Abstract
Classical population genetics shows that varying permutations of genes and risk factors permit or disallow the effects of causative agents, depending on circumstance. For example, genes and environment determine whether a fox kills black or white rabbits on snow or black ash covered islands. Risk promoting effects are different on each island, but obscured by meta-analysis or GWAS data from both islands, unless partitioned by different contributory factors. In Alzheimer's disease, the foxes appear to be herpes, borrelia or chlamydial infection, hypercholesterolemia, hyperhomocysteinaemia, diabetes, cerebral hypoperfusion, oestrogen depletion, or vitamin A deficiency, all of which promote beta-amyloid deposition in animal models—without the aid of gene variants. All relate to risk factors and subsets of susceptibility genes, which condition their effects. All are less prevalent in convents, where nuns appear less susceptible to the ravages of ageing. Antagonism of the antimicrobial properties of beta-amyloid by Abeta autoantibodies in the ageing population, likely generated by antibodies raised to beta-amyloid/pathogen protein homologues, may play a role in this scenario. These agents are treatable by diet and drugs, vitamin supplementation, pathogen detection and elimination, and autoantibody removal, although again, the beneficial effects of individual treatments may be tempered by genes and environment.
1. Introduction
If there is one factor common to complex polygenic diseases it is the heterogeneity in both gene and risk factor association studies.
Although these have discovered key genes and risk factors, the results for most are invariably confounded by conflicting data [1]. In the genetic arena, the clear familial component of many diseases has driven the search for major genes using genome-wide association studies (GWAS) with large numbers of patients pooled from different regions [2]. Such studies have been able to discover rare variants that play a major role in a small percentage of patients, for example VIPR2 in schizophrenia [3]. However, in complex diseases, these have failed to find major genes relevant to all patients [4], instead unearthing yet more genes of small effect, whose risk promoting effects are yet again contested, as is the case with CR1 and PICALM, which have not been confirmed as risk factors for Alzheimer's disease in Chinese patients [5] despite extensive evidence in Caucasian studies [6]. GWAS studies have, however, been more successful in uncovering larger numbers of genes of greater effect for simpler traits such as lipid levels [7].
Viruses and other pathogens have been implicated as risk factors in many diseases, although again, conflicting evidence leads to scepticism in many areas. For example, the involvement of the Epstein-Barr virus in multiple sclerosis is hotly contested [8–10].
Gene-gene and gene-environment interactions may play an important role in such inconsistency. For example, the risk promoting effects of genes can be better explained when using pathway analysis or combining the effects of genes with common function, rather than by studying single genes in isolation [11, 12]. Genes and risk factors can also act together, and in certain cases genes can be linked to environmental variables. For example, many of the genes implicated in schizophrenia or Alzheimer's disease are involved in the life cycles of the pathogens involved in the diseases [13, 14]. Environment-environment interactions are also apparent. For example, the effects of vitamin E on lifespan, or on resistance to various infections can be null, deleterious, or protective, depending on confounding factors such as age, exercise, smoking, and vitamin C consumption [15–17].
Complex diseases are also composed of many endophenotypes or underlying pathologies, and different genes or risk factors may contribute to any of these. Many different processes contribute to cell death in Alzheimer's disease, for example, beta amyloid, glutamate, calcium, or free radical mediated toxicity [18, 19]. The efficiency of each of these subprocesses is controlled by genes, many of which have been implicated in association studies (see Table 1).
Table 1.
A summary of the KEGG pathway analysis of Alzheimer's disease susceptibility genes. The number of genes in each pathway is shown in brackets (see http://www.polygenicpathways.co.uk/alzkegg.htm for coloured figures).
| Immune system and pathogen defence | Pathogen entry pathways | Structural and DNA repair (and HSV-1 pathways) |
|---|---|---|
| Cytokine-cytokine receptor interaction (13) | Chagas disease (17) | Regulation of actin cytoskeleton (8) |
| Hematopoietic cell lineage (11) | Hepatitis C (13) | Endocytosis (8) |
| Complement and coagulation cascades (11) | Malaria (12) | Protein processing in endoplasmic reticulum (8) |
| Natural killer cell-mediated cytotoxicity (10) | Amoebiasis (11) | Nucleotide excision repair (4) |
| Chemokine signaling pathway (9) | Microbial metabolism in diverse environments (10) | Spliceosome (4) |
| Phagosome (9) | Leishmaniasis (9) | DNA replication (3) |
| Lysosome (8) | Viral myocarditis (6) | Homologous recombination (3) |
| T cell receptor signaling pathway (8) | Staphylococcus aureus infection (6) | RNA transport (2) |
| Toll-like receptor signaling pathway (8) | Bacterial invasion of epithelial cells (4) | Mismatch repair (2) |
| NOD-like receptor signaling pathway—(7) | Pathogenic Escherichia coli infection (3) | Base excision repair (2) |
| Systemic lupus erythematosus (7) | Epithelial cell signaling in Helicobacter pylori infection (2) | Apoptosis and oxidative stress |
| B cell receptor signaling pathway (6) | Shigellosis (2) | Apoptosis (10) |
| Graft-versus-host disease (6) | Metabolism | Drug metabolism cytochrome P450 (6) |
| Cytosolic DNA-sensing pathway (5) | Oxidative phosphorylation (14) | Glutathione metabolism (5) |
| Antigen processing and presentation (5) | Arginine and proline metabolism (7) | Metabolism of xenobiotics by cytochrome P450 (5) |
| Intestinal immune network for IgA production (5) | Glycolysis/gluconeogenesis (5) | Peroxisome (3) |
| Type I diabetes mellitus (5) | Valine, leucine, and isoleucine degradation (4) | Drug metabolism—other enzymes (2) |
| Salivary secretion (5) | One carbon pool by folate (3) | Signalling pathways |
| Adipocytokine signaling pathway (5) | Terpenoid backbone biosynthesis (3) | MAPK signalling (35) |
| Fc epsilon RI signaling pathway (4) | Pyruvate metabolism (3) | Calcium signaling pathway (13) |
| Allograft rejection (4) | Citrate cycle (TCA cycle) (3) | PPAR signaling pathway (12) |
| TGF-beta signaling pathway (4) | Glycine, serine, and threonine metabolism (3) | Neurotrophin signaling pathway (12) |
| Autoimmune thyroid disease (4) | Protein digestion and absorption (3) | Wnt signaling pathway (10) |
| RIG-I-like receptor signaling pathway (4) | Tyrosine metabolism (3) | Insulin signaling pathway (9) |
| Jak-STAT signaling pathway (4) | Steroid hormone biosynthesis (3) | VEGF signaling pathway (7) |
| Fc gamma R-mediated phagocytosis (3) | Steroid biosynthesis (3) | Vascular smooth muscle contraction (6) |
| Leukocyte transendothelial migration (3) | Glycerolipid metabolism (3) | Notch signaling pathway (5) |
| Asthma (3) | Porphyrin and chlorophyll metabolism (3) | ABC transporters (5) |
| Primary immunodeficiency (2) | Histidine metabolism (2) | Renin-angiotensin system (4) |
| Sphingolipid metabolism (2) | Cardiac muscle contraction (4) | |
| Cysteine and methionine metabolism (2) | mTOR signaling pathway (3) | |
| Purine metabolism (2) | ErbB signaling pathway (3) | |
| Tryptophan metabolism (2) | Aldosterone-regulated sodium reabsorption (3) | |
| Lysine degradation (2) | Progesterone-mediated oocyte maturation (3) | |
| Primary bile acid biosynthesis (2) | GnRH signaling pathway (2) | |
| Hedgehog signaling pathway (2) |
In genetic association studies, the drive has been to increase statistical power by increasing the numbers of subjects enrolled. This has resulted in the discovery of important genes and rare genetic variants, but has not delivered genes that confer a high degree of risk in the majority of patients. However, as illustrated below, more could perhaps be gained by a reanalysis of existing data in relation to other genetic and risk factor variables that could result in elucidation of the causes rather than the risks.
2. Methods
Alzheimer's disease susceptibility genes and risk factors are stocked in an online database at http://www.polygenicpathways.co.uk/alzenvrisk.htm. KEGG pathway analysis of over 400 associated genes was performed [20], and the results of the exercise were posted at http://www.polygenicpathways.co.uk/alzkegg.htm. In these figures, yellow genes have been implicated in Alzheimer's disease and red genes are also implicated in the herpes simplex life cycle. Other gene-risk factor relationships were identified by literature survey. B cell and T cell epitopes within the beta-amyloid peptide were identified using the immune epitope database server http://tools.immuneepitope .org/main/index.html which predicts the antigenicity of peptide sequences, based on their charge and hydrophobicity properties [21]. Sequence comparisons of the beta-amyloid peptide versus selected bacterial, fungal, or viral proteomes was performed using the NCBI blast server [22, 23].
3. Results and Discussion
3.1. Kegg Pathway Analysis of Alzheimer's Disease Susceptibility Genes
The overall results of this analysis are shown in Table 1. The pathways include many that are relevant to the known pathologies and risk factors of Alzheimer's disease, including the Alzheimer's disease pathway itself, primarily related to beta-amyloid and tau processing, but also to glutamate-related pathways (long-term potentiation and depression), apoptosis, insulin and diabetes pathways, neurotrophin signalling, oxidative stress (glutathione/oxidative phosphorylation), cerebral hypometabolism (oxidative phosphorylation, glycolysis and the Krebs cycle), arginine and proline metabolism (including nitric oxide), and folate, methionine and homocysteine metabolism, and steroid hormone synthesis (together with androgen and oestrogen receptors AR, ESR1, and ESR2). PPAR signalling regulates many lipoprotein-related genes and cholesterol/lipid pathways are dispersed in terpenoid backbone biosynthesis (FDPS, HMGCR, HMGCS2), steroid hormone biosynthesis (HSD11B1), steroid biosynthesis (DHCR24, LIPA, SOAT1), glycerolipid metabolism (ALDH2, LIPC, LPL), and bile acid biosynthesis (CH25H, CYP46A1) pathways. Immune, complement, and cytokine-related pathways figure prominently, as do several pathogen defence pathways including the DNA sensing retinoic acid inducible gene (RIG-1) pathways that react to viral DNA/RNA by increasing the expression of interferons and other antiviral genes, and the Toll receptor and NOD pattern recognition pathway that control immune and cytokine networks [24–26]. Glutathione pathways were also present. Glutathione has potent viricidal and bactericidal properties and is often depleted by infections [27–30]. A number of pathogen entry pathways are also concerned, and although C. Pneumoniae or C. Neoformans pathways are not specifically represented, many of these pathways can be considered as generic pathways relevant to many bacteria and other pathogens. The H. Pylori pathway contains only two genes, IL8 and CSK, but others can be added to this list including all members of the PI 3-kinase/AKT signalling network which is activated by the H. pylori protein CagA [31] or Toll receptor pathways that are activated by H. Pylori heat shock protein, HSP60 [32]. Similarly, there is no specific HSV-1 viral entry pathway in the KEGG database, but the virus uses actin pathways, endocytosis, protein processing, and DNA repair pathways during its life cycle, which are heavily represented [33].
3.2. Vitamin-A-Related Genes
These were identified by literature survey and the most directly relevant are shown in Table 2. Of particular interest is a close relationship between cholesterol/lipoprotein-related genes and vitamin A. Both retinols and cholesterol are transported by lipoproteins, and the clusterin receptor, LRP2/megalin, is a key retinol entry point. APOE4 is the isoform least able to bind to retinyl palmitate. ABCA1 is also involved in cholesterol and retinol transport. Several genes (ALDH2, CYP46A1, GSTM1, GSTP1, LIPA, LPL, and LRAT) are involved in Vitamin A metabolism, and 24-s hydroxycholesterol, the product of CYP46A1, is a ligand for retinoic acid receptors (RARA and RARG). Retinoid coreceptors and binding partners include RXRA, ESR1, KLF5 NPAS2, NR1H2, PARP1, PIN1, POU2F1, PPARA, PPARG, THRA, UBQLN1, and VDR. Retinoids modulate APP processing, via regulation of beta and gamma secretases while the RIG-1 pathway is crucial in viral defence. A large number of genes are also regulated by retinoids or retinoid receptors.
Table 2.
The relationships of Alzheimer's disease susceptibility genes with vitamin A. NF = none found.
| Gene | Name | Relationships with vitamin A |
|---|---|---|
| Transport and entry | ||
| ALB | Albumin | Together with retinol binding protein forms the retinol transporter [39] |
| APOE | Apolipoprotein E | Expression regulated by LXR/RXR dimers [40] Involved in retinyl palmitate transport [41] |
| TTR | Transthyretin (prealbumin, amyloidosis type I) | Carrier protein for the retinol binding protein [42] |
| APOA1 | Apolipoprotein A-I | RORA target [43]: associates with transthyretin in plasma [44] |
| HSPG2 | Perlecan: (heparan sulfate proteoglycan 2) | Binds to transthyretin [45] |
| A2M | Alpha-2-macroglobulin | Synthesis decreased in vitamin-A- deficient rats [46] |
| ABCA1 | ATP-binding cassette, subfamily A (ABC1), member 1 | 22R-hydroxycholesterol and 9-cis-retinoic acid induce ABCA1 expression and cholesterol efflux in brain cells and decrease Beta-amyloid secretion [47]. Involved in retinol and alpha- and gamma-tocopherol transport [48, 49] |
| CLU | Clusterin (APOJ) LRP2 ligand | The clusterin promoter contains a RARE sequence: Expression is suppressed by all-trans-retinoic acid [50]. Vitamin A deficiency increases clusterin expression in sertoli cells [51] |
| LRP2 | Low density lipoprotein-related protein 2 (clusterin receptor) | Mediates the endocytosis of retinol via binding to retinol binding proteins and transthyretin [52, 53] |
| LRPAP1 | Low density lipoprotein receptor-related protein associated protein 1 | Regulates the uptake of retinol by LRP2 [54] |
|
| ||
| Metabolism | ||
| ALDH2 | Aldehyde dehydrogenase 2 family (mitochondrial) | Exhibits low NAD(+)-dependent retinaldehyde activity [55]: regulated by RARB [56] |
| CYP46A1 | Cytochrome P450, family 46, subfamily A, polypeptide 1 | Synthesises 24-S hydroxycholesterol, a ligand for RARA and RARG [57] |
| GSTM1 | Glutathione S-transferase M1 | Weakly catalyses the enzymic isomerization of 13-cis-retinoic acid to all-trans-retinoic acid [58] |
| GSTP1 | Glutathione S-transferase pi | Catalyses the enzymic isomerization of 13-cis-retinoic acid to all-trans-retinoic acid [58] |
| LIPA | Lipase A, lysosomal acid, cholesterol esterase (Wolman disease) | Metabolises carotenoid mono- and diesters providing a source of free carotenoids in the gut [59] |
| LPL | Lipoprotein lipase | Metabolises retinyl esters [60]. RORA target [61] |
| LRAT | Lecithin retinol acyltransferase (phosphatidylcholine—retinol O-acyltransferase) | Lecithin retinol acyltransferase (phosphatidylcholine—retinol O-acyltransferase) |
| MEF2A | Myocyte enhancer factor 2A | Regulates beta-carotene 15,15′-monooxygenase 1 which cleaves beta-carotene to all-trans retinal and is the key enzyme in the intestinal metabolism of carotenes to vitamin A [62] |
|
| ||
| Receptors, coreceptors and receptor binding partners | ||
| CHD4 | Chromodomain helicase DNA binding protein 4 | Binds to RORG [63] |
| ESR1 | Estrogen receptor 1 | Dimerises with RAR and RXRA [52] |
| KLF5 | Kruppel-like factor 5 (intestinal) | Binds to RARA [64] |
| NPAS2 | Neuronal PAS domain protein 2 | RAR alpha and RXR alpha bind to CLOCK and NPAS2 [65]. RORA target [66] |
| NR1H2 | Nuclear receptor subfamily 1, group H, member 2: liver X receptor beta | LXRs form obligate heterodimers with retinoid X receptors RARA, RXRA, RXRB, RXRG (Entrez gene) |
| PARP1 | Poly (ADP-ribose) polymerase family, member 1 | Interacts with RARB [67] |
| PIN1 | Protein (peptidylprolyl cis/trans isomerase) NIMA-interacting 1 | RARalpha directly interacts with Pin1. Overexpression of Pin1 inhibits ligand-dependent activation of RARalpha [68] |
| POU2F1 | POU class 2 homeobox 1 | Binds to RXR [69] |
| PPARA | Peroxisome proliferator-activated receptor alpha | Dimerises with RXRA and RXRG receptors [70] |
| PPARG | Peroxisome proliferator-activated receptor gamma | Dimerises with RXRA receptors [71] |
| RXRA | Retinoid X receptor, alpha | Retinoic acid receptor |
| THRA | Thyroid hormone receptor, alpha (erythroblastic leukemia viral (v-erb-a) oncogene homolog, avian) | Dimerises with RXRA [72] |
| UBQLN1 | Ubiquilin 1 | Binds to retinoic acid receptor alpha [73] |
| VDR | Vitamin D (1,25-dihydroxyvitamin D3) receptor | Heterodimerises with RXR and RARG [74] |
|
| ||
| APP and tau processing | ||
| APP | Amyloid beta (A4) precursor protein (peptidase nexin-II, Alzheimer disease) | A gamma 57 gamma secretase cleavage product suppresses retinoid signalling [75] |
| BACE1 | Beta-site APP-cleaving enzyme 1 | Regulated by all-trans-retinoic acid [76] |
| NCSTN | Nicastrin | Blocks the effects of retinoic acid on neurogenesis [77] |
| PSEN1 | Presenilin 1 (Alzheimer disease 3) | Regulated by and regulates the effects of retinoic acid on neuronal differentiation [78, 79] |
| PSEN2 | Presenilin 2 (Alzheimer disease 4) | Activated by all-trans-retinoic acid in osteoblasts [80] |
| CDK5 | Cyclin-dependent kinase 5 | Activated by retinoic acid [81] |
| GSK3B | Glycogen synthase kinase 3 beta | SH-SY5Y cells differentiate to neuron-like cells when treated with Retinoic acid/BDNF leading to increases in tau and tau phosphorylation, mediated primarily by GSK3B [82]: GSK3B inhibitors inhibit RARbeta-induced adipogenesis in mouse embryonic stem cells [83]. |
| MAPT | Microtubule-associated protein tau | Phosphorylation of tau at the 12E8 (Ser-262/Ser-356) epitope decreased in retinoic acid treated cells: increased at Ser-195/Ser-198/Ser-199/Ser-202) and (Ser-396/Ser-404) [84] |
|
| ||
| Viral and bacterial defence RIG-1, PKR, NOD and Toll receptor signalling | ||
| CARD8 | Caspase recruitment domain family, member 8 | NF |
| CD14 | CD14 molecule | Expression regulated by retinoids [85]: binds to H. Pylori lipopolysaccharide [86]. |
| CD86 | CD86 molecule | Expression modulated by and the viral DNA minic polyriboinosinic:polyribocytidylic acid [87] |
| CST3 | Cystatin C | NF antimicrobial peptide [88] |
| DEFB122 | Defensin, beta 122: Antimicrobial peptide | NF |
| EIF2AK2 | Eukaryotic translation initiation factor 2-alpha kinase 2: (PKR activated by viral DNA) | Upregulated by retinoic acid in HL-60 leukemia cells [89] |
| GBP2 | Guanylate binding protein 2, interferon inducible | NF |
| MEFV | Mediterranean fever | NF |
| MPO | Myeloperoxidase | Antimicrobial peptide [88], expression regulated by RXR/PPAR gamma heterodimer [90] |
| PIN1 | peptidylprolyl cis/trans isomerase, NIMA-interacting 1 | Binds to and negatively regulates IRF3 [91] |
| TF | Transferrin | Antimicrobial peptide [88]. Vitamin A deficiency is associated with modified iron homeostasis that can be reversed by retinoid supplementation, TF contains a peroxisome proliferator-activated receptor-retinoic acid X receptor heterodimer binding site [92] |
| TRAF2 | TNF receptor-associated factor 2 | Infection with RNA viruses activates the cytoplasmic retinoic acid-inducible gene-I (RIG-I) pathway which activates transcription factor IRF-3 which in turn induces many antiviral genes. It also induces apoptosis via TRAF2 [25] |
| TLR4 | Toll-like receptor 4 | Expression suppressed by retinoic acid [93] |
| PVRL2 | Poliovirus receptor-related 2 (herpesvirus entry mediator B) | NF: herpes simplex receptor |
| ZBP1 | Z-DNA binding protein 1: DNA-dependent activator of interferon regulatory factors | NF |
|
| ||
| Cholesterol lipoprotein networks and lipid rafts | ||
| ABCA1 | Retinol transporter (see above) | |
| ABCG1 | ATP-binding cassette, subfamily G (WHITE), member 1 | Expression regulated by 9-cis retinoic acid and 22-hydroxycholesterol [94] |
| APOA5 | Apolipoprotein A-V | Regulated by RORA [95]. APOA5 polymorphisms modify lipoprotein bound retinyl palmitate concentrations [96] |
| APOC2 | Apolipoprotein C-II | Expression regulated by 9-cis-retinoic acid [97]. |
| APOC3 | Apolipoprotein C-III | RORA target [43] |
| APOC4 | Apolipoprotein C-IV | Expression regulated by RXR ligands [98] |
| APOD | Apolipoprotein D | Expression regulated by RARA [99] |
| CETP | Cholesteryl ester transfer protein, plasma | Expression induced by 9-cis retinoic acid (RXR agonist) [100] |
| FDPS | Farnesyl diphosphate synthase (farnesyl pyrophosphate synthetase, dimethylallyltranstransferase, geranyltranstransferase) | Activated by the LXR/retinoid X receptor dimer [101] |
| LPA | Lipoprotein, Lp(a) | Isotretinoin reduces LPA serum levels [102] |
| LDLR | Low-density lipoprotein receptor (familial hypercholesterolemia) | NF |
| LRP1 | Low-density lipoprotein-related protein 1 (alpha-2-macroglobulin receptor) | NF |
| LRP2 | See above (retinol receptor) | |
| LRP6 | Low-density lipoprotein receptor-related protein 6 | Expression induced by retinoic acid [103] |
| LRP8 | Low-density lipoprotein receptor-related protein 8, apolipoprotein e receptor | NF |
| NPC1 | Niemann-Pick disease, type C1 | NF |
| NPC2 | Niemann-Pick disease, type C2 | NF |
| OLR1 | Oxidized low-density lipoprotein (lectin-like) receptor 1 | NF |
| RFTN1 | Raftlin, lipid raft linker 1 | NF |
| SOAT1 | sterol O-acyltransferase 1: cholesterol acyltransferase | NF |
| SREBF1 | Sterol regulatory element binding transcription factor 1 | Liver X receptor/RXR target [104] |
| VLDLR | Very-low-density lipoprotein receptor | All-trans retinoic acid increases expression in adenocarcinoma cells [105] |
|
| ||
| Chemokines and cytokines and inflammation | ||
| AGER | Advanced glycosylation end product-specific receptor | Expression upregulated by retinol and vitamin A [106, 107] |
| ALOX5 | Arachidonate 5-lipoxygenase | RORA target [108] |
| CCL2 | Chemokine (C-C motif) ligand 2 | All-trans-retinoic acid suppresses bacterial lipopolysaccharide-induced expression and release in astrocytes [109] |
| CCL3 | Chemokine (C-C motif) ligand 3 | See CCL2 above |
| CCR2 | Chemokine (C-C motif) receptor 2 | Expression regulated by 9-cis-Retinoic acid [110] |
| IL10 | Interleukin 10 | All trans-retinoic acid increases IL10 production in monocytes and macrophages [111] |
| IL18 | Interleukin 18 (interferon-gamma-inducing factor) | Differentiation of SH-SY5Y neuroblastoma cells by all-trans retinoic acid activates IL18 [112]. |
| IL1A | Interleukin 1, alpha | Retinoic acid decreases expression in thymic epithelial cells [113] |
| IL1B | Interleukin 1, beta | Intraperitoneal retinoic acid reduces IL-1β, IL-6 and TNFα mRNA levels in the spinal cord after injury [114]. All-trans-retinoic acid increases IL1B expression in human aortic smooth muscle cells [115] |
| IL33 | Interleukin 33 | NF |
| IL6 | Interleukin 6 (interferon, beta 2) | Retinoic acid increases expression in thymic epithelial cells [113]. |
| IL8 | Interleukin 8 | Retinoid administration decreases polymorphonuclear neutrophilic leukocyte accumulation in mammary alveoli activated by lipopolysaccharide, and decreases IL-8 serum levels [116] |
| IL1RN | interleukin 1 receptor antagonist | Retinoic acid enhances IL-1 beta and inhibited IL-1ra production in 4beta phorbol 12beta-myristate-13alpha acetate - and lipopolysaccharide-activated human alveolar macrophages [117]. |
| PTGS2 | Prostaglandin-endoperoxide synthase 2 (prostaglandin G/H synthase and cyclooxygenase) | Suppressed by RARB [118] |
| TGFB1 | Transforming growth factor, beta 1 | Repressed by RXRA.PPARG dimers [119] |
| TNF | Tumor necrosis factor (TNF superfamily, member 2) | LPS from bacterial pathogens activates Retinoic inducible gene RIG-I which plays a key role in the expression of TNF-alpha in macrophages in response to LPS stimulation [120] |
| FAS | Fas (TNF receptor superfamily, member 6) | Retinoic acid increases the expression of FAS in adipocytes: all-trans retinoid acid reduces FAS expression in HELA cells |
|
| ||
| Complement and immune system | ||
| C4A | Complement component 4A (Rodgers blood group) | Complement C4 levels correlate with those of retinol in plasma [121] |
| C4B | Complement component 4B (Chido blood group) | See above |
| CFH | Complement factor H | Expression controlled by RAR beta [122] |
| CLU | Clusterin | See above |
| CR1 | Complement component (3b/4b) receptor 1 (Knops blood group) | NF |
| CRP | C-reactive protein, pentraxin related | Serum CRP levels negatively correlate with vitamin A levels [123] |
| CD33 | CD33 molecule | NF |
| CD36 | CD36 molecule (thrombospondin receptor) | RORA target [61] |
| HLA-A | Major histocompatibility complex, class I, A | Upregulated by differentiation of teratoma cells into neuronal cells by retinoic acid [124] |
| HLA-A2 | Major histocompatibility complex, class I, A2 | Upregulated by interferon alpha-2b and retinoic acid combined treatment in cervical cancer cells [125] |
| MICA | MHC class I polypeptide-related sequence A | Expression upregulated by retinoic acid in hepatic carcinoma cells [126] |
|
| ||
| Oestrogen and androgen related | ||
| AR | Androgen receptor (dihydrotestosterone receptor; testicular feminization; spinal and bulbar muscular atrophy; Kennedy disease) | |
| ESR1 | See above | |
| ESR2 | Estrogen receptor 2 (ER beta) | 9-cis retinoic acid stimulates expression in breast cancer cells [127] |
| CYP19A1 | Cytochrome P450, family 19, subfamily A, polypeptide 1: aromatase: estrogen synthase | Activated by RORA [128] |
| HSD11B1 | Hydroxysteroid (11-beta) dehydrogenase 1 | NF |
|
| ||
| Growth factor networks | ||
| BDNF | Brain-derived neurotrophic factor | Expression regulated by RARalpha/beta and vitamin A [129, 130], but all-trans retinoic acid reduces BDNF and TrkB gene expression in SH-SY5Y cells [131] |
| CSK | C-src tyrosine kinase | CSK negatively regulates RAR functions in relation to neurite differentiation [132] |
| FGF1 | Fibroblast growth factor 1 (acidic) | Protects fibroblasts from apoptosis induced by retinoid CD437 [133] |
| GAB2 | GRB2-associated binding protein 2 | Gab2 silencing results in hypersensitivity to retinoic acid -induced apoptosis in neuronal cells [134] |
| IGF1 | Insulin-like growth factor 1 (somatomedin C) | Pulmonary expression reduced in RORalpha knockout mice [135] |
| NTRK1 | Neurotrophic tyrosine kinase, receptor, type 1 | Retinoic acid restores adult hippocampal neurogenesis and reverses spatial memory deficit in vitamin-A-deprived rats, partly by upregulating NTRK1 (TrkA) [136] |
| NTRK2 | Neurotrophic tyrosine kinase, receptor, type 2 | All-trans retinoic acid reduces BDNF and TrkB gene expression in SH-SY5Y cells [131] |
| VEGFA | vascular endothelial growth factor A | Expression regulated by retinoid acid [137] |
| Other signalling | ||
| DKK1 | Dickkopf homolog 1 (Xenopus laevis) | Expression regulated by retinoic acid in stem cells [103] |
| DPYSL2 | Dihydropyrimidinase-like 2 | Upregulated in cortex and hippocampus by Vitamin A depletion [138] |
|
| ||
| Homocysteine and methionine metabolism | ||
| BLMH | Bleomycin hydrolase | Hydrolyses homocysteine thiolactone [139] |
| CBS | Cystathionine-beta-synthase | Converts homocysteine to cystathionine suppressed by all-trans-retinoic acid [140] |
| MSRA | methionine sulfoxide reductase A | Regulated by retinoic acid via two promoters including RARA [141] |
| MTHFD1L | Methylenetetrahydrofolate dehydrogenase (NADP+ dependent) 1-like | NF |
| MTHFR | 5,10-methylenetetrahydrofolate reductase (NADPH) | Methylenetetrahydrofolate reductase activity is suppressed in retinol-fed rats [142] |
| MTR | 5-methyltetrahydrofolate-homocysteine methyltransferase | In rats, a retinol-rich diet enhances the folate-dependent oxidation to CO2 of formate and histidine. The activity of hepatic methylenetetrahydrofolate reductase, which regulates liver folate metabolism, is suppressed, leading to decreased 5-methyltetrahydrofolate synthesis [142] |
| MTRR | 5-methyltetrahydrofolate-homocysteine methyltransferase reductase | NF |
| PON1 | Paraoxonase 1 | Hydrolyses homocysteine thiolactone [143]: vitamin A deficiency reduced serum PON1 activity in rats [144]. |
|
| ||
| Oxidative stress, Iron and mitochondria | ||
| COX1 | Mitochondrially encoded cytochrome c oxidase I | 9-cis retinoic acid treatment increases mitochondrial DNA transcription, including ND1, ND6, and COX1 [145] |
| COX2 | Mitochondrially encoded cytochrome c oxidase II | Expression increased by all-trans retinoic acid [146] |
| GAPDH | Glyceraldehyde-3-phosphate dehydrogenase | Retinoic acid target [147] |
| GSTM3 | Glutathione S-transferase M3 (brain) | Contains a retinoid X receptor-binding site [148] |
| HBG2 | Hemoglobin, gamma G | Vitamin A increases haemoglobin concentrations in children [149] |
| HFE | hemochromatosis | Neuroblastoma cells carrying the C282Y HFE variant do not differentiate when exposed to retinoic acid [150] |
| HMOX1 | Heme oxygenase (decycling) 1 | The increase in the expression of heme oxygenase-1 and the growth arrest and DNA damage-inducible transcription factor 153 caused by reactive oxygen species is blocked by aRARalpha-specific antagonist AGN194301 in retinal epithelial cells [151] |
| ND1 | NADH dehydrogenase subunit 1 | 9-cis retinoic acid treatment increases mitochondrial DNA transcription, including ND1, ND6, and COX1 [145] |
| ND4 | NADH dehydrogenase subunit 4 | Upregulated by all-trans retinoic acid in neutrophils [152] |
| ND6 | NADH dehydrogenase subunit 6 | 9-cis retinoic acid treatment increases mitochondrial DNA transcription, including ND1, ND6, and COX1 [145] |
| NFE2L2 | Nuclear factor (erythroid-derived 2)-like 2 | Inhibited by retinoic acid via RARalpha resulting in lack of expression of Nrf2 target genes [153] in mammary cells, but retinoic acid and 12-O-tetradecanoylphorbol acetate are also able to induce Nrf2 and its target gene NAD(P)H quinone oxidoreductase 1 in the SH-SY5Y neuroblastoma cell line [154]. |
| NOS1 | Nitric oxide synthase 1 (neuronal) | Expression regulated by retinoic acid [84] |
| NOS2 | Nitric oxide synthase 2, inducible | Ditto |
| NOS3 | Nitric oxide synthase 3 (endothelial cell) | Ditto |
| NQO1 | NAD(P)H dehydrogenase, quinone 1 | Retinoic acid (RA) and 12-O-tetradecanoylphorbol acetats are able to induce Nrf2 and its target gene NAD(P)H quinone oxidoreductase 1 in the SH-SY5Y neuroblastomacell line [154] |
| SOD2 | Superoxide dismutase 2, mitochondrial | All-trans-retinoic acid induces manganese superoxide dismutase in a human neuroblastoma cell line [155] |
| PCK1 | Phosphoenolpyruvate carboxykinase 1 (soluble) | Three RXR-binding elements (retinoic acid response element (RARE)1/PCK1, RARE2, and RARE3/PCK2) are located in the promoter of Pck1 [156] |
| PON2 | Paraoxonase 2 | NF |
| PON3 | Paraoxonase 3 | NF |
| TFAM | Transcription factor A, mitochondrial | Levels are increased by vitamin A [157] |
|
| ||
| Heat shock | ||
| DNAJC28 | DnaJ (Hsp40) homolog, subfamily C, member 28 | NF |
| HSPA1B | Heat shock 70 kDa protein 1B | NF |
| HSPA5 | Heat shock 70 kDa protein 5 (glucose-regulated protein, 78 kDa) | Endoplasmic reticulum stress is increased in hepatocarcinoma cells by all-trans retinoic acid, characterised by increased expression of HSPA5 (grp78), GADD153, and XBP1[158] |
|
| ||
| Monoamine networks | ||
| ADRB1 | Adrenergic, beta-1-, receptor | RARA target [159] |
| ADRB2 | Adrenergic, beta-2-, receptor, surface | Expression regulated by all-trans retinoic acid [160] |
| COMT | Catechol-O-methyltransferase | Expression stimulated by all-trans retinoic acid [161] |
| PNMT | Phenylethanolamine N-methyltransferase | Retinoic acid differentiates embryonic carcinoma cells into neuronal cells, 70% of which stain for tyrosine hydroxylase, dopamine beta-hydroxylase, and phenylethanolamine N-methyltransferase [162]. |
|
| ||
| Cholinergic | ||
| CHAT | Choline acetyltransferase | Expression controlled by retinoic acid [163] |
| CHRNA3 | Cholinergic receptor, nicotinic, alpha 3 | Expression increased by retinoid acid [164] |
| CHRNA4 | Cholinergic receptor, nicotinic, alpha 4 | Expression decreased by retinoic acid [164] |
| CHRNB2 | Cholinergic receptor, nicotinic, beta 2 (neuronal) | Expression increased by retinoid acid [164] |
|
| ||
| Neuropeptide | ||
| GRN | Granulin | All-trans retinoic acid increases expression in myeloid cells [165] |
|
| ||
| Adhesion and proteoglycans | ||
| ACAN | Aggrecan | Expression modulated by 13-cis retinoic acid in fibroblasts [166] |
| ICAM1 | Intercellular adhesion molecule 1 (CD54), human rhinovirus receptor | All-trans retinoic acid downregulates ICAM1 expression in bone marrow stromal cells [167] |
|
| ||
| Structural, dynamins, and kinesins | ||
| COL11A1 | Collagen, type XI, alpha 1 | Expression controlled by all-trans-retinoic acid [168] |
| DSC1 | Desmocollin 1 | Retinoic acid decreases expression in oral keratinocytes [169] |
| LMNA | Lamin A/C (nuclear) | Promoter contains a retinoic acid-responsive element (L-RARE) [170] |
|
| ||
| Ubiquitin | ||
| UBD | Ubiquitin D | All-trans retinoic acid activated the ubiquitin/proteasome pathway in human acute myeloid leukemia cell lines [171] |
| UBE2I | Ubiquitin-conjugating enzyme E2I (UBC9 homolog, yeast) | See above |
|
| ||
| DNA repair | ||
| XRCC1 | X-ray repair complementing defective repair in Chinese hamster cells 1 | N-[4-hydroxyphenyl] retinamide induces apoptosis in bladder cancer cell line and downregulates XRCC1 [172] |
|
| ||
| Cell cycle and tumour | ||
| CDC2 | Cell division cycle 2, G1 to S, and G2 to M | Activated by retinoic acid [173] |
|
| ||
| Miscellaneous metabolism | ||
| ACAD8 | Acyl-coenzyme A dehydrogenase family, member 8 | Catalyzes the dehydrogenation of acyl-CoA derivatives in the metabolism of fatty acids or branch chained amino acids. The encoded protein is a mitochondrial enzyme that functions in catabolism of the branched-chain amino acid valine. |
| ALDH18A1 | Aldehyde dehydrogenase 18 family, member A1 | NF the encoded protein catalyzes the reduction of glutamate to delta1-pyrroline-5-carboxylate, a critical step in the de novo biosynthesis of proline, ornithine and arginine. |
| ARSA | Arylsulfatase A: hydrolyzes cerebroside sulfate to cerebroside and sulphate | Increased urinary excretion of both arylsulfatases A and B is increased in cases of severe vitamin A deficiency coupled with malnutrition [174] |
| ELAVL4 | ELAV (embryonic lethal, abnormal vision, drosophila)-like 4 (Hu antigen D) | Inhibition reduces retinoic acid-induced neuronal differentiation of mouse embryonal carcinoma P19 cells [175] |
| SGPL1 | Sphingosine-1-phosphate lyase 1 | Treatment of F9 embryonal carcinoma cells with retinoic acid induces differentiation to primitive endoderm (PrE). This effect is attenuated by SGPL1 knockout [176]. |
|
| ||
| Miscellaneous | ||
| CELF2 | CUGBP, Elav-like family member 2 | Splicing regulated by retinoic acid [177] |
| CUBN | Cubilin (intrinsic factor-cobalamin receptor) | Expression regulated by all-trans-retinoic acid [178] |
| F13A1 | Coagulation factor XIII, A1 polypeptide | Vitamin A reduces factor XIII levels in rats fed an atherogenic diet [179]. |
| HHEX | Hematopoietically expressed homeobox | All-trans retinoic acid enhances expression in normal and tumorous mammary tissue [180] |
| NEDD9 | Neural precursor cell expressed, developmentally downregulated 9 | Downstream target of all-trans retinoic acid and its receptors in the human SH-SY5Y neuroblastoma cell line [181] |
| RELN | Reelin | Retinoic acid-induced differentiation of NT2 cells to hNT neurons increases reelin expression [182]. |
| RNR1 | RNA, ribosomal 1 | NF |
| RPS3A | Ribosomal protein S3A | Downregulated by retinoid-induced differentiation of HL-60 cells [183] |
| RUNX1 | Runt-related transcription factor 1 (acute myeloid leukemia 1; aml1 oncogene) | RUNX1 knockdown inhibits retinoid-induced differentiation of HL-60 myeloid leukaemia cells [184]. |
| SEPT3 | Septin 3 | Expressed in SH-SY5Y, after retinoic acid-induced differentiation [185] |
| SNCA | Synuclein, alpha (non-A4 component of amyloid precursor) | Vitamin A, beta-carotene and coenzyme Q10 inhibit the formation of synuclein fibrils [186] |
| SYN3 | Synapsin III | Synapsins including SYN3 are upregulated by retinoic acid-induced differentiation of NTera-2cl.D1 cells [187] |
| TARDBP | TAR DNA binding protein | NF |
| VCP | Valosin-containing protein | Retinoic acid receptor responder (RARRES1) regulates VCP expression in human prostatic epithelial cells [188] |
3.3. The Fox, the Rabbits, Gene, and Environmental Variables
This is an adaptation of Lees's classical population genetics example of the peppered moth, whose dark or pale colouring confers advantage or disadvantage depending upon the degree of industrial pollution that covers trees with soot. It has served to illustrate the concept of natural selection where, over time, dark genes become more common in polluted areas, an effect that could eventually lead to speciation [34].
On two islands one covered in snow and the other in black volcanic ash live an equal number of black and white rabbits and a family of foxes, who will find it easier to trap the black rabbits on the snowy island and the white rabbits on the island covered in black ash. Gene association studies would correctly identify the black and white genes as being protective or risk promoting depending upon the environment. The snow, the ash, or the fox, being equally present on each island, regardless of the toll of dead rabbits, could not be considered as risk factors. Genetic meta-analysis or pooled GWAS data would also rule out any genetic involvement, leaving no susceptibility genes, no risk factors, and no cause. However, a GWAS study, apportioning the genetic data in relation to ash, snow, and fox would be able to correctly surmise that the white gene is a risk factor on the ash-covered island, and the black gene a risk factor on the snowy island, as would have D. R. Lees. Again the fox is undetectable, being present in all compartments.
On other similar islands, live further populations of black and white rabbits with no fox, an equal number of deaths due to old age, and no reason to investigate either genes or risk factors. However, it is only by including this island, again partitioning GWAS data in relation to all variables, that the genes, the risk factors, and the cause can be correctly allotted their respective roles.
In this example, the genes and environmental variable are risk or protective factors for the cause as well as for the deaths, depending on circumstance. The genes or risk factors are not killing the rabbits, but are allowing the cause to do so. Nonstratified association studies would thus seem to be ill-suited to find important genes, risk factors, or causes, and the pursuit of greater statistical power may well be futile, although such strategies can find rare variants that may cause disease in a minority of patients, which is evidently useful. However, for the majority of cases, much could perhaps be gained from a reappraisal of existing data and by partitioning GWAS data in relation to the many known risk factors in each disease.
The situation is evidently more complex in polygenic diseases, where hundreds of interacting genes, many risk factors, and probably many causes are present. This is already appreciated, and several groups have analysed the statistical problems involved due to the mass of genes and risk factors [35–37]. However, it is likely that an appropriate selection of genes and risk factors could markedly affect the degree of risk. For example, the odds ratio for APOE4 was shown to be 1.67 in Alzheimer's disease patients without cerebral HSV-1 DNA and 16.8 in patients where viral DNA was detected [38]. The population genetics example, and the discussion below, suggests that certain susceptibility genes are restricted to risk factor subsets.
From the above, it would appear that a cause can be present in equal proportion in control and disease populations but should be able to produce the pathological features of the disease, and the disease incidence should be reduced where the causes are few. A cause can kill regardless of the genes (black or white) or risk factors (snow or volcanic ash) but its effects are tempered by a combination of the two (fox + snow + black gene or fox + ash + white gene = death and fox + snow + white gene or fox + ash + black gene, or no fox and any combination = life). The genes and risk factors are, however, both able to influence the cause.
In relation to Alzheimer's disease, beta-amyloid deposition can be produced by herpes simplex [189–191] or chlamydia pneumoniae infection [192, 193], hypercholesterolemia (which also causes cholinergic neuronal loss and memory deficits in rats [194–197]), by or hyperhomocysteinaemia, an effect reversed by folate and vitamin-B12 [198], by NGF deprivation [199], by reduced cerebral perfusion (hypoxia, cerebral ischaemia, or carotid artery occlusion [200–203]), as well as by experimental diabetes and streptozotocin [204, 205], oestrogen depletion [206], or vitamin A deficiency, which also reduces choline acetyltransferase activity in the forebrain [207]—all without the aid of any variant genes, in animal models. While none of the animal models faithfully reproduce the entire symptomatology of Alzheimer's disease, in the clinical setting these risk factors coexist to varying degrees, rendering the situation rather more complex.
The risk factors in Alzheimer's disease include herpes simplex infection [208] acting in combination with APOE4 [209], C. Pneumoniae [210, 211] or Helicobacter pylori infection [212, 213], mild hypercholesterolaemia [214], but declining cholesterol levels from midlife to late life [215], atherosclerosis of the carotid arteries, leptomeningeal arteries, or the circle of Willis, and stroke, leading to cerebral hypoperfusion [216–219], hyperhomocysteinaemia [220], type 2 diabetes and modified insulin metabolism [221], age-related loss of sex steroid hormones in both women and men [222], but high total oestradiol levels [223, 224], and vitamin A deficiency [225]. These factors may be confounded by interrelationships, and in some cases by the fact that death due to other causes—for example, atherosclerosis-related myocardial infarction or stroke may lead to an apparent paucity of comorbid risk factors in Alzheimer's disease groups at later ages.
The genes implicated in Alzheimer's disease are related to the herpes simplex life cycle [13, 226], bacterial and viral entry pathways, viral and pathogen defence (Table 1), and the immune network [227], cholesterol and lipoprotein pathways [11, 228], folate and homocysteine pathways [229], and insulin, or neurotrophin signalling pathways, steroid metabolism and receptors (Table 1 and 2), and vitamin A metabolism and function (Table 2).
The genes, risk factors and agents known to increase beta-amyloid deposition all concur, suggesting that Alzheimer's disease is multifactorial with many foxes, each with their respective genes and risk factors, any of which can lead to beta-amyloid deposition in multifarious ways. Each risk factor can act independently of any gene or other risk factor variant, in animal models—as with the fox. This in turn might suggest that it is not the risk promoting polymorphisms in the Alzheimer's disease patients that are crucial, as the risk factors can in any case promote beta-amyloid deposition, but the equivalent polymorphisms in the control group, that are providing protection; a subtle distinction that awaits characterisation of the functional effects of many different gene variants. The reasoning also suggests that beta-amyloid deposition is the consequence and not the cause of the many factors able to promote Alzheimer's disease. Anoxia, ischaemia, hypoglycaemia, hypercholesterolaemia, and vitamin A deficiency are all able to kill neurones, in some cases including cholinergic neurones, without the aid of beta amyloid.
3.4. Low Incidence of Alzheimer's Disease and Protective Factors
In relation to Alzheimer's disease, there is an island where longevity is increased, related to the nun study [231–234]. Nuns do not have children, (the number of pregnancies is a risk factor in Alzheimer's disease [235]), do not consume high concentrations of saturated fats (low cholesterol), and are unlikely to have sexually transmitted diseases or viral and other common pathogen diseases vectored by childhood infections (Herpes and chlamydia, inter alia). Their vitamin A levels and general health are sustained by a healthy diet, regular fish on Fridays, and exercise.
There are few strategies that have been shown to reduce the severity of Alzheimer's disease, once established. It has, however, been shown that Helicobacter pylori elimination increases the cognitive abilities and the lifespan of Alzheimer's disease patients [236]. In addition, two separate case reports have shown complete reversal of dementia in two patients diagnosed with Alzheimer's disease, by identification and eradication of the fungal pathogen Cryptococcus Neoformans [237, 238].The TNF antagonist, etanercept, has also been reported to produce a striking remedial effect on symptomatology, following perispinal application [239]. However, the use of TNF antagonists is also associated with an increased incidence of opportunistic bacterial, fungal, and viral infestations, including cytomegalovirus, and cryptococcal infections [240], perhaps a contraindication for their prolonged use.
A number of epidemiological studies have shown that the incidence of Alzheimer's disease can be reduced, although, once the disease is established, there is little evidence for any curative effects of any treatment other than the above. These protective factors are in most cases the obverse of the risk factors and include diets rich in fish or polyunsaturated fatty acids [241, 242], the Mediterranean diet [243] and the use of statins [244], which are counter to the effects of high cholesterol. A diet rich in fruit and vegetables is associated with reduced dementia incidence [245] and is able to sustain Vitamin A levels and reduce homocysteine levels in the elderly population [246]. High folate intake, which reduces homocysteine levels [247], and the use of nonsteroidal anti-inflammatories have also been reported to reduce risk [248]. Again these are related to the risk factors and to the genes, which may condition their success (cf. Vitamin E).
3.5. Relevance of These Factors to the Genes Identified in Genome-Wide Association Studies
Four major genes have been discovered prior to and from GWAS studies, APOE4, clusterin, complement receptor 1, and PICALM [6, 249]. The close relationships between these genes and herpes simplex infection have been the subject of a previous article [226]. APOE4 also favours the binding of C. Pneumoniae elementary bodies to host cells [250]. It is also a risk factor for hypercholesterolaemia, per se [251], and for carotid artery atherosclerosis in men with diabetes [252]. APOE4 is also the isoform least able to promote lipid efflux from neuronal cells [253], a factor that may enhance the cholesterol dependent cleavage of beta-amyloid by beta and gamma secretase [254]. It is also the least able isoform binding the vitamin A precursor retinyl palmitate [255] (see below). Complement receptor 1 is a pathogen receptor for both herpes simplex [256], and C. Neoformans [257] and also for the atherogenic pathogen, P. Gingivalis [258], a key cause of periodontitis/gum disease, which has also been implicated as a risk factor in dementia [259]. Both Helicobacter pylori and C. Pneumoniae [260] use the mannose-6-phosphate IGF2 receptor (inter alia) for entry. This binds to clusterin and its endocytosis is controlled by PICALM [226]. PICALM (phosphatidylinositol binding clathrin assembly protein), as its name implies, is involved in clathrin-mediated endocytosis [261], a process used by C. Pneumoniae to gain cellular entry [262], for the internalisation of herpes simplex glycoprotein D [263] or the cytomegalovirus chemokine receptor [264] and for the uptake of outer membrane vesicles from certain strains of H. pylori, into gastric epithelial cells [265]. Clathrin also associates with HHV-6 virions [266]. Clusterin is an inhibitor of the membrane attack complex that is inserted into microbial membranes causing death by lysis [267]. It is also a ligand for the retinol/lipoprotein receptor LRP2 [268], and the gene contains a retinoid response element (Table 2). Thus it would seem that the key role of these genes may be related to their ability to target multiple aspects of diverse risk factor networks.
3.6. Relationships between Risk Factors and a Key Role for Herpes Simplex Activation (Figure 1)
Figure 1.
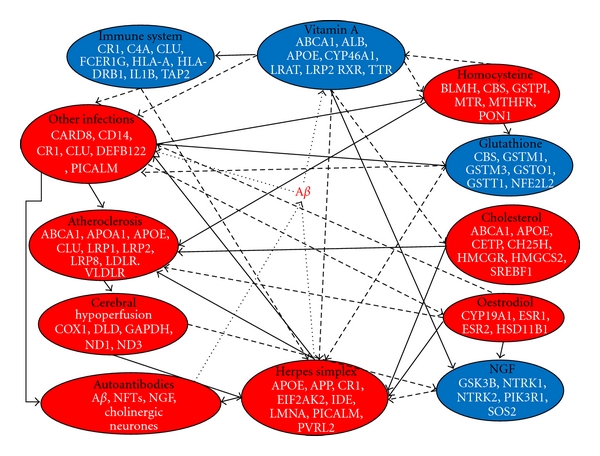
An environmental risk factor-gene interactome in Alzheimer's disease. Risk factors diminished in Alzheimer's disease (vitamin A deficiency, NGF levels, immune competence, and glutathione depletion) are shown in blue and those increased in red. Solid lines indicate a positive, and dashed or dotted lines a negative effect of risk factor X on risk factor Y. All risk factors feed into increased beta-amyloid deposition. A selection of susceptibility genes relevant to each process is shown (see Table 2 and http://www.polygenicpathways.co.uk/alzpolys.html.
Hypercholesterolaemia can evidently be related to other dietary risk factors such as saturated fat consumption, and to atherosclerosis. Docosahexaenoic acid increases total plasma cholesterol levels in hymans, but only in APOE4 carriers, an effect that may negate the cardioprotective effects of fish oil supplementation [269]. Helicobacter pylori infection also causes malabsorption of vitamin B12 and folate, leading to increased homocysteine levels, that can be restored by H. pylori eradication [270]. Homocysteine metabolism is also related to glutathione synthesis via the transsulfuration pathway (homocysteine→cysteine→glutathione). Increased levels of homocysteine and reduced levels of glutathione in Alzheimer's disease suggest impairments in the transsulfuration pathway [271]. Glutathione is a potent antiviral and bactericidal agent with effects targeted at herpes simplex and C. Pneumoniae, inter alia both of which also diminish glutathione levels in infected cells [27, 272, 273]. H. pylori expresses an enzyme, gamma-glutamyltranspeptidase that enables it to metabolise the host's extracellular glutamine and glutathione which are hydrolysed to glutamate, which is fed into the H. pylori Krebs cycle, resulting in diminished glutathione levels that can be restored by H. pylori elimination [27, 273]. Glutathione levels are reduced in Alzheimer's disease and many others [274].
In both coronary artery disease and carotid artery atherosclerosis, high plasma levels of homocysteine are positively correlated with C. Pneumoniae seropositivity suggesting a role for the bacterium in promoting high homocysteine levels. [275, 276]. Indeed carotid artery atherosclerosis is correlated with antibodies to C. Pneumoniae, and to a lesser extent with antibodies to H. pylori, but in this case, only in individuals with low social status [277].
The growth of C. Neoformans is attenuated by diethylstilbestrol and oestradiol but not by progesterone or testosterone [278]. Helicobacter pylori adsorbs a number of steroids including pregnenolone and two androgens (dehydroepiandrosterone and epiandrosterone and 3-hydroxylated oestrogens (oestrone and oestradiol). These are glucosylated and the glucosyl-steroid hormone derivatives used as membrane lipid components [279]. Oestradiol, androstenedione, and progesterone are all able to inhibit the growth of H. pylori [280].
These complex interactions, of which there are likely many more, suggest that in addition to epistasis and gene-environment interactions, environment-environment interactions have to be factored in to an already complex equation (cf. vitamin E).
Factors known to reactivate herpes simplex include heat [281], 17-beta oestradiol [282] and the inflammatory cytokine interleukin 6 [283] where a role for corticosterone has been proposed [284]. NGF deprivation [285] also reactivates the virus and NGF promotes viral latency via the TrkA receptor [286] (cf. neurotrophin signalling). Vitamin A supplementation in rats increases the cerebral levels of both NGF and BDNF [129] while oestrogen deficiency lowers cerebral NGF levels, an effect reversed by 17-beta oestradiol [287]. Transient cerebral ischaemia lowers NGF levels [288]. Hypoxia is also able to increase the replication of herpes simplex [289].
Fevers induced by diverse infections might thus be expected to reactivate herpes simplex, as well as cerebral hypoperfusion. IL6 plasma and CSF levels have been reported to be increased in Alzheimer's disease and the secretion of IL6 from monocytes is increased [290–292]. IL6 plasma levels are raised by infection with C. Pneumoniae [293] or Helicobacter pylori [294], and IL6 production in monocytes is stimulated by C. Neoformans [295]. Cortisol levels are also increased in the ageing population and in Alzheimer's disease [296, 297]. High levels of total oestradiol have been reported as a risk factor for Alzheimer's disease in both women and men [223, 224].
As so many other risk factors seem able to reactivate the virus, this may be a key precipitant for the final curtain. Herpes simplex viral DNA is present in Alzheimer's disease plaques [298], and the plaques and tangles in Alzheimer's disease contain a very high proportion of herpes simplex interacting proteins, as well as immune-related components. The presence of the complement membrane attack complex in neurones suggests that the neuronal destruction in Alzheimer's disease might well be related to the consequences of battle between the virus and the immune network that has eliminated the virus at a terrible cost of collateral neuronal damage [33]. IgM+ antibodies, which preferentially index HSV-1 reactivation, have been shown to be able to predict the future risk of developing Alzheimer's disease [208], and the ability of other risk factors, particularly other infections, to reactivate the virus suggests a complex interplay of genes and risk factors that funnel towards viral reactivation and plaque and tangle formation.
3.7. The Importance of Vitamin A
Low vitamin A levels are a problem in the ageing population, and even in successfully ageing persons can be observed in 50% of the population over the age of 80–85 [299] (cf. the fox). Low vitamin A levels are also a risk factor for Alzheimer's disease [225]. Vitamin A plays an important role in maintaining the immune system [300], many genes of which are implicated in Alzheimer's disease. APP is involved in the vitamin A arena, as a gamma57 gamma secretase cleavage product suppresses retinoid signalling [75].
The vitamin A derivative, retinoic acid, inhibits herpes simplex replication [301, 302] as well as chlamydial infection and growth [303]. Vitamin A also stunts the growth of Helicobacter pylori [304]. The effects of vitamin A on C. Neoformans do not appear to have been examined. However, glucuronoxylomannan, the polysaccharide component of the capsular material of cryptococcus neoformans, exhibits potent immunosuppressive properties. This compound downregulates TNF-alpha and IL-1beta, and upregulates the inhibitory cytokine IL-10, but also inhibits retinoic receptor (RORG) synthesis [305]. Retinoic acid is also able to lower plasma homocysteine levels via the induction of hepatic glycine N-methyltransferase. Homocysteine in contrast inhibits retinoic acid synthesis [306, 307].
Vitamin A levels are in fact higher in hypercholesterolemia patients [308]. This may perhaps be due to the fact that retinyl palmitate, the vitamin A precursor, like cholesterol, is also transported by lipoproteins in the blood, mainly in the VLDL fraction (which primarily consist of APOC2/APOE) and the LDL fraction (which primarily consists of APOB) [41]. Retinyl palmitate concentrations in the blood are affected by APOE polymorphisms and radiolabelled retinyl palmitate binding in total plasma and nonchylomicron fractions is least in APOE4+/+ carriers [255]. The aortic concentrations of triglycerides, total cholesterol, free and esterified cholesterol, and phospholipids are increased in vitamin A deficient rats, an effect reversed by vitamin A supplementation [144]
A large number of Alzheimer's disease genes are related to vitamin A (Table 2), and an even larger number responsive to retinoic acid via the action of RAR or RXR transcriptional control.
3.8. Autoantibodies to the Antimicrobial Peptide Beta Amyloid: Likely Derivation from Antibodies to Pathogens
Beta-amyloid is a potent antimicrobial peptide. Although not tested against C. Neoformans, H. pylori, or C. Pneumoniae, it was found to have broad spectrum activity against a variety of yeasts and bacteria, effects that were attenuated by anti-Aβ antibodies. [309]. Lactotransferrin is also an antimicrobial peptide that colocalises to plaques and tangle in the Alzheimer's disease brain [310] and other antimicrobial peptides include the susceptibility gene products cystatin C, defensin DEFB122, myeloperoxidase, and transferrin [88]. beta-amyloid, like acyclovir, also attenuates the stimulatory effects of HSV-1 on miRNA-146a levels in neuronal cells [311]. The antimicrobial and antiviral properties of beta amyloid are, however, likely to be abrogated by the presence of beta-amyloid antibodies in the sera of the ageing population [312] and in Alzheimer's disease [313].
As shown in Table 3, a number of pathogens implicated in Alzheimer's disease or its attendant risk factors, express proteins with a high degree of homology to beta-amyloid. These include proteins from HSV-1, HHV-6, the cytomegalovirus, C. Neoformans, H. pylori, C. Pneumoniae, B. Burgdorferi and, P. Gingivalis. Antibodies to B. Burgdorferi [314] and C. Pneumoniae [210] and Herpes simplex and HHV-6 viral DNA [298, 315] have all been reported in or around Alzheimer's disease plaques, and antibodies to H. pylori recovered from Alzheimer's disease serum and cerebrospinal fluid [316]. A recent study showed that P. Gingivalis antibodies, cross-reactive with human HSP60, were observed in 100% of a sample of 20 atherosclerosis patients [317]. The immune system is not designed to raise antibodies to a self-protein, and this high degree of homology suggests that the autoantibodies to beta-amyloid are created by antibodies to homologous pathogens' proteins.
Table 3.
Viral, bacterial, and fungal protein homology with beta-amyloid; beta-amyloid segments were compared with Borrelia Burgdorferi, C. Neoformans, C. Pneumoniae, H. Pylori, P. Gingivalis, and herpes viruses (HSV1, HHV6, and cytomegalovirus) proteomes by BLAST analysis. The B cell and T cell antigenicity indices are shown, and those above the server set threshold of 0.35 (B cell epitope) or 0.5 (T cell epitope) are highlighted in bold. The first column shows the amino acid sequence of beta-amyloid1-42 and the alignments with pathogen proteins are shown. Spaces represent nonidentical amino acids and + signs amino acids with similar physicochemical properties. Only highly antigenic regions of pentapeptides or more were processed. The VGGVV sequence, antibodies to which label beta-amyloid in brain tissue, despite relatively low antigenicity, has already been reported to be identical to proteins expressed by 69 viruses including HSV-1, HSV-2, and HHV6 [230].
| B cell | T cell | Alignments | |
|---|---|---|---|
| D | 0.41 | 0.04 | +AE HDSG+ C. Neoformans DAE F H+SG EV Borrelia burgdorferi DAEF H. Pylori DA FRH H. Pylori +AE RH HSV-1 D FR DS HHV-6 +AEFR P. Gingivalis DA EFRHD and +AEFR +SG C. Pneumoniae |
| A | 0.35 | 0.78 | AEFR D GY+V C. Neoformans AEF D S YE H. pylori AE+RH+ H. pylori AEF H+ Borrelia burgdorferi AEFR HD Cytomegalovirus AE R SG HSV-1 AE+ HD HHV-6 A+F H+S and AEFR P. Gingivalis AEF DSG C. Pneumoniae |
| E | 0.62 | 0.02 | EFRHD H. Pylori EF DSG HHV-6 EFR DS Borrelia Burgdorferi EF R DS YE C. Neoformans E R DSGY V P. Gingivalis EF SGYEV C. Pneumoniae |
| F | 0.73 | 0.93 | FRHDS C. Neoformans +RH SGY++ Borrelia burgdorferi F HD EV H. Pylori F H+SG H. Pylori FR SGY Cytomegalovirus +RHDS P. Gingivalis F H+SGY C. Pneumonia |
| R | 0.85 | 0.05 | R D GYEV C. Neoformans R SGYE H. pylori RHDS Y V H. pylori RH+ GY Borrelia burgdorferi RHDSG Cytomegalovirus RHD YE cytomegalovirus RH SG HSV-1 RHDS HHV-6 R+DS Y+ P. Gingivalis |
| H | 0.57 | 0.14 | HDSGY C. Neoformans HD G EV H. pylori +DSGY H. pylori H+SG Y+V Borrelia burgdorferi H+SG HSV-1 HDSG P. Gingivalis ++SGY+V C. Pneumoniae |
| D | 0.69 | 0.03 | DSGY+V C. Neoformans +SG+EV H. pylori DSGY HSV-1 DSG+EV P. Gingivalis DSGY V C. Pneumoniae |
| S | 0.38 | 0.02 | SGYEV P. Gingivalis SGYE H. pylori SGY++ C. Neoformans SG+EV C. Pneumoniae |
| G | 0.63 | 0.04 | GYEVH H. pylori GYE V KL+ Borrelia Burgdorferi GYE LV and GY++ + LV C. Neoformans GYEV P. Gingivalis GYEV and GY HH C. Pneumoniae |
| Y | 0.56 | 0.96 | YE HH and YE+ HQ and Y++H Q and YE HHQ H. pylori YEVH Cytomegalovirus YE+ KL Borrelia Burgdorferi YE + QK FC. Neoformans Y++H H+K P. Gingivalis Y+V +Q LV C. Pneumoniae |
| E | 0.58 | 0.02 | EV +QK H. pylori EV HQ L Cytomegalovirus EV +KL Borrelia Burgdorferi EV Q LV C. Neoformans EV KLV P. Gingivalis EV QKLV C. Pneumoniae |
| V | 0.35 | 0.90 | .+H QK H. pylori V HQ LV Cytomegalovirus VH QK+V HHV-6 VH KL Borrelia Burgdorferi +HH LV C. Neoformans VH + LV P. Gingivalis V HQKL C. Pneumoniae |
| H | −0.17 | 0.10 | HHQK H. pylori and C. Pneumoniae HH KL Cytomegalovirus HH KL P. Gingivalis |
| H | −0.66 | 0.11 | HQKL+ Borreli Burgdorferi HQKL C. Pneumoniae and HSV-1 +QKLV P. Gingivalis |
| Q | −1.03 | 0.03 | QKLV C. Neoformans and P. Gingivalisand C. Pneumoniae |
| K | −1.47 | 0.93 | KLVFF H. pylori: Cryptococcus neoformans Borrelia Burgdorferi Chlamydophila pneumoniae KLVF Human herpesvirus 1 |
| L | −1.34 | 0.95 | LVFF Human herpesvirus 5: Human herpesvirus 6 |
| V | −1.20 | 0.68 | |
| F | −0.93 | 0.69 | |
| F | −0.98 | 0.74 | |
| A | −0.82 | 0.05 | |
| E | −0.31 | 0.05 | |
| D | 0.23 | 0.11 | |
| V | 0.81 | 0.88 | VGSNK Borrelia burgdorferi Cryptococcus neoformans Porphyromonas gingivalis +GSNK Cytomegalovirus VGSN Helicobacter pylori Chlamydophila pneumoniae |
| G | 1.24 | 0.03 | GSNK Helicobacter Pylori Chlamydophila pneumoniae |
| S | 1.22 | 0.03 | |
| N | 0.90 | 0.03 | |
| K | 0.36 | 0.30 | |
| G | 0.30 | 0.10 | |
| A | −0.24 | 0.05 | |
| I | −0.58 | 0.07 | |
| I | −1.00 | 0.13 | |
| G | −1.14 | 0.03 | |
| L | −1.19 | 0.72 | |
| M | −1.23 | 0.13 | |
| V | −1.16 | 0.23 | VGGVV 69 viruses/phages |
| G | −0.97 | 0.03 | |
| G | −1.02 | 0.03 | |
| V | −0.63 | 0.23 | |
| V | −0.45 | 0.33 | |
| I | −0.80 | 0.95 | |
| A | −1.06 | 0.83 |
Several other autoantibodies have been reported in Alzheimer's disease, including targets such as nerve growth factor [318], cholinergic neurones [319], the choroid plexus [320], and neurofibrillary tangles, inter alia [321]. The very extensive sharing of viral and bacterial protein sequences with the human proteome [230, 322–324] suggests that these too might be derived from cross-reactive microbial antigens. Again the ability to create autoantibodies is conditioned by genes, particularly HLA-antigens [325, 326]. Autoantibodies are often regarded as an epiphenomenon, but their ability to traverse the blood-brain barrier [327], and the recent recognition of their ability to enter cells [328] casts them in a new light as pathological immunopharmacological agents able to block the function of their target proteins: this has indeed been shown for Alzheimer's disease-derived ATP synthase autoantibodies which block ATP synthesis and cause apoptosis in neuroblastoma cells [329].
4. Summary
The classical population genetics example of the foxes and rabbits illustrates how genes and risk factors can differentially permit or disallow the effects of a causative agent, depending on a permutation of circumstance. Applying this model to Alzheimer's disease also suggests that many of the environmental risk factors in Alzheimer's disease are in fact causative agents, at least in terms of an ability to produce beta-amyloid deposition, per se, as shown in nontransgenic animal models. Their effects are also clearly related to other risk factors and genes. This would infer that the susceptibility genes in Alzheimer's disease permit the actions of these agents but, perhaps more importantly, that polymorphisms in the control population do not. Functional characterisation of these control variants may provide important clues to overall methods of protection.
Many of these risk factors are avoidable or amenable to therapy. Diet is already known to be an important risk/protective factor with regard to the incidence of Alzheimer's disease. For example there is clear evidence that the omega-3 fatty acid docosahexaenoic acid (DHA), a component of fish and the Mediterranean diet, also protective factors [243, 330], is associated with a reduced risk of dementia [331], although a recent study with DHA in mild to moderate Alzheimer's disease, failed to show disease arrest or diminution [332]. However, in agreement with epidemiology, DHA significantly benefited two measures of cognition in mild to moderate non-ApoE4 carriers [333]. High vitamin A and low homocysteine levels are related to a high intake of fruit and vegetables in elderly patients [246]. Fruit and vegetable juice consumption is also associated with reduced Alzheimer's disease incidence [334].
Given the fact that the potential causes of Alzheimer's disease appear to be multifactorial, perhaps a multifactorial therapeutic effort is also needed. Such approaches might include a greater attention to diet, homocysteine and cholesterol levels, vitamin A supplementation where necessary, and the regular detection and elimination of herpes simplex, B. Burgdorferi, C. Pneumoniae, H. pylori, C. Neoformans, and other pathogens in the ageing population. The removal of beta-amyloid antibodies and of others prevalent in Alzheimer's disease might also be of benefit. These are simple preventive measures, requiring public health attention, whose corporate instigation might markedly reduce the incidence, and perhaps halt or reverse the progression, of Alzheimer's disease.
References
- 1.Bertram L, Tanzi RE. Alzheimer’s disease: one disorder, too many genes? Human Molecular Genetics. 2004;13(1):R135–R141. doi: 10.1093/hmg/ddh077. [DOI] [PubMed] [Google Scholar]
- 2.Cichon S, Craddock N, Daly M, et al. Genomewide association studies: history, rationale, and prospects for psychiatric disorders. American Journal of Psychiatry. 2009;166(5):540–556. doi: 10.1176/appi.ajp.2008.08091354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vacic V, McCarthy S, Malhotra D, et al. Duplications of the neuropeptide receptor gene VIPR2 confer significant risk for schizophrenia. Nature. 2011;471(7339):499–503. doi: 10.1038/nature09884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bondy B. Genetics in psychiatry: are the promises met? The World Journal of Biological Psychiatry. 2011;12(2):81–88. doi: 10.3109/15622975.2010.546428. [DOI] [PubMed] [Google Scholar]
- 5.Li HL, Shi SS, Guo QH, et al. PICALM and CR1 variants are not associated with sporadic Alzheimer's disease in Chinese patients. doi: 10.3233/JAD-2011-101917. Journal of Alzheimer's Disease. http://www.ncbi.nlm.nih.gov/pubmed/21358043. In press. [DOI] [PubMed] [Google Scholar]
- 6.Jun G, Naj AC, Beecham GW, et al. Meta-analysis confirms CR1, CLU, and PICALM as Alzheimer disease risk loci and reveals interactions with APOE genotypes. Archives of Neurology. 2010;67(12):1473–1484. doi: 10.1001/archneurol.2010.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Talmud PJ, Yiannakouris N, Humphries SE. Lipoprotein association studies: taking stock and moving forward. Current Opinion in Lipidology. 2011;22(2):106–112. doi: 10.1097/MOL.0b013e3283423f81. [DOI] [PubMed] [Google Scholar]
- 8.Handel AE, Williamson AJ, Disanto G, Handunnetthi L, Giovannoni G, Ramagopalan SV. An updated meta-analysis of risk of multiple sclerosis following infectious mononucleosis. PLoS ONE. 2010;5(9):1–5. doi: 10.1371/journal.pone.0012496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ingram G, Bugert JJ, Loveless S, Robertson NP. Anti-EBNA-1 IgG is not a reliable marker of multiple sclerosis clinical disease activity. European Journal of Neurology. 2010;17(11):1386–1389. doi: 10.1111/j.1468-1331.2010.03083.x. [DOI] [PubMed] [Google Scholar]
- 10.Franciotta D, Bestetti A, Sala S, et al. Broad screening for human herpesviridae DNA in multiple sclerosis cerebrospinal fluid and serum. Acta Neurologica Belgica. 2009;109(4):277–282. [PubMed] [Google Scholar]
- 11.Papassotiropoulos A, Wollmer MA, Tsolaki M, et al. A cluster of cholesterol-related genes confers susceptibility for Alzheimer’s disease. Journal of Clinical Psychiatry. 2005;66(7):940–947. [PubMed] [Google Scholar]
- 12.Wu X, Gu J, Grossman HB, et al. Bladder cancer predisposition: a multigenic approach to DNA-repair and cell-cycle-control genes. American Journal of Human Genetics. 2006;78(3):464–479. doi: 10.1086/500848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carter CJ. Interactions between the products of the Herpes simplex genome and Alzheimer’s disease susceptibility genes: relevance to pathological-signalling cascades. Neurochemistry International. 2008;52(6):920–934. doi: 10.1016/j.neuint.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 14.Carter CJ. Schizophrenia susceptibility genes directly implicated in the life cycles of pathogens: cytomegalovirus, influenza, herpes simplex, rubella, and Toxoplasma gondii . Schizophrenia bulletin. 2009;35(6):1163–1182. doi: 10.1093/schbul/sbn054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hemilä H, Kaprio J. Vitamin E supplementation and pneumonia risk in males who initiated smoking at an early age: effect modification by body weight and dietary vitamin C. Nutrition Journal. 2008;7(1, article 33) doi: 10.1186/1475-2891-7-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hemilä H, Kaprio J. Modification of the effect of vitamin E supplementation on the mortality of male smokers by age and dietary vitamin C. American Journal of Epidemiology. 2009;169(8):946–953. doi: 10.1093/aje/kwn413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hemilä H, Kaprio J. Vitamin E may affect the life expectancy of men, depending on dietary vitamin C intake and smoking. Age and Ageing. 2011;40(2):215–220. doi: 10.1093/ageing/afq178. [DOI] [PubMed] [Google Scholar]
- 18.Ferreira IL, Resende R, Ferreiro E, Rego AC, Pereira CF. Multiple defects in energy metabolism in Alzheimer's disease. Current Drug Targets. 2010;11(10):1193–1206. doi: 10.2174/1389450111007011193. [DOI] [PubMed] [Google Scholar]
- 19.Facheris M, Beretta S, Ferrarese C. Peripheral markers of oxidative stress and excitotoxicity in neurodegenerative disorders: tools for diagnosis and therapy? Journal of Alzheimer’s Disease. 2004;6(2):177–184. doi: 10.3233/jad-2004-6210. [DOI] [PubMed] [Google Scholar]
- 20.Goto S, Bono H, Ogata H, et al. Organizing and computing metabolic pathway data in terms of binary relations. Pacific Symposium on Biocomputing. 1997:175–186. [PubMed] [Google Scholar]
- 21.Larsen JE, Lund O, Nielsen M. Improved method for predicting linear B-cell epitopes. Immunome Research. 2006;2, article 2 doi: 10.1186/1745-7580-2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Altschul SF, Madden TL, Schäffer AA, et al. Gapped BLAST and PSI-BLAST: a new generation of protein database search programs. Nucleic Acids Research. 1997;25(17):3389–3402. doi: 10.1093/nar/25.17.3389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nielsen M, Lundegaard C, Lund O, Keşmir C. The role of the proteasome in generating cytotoxic T-cell epitopes: insights obtained from improved predictions of proteasomal cleavage. Immunogenetics. 2005;57(1-2):33–41. doi: 10.1007/s00251-005-0781-7. [DOI] [PubMed] [Google Scholar]
- 24.Takaoka A, Shinohara S. DNA sensors in innate immune system. Uirusu. 2008;58(1):37–46. doi: 10.2222/jsv.58.37. [DOI] [PubMed] [Google Scholar]
- 25.Chattopadhyay S, Marques JT, Yamashita M, et al. Viral apoptosis is induced by IRF-3-mediated activation of Bax. EMBO Journal. 2010;29(10):1762–1773. doi: 10.1038/emboj.2010.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murillo LS, Morré SA, Peña AS. Toll-like receptors and NOD/CARD proteins: pattern recognition receptors are key elements in the regulation of immune response. Drugs of Today. 2003;39(6):415–438. [PubMed] [Google Scholar]
- 27.Oijen AH, Verhulst ML, Roelofs HM, Peters WH, de Boer WA, Jansen JB. Eradication of Helicobacter pylori restores glutathione S-transferase activity and glutathione levels in antral mucosa. Japanese Journal of Cancer Research. 2001;92(12):1329–1334. doi: 10.1111/j.1349-7006.2001.tb02157.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fraternale A, Paoletti MF, Casabianca A, et al. GSH and analogs in antiviral therapy. Molecular Aspects of Medicine. 2009;30(1-2):99–110. doi: 10.1016/j.mam.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 29.Zhang YN, Duan KM. Glutathione exhibits antibacterial activity and increases tetracycline efficacy against Pseudomonas aeruginosa . Science in China Series C. 2009;52(6):501–505. doi: 10.1007/s11427-009-0074-8. [DOI] [PubMed] [Google Scholar]
- 30.Páez PL, Becerra MC, Albesa I. Effect of the association of reduced glutathione and ciprofloxacin on the antimicrobial activity in Staphylococcus aureus . FEMS Microbiology Letters. 2010;303(1):101–105. doi: 10.1111/j.1574-6968.2009.01867.x. [DOI] [PubMed] [Google Scholar]
- 31.Nakayama M, Hisatsune J, Yamasaki E, et al. Helicobacter pylori VacA-induced inhibition of GSK3 through the PI3K/Akt signaling pathway. Journal of Biological Chemistry. 2009;284(3):1612–1619. doi: 10.1074/jbc.M806981200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Takenaka R, Yokota K, Ayada K, et al. Helicobacter pylori heat-shock protein 60 induces inflammatory responses through the Toll-like receptor-triggered pathway in cultured human gastric epithelial cells. Microbiology. 2004;150(12):3913–3922. doi: 10.1099/mic.0.27527-0. [DOI] [PubMed] [Google Scholar]
- 33.Carter CJ. Alzheimer's disease plaques and tangles: cemeteries of a Pyrrhic victory of the immune defence network against herpes simplex infection at the expense of complement and inflammation-mediated neuronal destruction. Neurochemistry International. 2011;58(3):301–320. doi: 10.1016/j.neuint.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 34.Lees DR. Genetic control of the melanic form insularia of the peppered moth biston betularia (L.) Nature. 1968;220(5173):1249–1250. doi: 10.1038/2201249a0. [DOI] [PubMed] [Google Scholar]
- 35.Figueiredo JC, Lewinger JP, Song C, et al. Genotype-environment interactions in MSS/MSI-low colorectal cancer: results from a genome-wide association study. Cancer Epidemiology, Biomarkers & Prevention. 2011;20:p. 758. doi: 10.1158/1055-9965.EPI-10-0675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oexle K, Meitinger T. Sampling GWAS subjects from risk populations. Genetic Epidemiology. 2011;35(3):148–153. doi: 10.1002/gepi.20562. [DOI] [PubMed] [Google Scholar]
- 37.Aschard H, Hancock DB, London SJ, Kraft P. Genome-wide meta-analysis of joint tests for genetic and gene-environment interaction effects. Human Heredity. 2010;70(4):292–300. doi: 10.1159/000323318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Itzhaki RF, Lin WR, Shang D, Wilcock GK, Faragher B, Jamieson GA. Herpes simplex virus type 1 in brain and risk of Alzheimer’s disease. Lancet. 1997;349(9047):241–244. doi: 10.1016/S0140-6736(96)10149-5. [DOI] [PubMed] [Google Scholar]
- 39.Goodman DS. Plasma retinol-binding protein. Annals of the New York Academy of Sciences. 1980;348:378–390. doi: 10.1111/j.1749-6632.1980.tb21314.x. [DOI] [PubMed] [Google Scholar]
- 40.Liang Y, Lin S, Beyer TP, et al. A liver X receptor and retinoid X receptor heterodimer mediates apolipoprotein E expression, secretion and cholesterol homeostasis in astrocytes. Journal of Neurochemistry. 2004;88(3):623–634. doi: 10.1111/j.1471-4159.2004.02183.x. [DOI] [PubMed] [Google Scholar]
- 41.Schindler R, Klopp A. Transport of esterified retinol in fasting human blood. International Journal for Vitamin and Nutrition Research. 1986;56(1):21–27. [PubMed] [Google Scholar]
- 42.Naylor HM, Newcomer ME. The structure of human retinol-binding protein (RBP) with its carrier protein transthyretin reveals an interaction with the carboxy terminus of RBP. Biochemistry. 1999;38(9):2647–2653. doi: 10.1021/bi982291i. [DOI] [PubMed] [Google Scholar]
- 43.Boukhtouche F, Mariani J, Tedgui A. The "CholesteROR" protective pathway in the vascular system. Arteriosclerosis, Thrombosis, and Vascular Biology. 2004;24(4):637–643. doi: 10.1161/01.ATV.0000119355.56036.de. [DOI] [PubMed] [Google Scholar]
- 44.Sousa MM, Berglund L, Saraiva MJ. Transthyretin in high density lipoproteins: association with apolipoprotein A-I. Journal of Lipid Research. 2000;41(1):58–65. [PubMed] [Google Scholar]
- 45.Smeland S, Kolset SO, Lyon M, Norum KR, Blomhoff R. Binding of perlecan to transthyretin in vitro. Biochemical Journal. 1997;326(3):829–836. doi: 10.1042/bj3260829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kiorpes TC, Anderson RS, Wolf G. Effect of vitamin A deficiency on glycosylation of rat serum α-macroglobulin. Journal of Nutrition. 1981;111(12):2059–2068. doi: 10.1093/jn/111.12.2059. [DOI] [PubMed] [Google Scholar]
- 47.Koldamova RP, Lefterov IM, Ikonomovic MD, et al. 22R-hydroxycholesterol and 9-cis-retinoic acid induce ATP-binding cassette transporter A1 expression and cholesterol efflux in brain cells and decrease amyloid β secretion. Journal of Biological Chemistry. 2003;278(15):13244–13256. doi: 10.1074/jbc.M300044200. [DOI] [PubMed] [Google Scholar]
- 48.During A, Harrison EH. Mechanisms of provitamin A (carotenoid) and vitamin A (retinol) transport into and out of intestinal Caco-2 cells. Journal of Lipid Research. 2007;48(10):2283–2294. doi: 10.1194/jlr.M700263-JLR200. [DOI] [PubMed] [Google Scholar]
- 49.Reboul E, Trompier D, Moussa M, et al. ATP-binding cassette transporter A1 is significantly involved in the intestinal absorption of alpha- and gamma-tocopherol but not in that of retinyl palmitate in mice. The American Journal of Clinical Nutrition. 2009;89(1):177–184. doi: 10.3945/ajcn.2008.26559. [DOI] [PubMed] [Google Scholar]
- 50.Gaemers IC, Van Pelt AMM, Themmen APN, De Rooij DG. Isolation and characterization of all-trans-retinoic acid-responsive genes in the rat testis. Molecular Reproduction and Development. 1998;50(1):1–6. doi: 10.1002/(SICI)1098-2795(199805)50:1<1::AID-MRD1>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 51.Morales CR, Griswold MD. Variations in the level of transferrin and SGP-2 mRNAs in Sertoli cells of vitamin A-deficient rats. Cell and Tissue Research. 1991;263(1):125–130. doi: 10.1007/BF00318407. [DOI] [PubMed] [Google Scholar]
- 52.Lee SK, Choi HS, Song MR, Lee MO, Lee JW. Estrogen receptor, a common interaction partner for a subset of nuclear receptors. Molecular Endocrinology. 1998;12(8):1184–1192. doi: 10.1210/mend.12.8.0146. [DOI] [PubMed] [Google Scholar]
- 53.Adly MA. Expression of the carrier protein transthyretin and its receptor megalin in human skin: preliminary findings. British Journal of Dermatology. 2010;162(1):213–215. doi: 10.1111/j.1365-2133.2009.09519.x. [DOI] [PubMed] [Google Scholar]
- 54.Christensen EI, Moskaug JO, Vorum H, et al. Evidence for an essential role of megalin in transepithelial transport of retinol. Journal of the American Society of Nephrology. 1999;10(4):685–695. doi: 10.1681/ASN.V104685. [DOI] [PubMed] [Google Scholar]
- 55.Ambroziak W, Izaguirre G, Pietruszko R. Metabolism of retinaldehyde and other aldehydes in soluble extracts of human liver and kidney. Journal of Biological Chemistry. 1999;274(47):33366–33373. doi: 10.1074/jbc.274.47.33366. [DOI] [PubMed] [Google Scholar]
- 56.Pinaire J, Chou WY, Morton M, et al. Identification of a retinoid receptor response element in the human aldehyde dehydrogenase-2 promoter. Alcoholism. 2003;27(12):1860–1866. doi: 10.1097/01.ALC.0000100941.86227.4F. [DOI] [PubMed] [Google Scholar]
- 57.Wang Y, Kumar N, Crumbley C, Griffin PR, Burris TP. A second class of nuclear receptors for oxysterols: regulation of RORalpha and RORgamma activity by 24S-hydroxycholesterol (cerebrosterol) Biochimica et Biophysica Acta. 2010;1801(8):917–923. doi: 10.1016/j.bbalip.2010.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chen H, Juchau MR. Recombinant human glutathione S-transferases catalyse enzymic isomerization of 13-cis-retinoic acid to all-trans-retinoic acid in vitro. Biochemical Journal. 1998;336(1):223–226. doi: 10.1042/bj3360223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Breithaupt DE, Bamedi A, Wirt U. Carotenol fatty acid esters: easy substrates for digestive enzymes? Comparative Biochemistry and Physiology—B. 2002;132(4):721–728. doi: 10.1016/s1096-4959(02)00096-9. [DOI] [PubMed] [Google Scholar]
- 60.Harrison EH. Lipases and carboxylesterases: possible roles in the hepatic utilization of vitamin A. Journal of Nutrition. 2000;130(2):340S–344S. doi: 10.1093/jn/130.2.340S. [DOI] [PubMed] [Google Scholar]
- 61.Woods A, James CG, Wang G, Dupuis H, Beier F. Control of chondrocyte gene expression by actin dynamics: a novel role of cholesterol/Ror-α signalling in endochondral bone growth. Journal of Cellular and Molecular Medicine. 2009;13(9):3497–3516. doi: 10.1111/j.1582-4934.2009.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gong X, Tsai SW, Yan B, Rubin LP. Cooperation between MEF2 and PPARγ in human intestinal β,β-carotene 15, 15′-monooxygenase gene expression. BMC Molecular Biology. 2006;7, article 7 doi: 10.1186/1471-2199-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Johnson DR, Lovett JM, Hirsch M, Xia F, Chen JD. NuRD complex component Mi-2beta binds to and represses RORgamma-mediated transcriptional activation. Biochemical and Biophysical Research Communications. 2004;318(3):714–718. doi: 10.1016/j.bbrc.2004.04.087. [DOI] [PubMed] [Google Scholar]
- 64.Zhang XH, Zheng B, Han M, Miao SB, Wen JK. Synthetic retinoid Am80 inhibits interaction of KLF5 with RARα through inducing KLF5 dephosphorylation mediated by the PI3K/Akt signaling in vascular smooth muscle cells. FEBS Letters. 2009;583(8):1231–1236. doi: 10.1016/j.febslet.2009.03.016. [DOI] [PubMed] [Google Scholar]
- 65.McNamara P, Seo SB, Rudic RD, Sehgal A, Chakravarti D, FitzGerald GA. Regulation of CLOCK and MOP4 by nuclear hormone receptors in the vasculature: a humoral mechanism to reset a peripheral clock. Cell. 2001;105(7):877–889. doi: 10.1016/s0092-8674(01)00401-9. [DOI] [PubMed] [Google Scholar]
- 66.Crumbley C, Wang Y, Kojetin DJ, Burris TP. Characterization of the core mammalian clock component, NPAS2, as a REV-ERBalpha/RORalpha target gene. The Journal of Biological Chemistry. 2010;285(46):35386–35392. doi: 10.1074/jbc.M110.129288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pavri R, Lewis B, Kim TK, et al. PARP-1 determines specificity in a retinoid signaling pathway via direct modulation of mediator. Molecular Cell. 2005;18(1):83–96. doi: 10.1016/j.molcel.2005.02.034. [DOI] [PubMed] [Google Scholar]
- 68.Gianni’ M, Boldetti A, Guarnaccia V, et al. Inhibition of the peptidyl-prolyl-isomerase Pin1 enhances the responses of acute myeloid leukemia cells to retinoic acid via stabilization of RARα and PML-RARα . Cancer Research. 2009;69(3):1016–1026. doi: 10.1158/0008-5472.CAN-08-2603. [DOI] [PubMed] [Google Scholar]
- 69.Kakizawa T, Miyamoto T, Ichikawa K, et al. Functional interaction between Oct-1 and retinoid X receptor. Journal of Biological Chemistry. 1999;274(27):19103–19108. doi: 10.1074/jbc.274.27.19103. [DOI] [PubMed] [Google Scholar]
- 70.Gorla-Bajszczak A, Juge-Aubry C, Pernin A, Burger AG, Meier CA. Conserved amino acids in the ligand-binding and tau(i) domains of the peroxisome proliferator-activated receptor alpha are necessary for heterodimerization with RXR. Molecular and Cellular Endocrinology. 1999;147(1-2):37–47. doi: 10.1016/s0303-7207(98)00217-2. [DOI] [PubMed] [Google Scholar]
- 71.Wang T, Xu J, Yu X, Yang R, Han ZC. Peroxisome proliferator-activated receptor gamma in malignant diseases. Critical Reviews in Oncology / Hematology. 2006;58(1):1–14. doi: 10.1016/j.critrevonc.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 72.Muscat GEO, Mynett-Johnson L, Dowhan D, Downes M, Griggs R. Activation of myoD gene transcription by 3,5,3’-triiodo-L-thyronine: a direct role for the thyroid hormone and retinoid X receptors. Nucleic Acids Research. 1994;22(4):583–591. doi: 10.1093/nar/22.4.583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhu D, Wang C, Liu B, Wu Y, Zhong L, Wang C. Interaction between nuclear localization signal-retinoic acid receptor alpha and Ubiquilin 1. Journal of Central South University. 2010;35(7):649–654. doi: 10.3969/j.issn.1672-7347.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 74.Koszewski NJ, Herberth J, Malluche HH. Retinoic acid receptor gamma 2 interactions with vitamin D response elements. Journal of Steroid Biochemistry and Molecular Biology. 2010;120(4-5):200–207. doi: 10.1016/j.jsbmb.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 75.Gao Y, Pimplikar SW. The γ-secretase-cleaved C-terminal fragment of amyloid precursor protein mediates signaling to the nucleus. Proceedings of the National Academy of Sciences of the United States of America. 2001;98(26):14979–14984. doi: 10.1073/pnas.261463298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Koryakina A, Aeberhard J, Kiefer S, Hamburger M, Küenzi P. Regulation of secretases by all-trans-retinoic acid. FEBS Journal. 2009;276(9):2645–2655. doi: 10.1111/j.1742-4658.2009.06992.x. [DOI] [PubMed] [Google Scholar]
- 77.Sarkar SN, Das HK. Regulatory roles of presenilin-1 and nicastrin in neuronal differentiation during in vitro neurogenesis. Journal of Neurochemistry. 2003;87(2):333–343. doi: 10.1046/j.1471-4159.2003.02006.x. [DOI] [PubMed] [Google Scholar]
- 78.Flood F, Sundström E, Samuelsson EB, et al. Presenilin expression during induced differentiation of the human neuroblastoma SH-SY5Y cell line. Neurochemistry International. 2004;44(7):487–496. doi: 10.1016/j.neuint.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 79.Uemura K, Kitagawa N, Kohno R, et al. Presenilin 1 mediates retinoic acid-induced differentiation of SH-SY5Y cells through facilitation of Wnt signaling. Journal of Neuroscience Research. 2003;73(2):166–175. doi: 10.1002/jnr.10641. [DOI] [PubMed] [Google Scholar]
- 80.Kitching R, Qi S, Li V, Raouf A, Vary CPH, Seth A. Coordinate gene expression patterns during osteoblast maturation and retinoic acid treatment of MC3T3-E1 cells. Journal of Bone and Mineral Metabolism. 2002;20(5):269–280. doi: 10.1007/s007740200039. [DOI] [PubMed] [Google Scholar]
- 81.Kuo HS, Hsu FN, Chiang MC, et al. The role of Cdk5 in retinoic acid-induced apoptosis of cervical cancer cell line. Chinese Journal of Physiology. 2009;52(1):23–30. doi: 10.4077/cjp.2009.amg067. [DOI] [PubMed] [Google Scholar]
- 82.Jämsä A, Hasslund K, Cowburn RF, Bäckström A, Vasänge M. The retinoic acid and brain-derived neurotrophic factor differentiated SH-SY5Y cell line as a model for Alzheimer's disease-like tau phosphorylation. Biochemical and Biophysical Research Communications. 2004;319(3):993–1000. doi: 10.1016/j.bbrc.2004.05.075. [DOI] [PubMed] [Google Scholar]
- 83.Monteiro MC, Wdziekonski B, Villageois P, et al. Commitment of mouse embryonic stem cells to the adipocyte lineage requires retinoic acid receptor β and active GSK3. Stem Cells and Development. 2009;18(3):457–463. doi: 10.1089/scd.2008.0154. [DOI] [PubMed] [Google Scholar]
- 84.Haque N, Tanaka T, Iqbal K, Grundke-Iqbal I. Regulation of expression, phosphorylation and biological activity of tau during differentiation in SY5Y cells. Brain Research. 1999;838(1-2):69–77. doi: 10.1016/s0006-8993(99)01622-4. [DOI] [PubMed] [Google Scholar]
- 85.Oeff MK, Seltmann H, Hiroi N, et al. Differential regulation of toll-like receptor and CD14 pathways by retinoids and corticosteroids in human sebocytes. Dermatology. 2006;213(3):p. 266. doi: 10.1159/000095056. [DOI] [PubMed] [Google Scholar]
- 86.Bliss CM, Jr., Golenbock DT, Keates S, Linevsky JK, Kelly CP. Helicobacter pylori lipopolysaccharide binds to CD14 and stimulates release of interleukin-8, epithelial neutrophil-activating peptide 78, and monocyte chemotactic protein 1 by human monocytes. Infection and Immunity. 1998;66(11):5357–5363. doi: 10.1128/iai.66.11.5357-5363.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ma Y, Chen Q, Ross AC. Retinoic acid and polyriboinosinic: polyribocytidylic acid stimulate robust anti-tetanus antibody production while differentially regulating type 1/type 2 cytokines and lymphocyte populations. Journal of Immunology. 2005;174(12):7961–7969. doi: 10.4049/jimmunol.174.12.7961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gorr SU, Abdolhosseini M. Antimicrobial peptides and periodontal disease. Journal of Clinical Periodontology. 2011;38(supplement 11):126–141. doi: 10.1111/j.1600-051X.2010.01664.x. [DOI] [PubMed] [Google Scholar]
- 89.Yen A, Lin DM, Lamkin TJ, Varvayanis S. Retinoic acid, bromodeoxyuridine, and the Δ205 mutant polyoma virus middle T antigen regulate expression levels of a common ensemble of proteins associated with early stages of inducing HL-60 leukemic cell differentiation. In Vitro Cellular and Developmental Biology. 2004;40(7):216–241. doi: 10.1290/1543-706X(2004)40<216:RABATM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 90.Desreumaux P, Dubuquoy L, Nutten S, et al. Attenuation of colon inflammation through activators of the retinoid X receptor (RXR)/peroxisome proliferator-activated receptor gamma (PPARgamma) heterodimer. A basis for new therapeutic strategies. The Journal of Experimental Medicine. 2001;193(7):827–838. doi: 10.1084/jem.193.7.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Saitoh T, Tun-Kyi A, Ryo A, et al. Negative regulation of interferon-regulatory factor 3-dependent innate antiviral response by the prolyl isomerase Pin1. Nature Immunology. 2006;7(6):598–605. doi: 10.1038/ni1347. [DOI] [PubMed] [Google Scholar]
- 92.Hertz R, Seckbach M, Zakin MM, Bar-Tana J. Transcriptional suppression of the transferrin gene by hypolipidemic peroxisome proliferators. Journal of Biological Chemistry. 1996;271(1):218–224. doi: 10.1074/jbc.271.1.218. [DOI] [PubMed] [Google Scholar]
- 93.Gu B, Miao J, Fa Y, Lu J, Zou S. Retinoic acid attenuates lipopolysaccharide-induced inflammatory responses by suppressing TLR4/NF-κB expression in rat mammary tissue. International Immunopharmacology. 2010;10(7):799–805. doi: 10.1016/j.intimp.2010.04.022. [DOI] [PubMed] [Google Scholar]
- 94.Murthy S, Born E, Mathur SN, Field FJ. LXR/RXR activation enhances basolateral efflux of cholesterol in CaCo-2 cells. Journal of Lipid Research. 2002;43(7):1054–1064. doi: 10.1194/jlr.m100358-jlr200. [DOI] [PubMed] [Google Scholar]
- 95.Lind U, Nilsson T, McPheat J, et al. Identification of the human ApoAV gene as a novel RORalpha target gene. Biochemical and Biophysical Research Communications. 2005;330(1):233–241. doi: 10.1016/j.bbrc.2005.02.151. [DOI] [PubMed] [Google Scholar]
- 96.Moreno R, Perez-Jimenez F, Marin C, et al. A single nucleotide polymorphism of the apolipoprotein A-V gene -1131T > C modulates postprandial lipoprotein metabolism. Atherosclerosis. 2006;189(1):163–168. doi: 10.1016/j.atherosclerosis.2005.11.029. [DOI] [PubMed] [Google Scholar]
- 97.Kardassis D, Roussou A, Papakosta P, Boulias K, Talianidis I, Zannis VI. Synergism between nuclear receptors bound to specific hormone response elements of the hepatic control region-1 and the proximal apolipoprotein C-II promoter mediate apolipoprotein C-II gene regulation by bile acids and retinoids. Biochemical Journal. 2003;372(2):291–304. doi: 10.1042/BJ20021532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mak PA, Laffitte BA, Desrumaux C, et al. Regulated expression of the apolipoprotein E/C-I/C-IV/C-II gene cluster in murine and human macrophages: a critical role for nuclear liver X receptors α and β . Journal of Biological Chemistry. 2002;277(35):31900–31908. doi: 10.1074/jbc.M202993200. [DOI] [PubMed] [Google Scholar]
- 99.Lopez-Boado YS, Klaus M, Dawson MI, Lopez-Otin C. Retinoic acid-induced expression of apolipoprotein D and concomitant growth arrest in human breast cancer cells are mediated through a retinoic acid receptor RARalpha-dependent signaling pathway. The Journal of Biological Chemistry. 1996;271(50):32105–32111. doi: 10.1074/jbc.271.50.32105. [DOI] [PubMed] [Google Scholar]
- 100.Norata GD, Ongari M, Uboldi P, Pellegatta F, Catapano AL. Liver X receptor and retinoic X receptor agonists modulate the expression of genes involved in lipid metabolism in human endothelial cells. International Journal of Molecular Medicine. 2005;16(4):717–722. [PubMed] [Google Scholar]
- 101.Fukuchi J, Song C, Ko AL, Liao S. Transcriptional regulation of farnesyl pyrophosphate synthase by liver X receptors. Steroids. 2003;68(7-8):685–691. doi: 10.1016/s0039-128x(03)00100-4. [DOI] [PubMed] [Google Scholar]
- 102.Georgala S, Schulpis KH, Potouridou I, Papadogeorgaki H. Effects of isotretinoin therapy on lipoprotein (a) serum levels. International Journal of Dermatology. 1997;36(11):863–864. doi: 10.1046/j.1365-4362.1997.00306.x. [DOI] [PubMed] [Google Scholar]
- 103.Verani R, Cappuccio I, Spinsanti P, et al. Expression of the Wnt inhibitor Dickkopf-1 is required for the induction of neural markers in mouse embryonic stem cells differentiating in response to retinoic acid. Journal of Neurochemistry. 2007;100(1):242–250. doi: 10.1111/j.1471-4159.2006.04207.x. [DOI] [PubMed] [Google Scholar]
- 104.Padovani AM, Molina MF, Mann KK. Inhibition of liver X receptor/retinoid X receptor-mediated transcription contributes to the proatherogenic effects of arsenic in macrophages in vitro. Arteriosclerosis, Thrombosis, and Vascular Biology. 2010;30(6):1228–1236. doi: 10.1161/ATVBAHA.110.205500. [DOI] [PubMed] [Google Scholar]
- 105.Yang P, Liu Z, Wang H, et al. Enhanced activity of very low density lipoprotein receptor II promotes SGC7901 cell proliferation and migration. Life Sciences. 2009;84(13-14):402–408. doi: 10.1016/j.lfs.2008.12.020. [DOI] [PubMed] [Google Scholar]
- 106.de Oliveira MR, Oliveira MWS, Behr GA, Pasquali MAB, Moreira JCF. Increased receptor for advanced glycation endproducts immunocontent in the cerebral cortex of vitamin a-treated rats. Neurochemical Research. 2009;34(8):1410–1416. doi: 10.1007/s11064-009-9927-6. [DOI] [PubMed] [Google Scholar]
- 107.Gelain DP, Pasquali MAB, Caregnato FF, Zanotto-Filho A, Moreira JC. Retinol up-regulates the receptor for advanced glycation endproducts (RAGE) by increasing intracellular reactive species. Toxicology in Vitro. 2008;22(5):1123–1127. doi: 10.1016/j.tiv.2008.02.016. [DOI] [PubMed] [Google Scholar]
- 108.Moretti RM, Montagnani MM, Sala A, Motta M, Limonta P. Activation of the orphan nuclear receptor RORα counteracts the proliferative effect of fatty acids on prostate cancer cells: crucial role of 5-lipoxygenase. International Journal of Cancer. 2004;112(1):87–93. doi: 10.1002/ijc.20387. [DOI] [PubMed] [Google Scholar]
- 109.van Neerven S, Regen T, Wolf D, et al. Inflammatory chemokine release of astrocytes in vitro is reduced by all-trans retinoic acid. Journal of Neurochemistry. 2010;114(5):1511–1526. doi: 10.1111/j.1471-4159.2010.06867.x. [DOI] [PubMed] [Google Scholar]
- 110.Ko J, Yun CY, Lee JS, Kim JH, Kim IS. p38 MAPK and ERK activation by 9-cis-retinoic acid induces chemokine receptors CCR1 and CCR2 expression in human monocytic THP-1 cells. Experimental and Molecular Medicine. 2007;39(2):129–138. doi: 10.1038/emm.2007.15. [DOI] [PubMed] [Google Scholar]
- 111.Wang X, Allen C, Ballow M. Retinoic acid enhances the production of IL-10 while reducing the synthesis of IL-12 and TNF-α from LPS-stimulated monocytes/macrophages. Journal of Clinical Immunology. 2007;27(2):193–200. doi: 10.1007/s10875-006-9068-5. [DOI] [PubMed] [Google Scholar]
- 112.Sallmon H, Hoene V, Weber SC, Dame C. Differentiation of human SH-SY5Y neuroblastoma cells by all-trans retinoic acid activates the interleukin-18 system. Journal of Interferon and Cytokine Research. 2010;30(2):55–58. doi: 10.1089/jir.2009.0036. [DOI] [PubMed] [Google Scholar]
- 113.Napolitano M, Bellavia D, Maroder M, et al. Modulation of cytokine gene expression by thymic lympho-stromal cell to cell interaction: effect of retinoic acid. Thymus. 1997;24(4):247–258. [PubMed] [Google Scholar]
- 114.van Neerven S, Mey J, Joosten EA, et al. Systemic but not local administration of retinoic acid reduces early transcript levels of pro-inflammatory cytokines after experimental spinal cord injury. Neuroscience Letters. 2010;485(1):21–25. doi: 10.1016/j.neulet.2010.08.051. [DOI] [PubMed] [Google Scholar]
- 115.Wågsäter D, Jatta K, Ocaya P, Dimberg J, Sirsjö A. Expression of IL-1β, IL-1 receptor type I and IL-1 receptor antagonist in human aortic smooth muscle cells: effects of all-trans-retinoic acid. Journal of Vascular Research. 2006;43(4):377–382. doi: 10.1159/000094258. [DOI] [PubMed] [Google Scholar]
- 116.Gu B, Zhu Y, Zhu W, Miao J, Deng Y, Zou S. Retinoid protects rats against neutrophil-induced oxidative stress in acute experimental mastitis. International Immunopharmacology. 2009;9(2):223–229. doi: 10.1016/j.intimp.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 117.Hashimoto S, Hayashi S, Yoshida S, et al. Retinoic acid differentially regulates interleukin-1β and interleukin-1 receptor antagonist production by human alveolar macrophages. Leukemia Research. 1998;22(11):1057–1061. doi: 10.1016/s0145-2126(98)00119-2. [DOI] [PubMed] [Google Scholar]
- 118.Song S, Guan B, Men T, Hoque A, Lotan R, Xu XC. Antitumor effect of retinoic acid receptor-β associated with suppression of cyclooxygenase-2. Cancer Prevention Research. 2009;2(3):274–280. doi: 10.1158/1940-6207.CAPR-08-0180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lee SJ, Yang EK, Kim SG. Peroxisome proliferator-activated receptor-gamma and retinoic acid X receptor alpha represses the TGFbeta1 gene via PTEN-mediated p70 ribosomal S6 kinase-1 inhibition: role for Zf9 dephosphorylation. Molecular Pharmacology. 2006;70(1):415–425. doi: 10.1124/mol.106.022954. [DOI] [PubMed] [Google Scholar]
- 120.Wang J, Wu S, Jin X, et al. Retinoic acid-inducible gene-i mediates late phase induction of TNF-α by lipopolysaccharide. Journal of Immunology. 2008;180(12):8011–8019. doi: 10.4049/jimmunol.180.12.8011. [DOI] [PubMed] [Google Scholar]
- 121.Fidanza F, Sarchielli P, Jordan P, Lüdin E, Schalch W, Weimann BJ. Vitamin nutritional status and immunocompetence of elderly in Perugia (Italy): an epidemiological approach. International Journal for Vitamin and Nutrition Research. 1991;61(3):224–231. [PubMed] [Google Scholar]
- 122.Munoz-Canoves P, Vik DP, Tack BF. Mapping of a retinoic acid-responsive element in the promoter region of the complement factor H gene. Journal of Biological Chemistry. 1990;265(33):20065–20068. [PubMed] [Google Scholar]
- 123.Greer RM, Buntain HM, Lewindon PJ, et al. Vitamin A levels in patients with CF are influenced by the inflammatory response. Journal of Cystic Fibrosis. 2004;3(3):143–149. doi: 10.1016/j.jcf.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 124.Thompson S, Stern PL, Webb M, et al. Cloned human teratoma cells differentiate into neuron-like cells and other cell types in retinoic acid. Journal of Cell Science. 1984;72:37–64. doi: 10.1242/jcs.72.1.37. [DOI] [PubMed] [Google Scholar]
- 125.Lancillotti F, Giandomenico V, Affabris E, Fiorucci G, Romeo G, Rossi GB. Interferon α-2b and retinoic acid combined treatment affects proliferation and gene expression of human cervical carcinoma cells. Cancer Research. 1995;55(14):3158–3164. [PubMed] [Google Scholar]
- 126.Jinushi M, Takehara T, Tatsumi T, et al. Expression and role of MICA and MICB in human hepatocellular carcinomas and their regulation by retinoic acid. International Journal of Cancer. 2003;104(3):354–361. doi: 10.1002/ijc.10966. [DOI] [PubMed] [Google Scholar]
- 127.Czeczuga-Semeniuk E, Jarzabek K, Lemancewicz D, Wolczynski S. The vitamin A family can significantly decrease the expression of ERbeta of ERs positive breast cancer cells in the presence or absence of ER ligands and paclitaxel. Gynecological Endocrinology. 2009;25(5):287–293. doi: 10.1080/09513590802530924. [DOI] [PubMed] [Google Scholar]
- 128.Odawara H, Iwasaki T, Horiguchi J, et al. Activation of aromatase expression by retinoic acid receptor-related orphan receptor (ROR) α in breast cancer cells: identification of a novel ROR response element. Journal of Biological Chemistry. 2009;284(26):17711–17719. doi: 10.1074/jbc.M109.009241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kheirvari S, Uezu K, Yamamoto S, Nakaya Y. High-dose dietary supplementation of vitamin A induces brain-derived neurotrophic factor and nerve growth factor production in mice with simultaneous deficiency of vitamin A and zinc. Nutritional Neuroscience. 2008;11(5):228–234. doi: 10.1179/147683008X301603. [DOI] [PubMed] [Google Scholar]
- 130.Katsuki H, Kurimoto E, Takemori S, et al. Retinoic acid receptor stimulation protects midbrain dopaminergic neurons from inflammatory degeneration via BDNF-mediated signaling. Journal of Neurochemistry. 2009;110(2):707–718. doi: 10.1111/j.1471-4159.2009.06171.x. [DOI] [PubMed] [Google Scholar]
- 131.Chen CC, Hsu LW, Huang LT, Huang TL. Chronic administration of cyclosporine a changes expression of BDNF and TrkB in rat hippocampus and midbrain. Neurochemical Research. 2010;35(7):1098–1104. doi: 10.1007/s11064-010-0160-0. [DOI] [PubMed] [Google Scholar]
- 132.Dey N, De PK, Wang M, et al. CSK controls Retinoic Acid Receptor (RAR) signaling: a RAR-c-SRC signaling axis is required for neuritogenic differentiation. Molecular and Cellular Biology. 2007;27(11):4179–4197. doi: 10.1128/MCB.01352-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wan X, Nass P, Duncan MD, Harmon JW. Acidic fibroblast growth factor overexpression partially protects 3T3 fibroblasts from apoptosis induced by synthetic retinoid CD437. Journal of Molecular Medicine. 2001;79(2):143–148. doi: 10.1007/s001090100201. [DOI] [PubMed] [Google Scholar]
- 134.Mao Y, Lee AWM. A novel role for Gab2 in bFGF-mediated cell survival during retinoic acid-induced neuronal differentiation. Journal of Cell Biology. 2005;170(2):305–316. doi: 10.1083/jcb.200505061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Jaradat M, Stapleton C, Tilley SL, et al. Modulatory role for retinoid-related orphan receptor alpha in allergen-induced lung inflammation. American Journal of Respiratory and Critical Care Medicine. 2006;174(12):1299–1309. doi: 10.1164/rccm.200510-1672OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Bonnet E, Touyarot K, Alfos S, Pallet V, Higueret P, Abrous DN. Retinoic acid restores adult hippocampal neurogenesis and reverses spatial memory deficit in vitamin A deprived rats. PLoS ONE. 2008;3(10) doi: 10.1371/journal.pone.0003487. Article ID e3487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Sidell N, Feng Y, Hao L, et al. Retinoic acid is a cofactor for translational regulation of vascular endothelial growth factor in human endometrial stromal cells. Molecular Endocrinology. 2010;24(1):148–160. doi: 10.1210/me.2009-0155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Zhang M, Huang K, Zhang Z, et al. Proteome alterations of cortex and hippocampus tissues in mice subjected to vitamin A depletion. doi: 10.1016/j.jnutbio.2010.08.012. Journal of Nutritional Biochemistry. http://www.ncbi.nlm.nih.gov/pubmed/21190828. In press. [DOI] [PubMed] [Google Scholar]
- 139.Zimny J. Mechanisms that protect against homocysteine toxicity. Postepy biochemii. 2008;54(1):91–98. [PubMed] [Google Scholar]
- 140.Xu YY, Guan DY, Yang M, Wang H, Shen ZH. All-trans-retinoic acid intensifies endoplasmic reticulum stress in N-acetylglucosaminyltransferase V repressed human hepatocarcinoma cells by perturbing homocysteine metabolism. Journal of Cellular Biochemistry. 2010;109(3):468–477. doi: 10.1002/jcb.22423. [DOI] [PubMed] [Google Scholar]
- 141.Pascual I, Larrayoz IM, Rodriguez IR. Retinoic acid regulates the human methionine sulfoxide reductase A (MSRA) gene via two distinct promoters. Genomics. 2009;93(1):62–71. doi: 10.1016/j.ygeno.2008.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Fell D, Steele RD. Modification of hepatic folate metabolism in rats fed excess retinol. Life Sciences. 1986;38(21):1959–1965. doi: 10.1016/0024-3205(86)90225-0. [DOI] [PubMed] [Google Scholar]
- 143.Bayrak A, Bayrak T, Demirpence E, Kilinc K. Differential hydrolysis of homocysteine thiolactone by purified human serum 192Q and 192R PON1 isoenzymes. Journal of Chromatography B. 2011;879(1):49–55. doi: 10.1016/j.jchromb.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 144.Gatica LV, Vega VA, Zirulnik F, Oliveros LB, Gimenez MS. Alterations in the lipid metabolism of rat aorta: effects of vitamin A deficiency. Journal of Vascular Research. 2006;43(6):602–610. doi: 10.1159/000096247. [DOI] [PubMed] [Google Scholar]
- 145.Lin YW, Lien LM, Yeh TS, Wu HM, Liu YL, Hsieh RH. 9-cis retinoic acid induces retinoid X receptor localized to the mitochondria for mediation of mitochondrial transcription. Biochemical and Biophysical Research Communications. 2008;377(2):351–354. doi: 10.1016/j.bbrc.2008.09.122. [DOI] [PubMed] [Google Scholar]
- 146.Amengual J, Ribot J, Bonet ML, Palou A. Retinoic acid treatment increases lipid oxidation capacity in skeletal muscle of mice. Obesity. 2008;16(3):585–591. doi: 10.1038/oby.2007.104. [DOI] [PubMed] [Google Scholar]
- 147.Trojanowicz B, Sekulla C, Lorenz K, et al. Proteomic approach reveals novel targets for retinoic acid-mediated therapy of thyroid carcinoma. Molecular and Cellular Endocrinology. 2010;325(1-2):110–117. doi: 10.1016/j.mce.2010.05.022. [DOI] [PubMed] [Google Scholar]
- 148.Giera S, Braeuning A, Kohle C, et al. Wnt/beta-catenin signaling activates and determines hepatic zonal expression of glutathione S-transferases in mouse liver. The Journal of Toxicological Sciences. 2010;115(1):22–33. doi: 10.1093/toxsci/kfq033. [DOI] [PubMed] [Google Scholar]
- 149.Jimenez C, Leets I, Puche R, et al. A single dose of vitamin A improves haemoglobin concentration, retinol status and phagocytic function of neutrophils in preschool children. British Journal of Nutrition. 2010;103(6):798–802. doi: 10.1017/S0007114509992765. [DOI] [PubMed] [Google Scholar]
- 150.Lee SY, Liu S, Mitchell RM, et al. HFE polymorphisms influence the response to chemotherapeutic agents via induction of p16INK4A. doi: 10.1002/ijc.25888. International Journal of Cancer. http://www.ncbi.nlm.nih.gov/pubmed?term=21190189. In press. [DOI] [PubMed] [Google Scholar]
- 151.Samuel W, Kutty RK, Nagineni S, Vijayasarathy C, Chandraratna RAS, Wiggert B. N-(4-hydroxyphenyl)retinamide induces apoptosis in human retinal pigment epithelial cells: retinoic acid receptors regulate apoptosis, reactive oxygen species generation, and the expression of heme oxygenase-1 and Gadd153. Journal of Cellular Physiology. 2006;209(3):854–865. doi: 10.1002/jcp.20774. [DOI] [PubMed] [Google Scholar]
- 152.Mills KI, Woodgate LJ, Gilkes AF, et al. Inhibition of mitochondrial function in HL60 cells is associated with an increased apoptosis and expression of CD14. Biochemical and Biophysical Research Communications. 1999;263(2):294–300. doi: 10.1006/bbrc.1999.1356. [DOI] [PubMed] [Google Scholar]
- 153.Tan KP, Kosuge K, Yang M, Ito S. NRF2 as a determinant of cellular resistance in retinoic acid cytotoxicity. Free Radical Biology and Medicine. 2008;45(12):1663–1673. doi: 10.1016/j.freeradbiomed.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 154.Zhao F, Wu T, Lau A, et al. Nrf2 promotes neuronal cell differentiation. Free Radical Biology and Medicine. 2009;47(6):867–879. doi: 10.1016/j.freeradbiomed.2009.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Kiningham KK, Cardozo ZA, Cook C, et al. All-trans-retinoic acid induces manganese superoxide dismutase in human neuroblastoma through NF-κB. Free Radical Biology and Medicine. 2008;44(8):1610–1616. doi: 10.1016/j.freeradbiomed.2008.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Cadoudal T, Glorian M, Massias A, Fouque F, Forest C, Benelli C. Retinoids upregulate phosphoenolpyruvate carboxykinase and glyceroneogenesis in human and rodent adipocytes. Journal of Nutrition. 2008;138(6):1004–1009. doi: 10.1093/jn/138.6.1004. [DOI] [PubMed] [Google Scholar]
- 157.Everts HB, Claassen DO, Hermoyian CL, Berdanier CD. Nutrient-gene interactions: dietary vitamin A and mitochondrial gene expression. IUBMB Life. 2002;53(6):295–301. doi: 10.1080/15216540213465. [DOI] [PubMed] [Google Scholar]
- 158.Xu YY, Lu Y, Fan KY, Shen ZH. Apoptosis induced by all-trans retinoic acid in N- acetylglucosaminyltransferase V repressed human hepatocarcinoma cells is mediated through endoplasmic reticulum stress. Journal of Cellular Biochemistry. 2007;100(3):773–782. doi: 10.1002/jcb.21088. [DOI] [PubMed] [Google Scholar]
- 159.Bahouth SW, Beauchamp MJ, Park EA. Identification of a retinoic acid response domain involved in the activation of the β-adrenergic receptor gene by retinoic acid in F9 teratocarcinoma cells. Biochemical Pharmacology. 1998;55(2):215–225. doi: 10.1016/s0006-2952(97)00459-0. [DOI] [PubMed] [Google Scholar]
- 160.Liu L, Derguini F, Gudas LJ. Metabolism and regulation of gene expression by 4-oxoretinol versus all-trans retinoic acid in normal human mammary epithelial cells. Journal of Cellular Physiology. 2009;220(3):771–779. doi: 10.1002/jcp.21824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Salih SM, Jamaluddin M, Salama SA, Fadl AA, Nagamani M, Al-Hendy A. Regulation of catechol O-methyltransferase expression in granulosa cells: a potential role for follicular arrest in polycystic ovary syndrome. Fertility and Sterility. 2008;89(5):1414–1421. doi: 10.1016/j.fertnstert.2007.04.020. [DOI] [PubMed] [Google Scholar]
- 162.Sharma S, Notter MF. Characterization of neurotransmitter phenotype during neuronal differentiation of embryonal carcinoma cells. Developmental Biology. 1988;125(2):246–254. doi: 10.1016/0012-1606(88)90208-4. [DOI] [PubMed] [Google Scholar]
- 163.Castell X, Diebler MF, Tomasi M, et al. More than one way to toy with ChAT and VAChT. Journal of Physiology Paris. 2002;96(1-2):61–72. doi: 10.1016/s0928-4257(01)00081-x. [DOI] [PubMed] [Google Scholar]
- 164.Nilbratt M, Friberg L, Mousavi M, Marutle A, Nordberg A. Retinoic acid and nerve growth factor induce differential regulation of nicotinic acetylcholine receptor subunit expression in SN56 cells. Journal of Neuroscience Research. 2007;85(3):504–514. doi: 10.1002/jnr.21156. [DOI] [PubMed] [Google Scholar]
- 165.Ong CHP, He Z, Kriazhev L, Shan X, Palfree RGE, Bateman A. Regulation of progranulin expression in myeloid cells. American Journal of Physiology. 2006;291(6):R1602–R1612. doi: 10.1152/ajpregu.00616.2005. [DOI] [PubMed] [Google Scholar]
- 166.Oikarinen A, Vuorio T, Makela J, Vuorio E. 13-cis retinoic acid and dexamethasone modulate the gene expression of epidermal growth factor receptor and fibroblast proteoglycan 40 core protein in human skin fibroblasts. Acta Dermato-Venereologica. 1989;69(6):466–469. [PubMed] [Google Scholar]
- 167.Chang C, Chen XH, Kong PY, et al. In vitro effect of all-trans retinoic acid on cell adhesion molecule expression and adhesion capacity of bone marrow stromal cells in patients received peripheral blood stem cell transplantation. Journal of experimental hematology / Chinese Association of Pathophysiology. 2006;14(4):768–772. [PubMed] [Google Scholar]
- 168.Davies MR, Ribeiro LR, Downey-Jones M, Needham MRC, Oakley C, Wardale J. Ligands for retinoic acid receptors are elevated in osteoarthritis and may contribute to pathologic processes in the osteoarthritic joint. Arthritis and Rheumatism. 2009;60(6):1722–1732. doi: 10.1002/art.24550. [DOI] [PubMed] [Google Scholar]
- 169.Hatakeyama S, Hayashi S, Yoshida Y, et al. Retinoic acid disintegrated desmosomes and hemidesmosomes in stratified oral keratinocytes. Journal of Oral Pathology and Medicine. 2004;33(10):622–628. doi: 10.1111/j.1600-0714.2004.00245.x. [DOI] [PubMed] [Google Scholar]
- 170.Okumura K, Hosoe Y, Nakajima N. c-Jun and Sp1 family are critical for retinoic acid induction of the lamin A/C retinoic acid-responsive element. Biochemical and Biophysical Research Communications. 2004;320(2):487–492. doi: 10.1016/j.bbrc.2004.05.191. [DOI] [PubMed] [Google Scholar]
- 171.Fang Y, Zhou X, Lin M, et al. The ubiquitin-proteasome pathway plays essential roles in ATRA-induced leukemia cells G0/G1 phase arrest and transition into granulocytic differentiation. Cancer Biology and Therapy. 2010;10(11):1157–1167. doi: 10.4161/cbt.10.11.13556. [DOI] [PubMed] [Google Scholar]
- 172.Liu J, Li AP, Li CP, Zhang ZD, Zhou JW. The role of reactive oxygen species in N-[4-hydroxyphenyl] retinamide induced apoptosis in bladder cancer cell lineT24. Chinese journal of industrial hygiene and occupational diseases. 2005;23(3):191–194. [PubMed] [Google Scholar]
- 173.Lee LT, Tan-Un KC, Chow BK. Retinoic acid-induced human secretin gene expression in neuronal cells is mediated by cyclin-dependent kinase 1. Annals of the New York Academy of Sciences. 2006;1070:393–398. doi: 10.1196/annals.1317.051. [DOI] [PubMed] [Google Scholar]
- 174.Latif KA, Amla I, Rao PB. Urinary excretion of arylsulfatases in malnourished/vitamin A deficient children. Clinica Chimica Acta. 1979;96(1-2):131–138. doi: 10.1016/0009-8981(79)90062-7. [DOI] [PubMed] [Google Scholar]
- 175.Kasashima K, Terashima K, Yamamoto K, Sakashita E, Sakamoto H. Cytoplasmic localization is required for the mammalian ELAV-like protein HuD to induce neuronal differentiation. Genes to Cells. 1999;4(11):667–683. doi: 10.1046/j.1365-2443.1999.00292.x. [DOI] [PubMed] [Google Scholar]
- 176.Kihara A, Ikeda M, Kariya Y, Lee EY, Lee YM, Igarashi Y. Sphingosine-1-phosphate lyase is involved in the differentiation of F9 embryonal carcinoma cells to primitive endoderm. Journal of Biological Chemistry. 2003;278(16):14578–14585. doi: 10.1074/jbc.M211416200. [DOI] [PubMed] [Google Scholar]
- 177.Dembowski JA, Grabowski PJ. The CUGBP2 splicing factor regulates an ensemble of branchpoints from perimeter binding sites with implications for autoregulation. PLoS Genetics. 2009;5(8) doi: 10.1371/journal.pgen.1000595. Article ID e1000595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Chlon TM, Taffany DA, Welsh J, Rowling MJ. Retinoids modulate expression of the endocytic partners megalin, cubilin, and disabled-2 and uptake of vitamin D-binding protein in human mammary cells. Journal of Nutrition. 2008;138(7):1323–1328. doi: 10.1093/jn/138.7.1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Kudriashov BA, Ul’ianov AM, Bazaz’ian GG, Sytina NP. Factor XIII activity in the presence of suppression of the function of the anticoagulant system and its restoration in animals on an atherogenic ration. Voprosy pitaniia. 1976;(5):54–57. [PubMed] [Google Scholar]
- 180.Puppin C, Puglisi F, Pellizzari L, et al. HEX expression and localization in normal mammary gland and breast carcinoma. BMC Cancer. 2006;6, article 192 doi: 10.1186/1471-2407-6-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Knutson DC, Clagett-Dame M. atRA Regulation of NEDD9, a gene involved in neurite outgrowth and cell adhesion. Archives of Biochemistry and Biophysics. 2008;477(1):163–174. doi: 10.1016/j.abb.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 182.Chen Y, Sharma RP, Costa RH, Costa E, Grayson DR. On the epigenetic regulation of the human reelin promoter. Nucleic Acids Research. 2002;30(13):2930–2939. doi: 10.1093/nar/gkf401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Russell L, Naora H, Naora H. Down-regulated RPS3a/nbl expression during retinoid-induced differentiation of HL-60 cells: a close association with diminished susceptibility to actinomycin D-stimulated apoptosis. Cell Structure and Function. 2000;25(2):103–113. doi: 10.1247/csf.25.103. [DOI] [PubMed] [Google Scholar]
- 184.Zhang J, Song LP, Huang Y, Zhao Q, Zhao KW, Chen GQ. Accumulation of hypoxia-inducible factor-1α protein and its role in the differentiation of myeloid leukemic cells induced by all-trans retinoic acid. Haematologica. 2008;93(10):1480–1487. doi: 10.3324/haematol.13096. [DOI] [PubMed] [Google Scholar]
- 185.Takehashi M, Tanaka S, Stedeford T, et al. Expression of septin 3 isoforms in human brain. Gene Expression. 2004;11(5-6):271–278. doi: 10.3727/000000003783992270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Ono K, Yamada M. Vitamin A potently destabilizes preformed alpha-synuclein fibrils in vitro: implications for Lewy body diseases. Neurobiology of Disease. 2007;25(2):446–454. doi: 10.1016/j.nbd.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 187.Leypoldt F, Flajolet M, Methner A. Neuronal differentiation of cultured human NTERA-2cl.D1 cells leads to increased expression of synapsins. Neuroscience Letters. 2002;324(1):37–40. doi: 10.1016/s0304-3940(02)00170-2. [DOI] [PubMed] [Google Scholar]
- 188.Sahab ZJ, Hall MD, Zhang L, Cheema AK, Byers SW. Tumor suppressor RARRES1 regulates DLG2, PP2A, VCP, EB1, and Ankrd26. Journal of Cancer. 2010;1:14–22. doi: 10.7150/jca.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.de Chiara G, Marcocci ME, Civitelli L, et al. APP processing induced by herpes simplex virus type 1 (HSV-1) yields several APP fragments in human and rat neuronal cells. PLoS ONE. 2010;5(11) doi: 10.1371/journal.pone.0013989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Piacentini R, Civitelli L, Ripoli C, et al. HSV-1 promotes Ca2+-mediated APP phosphorylation and Aβ accumulation in rat cortical neurons. doi: 10.1016/j.neurobiolaging.2010.06.009. Neurobiology of Aging. http://www.ncbi.nlm.nih.gov/pubmed?term=20674092[uid]. In press. [DOI] [PubMed] [Google Scholar]
- 191.Wozniak MA, Itzhaki RF, Shipley SJ, Dobson CB. Herpes simplex virus infection causes cellular β-amyloid accumulation and secretase upregulation. Neuroscience Letters. 2007;429(2-3):95–100. doi: 10.1016/j.neulet.2007.09.077. [DOI] [PubMed] [Google Scholar]
- 192.Boelen E, Stassen FR, van der Ven AJ, et al. Detection of amyloid beta aggregates in the brain of BALB/c mice after Chlamydia pneumoniae infection. Acta Neuropathologica. 2007;114(3):255–261. doi: 10.1007/s00401-007-0252-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Little CS, Hammond CJ, MacIntyre A, Balin BJ, Appelt DM. Chlamydia pneumoniae induces Alzheimer-like amyloid plaques in brains of BALB/c mice. Neurobiology of Aging. 2004;25(4):419–429. doi: 10.1016/S0197-4580(03)00127-1. [DOI] [PubMed] [Google Scholar]
- 194.Thirumangalakudi L, Prakasam A, Zhang R, et al. High cholesterol-induced neuroinflammation and amyloid precursor protein processing correlate with loss of working memory in mice. Journal of Neurochemistry. 2008;106(1):475–485. doi: 10.1111/j.1471-4159.2008.05415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Prasanthi RPJ, Schommer E, Thomasson S, Thompson A, Feist G, Ghribi O. Regulation of β-amyloid levels in the brain of cholesterol-fed rabbit, a model system for sporadic Alzheimer’s disease. Mechanisms of Ageing and Development. 2008;129(11):649–655. doi: 10.1016/j.mad.2008.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Sharma S, Prasanthi RPJ, Schommer E, Feist G, Ghribi O. Hypercholesterolemia-induced Aβ accumulation in rabbit brain is associated with alteration in IGF-1 signaling. Neurobiology of Disease. 2008;32(3):426–432. doi: 10.1016/j.nbd.2008.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 197.Ullrich C, Pirchl M, Humpel C. Hypercholesterolemia in rats impairs the cholinergic system and leads to memory deficits. Molecular and Cellular Neuroscience. 2010;45(4):408–417. doi: 10.1016/j.mcn.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Zhang CE, Wei W, Liu YH, et al. Hyperhomocysteinemia increases beta-amyloid by enhancing expression of gamma-secretase and phosphorylation of amyloid precursor protein in rat brain. The American Journal of Pathology. 2009;174:1481–1491. doi: 10.2353/ajpath.2009.081036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Capsoni S, Ugolini G, Comparini A, Ruberti F, Berardi N, Cattaneo A. Alzheimer-like neurodegeneration in aged antinerve growth factor transgenic mice. Proceedings of the National Academy of Sciences of the United States of America. 2000;97(12):6826–6831. doi: 10.1073/pnas.97.12.6826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Kitaguchi H, Tomimoto H, Ihara M, et al. Chronic cerebral hypoperfusion accelerates amyloid β deposition in APPSwInd transgenic mice. Brain Research. 2009;1294:202–210. doi: 10.1016/j.brainres.2009.07.078. [DOI] [PubMed] [Google Scholar]
- 201.Li L, Zhang X, Yang D, Luo G, Chen S, Le W. Hypoxia increases Abeta generation by altering beta- and gamma-cleavage of APP. Neurobiology of Aging. 2009;30:1091–1098. doi: 10.1016/j.neurobiolaging.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 202.Zhiyou C, Yong Y, Shanquan S, et al. Upregulation of BACE1 and β-amyloid protein mediated by chronic cerebral hypoperfusion contributes to cognitive impairment and pathogenesis of Alzheimer’s disease. Neurochemical Research. 2009;34(7):1226–1235. doi: 10.1007/s11064-008-9899-y. [DOI] [PubMed] [Google Scholar]
- 203.Pluta R, Ułamek M, Jabłoński M. Alzheimer’s mechanisms in ischemic brain degeneration. Anatomical Record. 2009;292(12):1863–1881. doi: 10.1002/ar.21018. [DOI] [PubMed] [Google Scholar]
- 204.Li ZG, Zhang W, Sima AAF. Alzheimer-like changes in rat models of spontaneous diabetes. Diabetes. 2007;56(7):1817–1824. doi: 10.2337/db07-0171. [DOI] [PubMed] [Google Scholar]
- 205.Salkovic-Petrisic M, Tribl F, Schmidt M, Hoyer S, Riederer P. Alzheimer-like changes in protein kinase B and glycogen synthase kinase-3 in rat frontal cortex and hippocampus after damage to the insulin signalling pathway. Journal of Neurochemistry. 2006;96(4):1005–1015. doi: 10.1111/j.1471-4159.2005.03637.x. [DOI] [PubMed] [Google Scholar]
- 206.Yang HQ, Sun ZK, Jiang QH, Shang Q, Xu J. Effect of estrogen-depletion and 17beta-estradiol replacement therapy upon rat hippocampus beta-amyloid generation. Chinese Medical Journal. 2009;89(37):2658–2661. [PubMed] [Google Scholar]
- 207.Corcoran JPT, So PL, Maden M. Disruption of the retinoid signalling pathway causes a deposition of amyloid β in the adult rat brain. European Journal of Neuroscience. 2004;20(4):896–902. doi: 10.1111/j.1460-9568.2004.03563.x. [DOI] [PubMed] [Google Scholar]
- 208.Letenneur L, Pérès K, Fleury H, et al. Seropositivity to Herpes Simplex Virus antibodies and risk of Alzheimer’s disease: a population-based cohort study. PLoS ONE. 2008;3(11) doi: 10.1371/journal.pone.0003637. Article ID e3637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Lin WR, Shang D, Itzhaki RF. Neurotropic viruses and Alzheimer disease: interaction of herpes simplex type I virus and apolipoprotein E in the etiology of the disease. Molecular and Chemical Neuropathology. 1996;28(1–3):135–141. doi: 10.1007/BF02815215. [DOI] [PubMed] [Google Scholar]
- 210.Hammond CJ, Hallock LR, Howanski RJ, Appelt DM, Little CS, Balin BJ. Immunohistological detection of Chlamydia pneumoniae in the Alzheimer's disease brain. BMC Neuroscience. 2010;11, article 121 doi: 10.1186/1471-2202-11-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Shima K, Kuhlenbäumer G, Rupp J. Chlamydia pneumoniae infection and Alzheimer's disease: a connection to remember? Medical Microbiology and Immunology. 2010;199(4):283–289. doi: 10.1007/s00430-010-0162-1. [DOI] [PubMed] [Google Scholar]
- 212.Kountouras J, Tsolaki M, Gavalas E, et al. Relationship between Helicobacter pylori infection and Alzheimer disease. Neurology. 2006;66(6):938–940. doi: 10.1212/01.wnl.0000203644.68059.5f. [DOI] [PubMed] [Google Scholar]
- 213.Malaguarnera M, Bella R, Alagona G, Ferri R, Carnemolla A, Pennisi G. Helicobacter pylori and Alzheimer’s disease: a possible link. European Journal of Internal Medicine. 2004;15(6):381–386. doi: 10.1016/j.ejim.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 214.Pappolla MA, Bryant-Thomas TK, Herbert D, et al. Mild hypercholesterolemia is an early risk factor for the development of Alzheimer amyloid pathology. Neurology. 2003;61(2):199–205. doi: 10.1212/01.wnl.0000070182.02537.84. [DOI] [PubMed] [Google Scholar]
- 215.Mielke MM, Zandi PP, Shao H, et al. The 32-year relationship between cholesterol and dementia from midlife to late life. Neurology. 2010;75(21):1888–1895. doi: 10.1212/WNL.0b013e3181feb2bf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.de la Torre JC. The vascular hypothesis of Alzheimer’s disease: bench to bedside and beyond. Neurodegenerative Diseases. 2010;7(1–3):116–121. doi: 10.1159/000285520. [DOI] [PubMed] [Google Scholar]
- 217.van Oijen M, de Jong FJ, Witteman JC, Hofman A, Koudstaal PJ, Breteler MM. Atherosclerosis and risk for dementia. Annals of Neurology. 2007;61:403–410. doi: 10.1002/ana.21073. [DOI] [PubMed] [Google Scholar]
- 218.Roher AE, Esh C, Kokjohn TA, et al. Circle of willis atherosclerosis is a risk factor for sporadic Alzheimer’s disease. Arteriosclerosis, Thrombosis, and Vascular Biology. 2003;23(11):2055–2062. doi: 10.1161/01.ATV.0000095973.42032.44. [DOI] [PubMed] [Google Scholar]
- 219.Roher AE, Esh C, Rahman A, Kokjohn TA, Beach TG. Atherosclerosis of cerebral arteries in Alzheimer disease. Stroke. 2004;35(11):2623–2627. doi: 10.1161/01.STR.0000143317.70478.b3. [DOI] [PubMed] [Google Scholar]
- 220.Miller JW. Homocysteine and Alzheimer’s disease. Nutrition Reviews. 1999;57(4):126–129. doi: 10.1111/j.1753-4887.1999.tb06936.x. [DOI] [PubMed] [Google Scholar]
- 221.Schrijvers EMC, Witteman JCM, Sijbrands EJG, Hofman A, Koudstaal PJ, Breteler MMB. Insulin metabolism and the risk of Alzheimer disease: the Rotterdam Study. Neurology. 2010;75(22):1982–1987. doi: 10.1212/WNL.0b013e3181ffe4f6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Pike CJ, Carroll JC, Rosario ER, Barron AM. Protective actions of sex steroid hormones in Alzheimer’s disease. Frontiers in Neuroendocrinology. 2009;30(2):239–258. doi: 10.1016/j.yfrne.2009.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Geerlings MI, Launer LJ, de Jong FH, et al. Endogenous estradiol and risk of dementia in women and men: the Rotterdam study. Annals of Neurology. 2003;53(5):607–615. doi: 10.1002/ana.10521. [DOI] [PubMed] [Google Scholar]
- 224.Ravaglia G, Forti P, Maioli F, et al. Endogenous sex hormones as risk factors for dementia in elderly men and women. Journals of Gerontology Series A. 2007;62(9):1035–1041. doi: 10.1093/gerona/62.9.1035. [DOI] [PubMed] [Google Scholar]
- 225.Jimenez-Jimenez FJ, Molina JA, de Bustos F, et al. Serum levels of beta-carotene, alpha-carotene and vitamin A in patients with Alzheimer's disease. European Journal of Neurology. 1999;6:495–497. doi: 10.1046/j.1468-1331.1999.640495.x. [DOI] [PubMed] [Google Scholar]
- 226.Carter CJ. APP, APOE, complement receptor 1, clusterin and PICALM and their involvement in the herpes simplex life cycle. Neuroscience Letters. 2010;483(2):96–100. doi: 10.1016/j.neulet.2010.07.066. [DOI] [PubMed] [Google Scholar]
- 227.Jones L, Holmans PA, Hamshere ML, et al. Genetic evidence implicates the immune system and cholesterol metabolism in the aetiology of Alzheimer's disease. PLoS ONE. 2010;5(11) doi: 10.1371/journal.pone.0013950. Article ID e13950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Carter CJ. Convergence of genes implicated in Alzheimer’s disease on the cerebral cholesterol shuttle: APP, cholesterol, lipoproteins, and atherosclerosis. Neurochemistry International. 2007;50(1):12–38. doi: 10.1016/j.neuint.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 229.Naj AC, Beecham GW, Martin ER, et al. Dementia revealed: novel chromosome 6 locus for Late-onset Alzheimer disease provides genetic evidence for Folate-pathway abnormalities. PLoS Genetics. 2010;6(9) doi: 10.1371/journal.pgen.1001130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Carter CJ. Alzheimer's disease: a pathogenetic autoimmune disorder caused by herpes simplex in a gene-dependent manner. International Journal of Alzheimer's Disease. 2010;2010:17 pages. doi: 10.4061/2010/140539. Article ID 140539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Iacono D, Markesbery WR, Gross M, et al. The Nun Study: clinically silent AD, neuronal hypertrophy, and linguistic skills in early life. Neurology. 2009;73(9):665–673. doi: 10.1212/WNL.0b013e3181b01077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Snowdon DA. Healthy aging and dementia: findings from the Nun Study. Annals of Internal Medicine. 2003;139(5):450–454. doi: 10.7326/0003-4819-139-5_part_2-200309021-00014. [DOI] [PubMed] [Google Scholar]
- 233.Tyas SL, Snowdon DA, Desrosiers MF, Riley KP, Markesbery WR. Healthy ageing in the Nun Study: definition and neuropathologic correlates. Age and Ageing. 2007;36(6):650–655. doi: 10.1093/ageing/afm120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Wolf DS, Gearing M, Snowdon DA, Mori H, Markesbery WR, Mirra SS. Progression of regional neuropathology in Alzheimer disease and normal elderly: findings from the Nun Study. Alzheimer Disease and Associated Disorders. 1999;13(4):226–231. doi: 10.1097/00002093-199910000-00009. [DOI] [PubMed] [Google Scholar]
- 235.Colucci M, Cammarata S, Assini A, et al. The number of pregnancies is a risk factor for Alzheimer’s disease. European Journal of Neurology. 2006;13(12):1374–1377. doi: 10.1111/j.1468-1331.2006.01520.x. [DOI] [PubMed] [Google Scholar]
- 236.Kountouras J, Boziki M, Gavalas E, et al. Eradication of Helicobacter pylori may be beneficial in the management of Alzheimer’s disease. Journal of Neurology. 2009;256(5):758–767. doi: 10.1007/s00415-009-5011-z. [DOI] [PubMed] [Google Scholar]
- 237.Ala TA, Doss RC, Sullivan CJ. Reversible dementia: a case of cryptococcal meningitis masquerading as Alzheimer’s disease. Journal of Alzheimer’s Disease. 2004;6(5):503–508. doi: 10.3233/jad-2004-6507. [DOI] [PubMed] [Google Scholar]
- 238.Hoffmann M, Muniz J, Carroll E, De Villasante J. Cryptococcal meningitis misdiagnosed as Alzheimer’s disease: complete neurological and cognitive recovery with treatment. Journal of Alzheimer’s Disease. 2009;16(3):517–520. doi: 10.3233/JAD-2009-0985. [DOI] [PubMed] [Google Scholar]
- 239.Tobinick EL, Gross H. Rapid cognitive improvement in Alzheimer’s disease following perispinal etanercept administration. Journal of Neuroinflammation. 2008;5, article 2 doi: 10.1186/1742-2094-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Marie I, Guglielmino E. Non tuberculous anti-TNF associated opportunistic infections. Revue de Medecine Interne. 2010;31(5):353–360. doi: 10.1016/j.revmed.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 241.Morris MC, Evans DA, Bienias JL, et al. Consumption of fish and n-3 fatty acids and risk of incident Alzheimer disease. Archives of Neurology. 2003;60(7):940–946. doi: 10.1001/archneur.60.7.940. [DOI] [PubMed] [Google Scholar]
- 242.Gu Y, Nieves JW, Stern Y, Luchsinger JA, Scarmeas N. Food combination and Alzheimer disease risk: a protective diet. Archives of Neurology. 2010;67(6):699–706. doi: 10.1001/archneurol.2010.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Scarmeas N, Stern Y, Mayeux R, Luchsinger JA. Mediterranean diet, Alzheimer disease, and vascular mediation. Archives of Neurology. 2006;63(12):1709–1717. doi: 10.1001/archneur.63.12.noc60109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Wolozin B, Kellman W, Ruosseau P, Celesia GG, Siegel G. Decreased prevalence of Alzheimer disease associated with 3-hydroxy-3-methyglutaryl coenzyme A reductase inhibitors. Archives of Neurology. 2000;57(10):1439–1443. doi: 10.1001/archneur.57.10.1439. [DOI] [PubMed] [Google Scholar]
- 245.Hughes TF, Andel R, Small BJ, et al. Midlife fruit and vegetable consumption and risk of dementia in later life in Swedish twins. American Journal of Geriatric Psychiatry. 2010;18(5):413–420. doi: 10.1097/JGP.0b013e3181c65250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Bermejo LM, Aparicio A, Andrés P, López-Sobaler AM, Ortega RM. The influence of fruit and vegetable intake on the nutritional status and plasma homocysteine levels of institutionalised elderly people. Public Health Nutrition. 2007;10(3):266–272. doi: 10.1017/S1368980007246580. [DOI] [PubMed] [Google Scholar]
- 247.Luchsinger JA, Tang MX, Miller J, Green R, Mayeux R. Higher folate intake is related to lower risk of Alzheimer’s disease in the elderly. Journal of Nutrition, Health and Aging. 2008;12(9):648–650. doi: 10.1007/BF03008276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.McGeer PL, Schulzer M, McGeer EG. Arthritis and anti-inflammatory agents as possible protective factors for Alzheimer’s disease: a review of 17 epidemiologic studies. Neurology. 1996;47(2):425–432. doi: 10.1212/wnl.47.2.425. [DOI] [PubMed] [Google Scholar]
- 249.Corder EH, Saunders AM, Strittmatter WJ, et al. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science. 1993;261(5123):921–923. doi: 10.1126/science.8346443. [DOI] [PubMed] [Google Scholar]
- 250.Gérard HC, Fomicheva E, Whittum-Hudson JA, Hudson AP. Apolipoprotein E4 enhances attachment of Chlamydophila (Chlamydia) pneumoniae elementary bodies to host cells. Microbial Pathogenesis. 2008;44(4):279–285. doi: 10.1016/j.micpath.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 251.de Chaves EP, Narayanaswami V. Apolipoprotein E and cholesterol in aging and disease in the brain. Future Lipidology. 2008;3(5):505–530. doi: 10.2217/17460875.3.5.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Elosua R, Ordovas JM, Cupples LA, et al. Association of APOE genotype with carotid atherosclerosis in men and women: the Framingham Heart Study. Journal of Lipid Research. 2004;45(10):1868–1875. doi: 10.1194/jlr.M400114-JLR200. [DOI] [PubMed] [Google Scholar]
- 253.Minagawa H, Gong JS, Jung CG, et al. Mechanism underlying apolipoprotein E (ApoE) isoform-dependent lipid efflux from neural cells in culture. Journal of Neuroscience Research. 2009;87(11):2498–2508. doi: 10.1002/jnr.22073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Xiong H, Callaghan D, Jones A, et al. Cholesterol retention in Alzheimer's brain is responsible for high beta- and gamma-secretase activities and Abeta production. Neurobiology of Disease. 2008;29(3):422–437. doi: 10.1016/j.nbd.2007.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Weintraub MS, Eisenberg S, Breslow JL. Dietary fat clearance in normal subjects is regulated by genetic variation in apolipoprotein E. Journal of Clinical Investigation. 1987;80(6):1571–1577. doi: 10.1172/JCI113243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Powers JH, Buster BL, Reist CJ, et al. Complement-independent binding of microorganisms to primate erythrocytes in vitro by cross-linked monoclonal antibodies via complement receptor 1. Infection and Immunity. 1995;63(4):1329–1335. doi: 10.1128/iai.63.4.1329-1335.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Levitz SM. Receptor-mediated recognition of Cryptococcus neoformans . Japanese Journal of Medical Mycology. 2002;43(3):133–136. doi: 10.3314/jjmm.43.133. [DOI] [PubMed] [Google Scholar]
- 258.Belstrom D, Holmstrup P, Damgaard C, et al. The atherogenicbacterium Porphyromonas gingivalis evades circulating phagocytes by adhering to erythrocytes. Infection and Immunity. 2011;79(4):1559–1565. doi: 10.1128/IAI.01036-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Kamer AR, Craig RG, Dasanayake AP, Brys M, Glodzik-Sobanska L, de Leon MJ. Inflammation and Alzheimer’s disease: possible role of periodontal diseases. Alzheimer’s and Dementia. 2008;4(4):242–250. doi: 10.1016/j.jalz.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 260.Puolakkainen M, Kuo CC, Campbell LA. Chlamydia pneumoniae uses the mannose 6-phosphate/insulin-like growth factor 2 receptor for infection of endothelial cells. Infection and Immunity. 2005;73(8):4620–4625. doi: 10.1128/IAI.73.8.4620-4625.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Tebar F, Bohlander SK, Sorkin A. Clathrin assembly lymphoid myeloid leukemia (CALM) protein: localization in endocytic-coated pits, interactions with clathrin, and the impact of overexpression on clathrin-mediated traffic. Molecular Biology of the Cell. 1999;10(8):2687–2702. doi: 10.1091/mbc.10.8.2687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Stuart ES, Webley WC, Norkin LC. Lipid rafts, caveolae, caveolin-1, and entry by Chlamydiae into host cells. Experimental Cell Research. 2003;287(1):67–78. doi: 10.1016/s0014-4827(03)00059-4. [DOI] [PubMed] [Google Scholar]
- 263.Crump CM, Bruun B, Bell S, Pomeranz LE, Minson T, Browne HM. Alphaherpesvirus glycoprotein M causes the relocalization of plasma membrane proteins. Journal of General Virology. 2004;85(12):3517–3527. doi: 10.1099/vir.0.80361-0. [DOI] [PubMed] [Google Scholar]
- 264.Fraile-Ramos A, Kohout TA, Waldhoer M, Marsh M. Endocytosis of the viral chemokine receptor US28 does not require beta-arrestins but is dependent on the clathrin-mediated pathway. Traffic. 2003;4(4):243–253. doi: 10.1034/j.1600-0854.2003.00079.x. [DOI] [PubMed] [Google Scholar]
- 265.Parker H, Chitcholtan K, Hampton MB, Keenan JI. Uptake of Helicobacter pylori outer membrane vesicles by gastric epithelial cells. Infection and Immunity. 2010;78(12):5054–5061. doi: 10.1128/IAI.00299-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Hammarstedt M, Ahlqvist J, Jacobson S, Garoff H, Fogdell-Hahn A. Purification of infectious human herpesvirus 6A virions and association of host cell proteins. Virology Journal. 2007;4, article 101 doi: 10.1186/1743-422X-4-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Tschopp J, Chonn A, Hertig S, French LE. Clusterin, the human apolipoprotein and complement inhibitor, binds to complement C7, C8β, and the b domain of C9. Journal of Immunology. 1993;151(4):2159–2165. [PubMed] [Google Scholar]
- 268.Bell RD, Sagare AP, Friedman AE, et al. Transport pathways for clearance of human Alzheimer's amyloid beta-peptide and apolipoproteins E and J in the mouse central nervous system. Journal of Cerebral Blood Flow & Metabolism. 2007;27(5):909–918. doi: 10.1038/sj.jcbfm.9600419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Olano-Martin E, Anil E, Caslake MJ, et al. Contribution of apolipoprotein E genotype and docosahexaenoic acid to the LDL-cholesterol response to fish oil. Atherosclerosis. 2010;209(1):104–110. doi: 10.1016/j.atherosclerosis.2009.08.024. [DOI] [PubMed] [Google Scholar]
- 270.Evrengul H, Tanriverdi H, Kuru O, et al. Elevated homocysteine levels in patients with slow coronary flow: relationship with Helicobacter pylori infection. Helicobacter. 2007;12(4):298–305. doi: 10.1111/j.1523-5378.2007.00505.x. [DOI] [PubMed] [Google Scholar]
- 271.Vitvitsky V, Thomas M, Ghorpade A, Gendelman HE, Banerjee R. A functional transsulfuration pathway in the brain links to glutathione homeostasis. Journal of Biological Chemistry. 2006;281(47):35785–35793. doi: 10.1074/jbc.M602799200. [DOI] [PubMed] [Google Scholar]
- 272.Palamara AT, Perno CF, Ciriolo MR, et al. Evidence for antiviral activity of glutathione: in vitro inhibition of herpes simplex virus type 1 replication. Antiviral Research. 1995;27(3):237–253. doi: 10.1016/0166-3542(95)00008-a. [DOI] [PubMed] [Google Scholar]
- 273.Shibayama K, Wachino J, Arakawa Y, Saidijam M, Rutherford NG, Henderson PJ. Metabolism of glutamine and glutathione via gamma-glutamyltranspeptidase and glutamate transport in Helicobacter pylori: possible significance in the pathophysiology of the organism. Molecular Microbiology. 2007;64(2):396–406. doi: 10.1111/j.1365-2958.2007.05661.x. [DOI] [PubMed] [Google Scholar]
- 274.Ballatori N, Krance SM, Notenboom S, Shi S, Tieu K, Hammond CL. Glutathione dysregulation and the etiology and progression of human diseases. Biological Chemistry. 2009;390(3):191–214. doi: 10.1515/BC.2009.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Stanger OH, Semmelrock HJ, Rehak P, et al. Hyperhomocyst(e)inemia and Chlamydia pneumoniae IgG seropositivity in patients with coronary artery disease. Atherosclerosis. 2002;162(1):157–162. doi: 10.1016/s0021-9150(01)00686-4. [DOI] [PubMed] [Google Scholar]
- 276.Sawayama Y, Tatsukawa M, Maeda S, Ohnishi H, Furusyo N, Hayashi J. Association of hyperhomocysteinemia and Chlamydia pneumoniae infection with carotid atherosclerosis and coronary artery disease in Japanese patients. Journal of Infection and Chemotherapy. 2008;14(3):232–237. doi: 10.1007/s10156-008-0607-2. [DOI] [PubMed] [Google Scholar]
- 277.Mayr M, Kiechl S, Willeit J, Wick G, Xu Q. Infections, immunity, and atherosclerosis: associations of antibodies to Chlamydia pneumoniae, Helicobacter pylori, and cytomegalovirus with immune reactions to heat-shock protein 60 and carotid or femoral atherosclerosis. Circulation. 2000;102(8):833–839. doi: 10.1161/01.cir.102.8.833. [DOI] [PubMed] [Google Scholar]
- 278.Mohr JA, Long H, McKown BA, Muchmore HG. In vitro susceptibility of Cryptococcus neoformans to steroids. Sabouraudia Journal of Medical and Veterinary Mycology. 1972;10(2):171–172. [PubMed] [Google Scholar]
- 279.Hosoda K, Shimomura H, Hayashi S, Yokota K, Oguma K, Hirai Y. Anabolic utilization of steroid hormones in Helicobacter pylori . FEMS Microbiology Letters. 2009;297(2):173–179. doi: 10.1111/j.1574-6968.2009.01685.x. [DOI] [PubMed] [Google Scholar]
- 280.Hosoda K, Shimomura H, Hayashi S, Yokota K, Hirai Y. Steroid hormones as bactericidal agents to Helicobacter pylori . FEMS Microbiology Letters. 2011;318(1):68–75. doi: 10.1111/j.1574-6968.2011.02239.x. [DOI] [PubMed] [Google Scholar]
- 281.Clement C, Bhattacharjee PS, Kaufman HE, Hill JM. Heat-induced reactivation of HSV-1 in latent mice: upregulation in the TG of CD83 and other immune response genes and their LAT-ICP0 locus. Investigative Ophthalmology and Visual Science. 2009;50(6):2855–2861. doi: 10.1167/iovs.08-2430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Vicetti Miguel RD, Sheridan BS, Harvey SAK, Schreiner RS, Hendricks RL, Cherpes TL. 17-β estradiol promotion of herpes simplex virus type 1 reactivation is estrogen receptor dependent. Journal of Virology. 2010;84(1):565–572. doi: 10.1128/JVI.01374-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Kriesel JD, Ricigliano J, Spruance SL, Garza HH, Jr., Hill JM. Neuronal reactivation of herpes simplex virus may involve interleukin-6. Journal of NeuroVirology. 1997;3(6):441–448. doi: 10.3109/13550289709031190. [DOI] [PubMed] [Google Scholar]
- 284.Noisakran S, Halford WP, Veress L, Carr DJJ. Role of the hypothalamic pituitary adrenal axis and IL-6 in stress- induced reactivation of latent herpes simplex virus type 1. Journal of Immunology. 1998;160(11):5441–5447. [PubMed] [Google Scholar]
- 285.Wilcox CL, Johnson EM., Jr. Nerve growth factor deprivation results in the reactivation of latent herpes simplex virus in vitro. Journal of Virology. 1987;61(7):2311–2315. doi: 10.1128/jvi.61.7.2311-2315.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Camarena V, Kobayashi M, Kim JY, et al. Nature and duration of growth factor signaling through receptor tyrosine kinases regulates HSV-1 latency in neurons. Cell Host and Microbe. 2010;8(4):320–330. doi: 10.1016/j.chom.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Jiang B, Liao EY, Tan LM, Dai RC, Xiao ZJ, Liao HJ. Effects of long-term replacement therapy of compound nylestriol tablet or low-dose 17 beta-estradiol on the expression of nerve growth factor in OVX rat hippocampal formation. Journal of Central South University. 2004;29(5):529–533. [PubMed] [Google Scholar]
- 288.Hashimoto Y, Kawatsura H, Shiga Y, Furukawa S, Shigeno T. Significance of nerve growth factor content levels after transient forebrain ischemia in gerbils. Neuroscience Letters. 1992;139(1):45–46. doi: 10.1016/0304-3940(92)90853-y. [DOI] [PubMed] [Google Scholar]
- 289.Aghi MK, Liu TC, Rabkin S, Martuza RL. Hypoxia enhances the replication of oncolytic herpes simplex virus. Molecular Therapy. 2009;17(1):51–56. doi: 10.1038/mt.2008.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Sun YX, Minthon L, Wallmark A, Warkentin S, Blennow K, Janciauskiene S. Inflammatory markers in matched plasma and cerebrospinal fluid from patients with Alzheimer’s disease. Dementia and Geriatric Cognitive Disorders. 2003;16(3):136–144. doi: 10.1159/000071001. [DOI] [PubMed] [Google Scholar]
- 291.Kálmán J, Juhász A, Laird G, et al. Serum interleukin-6 levels correlate with the severity of dementia in down syndrome and in Alzheimer's disease. Acta Neurologica Scandinavica. 1997;96(4):236–240. doi: 10.1111/j.1600-0404.1997.tb00275.x. [DOI] [PubMed] [Google Scholar]
- 292.Shalit F, Sredni B, Stern L, Kott E, Huberman M. Elevated interleukin-6 secretion levels by mononuclear cells of Alzheimer’s patients. Neuroscience Letters. 1994;174(2):130–132. doi: 10.1016/0304-3940(94)90003-5. [DOI] [PubMed] [Google Scholar]
- 293.Kragsbjerg P, Vikerfors T, Holmberg H. Cytokine responses in patients with pneumonia caused by Chlamydia or Mycoplasma . Respiration. 1998;65(4):299–303. doi: 10.1159/000029280. [DOI] [PubMed] [Google Scholar]
- 294.Mehmet N, Refik M, Harputluoglu M, Ersoy Y, Aydin NE, Yildirim B. Serum and gastric fluid levels of cytokines and nitrates in gastric diseases infected with Helicobacter pylori . New Microbiologica. 2004;27(2):139–148. [PubMed] [Google Scholar]
- 295.Delfino D, Cianci L, Lupis E, et al. Interleukin-6 production by human monocytes stimulated with Cryptococcus neoformans components. Infection and Immunity. 1997;65(6):2454–2456. doi: 10.1128/iai.65.6.2454-2456.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Huang CW, Lui CC, Chang WN, Lu CH, Wang YL, Chang CC. Elevated basal cortisol level predicts lower hippocampal volume and cognitive decline in Alzheimer’s disease. Journal of Clinical Neuroscience. 2009;16(10):1283–1286. doi: 10.1016/j.jocn.2008.12.026. [DOI] [PubMed] [Google Scholar]
- 297.Davis KL, Davis BM, Greenwald BS, et al. Cortisol and Alzheimer’s disease. I: basal studies. American Journal of Psychiatry. 1986;143(3):300–305. doi: 10.1176/ajp.143.3.300. [DOI] [PubMed] [Google Scholar]
- 298.Wozniak MA, Mee AP, Itzhaki RF. Herpes simplex virus type 1 DNA is located within Alzheimer’s disease amyloid plaques. Journal of Pathology. 2009;217(1):131–138. doi: 10.1002/path.2449. [DOI] [PubMed] [Google Scholar]
- 299.Toffanello ED, Inelmen EM, Minicuci N, et al. Ten-year trends in vitamin intake in free-living healthy elderly people: the risk of subclinical malnutrition. Journal of Nutrition, Health and Aging. 2011;15(2):99–103. doi: 10.1007/s12603-011-0020-x. [DOI] [PubMed] [Google Scholar]
- 300.Semba RD. The role of vitamin A and related retinoids in immune function. Nutrition Reviews. 1998;56(1):S38–S48. doi: 10.1111/j.1753-4887.1998.tb01643.x. [DOI] [PubMed] [Google Scholar]
- 301.Isaacs CE, Kascsak R, Pullarkat RK, Xu W, Schneidman K. Inhibition of herpes simplex virus replication by retinoic acid. Antiviral Research. 1997;33(2):117–127. doi: 10.1016/s0166-3542(96)01009-1. [DOI] [PubMed] [Google Scholar]
- 302.Isaacs CE, Xu W, Pullarkat RK, Kascsak R. Retinoic acid reduces the yield of herpes simplex virus in Vero cells and alters the N-glycosylation of viral envelope proteins. Antiviral Research. 2000;47(1):29–40. doi: 10.1016/s0166-3542(00)00090-5. [DOI] [PubMed] [Google Scholar]
- 303.Puolakkainen M, Lee A, Nosaka T, Fukushi H, Kuo CC, Campbell LA. Retinoic acid inhibits the infectivity and growth of Chlamydia pneumoniae in epithelial and endothelial cells through different receptors. Microbial Pathogenesis. 2008;44(5):410–416. doi: 10.1016/j.micpath.2007.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Sjunnesson H, Sturegård E, Willén R, Wadström T. High intake of selenium, β-carotene, and vitamins A, C, and E reduces growth of Helicobacter pylori in the guinea pig. Comparative Medicine. 2001;51(5):418–423. [PubMed] [Google Scholar]
- 305.Monari C, Bevilacqua S, Piccioni M, et al. A microbial polysaccharide reduces the severity of rheumatoid arthritis by influencing Th17 differentiation and proinflammatory cytokines production. Journal of Immunology. 2009;183(1):191–200. doi: 10.4049/jimmunol.0804144. [DOI] [PubMed] [Google Scholar]
- 306.Limpach A, Dalton M, Miles R, Gadson P. Homocysteine inhibits retinoic acid synthesis: a mechanism for homocysteine-induced congenital defects. Experimental Cell Research. 2000;260(1):166–174. doi: 10.1006/excr.2000.5000. [DOI] [PubMed] [Google Scholar]
- 307.Tanghe KA, Garrow TA, Schalinske KL. Triiodothyronine treatment attenuates the induction of hepatic glycine N-methyltransferase by retinoic acid and elevates plasma homocysteine concentrations in rats. Journal of Nutrition. 2004;134(11):2913–2918. doi: 10.1093/jn/134.11.2913. [DOI] [PubMed] [Google Scholar]
- 308.Smith DK, Greene JM, Leonard SB, Kuske TT, Feldman DS, Feldman EB. Vitamin A in hypercholesterolemia. American Journal of the Medical Sciences. 1992;304(1):20–24. doi: 10.1097/00000441-199207000-00006. [DOI] [PubMed] [Google Scholar]
- 309.Soscia SJ, Kirby JE, Washicosky KJ, et al. The Alzheimer's disease-associated amyloid beta-protein is an antimicrobial peptide. PLoS ONE. 2010;5(3) doi: 10.1371/journal.pone.0009505. Article ID e9505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Kawamata T, Tooyama I, Yamada T, Walker DG, McGeer PL. Lactotransferrin immunocytochemistry in Alzheimer and normal human brain. American Journal of Pathology. 1993;142(5):1574–1585. [PMC free article] [PubMed] [Google Scholar]
- 311.Lukiw WJ, Cui JG, Yuan LY, et al. Acyclovir or Abeta42 peptides attenuate HSV-1-induced miRNA-146a levels in human primary brain cells. Neuroreport. 2010;21(14):922–927. doi: 10.1097/WNR.0b013e32833da51a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Sohn JH, So JO, Hong HJ, et al. Identification of autoantibody against beta-amyloid peptide in the serum of elderly. Frontiers in Bioscience. 2009;14:3879–3883. doi: 10.2741/3496. [DOI] [PubMed] [Google Scholar]
- 313.Paul S, Planque S, Nishiyama Y. Immunological origin and functional properties of catalytic autoantibodies to amyloid β peptide. Journal of Clinical Immunology. 2010;30(supplement 1):43–49. doi: 10.1007/s10875-010-9414-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Miklossy J, Khalili K, Gern L, et al. Borrelia burgdorferi persists in the brain in chronic lyme neuroborreliosis and may be associated with Alzheimer disease. Journal of Alzheimer’s Disease. 2004;6(6):639–649. doi: 10.3233/jad-2004-6608. [DOI] [PubMed] [Google Scholar]
- 315.Lin WR, Wozniak MA, Cooper RJ, Wilcock GK, Itzhaki RF. Herpesviruses in brain and Alzheimer’s disease. Journal of Pathology. 2002;197:395–402. doi: 10.1002/path.1127. [DOI] [PubMed] [Google Scholar]
- 316.Kountouras J, Boziki M, Gavalas E, et al. Increased cerebrospinal fluid Helicobacter pylori antibody in Alzheimer’s disease. International Journal of Neuroscience. 2009;119(6):765–777. doi: 10.1080/00207450902782083. [DOI] [PubMed] [Google Scholar]
- 317.Choi J, Lee SY, Kim K, Choi BK. Identification of immunoreactive epitopes of the Porphyromonas gingivalis heat shock protein in periodontitis and atherosclerosis. Journal of Periodontal Research. 2011;46(2):240–245. doi: 10.1111/j.1600-0765.2010.01339.x. [DOI] [PubMed] [Google Scholar]
- 318.Roy BF, Sunderland T, Murphy DL, Morihisa JM. Antibody for nerve growth factor detected in patients with Alzheimer’s disease. Annals of the New York Academy of Sciences. 1988;540:398–400. doi: 10.1111/j.1749-6632.1988.tb27113.x. [DOI] [PubMed] [Google Scholar]
- 319.Foley P, Bradford HF, Docherty M, et al. Evidence for the presence of antibodies to cholinergic neurons in the serum of patients with Alzheimer’s disease. Journal of Neurology. 1988;235(8):466–471. doi: 10.1007/BF00314249. [DOI] [PubMed] [Google Scholar]
- 320.Serot JM, Bene MC, Gobert B, Christmann D, Leheup B, Faure GC. Antibodies to choroid plexus in senile dementia of Alzheimer’s disease. Journal of Clinical Pathology. 1992;45(9):781–783. doi: 10.1136/jcp.45.9.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Kingsley BS, Gaskin F, Fu SM. Human antibodies to neurofibrillary tangles and astrocytes in Alzheimer’s disease. Journal of Neuroimmunology. 1988;19(1-2):89–99. doi: 10.1016/0165-5728(88)90038-0. [DOI] [PubMed] [Google Scholar]
- 322.Kanduc D, Stufano A, Lucchese G, Kusalik A. Massive peptide sharing between viral and human proteomes. Peptides. 2008;29(10):1755–1766. doi: 10.1016/j.peptides.2008.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Trost B, Kusalik A, Lucchese G, Kanduc D. Bacterial peptides are intensively present throughout the human proteome. Self/Nonself. 2010;1(1):71–74. doi: 10.4161/self.1.1.9588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Trost B, Lucchese G, Stufano A, Bickis M, Kusalik A, Kanduc D. No human protein is exempt from bacterial motifs, not even one. Self/Nonself. 2010;1(4):328–334. doi: 10.4161/self.1.4.13315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Jonsson R, Nakken B, Halse AK, Skarstein K, Brokstad K, Haga HJ. Heredity and immunology in Sjogren's syndrome. Tidsskr Nor Lægeforen. 2000;120(7):811–814. [PubMed] [Google Scholar]
- 326.Phillips D, Prentice L, Upadhyaya M, et al. Autosomal dominant inheritance of autoantibodies to thyroid peroxidase and thyroglobulin—studies in families not selected for autoimmune thyroid disease. Journal of Clinical Endocrinology and Metabolism. 1991;72(5):973–975. doi: 10.1210/jcem-72-5-973. [DOI] [PubMed] [Google Scholar]
- 327.Pardridge WM. Re-engineering biopharmaceuticals for delivery to brain with molecular Trojan horses. Bioconjugate Chemistry. 2008;19(7):1327–1338. doi: 10.1021/bc800148t. [DOI] [PubMed] [Google Scholar]
- 328.Mallery DL, McEwan WA, Bidgood SR, Towers GJ, Johnson CM, James LC. Antibodies mediate intracellular immunity through tripartite motif-containing 21 (TRIM21). In: Proceedings of the National Academy of Sciences of the United States of America, vol. 107; November 2010; pp. 19985–19990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Vacirca D, Delunardo F, Matarrese P, et al. Autoantibodies to the adenosine triphosphate synthase play a pathogenetic role in Alzheimer’s disease. doi: 10.1016/j.neurobiolaging.2010.05.013. Neurobiology of Aging. http://www.ncbi.nlm.nih.gov/pubmed?term=20594618. In press. [DOI] [PubMed] [Google Scholar]
- 330.Grant WB. Dietary links to Alzheimer’s disease: 1999 Update. Journal of Alzheimer’s Disease. 1999;1(4-5):197–201. doi: 10.3233/jad-1999-14-501. [DOI] [PubMed] [Google Scholar]
- 331.Lopez LB, Kritz-Silverstein D, Barrett-Connor E. High dietary and plasma levels of the omega-3 fatty acid docosahexaenoic acid are associated with decreased dementia risk: the Rancho Bernardo study. Journal of Nutrition, Health and Aging. 2011;15(1):25–31. doi: 10.1007/s12603-011-0009-5. [DOI] [PubMed] [Google Scholar]
- 332.Quinn JF, Raman R, Thomas RG, et al. Docosahexaenoic acid supplementation and cognitive decline in Alzheimer disease: a randomized trial. Journal of the American Medical Association. 2010;304(17):1903–1911. doi: 10.1001/jama.2010.1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Frautschy SA, Cole GM. What was lost in translation in the DHA trial is whom you should intend to treat. Alzheimer's Research & Therapy. 2011;3, article 2 doi: 10.1186/alzrt61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Dai Q, Borenstein AR, Wu Y, Jackson JC, Larson EB. Fruit and vegetable juices and Alzheimer’s disease: the Kame Project. American Journal of Medicine. 2006;119(9):751–759. doi: 10.1016/j.amjmed.2006.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]