Abstract
Morehouse School of Medicine chose to restructure its first year medical curriculum in 2005. The anatomy faculty had prior experience in integrating courses, stemming from the successful integration of individual anatomical sciences courses into a single course called Human Morphology. The integration process was expanded to include the other first year basic science courses (Biochemistry, Physiology, and Neurobiology) as we progressed toward an integrated curriculum. A team, consisting of the course directors, a curriculum coordinator and the Associate Dean for Educational and Faculty Affairs, was assembled to build the new curriculum. For the initial phase, the original course titles were retained but the lecture order was reorganized around the Human Morphology topic sequence. The material from all four courses was organized into four sequential units. Other curricular changes included placing laboratories and lectures more consistently in the daily routine, reducing lecture time from 120 to 90 minute blocks, eliminating unnecessary duplication of content, and increasing the amount of independent study time. Examinations were constructed to include questions from all courses on a single test, reducing the number of examination days in each block from three to one. The entire restructuring process took two years to complete, and the revised curriculum was implemented for the students entering in 2007. The outcomes of the restructured curriculum include a reduction in the number of contact hours by 28%, higher or equivalent subject examination average scores, enhanced student satisfaction, and a first year curriculum team better prepared to move forward with future integration.
Keywords: medical curriculum, course integration, curriculum restructure, medical anatomy gross anatomy education
INTRODUCTION
Traditionally, medical school curricula are organized around a fundamental design plan in which two years of mainly basic sciences are followed by two years of clinical rotations. In this model, the basic science curriculum is typically discipline-based and composed of independent courses such as gross anatomy, embryology, neurobiology, cell biology/histology, physiology, biochemistry, microbiology, pharmacology, and pathology. However, the effectiveness of this traditional approach has been questioned in recent years, resulting in a call for integration of the basic sciences with each other and with the clinical sciences in a new paradigm for medical education (Cooke et al., 2010). The need to evaluate medical education programs and implement curriculum changes has also been recognized outside the United States in Italy (Snelgrove et al., 2009), Korea (Kim and Kee, 2010), Sweden (Edgren et al., 2010), and Japan (Rao and Rao, 2009). Several issues may account for this world-wide movement in education such as the rapid and large-scale expansion of medical science knowledge, recent changes in medical practice associated with technological advances, health-care funding issues, and new health problems that have emerged (Leung et al., 2006).
Morehouse School of Medicine (MSM) was founded as a historically black institution in 1975. It is a private institution that specializes in training people of color and those individuals from under privileged backgrounds to address the healthcare needs of underserved populations. It excels in educating primary care physicians, meeting social mission (McCurdy et al., 1997; Mullan et al., 2010; Schofield and Bourgeois, 2010), and providing exceptional, culturally sensitive, patient care (Briggs and McBeath, 2010). The institution is dedicated to improving the health and well-being of individuals and communities; increasing the diversity of the health professional and scientific workforce; and addressing primary health care needs through programs in education, research, and service with emphasis on people of color and the underserved urban and rural populations. Each medical school class includes approximately 54 students.
Following a regular accreditation-renewal site visit in 2005, the Liaison Committee for Medical Education (LCME, 2011) suggested that MSM restructure its first year curriculum. At that time, our curriculum involved more lecture contact hours than the national average. Our curriculum was similar to most medical schools in the US in that it was departmentally based with little integration across disciplines (Drake, 1998). In addition, there was little cross-talk between departments or teaching faculty. The LCME advised MSM to move to a more centrally controlled curriculum and to reduce the number of classroom contact hours. The methods for achieving these goals were left to the institution.
The institutional Curriculum Committee and the Associate Dean for Educational and Faculty Affairs complied with the LCME finding, and approximately six months after the report was issued, they agreed to a basic restructuring plan. At other institutions this process has involved hiring new deans to participate in, and oversee, the reform process (Loeser et. al., 2007; O'Connor Grochowski et al., 2007), appointing a curriculum committee from within the faculty to do the work (Rao and Rao, 2007), or having a committee not involved in the process to evaluate the final plans (Hollander et al., 2002). Our overall process included neither changes in administrative personnel nor an external evaluation committee. All re-organization, planning, and implementation were the responsibility of faculty members already involved in the first year courses.
Transitioning from a discipline-based curriculum to an integrated format presents many conceptual and logistical challenges that may be best addressed and incorporated gradually over an extended period (Klement et al., 2008, 2010). There are different attitudes toward, and methods of, curriculum reform but the approach selected must address the institution's specific needs and cultural idiosyncrasies (Simunovic et al., 2007).
The long-term goal of our project is to move from a discipline-based, to an integrated, first-year medical curriculum. We recognized early on that to reach a fully integrated curriculum, changes at our institution would have to be accomplished in a step-wise fashion. This paper documents our experiences with the first phase of this process in which the traditional courses remained intact, but the course organization and schedule of topic presentation were changed to align course content. This experience and process offer a template that other institutions may find helpful as they embark on their own curriculum revision. The goals of the first phase in this restructuring project were to: (1) reduce unnecessary redundancy between courses, (2) reduce the number of lecture hours, (3) increase the time available for self-directed learning, (4) provide less-compartmentalized teaching and testing strategies, and (5) promote inter-topic integration to model the increasingly integrative nature of the Step 1 of the United States Medical Licensing Examination (USMLE).
We are making select modifications for each academic year. In this first phase of a stepwise approach to integration, we have rescheduled the content of existing courses and redeployed them around the regional dissection and the associated systems-based histology content. Future phases will involve further cross-course integration of individual subjects. There are many secondary outcomes resulting from curriculum change such as the impact on faculty time and productivity, student well-being, and the benefit to students in subsequent years of medical school. Here, however, we are reporting only the steps taken to achieve the first phase of the curriculum and the immediate and direct outcomes.
GETTING STARTED
The rationale for the restructuring was to: (1) follow the LCME recommendations, (2) build on the previous success of our Human Morphology (anatomical sciences) course in integrating systems and regional approaches to curriculum organization (Wineski and Paulsen, 2005; Klement et al., 2008, 2010), and (3) promote integration of basic science concepts for USMLE preparation (Zhang et al., 2004; Fincher et al., 2009; Lieberman at al., 2010). This first phase of curriculum restructuring took two years to design, plan, and implement (Fig. 1). Several administrative issues had to be addressed, including expected faculty resistance to curricular change and to removing control of course content and implementation from the academic departments. Many discussions were needed during the first year among departments, course directors, and individual faculty to build agreement by all parties that curriculum restructuring was needed, feasible, and would provide a better education for the students. Once there was general agreement to proceed with planning, another year was needed to determine how best to proceed, to organize the order of content delivery in lectures and laboratories, and to establish curriculum administrative and oversight responsibilities.
Figure 1.
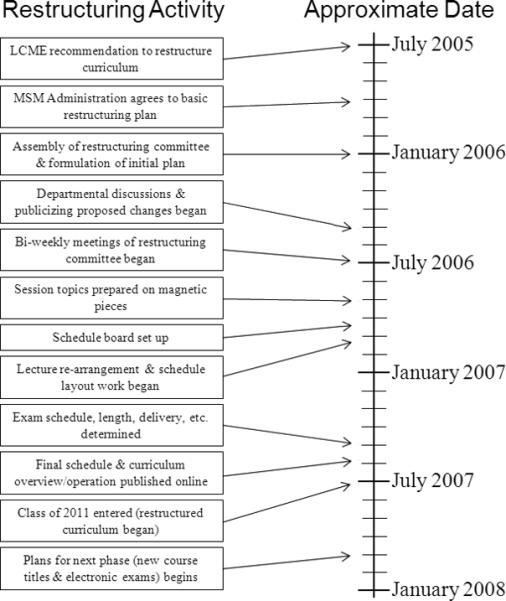
Timeline for preparing the first phase in curriculum restructure. The events for restructuring the curriculum were initiated in 2005 and put into place with the entering class in 2007. The major activities that contributed to the development of the restructured curriculum within these two years are noted.
The MSM first-year curriculum focuses on clinically relevant normal human biology. The basic science courses included here are Human Morphology, Biochemistry, Physiology, and Neurobiology. Disease mechanisms are covered during the second-year curriculum, which includes Pathology, Pathophysiology, Microbiology and Immunology, Nutrition, and Pharmacology. The Curriculum Committee felt it was prudent to focus first on integrating the first-year curriculum in order to gain experience with the process and outcome before considering wholesale restructuring of the entire preclinical curriculum.
Two of the first-year course directors had prior experience with course integration, providing a successful history on which to base the overall curriculum integration. The Human Morphology course was developed in the early 1990's as an integration of individual anatomical science courses. The Histology, Cell Biology, Gross Anatomy, and Embryology courses were integrated into a single course that had the Gross Anatomy regional dissection schedule as its backbone. Affording students the opportunity to complete a full dissection of the body is incompatible with a systems approach to dissection. Human Morphology had been very well received by both faculty and students and had been refined over the years based on both student and faculty input. The experience of melding these individual anatomical science courses into an integrated progression was an important first step in integrating the entire first year curriculum at MSM.
The anatomy dissection sequence that evolved during the development of Human Morphology provided a proven basis for successful integration. This sequence is not unlike that for stand-alone gross anatomy courses at many medical schools. Dissection begins with the back, then proceeds through the upper extremities, thorax, abdomen, pelvis and perineum, lower extremities, and concludes with the head and neck. The placement of the back at the beginning of the dissection schedule and head and neck at the end reflects the relative difficulty of the dissection of these regions and the desire for close proximity in the schedule between covering head and neck anatomy and the Neurobiology course. Human Morphology's success in integrating regional dissection in Gross Anatomy with the more-traditional, systems-based approach in Histology allowed us to build on the strengths of an existing order of presentation in the restructuring. The unique feature of our new curriculum is basing the integrated curriculum on a regional dissection of the body, rather than on the systems-based approach being used by most medical schools attempting integration. The entire curriculum is now organized around the systems concentrated in the various regions of the human body. A significant, but unforeseen, benefit of this approach, at least from the perspective of the clinicians who participate in the course, is that it mirrors in many ways the approach taken during physical examinations.
The first-year curriculum revision included four courses: Human Morphology, Biochemistry, Physiology, and Neurobiology, each with a different number of course credits (Table 1). Human Morphology was the largest course in the curriculum. During the restructuring process, the courses were disassembled, modified, and then reassembled. The lectures and laboratories of each course were rearranged so that the subject matter of all courses was aligned. When reassembling them, the Human Morphology course was used as the foundation. The end result of this first restructuring phase is that the course content from all four courses is organized around both a regional cadaver dissection and the body's organ systems. At the end of the academic year, students received a separate grade for each course.
Table 1.
Courses included in the restructuring process and the faculty involved.
| Courses | Credit hours | Faculty position involved | Role in restructuring |
|---|---|---|---|
| Human Morphology (HM) | 14 | Course Directors (2) | Maintenance of dissection schedule, topic expertise, knowledge of topic order |
| Biochemistry | 8 | Course Directors (2) | Alignment of Biochemistry topics with HM |
| Physiology | 10 | Course Directors (2) | Alignment of Physiology topics with HM |
| Neurobiology | 7 | Course Director (1) | Alignment of Neurobiology topics with HM head and neck topics |
| Administrative Participants | Curriculum Coordinator | Coordinated faculty meetings and schedule preparation sessions Updated and maintained schedule/calendar during development | |
| Associate Dean for Educational and Faculty Affairs | Oversight of entire process | ||
MECHANICS OF RESTRUCTURING
The first step in the restructuring process was to assemble a committee of willing and competent individuals to actually build the curriculum. The course directors of the existing independent courses were the obvious choice because they were most knowledgeable about their respective courses. In addition, a second key faculty member from each course, often a course co-director, was included to provide additional insights and to assure continuity in the meeting process during times when one or more course directors were unavailable. Another faculty member, who was not a course director, was also needed to coordinate meetings, record decisions, and maintain the curriculum schedule as it evolved. This role was designated as the Curriculum Coordinator. The Associate Dean for Educational and Faculty Affairs played a key role in answering questions from an administrative perspective and guiding the process. The final committee consisted of nine faculty members (Table 1), with consultations with other teaching faculty as needed. The faculty roles in restructuring included topic expertise and alignment of topics with the dissection order as well as administrative functions. The Human Morphology course directors were key players in maintaining the order of topic presentation and helped coordinate the efforts of other courses in aligning their subject matter around these topics.
To track the individual lectures and the order in which they would be presented, a schedule board was created. The topic and instructor's name for each individual lecture and laboratory session were printed on a small piece of paper with a magnet glued to the back. All sessions from each course were represented by a unique identifying color (Fig. 2A). These lecture pieces were placed onto a large, magnetic, dry-erase board where they could be easily rearranged (Fig. 2B). The lectures and laboratories could then be grouped by topic and a week-by-week schedule laid out. Because the pieces were so easy to move, lecture sessions could be rearranged quickly until the best order was achieved. At the weekly curriculum meetings, different faculty worked the board to experiment with ideas and instantly illustrate them for the others present. The result was an interactive and collaborative process that enhanced rapport and participation, and accelerated progress. Beginning with all the original lectures from the various courses was an important step in assuring the course directors that their material would be covered. The schedule formulated on the board was then recorded in an electronic spreadsheet file with color-coded cells containing the lecture title and instructor, and laboratory topics (Fig. 3). The schedule was then distributed electronically to faculty and students at the beginning of the academic year with updates and modifications occasionally sent out during the year.
Figure 2.
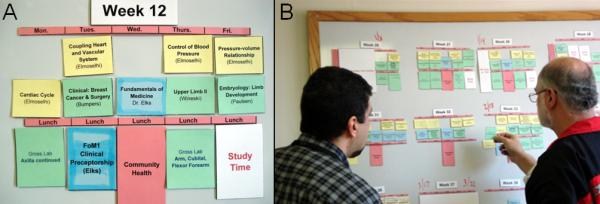
Organization of lecture and laboratory topics by subject throughout the year. Each lecture and laboratory session title and instructor name were printed on colored squares of paper. A different color was used for each course (e.g., green = Human Morphology, light blue = Biochemistry, yellow = Physiology). A magnet was affixed to the back of each square. The squares with the lecture titles were placed on a magnetic white board according to the day of the week and the time of day. Panel (A) shows a draft of topic order in a representative week using the colored squares on the white board. The colored topic squares could be easily rearranged and placed in different locations during drafting of the schedule. Panel (B) shows how members of the curriculum development team worked together at the white board to arrange the order and placement of topics.
Figure 3.
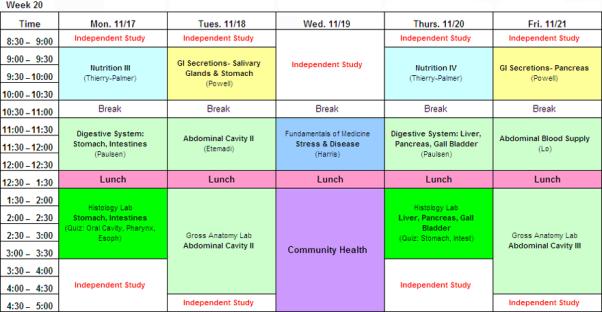
An example of schedule for one week in the curriculum. After the topic order was arranged on the white board, it was entered into an Excel spreadsheet with similar course color representations. The electronic version was e-mailed to members of the team during the drafting process and the final version was communicated to faculty and students. In the restructured curriculum, lectures are typically held in the morning and active learning sessions (laboratories) are held in the afternoon.
The frequent (usually weekly) curriculum meetings and the enhanced interactions between course directors led to informative discussions on lecture content and topic coverage. Another key goal of the restructuring was to reduce the number of contact hours and thereby free-up additional time for self-directed study. Identification of material covered by multiple faculty members helped to streamline lecture content. In some cases, off-line meetings among faculty covering related topics in different courses were instrumental in optimizing the time devoted to covering those topics. As lectures from all the courses were placed on the schedule in relationship to the various organ systems, much of the previous content duplication was identified and, where deemed unnecessary, eliminated. This step assured the course directors that critical information previously addressed in their own courses was being covered appropriately in the curriculum. The result was that lectures or portions of lectures could be omitted from each course, providing flexibility for increased coverage of more advanced and difficult concepts and allowing more time for self-directed learning activities.
CURRICULUM ORGANIZATION
For this first phase of restructuring, all course titles were maintained, and each course remained intact for grading purposes. Maintaining these boundaries during this first phase of integration served two key purposes in the evolution of the curriculum. First, it reduced some of the resistance to change stemming from the perceived loss of departmental autonomy in course control. Second, it provided a basis for comparing student performance on course and National Board of Medical Examiners (NBME) subject examinations in the prior and restructured curriculum. The primary change at this stage was reorganizing the lecture order within each course around the Human Morphology sequence (Table 2). The material from all four courses was organized into four sequential “Units,” two per semester. The first Unit was composed of material that was introductory in nature and covered the basic principles of each course. This introductory material provided the foundation needed by the students to prepare for more advanced topics. Unit One included subjects such as the core principles of biochemistry, cell structure, early embryology and histogenesis, basic cellular physiology, and the four basic tissue types. Units Two and Three treated the organ systems concentrated in the limbs, thorax, and abdomen/pelvis, respectively. These units included musculoskeletal, cardiovascular, respiratory, gastrointestinal, renal, endocrine and reproductive systems. Unit Four incorporated the head and neck portion of gross anatomy, embryology, and neurobiology.
Table 2.
Topics Covered In Each Course and Unit
| UNIT | HUMAN MORPHOLOGY | PHYSIOLOGY | BIOCHEMISTRY | NEUROBIOLOGY | ||
|---|---|---|---|---|---|---|
| GROSS ANATOMY | HISTOLOGY | EMBRYOLOGY | ||||
| I BASIC PRINCIPLES (July - August) | Cell structure Epithelium Blood Bone Connective tissues Nerve | Early Embryology | Cell membrane Ions | pH/acid-base Proteins and enzymes Metabolism Genetics Blood | ||
| II SYSTEMS 1 (September - December) | Peripheral nervous system Back Upper limb/breast Thorax Abdomen | Muscle Vessels Integument Lymphoid Cardiac Respiratory Digestive | Cardiovascular development Respiratory development GI development | Muscle Nerve Autonomic nervous system Cardiovascular Respiratory GI | Metabolism (amino acids) Immunogenetics Nutrition Metabolic interrelationship | |
| III SYSTEMS 2 (January - February) | Pelvis and Perineum Lower Limb | Renal Endocrinology Reproductive Biology | Urogenital development | Renal Endocrinology Reproductive Biology | ||
| IV SYSTEMS 3 (March - May) | Head and Neck | Head and Neck development Nervous system development | Neurobiology | |||
All the lectures relating to specific topic areas were organized on the schedule board (Fig. 2B) to build the daily and weekly curriculum schedule. Some topics were essentially stand-alone components (e.g., the lower limb), i.e., they had less correlation with the other courses and could be included in the curriculum where the schedule permitted. Flexibility was allowed for organs and systems that did not lend themselves as well to strict regional presentation schemes. As an example, pituitary and pineal histology and physiology were covered in Unit Three along with the other endocrine organs rather than in Unit Four with the head and neck.
In addition to coordinating the lecture topics among the courses, several other changes were made in the schedule (Table 3). The majority of the lecture sessions were placed in the morning and the laboratory and other active learning sessions were placed in the afternoon. Another step was to increase time for self-directed learning by replacing the previous two-hour lecture sessions in the schedule with two 90-minute sessions each morning. A 30-minute break was included between the morning lectures to provide the students time to complete their notes, consult with faculty from the first session, and prepare for the second. Further, the morning class start time was moved from 8:30am to 9:00am to accommodate faculty schedules and assist in increasing the time available to accommodate independent study and the students’ personal schedules. Two-hour laboratory sessions were scheduled for the histology and three-hour sessions for the gross anatomy and neurobiology laboratories. As a result, the students started their scheduled course work 30 minutes later each day, finished by 3:30 - 4:30 pm, (1-2 hours earlier than in previous years), and gained an added 30 minutes of independent time between lectures each day. Therefore, a total of 2-3 hours/day was shifted from direct contact hours to independent study time.
Table 3.
Improvements in daily schedule
| Before | After | Outcomes |
|---|---|---|
| 8:30 am start | 9:00 am start | More time allotted for independent study |
| 110 minute sessions | 90 minute sessions | Reduced lecture time per day and year |
| 10 minute break | 30 minute break | Time available to complete notes and prepare for next session |
| 5:00-6:00 pm finish | 3:30-4:30 pm finish | More time allotted for independent study |
| Lectures and laboratories interchanged between morning and afternoon | Lectures in morning Labs in afternoon | More consistent schedule. Better structure for position of listening time versus active learning time |
When preparing the schedule, some additional items had to be considered. For example, class sessions for two other courses occurring in the first-year curriculum also had to be accommodated. These courses, Fundamentals of Medicine and Community Health, required at least one morning and one afternoon session each week. In addition, independent study sessions were included in most weeks during at least one afternoon. These sessions allowed students to have additional designated time during the day free of class work. For some days, the first morning session was also reserved for independent study.
EXAMINATIONS
Examinations were arranged to cover 3-6 weeks of course work and placed where logical content breaks occurred or a topic ended. Ten in-course examinations were given during the year, as well as five National Board of Medical Examiners (NBME) subject examinations (Table 4). Each Unit included two examinations, except Unit two which had three full examinations and one smaller assessment. NBME subject examinations were administered at the end of the Unit in which the material covered on that examination was completed.
Table 4.
Course and subject examinations in each Unit.
| Unit (Material Covered) | Dates of Material Covered | Number of weeks included in each examination | Subject examinations given |
|---|---|---|---|
| I (Basic Principles) | July-September | 4, 3.5 | None |
| II (Above the Waist) | September- December | 4, 4, 3, 2.5 | Biochemistry |
| III (Below the Waist) | January- March | 4, 3.5 | Physiology Histology and Cell Biology |
| IV (Above the Neck) | March- May | 3, 5 | Gross Anatomy and Embryology Neurobiology |
Prior to the curricular restructuring, each course administered separate examinations during week-long examination blocks every four-to-six weeks during the year. Several changes in examination construction and delivery were implemented during restructuring (Table 5). The most significant change was the coordinated assembly of a single, multi-course examination for each block of material. The in-course examinations consisted of questions from all courses taught during the period covered. Adequate topic coverage and examination length were initial concerns. The course directors were faced with balancing the need for a sufficient number of questions to reflect topic volume and student progress, and ensuring that the examination could be completed in a reasonable amount of time to allow testing of knowledge and not simply stamina. After examining several models, it was determined that four questions per lecture would result in examinations that could be delivered in one morning, and although less than that used by each course previously, would provide adequate coverage of lecture content. In a few cases, additional questions were allowed where needed to assure appropriate coverage of the relevant learning objectives.
Table 5.
Changes in examination construction and delivery
| Before | After |
|---|---|
| Separate examination for each course (3 examinations/examination block) | 1 examination (includes questions from each course) |
| Multiple examination days (2-3 examination days) | 1 examination day only |
| Number questions determined by each course and material covered (5-6 questions/lecture) | Standard 4 questions/lecture for every course |
| Each examination ≤ 100 questions | Total number determined by number of lectures |
| Examinations with ≥ 120 questions split into 2 parts | |
| Only 1 course covered on each examination | All courses included in each examination |
| Separate examination review periods for each course | 1 examination review period |
| Answers recorded on Scantron® | Answers recorded on Scantron® |
| 1 Scantron® answer key | Multiple Scantron® keys for grading; 1 Scantron® answer key for each course |
The examination assembly process, which had previously been departmentally organized, was another item that had to be modified to a more centralized function. In the revised process, faculty members submitted examination questions to their departmental administrative assistants for each course. These assistants copied them into a master document and performed the initial word processing and formatting tasks. The Unit Coordinator (see Course Management, below) and Course Directors then proof-read the questions and sent them to a designated administrative assistant to assemble the full examination. The questions from each course were randomly placed within the examination so that the topic areas and questions from different courses were scrambled. For lecture examinations containing more than 120 questions, the examination was split into two parts, with a 30-minute break between them. After the lecture examination, there was a one hour break before the laboratory practical examination began. The lecture examinations were in multiple-choice format, delivered on paper, and the students recorded their answer on a Scantron® form (Scantron Corp, Eagen, MN). Examination keys were constructed so that the performance on questions originating from the individual courses could be determined and recorded. Examination proctoring, grading, and examination reviews were managed by the Department of Medical Education.
The anatomy laboratory practical examinations were delivered in the same format as in previous years. They consisted of students rotating through designated stations and recording the name of the indicated structure on an answer sheet. Most laboratory sessions were covered by four practical questions instead of the 5-6 that were used previously. For some examinations, the students took the examination in shifts because there were often more students than examination question stations. The Histology laboratory practical examinations were delivered via a secure software program on the students’ laptop computers. The questions were multiple-choice in nature and included a labeled light or electron microscopic image. These examinations were given in the lecture hall on the students’ laptops before the Gross Anatomy practical examination. In some cases when students were taking the Gross Anatomy practical in shifts, the class was split and half took the Gross Anatomy practical while the other half took the Histology practical.
The outcome from these arrangements meant that only 1 day was required for each examination, saving additional time for self-directed study, which was frequently scheduled in the days before the examinations. The standard four-question-per-lecture format assured topic equality for all courses and promoted equal attention by the students to each lecture topic, from course to course and throughout the year. Further, the mixed subject composition of the examinations more closely resembled the format of the USMLE, thus providing the students exposure to and training for that system.
COURSE MANAGEMENT
Another requirement of the restructuring was to establish a curriculum management system. Because the course names were maintained, each course retained its course directors. Their duties were the same as in past years and included such responsibilities as recording, calculating, and posting course grades, making course-related decisions, and communicating with course faculty and students. Because the curriculum re-organization included dividing the content of each course into Units, a Unit Coordinator was added to oversee each Unit. Each Unit Coordinator was chosen because of their teaching specialty and the heavy coverage of their course content in the Unit, as well as their availability and willingness to fill the position. Each Unit Coordinator had been a member of the restructuring team from the beginning of the process, and most of them also served as a course director. The Unit Coordinators mediated scheduling conflicts, communicated with faculty and students about curriculum or class changes, coordinated the examinations, and ensured that scores were sent to the course directors. Other duties included sending notices to faculty requesting examination questions, confirming that all questions were submitted, proof reading each question, and coordinating the examination assembly process.
After the new curriculum arrangements were implemented, the management team maintained the curriculum and assessed student performance. The management team consisted of all the individuals that participated in building the revised curriculum (faculty positions listed in Table 1). This team met weekly to bi-weekly during the year to evaluate and ensure that the courses and curriculum were on track. The Curriculum Coordinator led and organized these meetings and ensured that the team was aware of all issues, examination scores, and course events. The team ensured that all Units were operated and maintained uniformly. In addition to maintaining the current curriculum, this team made all decisions about the next phases of curriculum change.
UNEXPECTED EVENTS AND RESPONSES
One notable drawback that resulted from the reorganized lecture schedule was that student performance in the Biochemistry course was negatively affected in the first year of the new curriculum. None of the other courses experienced this downturn and the grade distribution of the other courses were similar to, or better than, in previous years.
After approximately three quarters of the Biochemistry course was complete, it was evident that overall student performance on the Biochemistry portion of the in-course examinations had suffered significantly. The course directors attributed this unexpected situation to the tight compression of the material into a much shorter time span than in previous years. A significant portion of the Biochemistry material was condensed, consolidated, omitted or presented in an alternative form. However, the majority of the course material was concentrated within the first seven weeks of the curriculum, during the time when students are still adjusting to the level of intensity required in medical school. Biochemistry had formerly been spread out over an entire semester. The poor performance prompted the Biochemistry faculty and Counseling Services to implement an in-course enrichment program for the students that were not passing the course. This enrichment program included directed learning sessions with problem solving and small group discussions, re-examination over previous content, and intense preparation for the NBME Biochemistry subject examination. As a result of these efforts, everyone passed the Biochemistry course, and the average performance on the subject examination was comparable to the previous year. In the following year the Biochemistry lecture material was decompressed by delivering it in ten weeks rather than seven.
Although there were no overall academic problems in the other courses, two organizational issues were identified; one in the Neurobiology course and one associated with the Gross Anatomy laboratory. There were only two examinations given during the presentation of the Neurobiology content. After evaluating student comments and Course Director impressions, it was determined that this course content was too much information to be included on only two examinations. During the next phase of curriculum change, an additional examination was scheduled during coverage of this material. The Gross Anatomy dissection lab extended from mid-September until mid-May, a much longer time for cadaver use than in previous years. The preservation quality of the cadavers declined, resulting in strenuous working conditions and difficulty in finding adequate structures for the examinations. In subsequent phases of curriculum change, the time frame for cadaver dissection was shortened so that this component was completed sooner.
IMPACT ON FACULTY
Three major issues impacted faculty as a result of this phase of restructuring: (1) less time to deliver the subject content during each session, (2) elimination of some lectures by some faculty members in order to reduce unnecessary duplication of content, and (3) the re-location of lecture times during the academic year. A great effort was made to inform and confirm lecture times with each faculty member because many lectures were moved to dates in the curriculum when those faculty members had not previously taught during the academic year.
The reduction in lecture time and elimination of some lectures was a difficult aspect for some faculty to accept. Informational sessions describing the planned changes were delivered to faculty before implementation of the curriculum. No workshops or tutorials were provided to faculty to assist in formulating lecture content to fit within the reduced session time. There were some instances of faculty not adhering to the time limit and extending their lecture into the break or lunch periods. The Course and/or Unit directors tried to reinforce the importance of revising lecture content and objectives to fit in the allotted time. Most faculty adapted well to the changes and made a good effort to revise their content or delivery emphasis to fit into the new curriculum parameters. As a result of this first phase of curriculum change, it was recognized that there was a need to implement a Faculty Development program to provide resources for the improvement of teaching and learning.
The reduction in class session time and the consolidation or elimination of some sessions had a beneficial impact on faculty as well as students. Although the total number of faculty members needed to teach the courses did not change, the time that each spent on academic endeavors was decreased. Faculty were able to devote more time to research and other institutional activities.
After the problem with the Biochemistry performance was identified, the Biochemistry faculty were very accommodating in giving of their time and effort to provide additional tutorial sessions. The problems that resulted in the biochemistry content were deemed not to be the fault of the faculty, but rather in the timing and spacing of biochemistry content delivery as a whole. The curriculum team addressed these concerns and made adjustments in the schedule for the following year.
OUTCOMES
The number of classroom contact hours for the four basic-science courses was reduced from a total of 880 to 630, resulting in a 28% reduction in classroom contact time. This outcome was accomplished by reducing lecture time, eliminating selected lectures, and decreasing non-essential redundancy. The time removed from the classroom was redistributed in the schedule as independent study. Adequate time for independent study has been linked with student satisfaction (Jelsing et al., 2007), and we envision that the additional time for this endeavor is beneficial for student well-being and performance.
One key measure of the success of the first phase of restructuring was NBME subject examination scores. The class averages for all five NBME subject examinations were comparable to previous years, with no observable decreases. In fact, all averages increased over the averages from the previous year. The Biochemistry average showed the least increase at 0.5%, while the Neurobiology average showed the greatest increase at 12%. The Histology and Cell Biology and Physiology average each increased by 7% while the Gross Anatomy and Embryology average was increased by 9%. In fact, the Histology and Cell Biology subject examination scores were the second highest average ever recorded at MSM while the Gross Anatomy and Embryology scores exceeded the results from the previous five years.
The students were very pleased with the revised curriculum. A survey administered at the end of the year (74% response rate, n = 53) showed an overall student satisfaction with the new elements adopted in content coverage and arrangement, the daily schedule, and the examination process. Especially noteworthy was that 92% of responders felt that the topics presented within the Units correlated well between courses. Satisfaction with examination frequency, number of examination questions per lecture, and time allotted to complete examinations was 82%, 87%, and 87%, respectively. In addition, 92% reported satisfaction in having the histology practical examinations delivered electronically. Survey items were subjected to t-test analysis, and all reported responses were significant (P < 0.0001). Students were also offered the opportunity to provide written comments about the curriculum. There were 126 written comments, which included praise, suggestions, and difficulties from the student perspective (Table 6). Many of these comments were taken into consideration during subsequent curriculum adjustments and used as the basis for modifying topic content and order and for fine tuning the curriculum for the next year.
Table 6.
Representative Student Comments
| Comments on Material Coverage, Course Content, Lecture Time and Breaks |
| The breaks were perfect. It was just enough time for us to prepare for the next class and handle any responsibilities that we had outside the classroom. |
| Biochemistry never really seemed to correlate completely with the other courses, but otherwise all the courses harmonized with each other. |
| I liked that the material covered was consistent between the different courses. The course content was well organized. The lecture time was sufficient. |
| Overall, different courses were well integrated. |
| The material covered was good, and the integration worked pretty well. |
| I liked that the material wasn't duplicated. When it was duplicated it was done appropriately and at the right time. The only thing I wish you could do is lengthen the Biochemistry and shorten the Gross. |
| The [Biochemistry] course may need more time to present the information. |
| The Human Morphology unit lasted too long. By the end of head and neck our body looked as though it had just been exhumed from the grave and we had significant difficulty identifying structures. |
| Comments on the Examination Process |
| Overall the examination process is fine. I like having everything on one examination. Neurobiology needs to have at least three written examinations, not two. All other courses were spaced out nicely. |
| I thought the examination process was well administered. I appreciate having at least a day before the test to prepare, and I especially enjoyed having examinations given on Fridays. It allows us to have a few weekends to look forward to over the school year. |
| The frequency of examinations is good. I feel that the last Neurobiology examination can be split into two. |
| I preferred the electronic delivery of Histology quizzes and tests. |
| At least 4 weeks between each Unit examination is a good amount of time. |
| I did not like when the Human Morphology practical examinations were given twice (class split into two groups) because it was very difficult to wait for an extended period of time to take the examination if you were in the second group. |
The plan for the next step in the curriculum integration process is to eliminate the current course titles. Each Unit will become a distinct course with a new title, and grade reporting will be by this title. Therefore, the traditional department-based courses will disappear and be replaced with a series of integrated block courses. An electronic examination delivery system will be utilized to aid in examination preparation, delivery, and grading. This system will further the integration process, but still allow performance in the four traditional course content areas to be tracked for student advisement and remediation purposes. The students will take all multiple-choice lecture examinations on their laptop computers using a secure examination delivery system. The result is expected to be in-course examinations that more closely mirror the mechanics of the USMLE and provide the students with more confidence in dealing with integrated examinations delivered by computer.
CONCLUSIONS
We have completed the first phase in what is projected to be a multi-phase process to revise our first year medical curriculum. The ultimate goal is to increase integration between topics. Achieving this final result will take several years and will be accomplished in a step-wise fashion. However, our goals for the first phase of reorganization have been met. Some processes used to accomplish these goals were similar to what others have done, but others are unique to our practices and institutional culture. Curriculum reform has ranged from far reaching modifications affecting multiple years of the curriculum (Taylor, 2010) to transition to a predominantly problem-based learning curriculum (Bernier et al., 2000), to more modest changes such as integrating a pharmacology electronic learning program into existing courses in an established curriculum (Dubois and Franson, 2009). We have chosen to make changes only to the first year curriculum, beginning in a relatively modest fashion with incremental changes occurring each year of this multiyear process.
Specific stages that occur in medical education reform have been identified (Loeser et al., 2007), and there are common factors used in formulating curricular changes (Bland et al., 2000). It is suggested that the curriculum chosen should fit the personality of the institution so that the best trained medical student can be produced (Drake, 1998). We have embraced this attitude, and although we are still in the process of achieving a fully integrated curriculum, we have incorporated many of the common stages and factors in the work completed. A need for revision has been identified, a vision for the ultimate integrated curriculum has been created, the development of major components and curricular design has been established, and implementation of the first curricular change has occurred. The way in which these objectives were carried out conformed to our expertise and institutional culture, due to the commitment and fortitude from each member of the restructuring team. Communication was also a key element in the success of this integration plan and is one of the elements shown to be critical in curriculum reform (Bland et al., 2000). The discussions between faculty and the camaraderie that developed were invaluable components of this process. Leadership goes hand in hand with communication, serving as an important and valuable component of the curriculum reform process (Bland et al., 2000; Loeser et al., 2007). Our institutional leaders gave approval to a faculty team to lead the change in the first year curriculum. This type of leadership afforded the luxury of using flexibility and creativity for accomplishing the work and in envisioning the final product of providing a curriculum to improve student training and learning.
Integrating a curriculum is a complex process and the understanding of the process differs by faculty, staff, and students (Muller et al., 2008). We experienced an initial period of resistance from the faculty; similar to that reported by others undergoing curriculum changes (Loeser et al., 2007). However, this potential obstacle was eventually overcome after several explanatory educational sessions delivered to faculty and staff in the basic science departments. This process was also aided by the establishment of a formal committee to oversee the restructuring process. Administrative reorganizations or appointment of committee members has been done by others (O'Connor Grochowsky et al., 2007; Rao and Rao, 2007; Frye et al., 2000), and creating a similar formalized structure for curriculum oversight worked well for us.
Anatomy education has long been recognized to be important for all areas of medicine (Sugand et al., 2010) and can influence a student's career choice (Bhangu et al., 2010). However, the amount of anatomy teaching included in medical curriculums has declined over the years (Drake et al., 2009), and there is disagreement about how much anatomy is sufficient in a curriculum (Bergman et al., 2008). Although human dissection is still regarded as the starting point in medical education, anatomy teaching methods have evolved to include more imaging, clinical correlation, and cross-sectional anatomy as well as having a role in learning about humanistic value and end-of-life attitudes (Leung et al., 2006). Cadaver dissection has also been recognized as beneficial for development of professional competencies such as teamwork, time management, and independent learning (Böckers et al., 2010). Although the majority of anatomy courses are not part of an integrated curriculum (Drake et al., 2009), our anatomy course became the cornerstone for the development of an integrated curriculum. Our course already contained much of the content considered to be optimal in a modern curriculum such as dissection/prosection, electronic learning tools, surface anatomy, and use of medical imaging modalities (Sugand et al., 2010). We chose to maintain our established anatomy sequence and orient the topics covered in other courses, around the systems-based presentation of the anatomy material.
There is a trend in medical education to decrease didactic lectures and increase self directed learning (Seifer, 1998). Students have been shown to value independent study and perceive this time as an asset to learning (Jelsing et al., 2007). In our first phase of integration, the amount of time available each week for independent study was significantly increased. The process involved to accomplish this goal was not always easy and took time, negotiation, evaluation, and diplomacy between faculty members. However, we view this increase in independent study time as a benefit for student morale, effectiveness in examination preparation, and increased opportunities for small group study, self-reliance, and independent and/or small group consultations with faculty.
Integration should also include the opportunity for students to make correlations between their learning in different topics rather than by discipline (Burge, 2003; Grochowsky et al., 2007). This concept integration has been achieved by grouping topics into the same time frame, and continuing to provide small group learning sessions. Our curriculum already provided for some small group learning sessions which helped to increase correlations between topics and these modules were maintained in the revised layout. Communication among disciplines can also be increased by the use of multidisciplinary examinations (Drake, 1998). We have adopted this process to further enhance the connection between topics presented in different courses. Although the students were still given a grade for each traditional course and not by topic, changes in course designation will occur during the next phase, so that the distinction of disciplines will become blurred.
Although there are many secondary features arising from curriculum change, the focus of this paper was to describe the methodology of creating a new curriculum. This methodology included assembly of the curriculum team, the mechanics of the restructuring process, the resultant organization of the curriculum, examination strategy, management of the courses and curriculum, and immediate outcomes. There are, of course, many other notable and interesting aspects associated with curriculum change such as faculty satisfaction, use of free faculty time for other institutional commitments, impact on research productivity, student performance in subsequent courses and on subsequent exams, and benefit of independent study time. These benefits will be addressed in subsequent publications.
The stepwise approach used in creating this first phase of course integration was instrumental in helping to accomplish curriculum restructuring by reducing turf warfare, and enhancing interactions between course directors. This process helped to quell the anticipated initial resistance to change and promoted a collaborative atmosphere among the institution's core basic science teaching faculty for making needed changes that all could accept. Meeting frequency, course director discussions, and re-organization of topics eliminated unnecessary topic duplication and redundancy. The time recovered was devoted to increasing opportunities for self directed learning. Alignment of topics between courses and the combined examinations resulted in less compartmentalization, which also promoted inter-topic integration and will better prepare the students for the integrative nature of the USMLE. The resulting curriculum is streamlined, more efficient, contains better course topic alignment, and has fewer examination days.
ACKNOWLEDGMENTS
The authors wish to acknowledge following individuals: Martha Elks, MD (Medical Education), Adel Elmoselhi, MD, PhD (Physiology), Jacqueline Hibbert, PhD (Biochemistry), John Patrickson, PhD (Neurobiology), Jacqueline Powell, PhD (Physiology), William Roth, PhD (Biochemistry), Gary Sanford, PhD (Biochemistry).
Grant Sponsor: NIH; Grant numbers: P03-1B040107; Grant sponsor: NIH; Grant number: G12-RR03034.
Footnotes
NOTES ON CONTRIBUTORS
BRENDA J. KLEMENT, Ph.D., is an assistant professor in the Department of Medical Education at Morehouse School of Medicine, Atlanta, Georgia. She is the year one medical school Curriculum Director and teaches histology to the first year medical and graduate students.
DOUGLAS F. PAULSEN, Ph.D., is a professor in the Department of Pathology and Anatomy and Associate Dean for Graduate Studies at Morehouse School of Medicine, Atlanta, Georgia. He teaches anatomy and histology to the first year medical and graduate students and is a graduate course director.
LAWRENCE E. WINESKI, Ph.D., is a professor in the Department of Pathology and Anatomy at Morehouse School of Medicine, Atlanta, Georgia. He teaches anatomy to the first year medical and graduate students. He is course director of one of the first year medical school courses.
LITERATURE CITED
- Bergman EM, Prince KJ, Drukker J, van der Vleuten CP, Scherpbier AJ. How much anatomy is enough? Anat Sci Educ. 2008;1:184–188. doi: 10.1002/ase.35. [DOI] [PubMed] [Google Scholar]
- Bernier GM, Jr, Adler S, Kanter S, Meyer WJ., 3rd On changing curricula: Lessons learned at two dissimilar medical schools. Acad Med. 2000;75:595–601. doi: 10.1097/00001888-200006000-00007. [DOI] [PubMed] [Google Scholar]
- Bhangu A, Boutefnouchet T, Yong X, Abrahams P, Joplin R. A three-year prospective longitudinal cohort study of medical students’ attitudes toward anatomy teaching and their career aspirations. Anat Sci Educ. 2010;3:184–190. doi: 10.1002/ase.165. [DOI] [PubMed] [Google Scholar]
- Bland CJ, Starnaman S, Wersal L, Moorehead-Rosenberg L, Zonia S, Henry R. Curricular change in medical schools: how to succeed. Acad Med. 2000;75:575–594. doi: 10.1097/00001888-200006000-00006. [DOI] [PubMed] [Google Scholar]
- Böckers A, Jerg-Bretzke L, Lamp C, Brinkmann A, Traue HC, Böckers TM. The gross anatomy course: An analysis of its importance. Anat Sci Educ. 2010;3:3–11. doi: 10.1002/ase.124. [DOI] [PubMed] [Google Scholar]
- Briggs HE, McBeath B. Infusing culture into practice: Developing and implementing evidence-based mental health services for African American foster youth. Child Welfare. 2010;89:31–60. [PubMed] [Google Scholar]
- Burge SM. Undergraduate medical curricula: Are students being trained to meet future service needs? Clin Med. 2003;3:243–246. doi: 10.7861/clinmedicine.3-3-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooke M, Irby DM, O'Brien BC. Educating Physicians: A Call for Reform of Medical School and Residency. 1st Ed. Jossey-Bass; San Francisco, CA: 2010. p. 320. [Google Scholar]
- Drake RL. Anatomy education in a changing medical curriculum. Anat Rec. 1998;253:28–31. doi: 10.1002/(SICI)1097-0185(199802)253:1<28::AID-AR11>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- Drake RL, McBride JM, Lachman N, Pawlina W. Medical education in the anatomical sciences: The winds of change continue to blow. Anat Sci Educ. 2009;2:253–259. doi: 10.1002/ase.117. [DOI] [PubMed] [Google Scholar]
- Dubois EA, Franson KL. Key steps for integrating a basic science throughout a medical school curriculum using an e-learning approach. Med Teach. 2009;31:822–828. doi: 10.1080/01421590903147584. [DOI] [PubMed] [Google Scholar]
- Edgren G, Haffling AC, Jakobsson U, McAleer S, Danielsen N. Comparing the educational environment (as measured by DREEM) at two different stages of curriculum reform. Med Teach. 2010;32:e233–e238. doi: 10.3109/01421591003706282. [DOI] [PubMed] [Google Scholar]
- Fincher RM, Wallach PM, Richardson WS. Basic science right, not basic science lite: Medical education at a crossroad. J Gen Intern Med. 2009;24:1255–1258. doi: 10.1007/s11606-009-1109-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frye AW, Solomon DJ, Lieberman SA, Levine RE. Fitting the means to the ends: One school's experience with quantitative and qualitative methods in curriculum evaluation during curriculum change. Med Educ Online. 2000;5:9. [Google Scholar]
- Hollander H, Loeser H, Irby D. An anticipatory quality improvement process for curricular reform. Acad Med. 2002;77:930. doi: 10.1097/00001888-200209000-00033. [DOI] [PubMed] [Google Scholar]
- Jelsing EJ, Lachman N, O'Neil AE, Pawlina W. Can a flexible medical curriculum promote student learning and satisfaction? Ann Acad Med Singapore. 2007;36:713–718. [PubMed] [Google Scholar]
- Kim KJ, Kee C. Reform of medical education in Korea. Med Teach. 2010;32:113–117. doi: 10.3109/01421590903197043. [DOI] [PubMed] [Google Scholar]
- Klement B, Paulsen DF, Wineski LE. An anatomical backbone for an integrated first-year medical curriculum.. Abstracts of Experimental Biology, FASEB 2008 Conference; San Diego, CA. 2008 Apr 5–9; 2008. [1 March 2011]. Abstract 236.3. American Association of Anatomists: Bethesda, MD. URL: http://www.fasebj.org/cgi/content/meeting_abstract/22/1_MeetingAbstracts/236.3. [Google Scholar]
- Klement B, Paulsen DF, Wineski LE. Evolution of an anatomy-based integrated curriculum.. Abstracts of Experimental Biology, FASEB 2010 Conference; Anaheim, CA. 2010 Apr 24–28; 2010. [1 March 2011]. Abstract 296.4. American Association of Anatomists: Bethesda, MD. URL: http://www.fasebj.org/cgi/content/meeting_abstract/24/1_MeetingAbstracts/296.4. [Google Scholar]
- LCME . Liaison Committee on Medical Education. The Association of American Medical Colleges (AAMC); the Council on Medical Education of the American Medical Association (AMA); Washington, DC: Chicago IL: 2011. [30 January 2011]. URL http://www.lcme.org. [Google Scholar]
- Leung KK, Lu KS, Huang TS, Hsieh BS. Anatomy instruction in medical schools: Connecting the past and the future. Adv Health Sci Educ Theory Pract. 2006;11:209–215. doi: 10.1007/s10459-005-1256-1. [DOI] [PubMed] [Google Scholar]
- Lieberman SA, Ainsworth MA, Asimakis GK, Thomas L, Cain LD, Mancuso MG, Rabek JP, Zhang N, Frye AW. Effects of comprehensive educational reforms on academic success in a diverse student body. Med Educ. 2010;44:1232–1240. doi: 10.1111/j.1365-2923.2010.03770.x. [DOI] [PubMed] [Google Scholar]
- Loeser H, O'Sullivan P, Irby DM. Leadership lessons from curricular change at the University of California, San Francisco, School of Medicine. Acad Med. 2007;82:324–330. doi: 10.1097/ACM.0b013e31803337de. [DOI] [PubMed] [Google Scholar]
- McCurdy L, Goode LD, Inui TS, Daugherty RM, Jr, Wilson DE, Wallace AG, Weinstein BM, Copeland EM., 3rd Fulfilling the social contract between medical schools and the public. Acad Med. 1997;72:1063–1070. doi: 10.1097/00001888-199712000-00016. [DOI] [PubMed] [Google Scholar]
- Mullan F, Chen C, Petterson S, Kolsky G, Spagnola M. The social mission of medical education: Ranking the schools. Ann Intern Med. 2010;152:804–811. doi: 10.7326/0003-4819-152-12-201006150-00009. [DOI] [PubMed] [Google Scholar]
- Muller JH, Jain S, Loeser H, Irby DM. Lessons learned about integrating a medical school curriculum: Perceptions of students, faculty and curriculum leaders. Med Educ. 2008;42:778–785. doi: 10.1111/j.1365-2923.2008.03110.x. [DOI] [PubMed] [Google Scholar]
- O'Connor Grochowski C, Halperin EC, Buckley EG. A curricular model for the training of physician scientists: The evolution of the Duke University School of Medicine curriculum. Acad Med. 2007;82:375–382. doi: 10.1097/ACM.0b013e3180333575. [DOI] [PubMed] [Google Scholar]
- Rao KH, Rao RH. Perspectives in medical education 5. Implementing a more integrated, interactive and interesting curriculum to improve Japanese medical education. Keio J Med. 2007;56:75–84. doi: 10.2302/kjm.56.75. [DOI] [PubMed] [Google Scholar]
- Rao KH, Rao RH. Perspectives in medical education 8. Enhancing preclinical education in Japan with a clinically focused, interactive anatomy curriculum. Keio J Med. 2009;58:210–215. doi: 10.2302/kjm.58.210. [DOI] [PubMed] [Google Scholar]
- Schofield A, Bourgeois D. Socially responsible medical education: Innovations and challenges in a minority setting. Med Educ. 2010;44:263–271. doi: 10.1111/j.1365-2923.2009.03573.x. [DOI] [PubMed] [Google Scholar]
- Seifer SD. Recent and emerging trends in undergraduate medical education. Curricular responses to a rapidly changing health care system. West J Med. 1998;168:400–411. [PMC free article] [PubMed] [Google Scholar]
- Simunovic VJ, Hren D, Ivanis A, Dørup J, Krivokuca Z, Ristic S, Verhaaren H, Sonntag HG, Ribaric S, Tomic S, Vojnikovic B, Seleskovic H, Dahl M, Marusic A, Marusic M. Survey of attitudes towards curriculum reforms among medical teachers in different socio-economic and cultural environments. Med Teach. 2007;29:833–835. doi: 10.1080/01421590701589201. [DOI] [PubMed] [Google Scholar]
- Snelgrove H, Familiari G, Gallo P, Gaudio E, Lenzi A, Ziparo V, Frati L. The challenge of reform: 10 years of curricula change in Italian medical schools. Med Teach. 2009;12:1047–1055. doi: 10.3109/01421590903178506. [DOI] [PubMed] [Google Scholar]
- Sugand K, Abrahams P, Khurana A. The anatomy of anatomy: A review for its modernization. Anat Sci Educ. 2010;3:83–93. doi: 10.1002/ase.139. [DOI] [PubMed] [Google Scholar]
- Taylor CR. Perspective: A tale of two curricula: A case for evidence-based education? Acad Med. 2010;85:507–511. doi: 10.1097/ACM.0b013e3181cc8f56. [DOI] [PubMed] [Google Scholar]
- Wineski LE, Paulsen DF. Course Syllabus for Human Morphology: Gross Anatomy, Embryology, Histology, Cytology. Department of Anatomy and Neurobiology, Morehouse School of Medicine; Atlanta, GA: 2005. [30 September 2010]. p. 71. URL: http://www.med-ed-online.org/resources/The_Human_Morphology_Course_Syllabus.pdf. [Google Scholar]
- Zhang C, Rauchwarger A, Toth C, O'Connell M. Student USMLE step 1 preparation and performance. Adv Health Sci Educ Theory Pract. 2004;9:291–297. doi: 10.1007/s10459-004-3925-x. [DOI] [PubMed] [Google Scholar]


