covinsky et al., 2003; Keepnews, Capitman, & Rosati, 2004) and with increased service use (Henton, Hays, Walker, & Atwood, 2002). Increasing severity of HF is associated with poorer outcomes (Hunt et al., 2005). Prevalence of multiple comorbidities is high among Medicare beneficiaries (Anderson & Horvath, 2004); chronic illness and co-occurrence of disease are associated with functional disability (Gijsen et al., 2001; Kriegsman, Deeg, & Stalman, 2004). The bivariate correlations between changes in ADL status, severity of HF, and number of comorbidities were negligible as well. These findings may be due to lack of variation within the study sample. Most of the patients (n = 94) had severity of HF scores of 2 or 3. Most of the patients in this sample (n = 68) have 1, 2, or 3 comorbidities. Thus, the lack of significance may reflect the limited number of comorbidities that could be included. In addition, the comorbidities were not classified as to their severity or the impact particular comorbid diagnoses have on required nursing care. For example, a comorbid diagnosis of mild osteoarthritis would not require the same level of nursing intensity as a comorbid diagnosis of moderate emphysema.
Consistent with past research with HF patients in home health care (Madigan, 2008), there was relatively little change in ADL and IADL status from home care admission to home care discharge. This may reflect, at least in part, the chronic and progressive nature of HF. Stabilization in status may be the optimal outcome for some patients, especially those with more severe disease. In addition, patients with HF receiving services in their homes generally require a certain level of functional ability to be able to remain at home. The patient must be able, with or without assistance, to safely transfer and ambulate back and forth to the bathroom, for example. The amount of improvement in functional ability that is possible in one episode of skilled home health care services is thus limited by the patient’s baseline function. In addition, one episode of skilled home health care services may not be a long enough to detect larger changes in patient functional status. When there were changes in functional status among patients in the present study, the changes were primarily positive: 57.1% showed improvement in ADL status, though the changes were modest in magnitude (1.3 unit change on average on a 20-point scale).
Findings of this study add to our understanding of the relationship between skilled home health care nursing service use and change in dyspnea from home care admission to discharge. Patients in this study who received higher nursing visit intensity were 7 times more likely to have improved or stabilized dyspnea, compared to patients who received lower nursing visit intensity. Improvements or stabilization in dyspnea associated with higher nursing visit intensity likely reflect the improvement and stabilization of the patient’s overall cardiac status. Worsening of the patient’s clinical condition, or onset of complications, would likely be the cause for rehospitalization of the patient rather than continuation of home care services. In one study of home health care patients with various primary diagnoses, severity of dyspnea was identified as a significant predictor of ending the home care episode with hospitalization (Fortinsky et al., 2006). Findings of the present study suggest that higher nursing visit intensity may contribute to improvement in the clinical condition of home health care patients with HF, averting or delaying hospitalization. Additional research is needed to confirm these findings for HF patients and to explore whether symptoms associated with other conditions are also sensitive to nursing visit intensity.
Further research is also needed to identify the most useful measure for home health care nursing service use. Although nursing visit intensity was significantly associated with ADL status and dyspnea in the present study, this measure may not be useful for detection of impact on other outcomes, such as hospitalization or medication adherence. For example, Rogers and colleagues (2007) did not identify an impact of frontloading nursing visits on the outcome of dyspnea for home health care patients with HF, though frontloading was associated with fewer rehospitalizations. Ideally, a measure can be identified and used in research that will detect the impact of skilled home health care nursing services on all outcomes of interest.
The type of nursing interventions provided to home care patients includes assessment of health status with resultant treatment or communication with other team members (physician, physical therapist, social worker, etc.). Also provided are treatments that the patient is not able to manage for him or herself. A particular focus of skilled home health care nursing is patient (and/or caregiver, when applicable) teaching for management of disease, medications, symptoms, ADLs, and IADLs. Higher nursing visit intensity is a response to instability of the patient’s condition, and/or inability to effectively and safely manage their condition and self-care activities between nursing visits. For example, a patient with HF who is receiving high nursing visit intensity is likely to be experiencing unstable cardiac status, including moderate or severe dyspnea, requiring frequent nursing assessment, coordination with the patient’s physician for medication changes, and follow-up evaluation of response to treatment. Other patient needs requiring high nursing visit intensity include problems with adherence to medications and symptom management and response. Patients often require more frequent and direct assistance from nurses with medications and symptom management, for example, when their condition is unstable because they are unable to manage independently. As their condition improves, patients are able to resume more independent management of their care. In addition, patient’s and/or caregiver’s acquisition of skill in self-management grows with ongoing teaching and coaching from nurses. More indepth teaching and coaching is provided at the beginning of the home care episode and tapers off as patients and care-givers demonstrate increased ability for safe and effective self-management.
Instrumental activities of daily living (IADLs) include shopping, housework, and meal preparation. Although these activities are important for general functioning at home, they may be less informative in home health care research. In this study, patient characteristics and nursing intensity do not significantly explain change in IADL status. Although about half (n = 43, 55.8%) of the patients improved between home care admission and discharge, the amount of improvement is not large. The lack of significant findings and very modest improvement between admission and discharge may be explained by a nursing visit focus on stabilization of cardiac status and recovery of baseline functional status rather than on patient management of IADLs, particularly since many patients receive assistance from family to complete these activities.
There are a number of limitations to this study. First, the calculation of a change score for functional status required measurement of functional status on admission and discharge. Thus, patients whose episodes of care ended with a hospital stay were not included in the present study, limiting the generalizability of the results to those who were the most likely to improve. Second, the data were collected between 1999 and 2001, during the implementation of the prospective payment system—an important period in home health care. Thus, the results may reflect the responses of the agencies to the payment changes. Whether the same results would be found presently is unknown. Finally, as OASIS data are collected primarily for clinical care purposes, the reliability and validity of the data may be questioned. However, researchers have found OASIS reliability and validity to be sufficient, particularly for ADL and IADL measures (Hittle et al., 2003; Madigan & Fortinsky, 2001; Tullai-McGuinness, Madigan, & Fortinsky, 2009). Research using OASIS data has also been limited by the lack of process of care items in the OASIS data set. Beginning January 1, 2010, however, the most recent revision of OASIS was implemented—OASIS-C. This new version of OASIS does include process of care items; therefore, future home health care research that uses OASIS data will be able to include variables for process of care.
Conclusion
Home health care for patients with heart failure is generally successful: Substantial numbers of patients stabilize or improve in functional and symptom status. The relationships identified between nursing visit intensity and functional status improvement, and nursing visit intensity and dyspnea, indicate that there is more to learn about optimal strategies for provision of home health care nursing services. Future studies should further explore the relationship between home health care nursing service use and patient outcomes as well as examine processes of care that are most effective for management of home health care patients with heart failure.
Acknowledgments
Funding
The author(s) received the following financial support for the research, authorship, and/or publication of this article: This project was supported in part by National Institute of Nursing Research grant RO1 NR005081, Principal Investigator: Richard H. Fortinsky, PhD.
Bios
Jennifer S. Riggs, PhD, RN, is an assistant professor, West Virginia University School of Nursing in Morgantown West Virginia.
Elizabeth A. Madigan, PhD, RN, FAAN, is a professor at the Frances Payne Bolton School of Nursing, Case Western Reserve University in Cleveland, Ohio.
Richard H. Fortinsky, PhD, is a professor of medicine, Physicians Health Services Endowed Chair in Geriatrics and Gerontology Center on Aging, University of Connecticut Health Center in Farmington, Connecticut.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Adams CE, Short R. Registered nurse use and patient outcomes in home health. In: Adams CE, Anthony AL, editors. Home health outcomes and resource utilization: Integrating today’s critical priorities. National League for Nursing; New York, NY: 1997. pp. 51–62. [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36(1):1–10. [PubMed] [Google Scholar]
- Anderson G, Horvath J. The growing burden of chronic disease in America. Public Health Reports. 2004;119(3):263–270. doi: 10.1016/j.phr.2004.04.005. doi: 10.1016/j.phr.2004.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bensink M, Hailey D, Wootton R. A systematic review of successes and failures in home telehealth. Part 2: final quality rating results. Journal of Telemedicine and Telecare. 2007;13(Suppl. 3):10–14. doi: 10.1258/135763307783247121. [Google Scholar]
- Bureau of Labor Statistics . Occupational Outlook Quarterly Online, Spring 2006. 1. Vol. 50. U.S. Department of Labor; Washington, DC: 2006. The 2004-14 job outlook: Table of occupations. Retrieved from http://www.bls.gov/opub/ooq/2006/spring/table.pdf. [Google Scholar]
- Centers for Medicare & Medicaid Services . Medicare benefit policy manual: Chapter 7—Home health services. 2005. Retrieved from http://www.cms.gov/manuals/Downloads/bp102c07.pdf. [Google Scholar]
- Centers for Medicare & Medicaid Services . National health expenditures projections: 2007-2017: Forecast summary. 2008. Retrieved from http://www.cms.hhs.gov/NationalHealthExpendData/Downloads/proj2007.pdf. [Google Scholar]
- Covinsky KE, Palmer RM, Fortinsky RH, Counsell SR, Stewart AL, Kresevic D, Landefeld CS. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: Increased vulnerability with age. Journal of the American Geriatrics Society. 2003;51(4):451–458. doi: 10.1046/j.1532-5415.2003.51152.x. doi: 10.1046/j.1532-5415.2003.51152.x. [DOI] [PubMed] [Google Scholar]
- Dennis LI, Blue CL, Stahl SM, Benge ME, Shaw CJ. The relationship between hospital readmissions of Medicare beneficiaries with chronic illnesses and home care nursing interventions. Home Healthcare Nurse. 1996;14(4):303–309. [PubMed] [Google Scholar]
- Fishman EZ, Penrod JD, Vladeck BC. Medicare home health utilization in context. Health Services Research. 2003;38(1, Part 1):107–112. doi: 10.1111/1475-6773.00107. doi: 10.1111/1475-6773.00107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortinsky RH, Fenster JR, Judge JO. Medicare and Medicaid home health and Medicaid waiver services for dually eligible older adults: Risk factors for use and correlates of expenditures. Gerontologist. 2004;44(6):739–749. doi: 10.1093/geront/44.6.739. doi: 10.1093/geront/44.6.739. [DOI] [PubMed] [Google Scholar]
- Fortinsky RH, Madigan EA. Home care resource consumption and patient outcomes: What are the relationships? Home Health Care Services Quarterly. 1997;16(3):55–73. doi: 10.1300/J027v16n03_05. 10.1300/J027v16n03_05. [DOI] [PubMed] [Google Scholar]
- Fortinsky RH, Madigan EA, Sheehan TJ, Tullai-McGuinness S, Fenster JR. Risk factors for hospitalization among Medicare home care patients. Western Journal of Nursing Research. 2006;28(8):902–917. doi: 10.1177/0193945906286810. 10.1177/0193945906286810. [DOI] [PubMed] [Google Scholar]
- Gijsen R, Hoeymans N, Schellevis FG, Ruwaard D, Satariano WA, van den Bos GA. Causes and consequences of comorbidity: A review. Journal of Clinical Epidemiology. 2001;54(7):661–674. doi: 10.1016/s0895-4356(00)00363-2. doi:10.1016/S0895-4356(00)00363-2. [DOI] [PubMed] [Google Scholar]
- Henton FE, Hays BJ, Walker SN, Atwood JR. Determinants of Medicare home healthcare service use among Medicare recipients. Nursing Research. 2002;51(6):355–362. doi: 10.1097/00006199-200211000-00003. [DOI] [PubMed] [Google Scholar]
- Hittle DF, Shaughnessy PW, Crisler KS, Powell MC, Richard AA, Conway KS, Engle K, et al. A study of reliability and burden of home health assessment using OASIS. Home Health Care Services Quarterly. 2003;22(4):43–63. 10.1300/J027v22n04_03. [PubMed] [Google Scholar]
- Holland R, Battersby J, Harvey I, Lenaghan E, Smith J, Hay L. Systematic review of multidisciplinary interventions in heart failure. Heart. 2005;91(7):899–906. doi: 10.1136/hrt.2004.048389. doi: 10.1136/hrt.2004.048389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Riegel B, et al. ACC/AHA 2005 Guideline update for the diagnosis and management of chronic heart failure in the adult. Circulation. 2005;112(12):1825–1852. doi: 10.1161/CIRCULATIONAHA.105.167586. doi: 10.1161/CIRCULATIONAHA.105.167587. [DOI] [PubMed] [Google Scholar]
- Keepnews D, Capitman JA, Rosati RJ. Measuring patient-level clinical outcomes of home health care. Journal of Nursing Scholarship. 2004;36(1):79–85. doi: 10.1111/j.1547-5069.2004.04017.x. doi: 10.1111/j.1547-5069.2004.04017.x. [DOI] [PubMed] [Google Scholar]
- Kriegsman DM, Deeg DJ, Stalman WA. Comorbidity of somatic chronic diseases and decline in physical functioning: The Longitudinal Aging Study Amsterdam. Journal of Clinical Epidemiology. 2004;57(1):55–65. doi: 10.1016/S0895-4356(03)00258-0. doi: 10.1016/S0895-4356(03)00258-0. [DOI] [PubMed] [Google Scholar]
- Liu K, Gage B, Harvell J, Stevenson D, Brennan N. Medicare’s post-acute care benefit: Background, trends, and issues to be faced. Urban Institute & U.S. Department of Health & Human Services; Washington, DC: 1999. Retrieved from http://aspe.hhs.gov/daltcp/reports/mpacb.htm. [Google Scholar]
- Madigan EA. People with heart failure and home health care resource use and outcomes. Journal of Clinical Nursing. 2008;17(7B):253–259. doi: 10.1111/j.1365-2702.2008.02334.x. doi: 10.1111/j.1365-2702.2008.02334.x. [DOI] [PubMed] [Google Scholar]
- Madigan EA, Fortinsky RH. Additional psychometric evaluation of the Outcomes and Assessment Information Set (OASIS) Home Health Care Services Quarterly. 2001;18(4):49–62. doi: 10.1300/j027v18n04_02. doi: 10.1300/J027v18n04_02. [DOI] [PubMed] [Google Scholar]
- McAlister FA, Stewart S, Ferrua S, McMurray JJJV. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: A systematic review of randomized trials. Journal of the American College of Cardiology. 2004;44(4):810–819. doi: 10.1016/j.jacc.2004.05.055. doi: 10.1016/j.jacc.2004.05.055. [DOI] [PubMed] [Google Scholar]
- McCall N, Petersons A, Moore S, Korb J. Utilization of home health services before and after the Balanced Budget Act of 1997: What were the initial effects? Health Services Research. 2003;38(1, Part 1):85–106. doi: 10.1111/1475-6773.00106. doi: 10.1111/1475-6773.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertler CA, Vannatta RA. Advanced and multivariate statistical methods. 3rd ed. Pyrczak Publishing; Glendale, CA: 2005. [Google Scholar]
- National Association for Home Care & Hospice . Basic statistics about home care: Updated 2008. Author; Washington, DC: 2008. Retrieved from http://www.nahc.org/facts/08HC_stats.pdf. [Google Scholar]
- National Center for Health Statistics . National home and hospice care survey: Data highlights: Home care current patients 2000. Centers for Disease Control & Prevention; Hyattsville, MD: 2004. [Google Scholar]
- Rogers J, Perlic M, Madigan EA. The effect of frontloading visits on patient outcomes. Home Healthcare Nurse. 2007;25(2):103–109. doi: 10.1097/00004045-200702000-00011. [DOI] [PubMed] [Google Scholar]
- Rosamond W, Flegal K, Friday G, Furie K, Go A, Greenlund K, Hong Y, et al. Heart disease and stroke statistics—2007 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115(5):69–17. doi: 10.1161/CIRCULATIONAHA.106.179918. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- Taft SH, Pierce CA, Gallo CL. From hospital to home and back again: A study in hospital admissions and deaths for home care patients. Home Health Care Management & Practice. 2005;17(6):467–480. doi: 10.1177/1084822305278129. [Google Scholar]
- Tullai-McGuinness S, Madigan EA, Fortinsky RH. Validity testing the Outcomes and Assessment Information Set (OASIS) Home Health Care Services Quarterly. 2009;28(1):45–57. doi: 10.1080/01621420802716206. doi: 10.1080/01621420802716206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanderboom CP, Madigan EA. Relationships of rurality, home health care use, and outcomes. Western Journal of Nursing Research. 2008;30(3):365–378. doi: 10.1177/0193945907303107. doi: 10.1177/0193945907303107. [DOI] [PubMed] [Google Scholar]
- Visiting Nurse Associations of America . VNAA Chronic Care Clearinghouse. 2010. web site: Heart failure pages. Retrieved from http://chronicconditions.org/ClearingHouse/cat/HeartFailure,61.aspx. [Google Scholar]


