Abstract
Radical cystectomy with pelvic lymphadenectomy represents the gold standard for treatment of muscle-invasive bladder cancer. Extent of the lymph node dissection and lymph node involvement during radical cystectomy are the most powerful prognostic factors associated with poor oncological outcome. However, the optimal boundaries of the lymph node dissection during a radical cystectomy are controversial. The published literature based mostly on retrospective studies suggests that increasing the number of nodes excised may have therapeutic and diagnostic benefits without significantly increasing the surgical morbidity. These conclusions are, however, influenced by selection and surgeon biases, inconsistencies in the quality of the surgery, and node count variability. In this paper, we establish the current understanding about the utility of lymphadenectomy during a radical cystectomy for muscle-invasive bladder cancer.
1. Introduction
Bladder cancer (BC) is the seventh most prevalent cancer worldwide and results in significant morbidity and mortality. In the United States, BC is the fourth most common cancer in males and the ninth in females with an estimated 70,980 new cases and 14,330 deaths in 2009 [1]. Muscle-invasive BC (MIBC) accounts for virtually all the mortality from bladder cancer and represents more than a quarter (≈25–40%) of all BC. MIBC spreads from the bladder in a predictable stepwise manner to the lymph nodes and then to visceral organs. Metastatic BC is incurable and invariably fatal. For patients with MIBC, radical cystectomy (RC) with pelvic lymphadenectomy (PLND) represents the mainstay of therapy. The PLND during RC represents both a chance to accurately stage the cancer as well as a chance to remove all the cancer from the body. An extended PLND may have prognostic and therapeutic benefits. However, there is still debate regarding the boundaries of adequate PLND during RC. In this paper, we will define the state of art regarding the extent of PLND and nodal prognostic factors and their effect on oncological outcomes of BC patients.
2. Lymphatic Drainage of the Bladder
The anatomy of lymphatic drainage of the urinary bladder is critically important for definition of the boundaries for an adequate PLND during RC. The bladder lymphatic drainage has well-defined origin from lymphatic plexus within its wall, in the submucosa and extending into the muscles. Lymphatic channels drain through anterior, lateral, and posterior intercalated lymph nodes (LNs) located within the perivesical fat. Efferent lymphatics then drain to the external iliac, obturator, internal iliac, and presacral LNs. Lymphatic trunks leading from the pelvic LNs subsequently drain into more proximal common iliac LNs and then to aortocaval LNs [2, 3]. Skip lesions have been reported, but their rarity suggests that the pelvic LNs are the primary landing site and that metastasis occurs in an orderly progression [2, 4–8].
3. Surgical Boundaries of the Lymphadenectomy
Figure 1 shows the template of extended PLND during RC. Extended PLND include LNs between the aortic bifurcation and common iliac vessels (proximally), the genitofemoral nerve (laterally), the circumflex iliac vein and LN of Cloquet (distally), and the internal iliac vessels (posteriorly), including the obturator fossa and the presacral LNs anterior to the sacral promontory. An extended dissection may also extend superiorly to the level of the inferior mesenteric artery. Importantly, the PLND along the external iliac vessels is completely circumferential while the proximal dissection along the common iliac and great vessels includes anterior and lateral nodal tissues [5, 7, 9]. Standard PLND differs in its cranial boundary which is limited to the level of the common iliac bifurcation. A limited PLND involves the lymph nodes in the obturator fossa.
Figure 1.
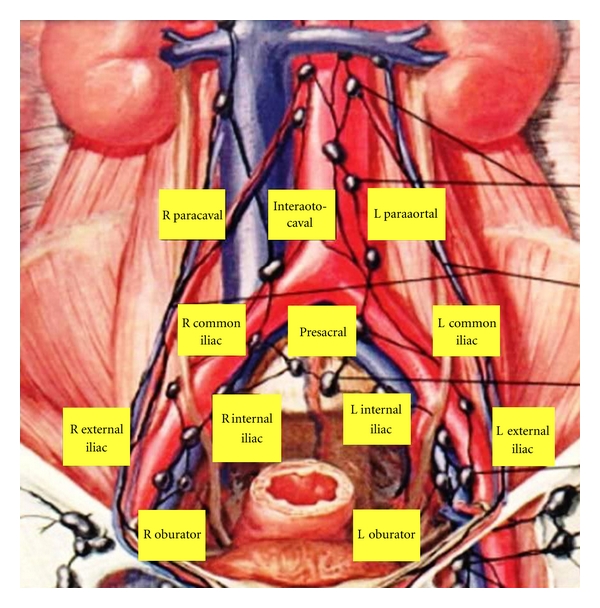
Template of extended lymph node dissection during radical cystectomy.
4. Incidence of Lymph Node Metastasis
The incidence of positive LNs in RC specimens is between 18–30% as shown in Table 1. Predictably, the incidence of LN involvement correlates with T stage, grade, and presence of lympho vascular invasion (LVI) [5, 10, 11]. Table 2 shows the correlation with stage in the largest RC series. The incidence of LN metastasis is ≤5% for <T2, around 25% in T2, and 40–45% in T3/T4 BC.
Table 1.
Incidence of lymph node metastasis in radical cystectomy.
| References | Year | No. of patients | No. of LN metastasis | (%) of LN metastasis |
|---|---|---|---|---|
| Vieweg et al. [12] | 1999 | 682 | 193 | 28.1 |
| Leissner et al. [13] | 2000 | 447 | 136 | 30.4 |
| Herr and Donat [14] | 2001 | 763 | 193 | 25.3 |
| Stein et al. [15] | 2001 | 1,054 | 246 | 23.3 |
| Gschwend et al. [16] | 2002 | 686 | 193 | 28.1 |
| Madersbacher et al. [17] | 2003 | 507 | 121 | 23.9 |
| Vazina et al. [10] | 2004 | 176 | 43 | 24.4 |
| Leissner et al. [5] | 2004 | 290 | 81 | 27.9 |
| Abdel-Latif et al. [11] | 2004 | 418 | 110 | 26.3 |
| Nishiyama et al. [18] | 2004 | 1,113 | 162 | 14.6 |
| Fleischmann et al. [19] | 2005 | 507 | 124 | 24.5 |
| Hautmann et al. [20] | 2006 | 788 | 142 | 18.0 |
| Shariat et al. [21] | 2006 | 833 | 198 | 23.8 |
| Koppie et al. [22] | 2006 | 1,110 | 243 | 21.9 |
| Stein et al. [23] | 2007 | 1,621 | 383 | 23.6 |
| Steven and Poulsen [24] | 2007 | 336 | 64 | 19.0 |
| Wright et al. [25] | 2007 | 5,201 | 1260 | 24.3 |
| Ghoneim et al. [26] | 2008 | 2,720 | 555 | 20.4 |
| Osawa et al. [27] | 2009 | 435 | 83 | 19.1 |
| Bruins et al. [28] | 2009 | 1,600 | 369 | 23.1 |
| Stephenson et al. [29] | 2010 | 763 | 178 | 23.3 |
| Seiler et al. [30] | 2010 | 840 | 162 | 19.3 |
Table 2.
Correlation of pathological T stage with LN metastases.
| Study | Poulsen et al. [31] | Viewg et al. [12] | Stein et al. [15] | Madersbacher et al. [17] | Leissner et al. [5] | Vazina et al. [10] | Abdel-Latif et al. [11] | Hautmann et al. [20] | Ghoneim and Abol-Enein [32] |
|---|---|---|---|---|---|---|---|---|---|
| Year | 1998 | 1999 | 2001 | 2003 | 2004 | 2004 | 2004 | 2006 | 2008 |
| period | 1990–1997 | 1980–1990 | 1971–1997 | 1985–2000 | 1999–2002 | 1992–2002 | 1997–1999 | 1986–2003 | 1971–2000 |
| Total no. of patients | 191 | 686 | 1054 | 507 | 290 | 176 | 418 | 788 | 2720 |
|
| |||||||||
| % of LN metastasis | |||||||||
|
| |||||||||
| pT0, pTis, and pT1 | 3 | 10 | 5 | 2 | 2 | 4 | 4 | 1 | 2 |
| pT2a | 18 | 9 | 18 | 17 | 13 | 16 | 7 | 10 | 8 |
| T2b | 25 | 23 | 27 | 34 | 22 | 40 | 25 | 41 | 19 |
| pT3 | 51 | 43 | 45 | 41 | 44 | 50 | 48 | 44 | 39 |
| pT4 | 44 | 41 | 45 | 50 | 65 | 36 | |||
|
| |||||||||
| Total | 26 | 28 | 23 | 24 | 28 | 24 | 26 | 18 | 20 |
5. Lymphadenectomy: Staging/Prognostic Benefits
Precise staging of LN status is an important clinico-pathological prognostic parameter following RC. Nodal involvement identifies a high-risk group that has the worst oncological outcomes and may benefit from adjuvant systemic therapies. Clearly, extending the field of PLND will increase the number of LNs removed and the chances of identifying positive nodes [5, 23, 24, 33]. Vazina et al. found 16% patients with T3/T4 disease to have LN metastasis proximal to the boundaries of standard PLND and 30% of patients with common iliac LN involvement also had involvement of presacral LNs [10]. Steven and Poulsen found 34.4% of positive LNs above the common iliac bifurcation [24]. An inadequately performed PLND may underestimate the true disease burden and underestimate the need for potentially therapeutic adjuvant therapies. An accurate PLND represents the best way to accurately stage patients with MIBC.
6. Lymphadenectomy: Therapeutic Benefits
Removal of involved lymph nodes theoretically can improve survival as it decreases overall tumor burden and allows the immune system and chemotherapeutics to target a smaller number of cancer cells, potentially with greater efficacy. Indeed, recent retrospective and prospective nonrandomized studies suggest a better oncological outcome from removing more LNs via an extended PLND during RC. Proponents for extended PLND note frequent involvement of nodes outside the standard PLND templates [10, 24, 34]. Some studies found more proximal LN metastases above the cranial boundary of the standard PLND (≈20%) where common iliac, presacral, and LNs above the aortic bifurcation were involved in 15–23%, 6–8%, and 4–10%, respectively [3, 5]. Additionally, up to 50% of patients with limited LN involvement can be rendered disease-free after extended PLND [2, 5]. The benefits of PLND in removing micrometastatic disease appear to be significant in BC. Extended PLND requires an additional time but does not add significantly to the morbidity of the procedure [2, 35–37]. However, there are other studies that did not find an advantage for extended PLND [6, 7, 11]. The difference between these studies may reflect the selection criteria for the patients. Further, while the removal of grossly negative but microscopically involved LN may have a therapeutic benefit, the removal of bulky involved LN is unlikely to improve survival. The level of PLND remains controversial and can only be determined by well-designed carefully controlled prospective randomized studies.
7. Therapeutic Benefits in Node Negative Bladder Cancer
The extent of PLND may act as a surrogate marker for overall surgical quality and survival benefits from PLND in node negative patients during RC were reported [13, 15, 31, 38, 39]. A thorough extended PLND might decrease positive surgical margins, and, hence improve the oncological outcome. The 5-year RFS with organ-confined tumors was 85% with an extended dissection compared to 64% with similar pathology undergoing a more limited PLND [31]. We recommend an extended PLND, whenever possible; even in clinically node negative patients.
8. Nodal Prognostic Factors
The prognosis in patients with lymph node-positive disease can be stratified by the stage of the primary bladder tumor, extent of PLND, the number of lymph nodes removed, the number of LNs involved (tumor burden), LN density, and the presence of nodal extracapsular extension. We would like to highlight the most commonly studied nodal prognostic factors.
8.1. Number of Lymph Nodes Removed
The median nodal counts reported from RC series is considerably variable and ranges from 9 to 30 (Table 3). This number has been used as a surrogate marker for the adequacy of PLND. A standard PLND yields an average of 8–14 nodes while extending PLND up to the aortic bifurcation often yields 25–45 nodes [2, 31, 34]. Different studies suggested different cut point for the number of LNs that should be removed to achieve adequate PLND (Table 4). SEER data showed that PLND and the number of LNs removed are variable, and dissection of at least 10 to 14 nodes during RC is the most important prognostic factor [40]. The number of LNs removed not only suggests the completeness of the PLND, but may have prognostic significance in both LN positive and negative patients [3, 13]. Koppie et al. could not find a minimum number of LNs to be sufficient for optimal oncological outcomes. Instead, the probability of survival continued to increase as the number of LNs removed increases [22].
Table 3.
Median number of lymph nodes removed in cystectomy series.
| References | Year | No. of patients | Median number of LNs removed (range) |
|---|---|---|---|
| Stein et al. [41] | 2003 | 244 | 30 (1–96) |
| Herr [42] | 2003 | 162 | 13 (2–32) |
| Kassouf et al. [43] | 2006 | 108 | 12 (1–58) |
| Kassouf et al. [44] | 2008 | 248 | 12 (2–58) |
| Fleischmann et al. [45] | 2005 | 101 | 22 (10–43) |
| Wright et al. [25] | 2008 | 1260 | 9 (1–75) |
| Steven et al. [24] | 2007 | 64 | 27 (11–49) |
| Abdel–Latif et al. [11] | 2004 | 110 | 18 (mean) |
| Lerner et al. [46] | 1993 | 132 | 31 (3–96) |
| Leissner et al. [13] | 2000 | 302 | 15 (1–46) |
| Herr et al. [47] | 2004 | 268 | 10 (0–54) |
| Koppie et al. [22] | 2006 | 1042 | 9 (0–53) |
| Poulsen et al. [31] | 1998 | 117 | 25 (9–67) extended |
| Dhar et al. [48] | 2008 | 336 (Cleveland Clinic) | 22 (10–43) extended |
| 322 (University of Bern) |
Table 4.
Suggested number of LNs to be removed to achieve better oncological outcomes.
| References | Year | No. of patients | Median number of LNs removed (range) | Cut-off number of LNs to be removed |
|---|---|---|---|---|
| Stein et al. [41] | 2003 | 244 | 30 (1–96) | 15 |
| Konety et al. [49] | 2003 | 361 | N/A | 10–14 |
| Herr [42] | 2003 | 162 | 13 (2–32) | 13 |
| Kassouf et al. [44] | 2008 | 248 | 12 (2–58) | 12 |
| Fleischmann et al. [45] | 2005 | 101 | 22 (10–43) | 5 |
| Wright et al. [25] | 2008 | 1260 | 9 (1–75) | 10 |
| Leissner et al. [13] | 2000 | 302 | 15 (1–46) | 16 |
| Herr et al. [47] | 2004 | 268 | 10 (0–54) | 10 |
| Herr et al. [39] | 2002 | 322 | 8 (0–44) for N0 | 8 for N0 |
| 11 (1–25) for N+ | 11 for N+ | |||
| Fang et al. [50] | 2010 | 349 | 17 (0–53) | 16 |
| Dangle et al. [33] | 2010 | 120 | 37 (11–87) | 23–27 |
| Shirotake et al. [51] | 2010 | 169 | 10 for N0 | 9 for N0 |
| 13 for N+ |
Unfortunately, with the striking interinstitution and intrainstitution variability in node counts and variability within patients, it is hard to define an exact minimum number of LNs to be removed. The same extended PLND may yield 20 or 80 LN depending on the patient, exposure to chemotherapy, surgical technique, institution at which performed, pathologist examining the LNs, and protocol used to evaluate LNs number. Thus, a cutoff of 30 would render the same extended PLND inadequate or adequate. We believe that the extent of PLND is more important marker for better surgical quality, and, finally, oncological outcome until pathologic processing and aforementioned variables can be addressed.
8.2. Lymph Node Yield
Many factors might explain the variability in node yield. Clinical, anatomical, pathological, surgical, and institutional factors may play a role [2, 4]. Old age and associated comorbidities may hinder extended PLND [2, 52]. There might be some anatomic variability in the number of nodes present in different individuals [4]. Tumor stage may be associated with nodal yield [2, 4, 39]. On the other hand, negative margin status has been associated with higher nodal yield [4, 47]. Recent BCG or neoadjuvant chemotherapy might have an effect, probably by causing inflammation and fibrosis thus helping more nodal yield [4]. Sending LNs in separate packages was reported to increase the nodal yield [15, 34]. The method of pathologic evaluation including the use of fat-clearing solutions may play a role as well [2, 4]. While there were contradictory reports about the effect of surgeon volume on LN yield [4, 47], academic or teaching hospitals with a higher RC volume tend to report higher LN counts [4, 47, 53]. Recently, Fang et al. implement a policy that at least 16 LNs has to be examined pathologically. They showed that implementation of this policy can improve the survival due to increased awareness to perform a more thorough PLND [50].
8.3. Number of Positive Nodes (Tumor Burden)
The number of positive LNs (tumor burden) is an important prognostic factor following RC [3, 7, 13, 15, 41]. Recurrence and survival are inversely related to an increasing number of positive LNs. Some studies reported the absolute number of LNs involved as an independent prognostic factor. Others defined cutoff numbers for worse prognosis [40]. Herr et al. determined a cut-off of 4 positive LNs [39], Steven and Poulsen detrmined 5 positive LNS [24], and Stein et al. showed significantly worse survival in patients with >8 metastatic LNs [41]. Furthermore, the study from Mansoura showed a significance difference in prognosis when stratifying positive LNs (1 versus 2–5 versus 5) [11]. This was also the case in a population-based study from the SEER database (1 versus 2 versus 3 versus >3) [25]. Collectively, It is obvious that larger tumor burden in LNs is associated with poor oncological outcomes. Further, bulky positive LNs are invariably associated with a poor prognosis [29].
9. The Concept of “Lymph Node Density”
The LN density could be a useful prognostic concept because it combines the extent of PLND as indicated by the total number of LNs removed and the tumor burden as indicated by the number of positive nodes. Herr and Stein were the first to introduce the concept of LN density (number of positive nodes/number of removed nodes) with a cutoff of 20% to stratify outcomes [41, 42]. Table 5 describes the cut-off values suggested for LN density in different studies and the oncological outcomes based on these cut-off values. A pooled analysis of MD Anderson and Memorial Sloan-Kettering Cancer Centers showed that LN density is superior to TNM nodal status in predicting oncological outcomes after RC [36]. Nevertheless, this index can be useful only if there is a standard number of nodes that have to be removed and a standard level of PLND. Certainly, a LN density of 20% based on 1 positive LN out of 5 LNs removed is different than 20% based on 8 positive out of 40 LNs. Perhaps, this is the reason why there has not been widespread clinical use of this parameter since its introduction in 2003.
Table 5.
Cut-off lymph node densities and their effect upon oncological outcomes.
| References | Year | No. of patients | Median number of LNs removed (range) | Cut-off PLND | 5-Y survival rates | |
|---|---|---|---|---|---|---|
| Below cut-off | Above cut-off | |||||
| Stein et al. [41] | 2003 | 244 | 30 (1–96) | 20 | 17 | 44 |
| Herr [42] | 2003 | 162 | 13 (2–32) | 20 | 8* | 64* |
| Kassouf et al. [43] | 2006 | 108 | 12 (1–58) | 25 | 11 | 38 |
| Kassouf et al. [44] | 2008 | 248 | 12 (2–58) | 20 | 15* | 55* |
| Fleischmann et al. [45] | 2005 | 101 | 22 (10–43) | 20 | 15 | 41 |
| Steven and Poulsen [24] | 2007 | 64 | 27 (11–49) | 20 | 25 | 47 |
| Abdel–Latif et al. [11] | 2004 | 110 | 18 (mean) | 20 | 16 | 39 |
| Wiesner et al. [54] | 2009 | 152 | 33 (15–77) | 11 | 8* | 34* |
| Osawa et al. [27] | 2009 | 435 | 12 (1–80) | 25 | 12* | 51* |
All studies reported RFS except *reported CSS.
10. Extracapsular Extension of Lymph Node Metastasis
Extracapsular extension (perforation of the capsule of LN by tumor tissue with extranodal growth) has recently been shown to double the risk of recurrence when compared to intranodal confined LN metastasis. Fleischman et al. evaluated 101 patients who underwent RC and extended PLND for LN+ disease and analyzed the influence of extracapsular extension (found in 58% of the patients) on patient prognoses. Patients with extracapsular extension had a significantly decreased recurrence free survival (RFS) (median, 12 versus 60 months, P < .001) and overall survival (OS) (median, 16 versus 60 months, P < .001) compared with those with intranodal metastases. Multivariate analyses confirmed that extracapsular extension of LN metastases was the strongest negative predictor for RFS [19]. However, others did not find a significant association between extracapsular extension and survival after RC, leading to issue of whether this pathological finding is really of importance [55].
11. The Concept of “Sentinel Lymph Node”
The sentinel node is defined as the initial site of lymphatic drainage from a primary tumor. Determination of sentinel node for BC should be on individualized basis rather than on anatomic location of primary tumor due to the variability of lymphatic drainage [4]. Ghoneim and Abol-Enein introduced the concept of sentinel region (intrapelvic LNs) rather than sentinel node [6, 7]. Involvement of the intrapelvic LNs may be the first step in nodal metastasis in most BCs and skip lesions might be very rare [26, 47, 52, 55–57]. However, higher number of patients and longer followup is needed before widespread practice is accepted.
Recently, Studer group used multimodality technique to locate the primary lymphatic landing sites of the bladder. Their technique counted upon cystoscopic-guided injection of technetium nanocolloid followed by preoperative radioactive LN detection with SPECT/CT followed by intraoperative verification with gamma probe. They found that limited pelvic PLND removed only about 50% of all primary lymphatic landing sites while extending the PLND up to the ureteroiliac crossing removed 90% [8]. Analysis of their study proves that the template or extent of PLND is more important than merely the number of LNs removed [58]. The concept of sentinel node remains investigational in BC. If sentinel nodes could be accurately identified on individual basis, this could guide the decision about the extent of PLND. Although, extended PLND can be safely and routinely performed with minimal additional morbidity, we do not currently see a need to compromise outcomes of patients with BC with a suboptimal nodal dissection and reliance on frozen section analyses.
12. A Tailored Approach to Lymphadenectomy
Tailoring PLND based on the clinical stage, so that patients with advanced tumors or evidence of nodal involvement would be treated with an extended PLND, whereas those with organ-confined disease and no evidence of nodal involvement would undergo standard PLND, has been advocated. However, the use of clinical stage of the primary tumor for determining of the extent of PLND is problematic [38]. Understaging could happen in approximately half of patients with clinically organ-confined disease [38, 59]. Intraoperative finding including inspection and palpation of more proximal lymphatic regions may miss a substantial percentage of positive LNs [38]. If the morbidity of PLND is minimal, then there should be minimal downside to the use of an extended PLND in all patients. Currently, there are no reliable models to guide the decision regarding the extent of PLND.
13. Morbidity of Lymphadenectomy
Early complications of 28% and perioperative mortality rates of 2.6–3% have been reported in large RC series [15, 26]. An extended PLND may prolong operative time by about 60 minutes. However, it does not appear to increase morbidity or mortality compared to the standard approach [2, 35–37]. Comparing LN positive versus LN negative cases, extended versus standard PLND confirmed that there are no significant differences in morbidity or mortality [2, 35–37, 41]. Extended PLND is a safe option in experienced hands that may improve oncological outcomes by decreasing positive surgical margins and resection of undetected micrometastases [36, 38]. Despite that the administration of neoadjuvant radiation or chemotherapy before RC may not increase the morbidity and mortality. Patients who have received these treatments should be judged carefully before performing an extended PLND, as there might be a higher risk of complications [9, 35, 36].
14. Laparoscopic-/Robotic-Assisted Surgery
Laparoscopic-/robotic-assisted RC and PLND were reported as safe feasible procedures with acceptable nodal yield and potentially equivalent oncological outcomes to open RC with no added morbidities [56, 60]. Complete removal of the LN-bearing tissue up to aortic bifurcation or inferior mesenteric artery is more challenging using minimally invasive modalities. Recently, extended PLND has been demonstrated with the robotic system, with comparable LN yields [57, 61, 62].
We believe that without long-term functional and oncologic outcome data, laparoscopic- and robotic-assisted RC should be considered investigative techniques, and patients chosen for these modalities should be appropriately selected and counseled.
15. Future Directions
Many of the controversies regarding the extent and the utility of PLND in RC stem from the fact that data in support or against their use have been obtained from retrospective analyses of databases and trials. As such none of these studies were powered to answer the questions regarding the utility of PLND in RC. A multicenter prospective randomized clinical trial is in the final stages of approval by SWOG (PI: Seth Lerner, Baylor College of Medicine), and it randomizes patients to standard versus extended lymphadenectomy during RC for bladder cancer. The trial is powered to detect differences in survival and when completed may truly establish the role of PLND on the outcomes of patients with bladder cancer.
16. Conclusions
The incidence of nodal disease in BC is around 25% and is influenced by other pathological factors, most importantly the pT stage. Extended PLND may provide prognostic and therapeutic advantages in both LN-positive and negative patients without significantly increasing morbidity. However, the extent of PLND during RC needs better definition through prospective randomized studies with long-term followup. Laparoscopic-/robotic-assisted RC and PLND are still new modalities that need longer evaluation before recommending for more patients.
Abbreviations
- BC:
Bladder cancer
- MIBC:
Muscle-invasive bladder cancer
- RC:
Radical cystectomy
- PLND:
Pelvic lymph node dissection = lymphadenectomy
- LN:
Lymph node
- LVI:
Lymphovascular invasion
- RFS:
Recurrence-free survival
- CSS:
Cancer-specific survival
- OS:
Overall survival
- SPECT/CT:
Single-photon emission computed tomography.
References
- 1.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer Journal for Clinicians. 2009;59(4):225–249. doi: 10.3322/caac.20006. [DOI] [PubMed] [Google Scholar]
- 2.Raj GV, Bochner BH. Radical cystectomy and lymphadenectomy for invasive bladder cancer: towards the evolution of an optimal surgical standard. Seminars in Oncology. 2007;34(2):110–121. doi: 10.1053/j.seminoncol.2006.12.011. [DOI] [PubMed] [Google Scholar]
- 3.Buscarini M, Josephson DY, Stein JP. Lymphadenectomy in bladder cancer: a review. Urologia Internationalis. 2007;79(3):191–199. doi: 10.1159/000107949. [DOI] [PubMed] [Google Scholar]
- 4.Sharir S, Fleshner NE. Lymph node assessment and lymphadenectomy in bladder cancer. Journal of Surgical Oncology. 2009;99(4):225–231. doi: 10.1002/jso.21253. [DOI] [PubMed] [Google Scholar]
- 5.Leissner J, Ghoneim MA, Abol-Enein H, et al. Extended radical lymphadenectomy in patients with urothelial bladder cancer: results of a prospective multicenter study. Journal of Urology. 2004;171(1):139–144. doi: 10.1097/01.ju.0000102302.26806.fb. [DOI] [PubMed] [Google Scholar]
- 6.Ghoneim MA, Abol-Enein H. Lymphadenectomy with cystectomy: is it necessary and what is its extent? European Urology. 2004;46(4):457–461. doi: 10.1016/j.eururo.2004.06.010. [DOI] [PubMed] [Google Scholar]
- 7.Abol-Enein H, El-Baz M, Abd El-Hameed MA, Abdel-Latif M, Ghoneim MA. Lymph node involvement in patients with bladder cancer treated with radical cystectomy: a patho-anatomical study—a single center experience. Journal of Urology. 2004;172(5 I):1818–1821. doi: 10.1097/01.ju.0000140457.83695.a7. [DOI] [PubMed] [Google Scholar]
- 8.Roth B, Wissmeyer MP, Zehnder P, et al. A new multimodality technique accurately maps the primary lymphatic landing sites of the bladder. European Urology. 2010;57(2):205–211. doi: 10.1016/j.eururo.2009.10.026. [DOI] [PubMed] [Google Scholar]
- 9.Stein JP, Quek ML, Skinner DG. Lymphadenectomy for invasive bladder cancer. II. Technical aspects and prognostic factors. British Journal of Urology International. 2006;97(2):232–237. doi: 10.1111/j.1464-410X.2006.05901.x. [DOI] [PubMed] [Google Scholar]
- 10.Vazina A, Dugi D, Shariat SF, Evans J, Link R, Lerner SP. Stage specific lymph node metastasis mapping in radical cystectomy specimens. Journal of Urology. 2004;171(5):1830–1834. doi: 10.1097/01.ju.0000121604.58067.95. [DOI] [PubMed] [Google Scholar]
- 11.Abdel-Latif M, Abol-Enein H, El-Baz M, Ghoneim MA. Nodal involvement in bladder cancer cases treated with radical cystectomy: incidence and prognosis. Journal of Urology. 2004;172(1):85–89. doi: 10.1097/01.ju.0000132132.72351.4c. [DOI] [PubMed] [Google Scholar]
- 12.Vieweg J, Gschwend JE, Herr HW, Fair WR. Pelvic lymph node dissection can be curative in patients with node positive bladder cancer. Journal of Urology. 1999;161(2):449–454. [PubMed] [Google Scholar]
- 13.Leissner J, Hohenfellner R, Thüroff JW, Wolf HK. Lymphadenectomy in patients with transitional cell carcinoma of the urinary bladder; Significance for staging and prognosis. British Journal of Urology International. 2000;85(7):817–823. doi: 10.1046/j.1464-410x.2000.00614.x. [DOI] [PubMed] [Google Scholar]
- 14.Herr HW, Donat SM. Outcome of patients with grossly node positive bladder cancer after pelvic lymph node dissection and radical cystectomy. Journal of Urology. 2001;165(1):62–64. doi: 10.1097/00005392-200101000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Stein JP, Lieskovsky G, Cote R, et al. Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1,054 patients. Journal of Clinical Oncology. 2001;19(3):666–675. doi: 10.1200/JCO.2001.19.3.666. [DOI] [PubMed] [Google Scholar]
- 16.Gschwend JE, Dahm P, Fair WR. Disease specific survival as endpoint of outcome for bladder cancer patients following radical cystectomy. European Urology. 2002;41(4):440–448. doi: 10.1016/s0302-2838(02)00060-x. [DOI] [PubMed] [Google Scholar]
- 17.Madersbacher S, Hochreiter W, Burkhard F, et al. Radical cystectomy for bladder cancer today—a homogeneous series without neoadjuvant therapy. Journal of Clinical Oncology. 2003;21(4):690–696. doi: 10.1200/JCO.2003.05.101. [DOI] [PubMed] [Google Scholar]
- 18.Nishiyama H, Habuchi T, Watanabe J, et al. Clinical outcome of a large-scale multi-institutional retrospective study for locally advanced bladder cancer: a survey including 1131 patients treated during 1990–2000 in Japan. European Urology. 2004;45(2):176–181. doi: 10.1016/j.eururo.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 19.Fleischmann A, Thalmann GN, Markwalder R, Studer UE. Prognostic implications of extracapsular extension of pelvic lymph node metastases in urothelial carcinoma of the bladder. American Journal of Surgical Pathology. 2005;29(1):89–95. doi: 10.1097/01.pas.0000147396.08853.26. [DOI] [PubMed] [Google Scholar]
- 20.Hautmann RE, Gschwend JE, de Petriconi RC, Kron M, Volkmer BG. Cystectomy for transitional cell carcinoma of the bladder: results of a surgery only series in the neobladder era. Journal of Urology. 2006;176(2):486–492. doi: 10.1016/j.juro.2006.03.038. [DOI] [PubMed] [Google Scholar]
- 21.Shariat SF, Karakiewicz PI, Palapattu GS, et al. Outcomes of radical cystectomy for transitional cell carcinoma of the bladder: a contemporary series from the Bladder Cancer Research Consortium. Journal of Urology. 2006;176(6):2414–2422. doi: 10.1016/j.juro.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Koppie TM, Vickers AJ, Vora K, Dalbagni G, Bochner BH. Standardization of pelvic lymphadenectomy performed at radical cystectomy: can we establish a minimum number of lymph nodes that should be removed? Cancer. 2006;107(10):2368–2374. doi: 10.1002/cncr.22250. [DOI] [PubMed] [Google Scholar]
- 23.Stein JP, Penson DF, Cai J, et al. Radical cystectomy with extended lymphadenectomy: evaluating separate package versus en bloc submission for node positive bladder cancer. Journal of Urology. 2007;177(3):876–882. doi: 10.1016/j.juro.2006.10.043. [DOI] [PubMed] [Google Scholar]
- 24.Steven K, Poulsen AL. Radical cystectomy and extended pelvic lymphadenectomy: survival of patients with lymph node metastasis above the bifurcation of the common iliac vessels treated with surgery only. Journal of Urology. 2007;178(4):1218–1224. doi: 10.1016/j.juro.2007.05.160. [DOI] [PubMed] [Google Scholar]
- 25.Wright JL, Lin DW, Porter MP. The association between extent of lymphadenectomy and survival among patients with lymph node metastases undergoing radical cystectomy. Cancer. 2008;112(11):2401–2408. doi: 10.1002/cncr.23474. [DOI] [PubMed] [Google Scholar]
- 26.Ghoneim MA, Abdel-Latif M, El-Mekresh M, et al. Radical cystectomy for carcinoma of the bladder: 2,720 consecutive cases 5 years later. Journal of Urology. 2008;180(1):121–127. doi: 10.1016/j.juro.2008.03.024. [DOI] [PubMed] [Google Scholar]
- 27.Osawa T, Abe T, Shinohara N, et al. Role of lymph node density in predicting survival of patients with lymph node metastases after radical cystectomy: a multi-institutional study. International Journal of Urology. 2009;16(3):274–278. doi: 10.1111/j.1442-2042.2008.02221.x. [DOI] [PubMed] [Google Scholar]
- 28.Bruins HM, Huang GJ, Cai J, Skinner DG, Stein JP, Penson DF. Clinical outcomes and recurrence predictors of lymph node positive urothelial cancer after cystectomy. Journal of Urology. 2009;182(5):2182–2187. doi: 10.1016/j.juro.2009.07.017. [DOI] [PubMed] [Google Scholar]
- 29.Stephenson AJ, Gong MC, Campbell SC, Fergany AF, Hansel DE. Aggregate lymph node metastasis diameter and survival after radical cystectomy for invasive bladder cancer. Urology. 2010;75(2):382–386. doi: 10.1016/j.urology.2009.07.1259. [DOI] [PubMed] [Google Scholar]
- 30.Seiler R, Von Gunten M, Thalmann GN, Fleischmann A. Pelvic lymph nodes: distribution and nodal tumour burden of urothelial bladder cancer. Journal of Clinical Pathology. 2010;63(6):504–507. doi: 10.1136/jcp.2009.075077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Poulsen AL, Horn T, Steven K. Radical cystectomy: extending the limits of pelvic lymph node dissection improves survival for patients with bladder cancer confined to the bladder wall. The Journal of urology. 1998;160(6):2015–2020. [PubMed] [Google Scholar]
- 32.Ghoneim MA, Abol-Enein H. Management of muscle-invasive bladder cancer: an update. Nature Clinical Practice Urology. 2008;5(9):501–508. doi: 10.1038/ncpuro1202. [DOI] [PubMed] [Google Scholar]
- 33.Dangle PP, Gong MC, Bahnson RR, Pohar KS. How do commonly performed lymphadenectomy templates influence bladder cancer nodal stage? Journal of Urology. 2010;183(2):499–504. doi: 10.1016/j.juro.2009.09.080. [DOI] [PubMed] [Google Scholar]
- 34.Bochner BH, Cho D, Herr HW, Donat M, Kattan MW, Dalbagni G. Prospectively packaged lymph node dissections with radical cystectomy: evaluation of node count variability and node mapping. Journal of Urology. 2004;172(4, part 1):1286–1290. doi: 10.1097/01.ju.0000137817.56888.d1. [DOI] [PubMed] [Google Scholar]
- 35.Ku JAH. Role of pelvic lymphadenectomy in the treatment of bladder cancer: a mini review. Korean Journal of Urology. 2010;51(6):371–378. doi: 10.4111/kju.2010.51.6.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yafi FA, Kassouf W. Role of lymphadenectomy for invasive bladder cancer. Journal of the Canadian Urological Association. 2009;3(6, supplement 4):S206–S210. doi: 10.5489/cuaj.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brössner C, Pycha A, Toth A, Mian C, Kuber W. Does extended lymphadenectomy increase the morbidity of radical cystectomy? British Journal of Urology International. 2004;93(1):64–66. doi: 10.1111/j.1464-410x.2004.04557.x. [DOI] [PubMed] [Google Scholar]
- 38.Sanderson KM, Skinner D, Stein JP. The prognostic and staging value of lymph node dissection in the treatment of invasive bladder cancer. Nature Clinical Practice Urology. 2006;3(9):485–494. doi: 10.1038/ncpuro0582. [DOI] [PubMed] [Google Scholar]
- 39.Herr HW, Bochner BH, Dalbagni G, Donat SM, Reuter VE, Bajorin DF. Impact of the number of lymph nodes retrieved on outcome in patients with muscle invasive bladder cancer. Journal of Urology. 2002;167(3):1295–1298. [PubMed] [Google Scholar]
- 40.Konety BR, Joslyn SA. Factors influencing aggressive therapy for bladder cancer: an analysis of data from the SEER program. Journal of Urology. 2003;170(5):1765–1771. doi: 10.1097/01.ju.0000091620.86778.2e. [DOI] [PubMed] [Google Scholar]
- 41.Stein JP, Cai J, Groshen S, Skinner DG. Risk factors for patients with pelvic lymph node metastases following radical cystectomy with en bloc pelvic lymphadenectomy: the concept of lymph node density. Journal of Urology. 2003;170(1):35–41. doi: 10.1097/01.ju.0000072422.69286.0e. [DOI] [PubMed] [Google Scholar]
- 42.Herr HW. Superiority of ratio based lymph node staging for bladder cancer. Journal of Urology. 2003;169(3):943–945. doi: 10.1097/01.ju.0000032474.22093.06. [DOI] [PubMed] [Google Scholar]
- 43.Kassouf W, Leibovici D, Munsell MF, Dinney CP, Grossman HB, Kamat AM. Evaluation of the relevance of lymph node density in a contemporary series of patients undergoing radical cystectomy. Journal of Urology. 2006;176(1):53–57. doi: 10.1016/S0022-5347(06)00510-6. [DOI] [PubMed] [Google Scholar]
- 44.Kassouf W, Agarwal PK, Herr HW, et al. Lymph node density is superior to TNM nodal status in predicting disease-specific survival after radical cystectomy for bladder cancer: analysis of pooled data from MDACC and MSKCC. Journal of Clinical Oncology. 2008;26(1):121–126. doi: 10.1200/JCO.2007.12.9247. [DOI] [PubMed] [Google Scholar]
- 45.Fleischmann A, Thalmann GN, Markwalder R, Studer UE. Extracapsular extension of pelvic lymph node metastases from urothelial carcinoma of the bladder is an independent prognostic factor. Journal of Clinical Oncology. 2005;23(10):2358–2365. doi: 10.1200/JCO.2005.03.084. [DOI] [PubMed] [Google Scholar]
- 46.Lerner SP, Skinner DG, Lieskovsky G, et al. The rationale for en bloc pelvic lymph node dissection for bladder cancer patients with nodal metastases: long-term results. Journal of Urology. 1993;149(4):758–765. doi: 10.1016/s0022-5347(17)36200-6. [DOI] [PubMed] [Google Scholar]
- 47.Herr HW, Faulkner JR, Grossman HB, et al. Surgical factors influence bladder cancer outcomes: a cooperative group report. Journal of Clinical Oncology. 2004;22(14):2781–2789. doi: 10.1200/JCO.2004.11.024. [DOI] [PubMed] [Google Scholar]
- 48.Dhar NB, Klein EA, Reuther AM, Thalmann GN, Madersbacher S, Studer UE. Outcome after radical cystectomy with limited or extended pelvic lymph node dissection. Journal of Urology. 2008;179(3):873–878. doi: 10.1016/j.juro.2007.10.076. [DOI] [PubMed] [Google Scholar]
- 49.Konety BR, Joslyn SA, O’Donnell MA. Extent of pelvic lymphadenectomy and its impact on outcome in patients diagnosed with bladder cancer: analysis of data from the surveillance, epidemiology and end results program data base. Journal of Urology. 2003;169(3):946–950. doi: 10.1097/01.ju.0000052721.61645.a3. [DOI] [PubMed] [Google Scholar]
- 50.Fang AC, Ahmad AE, Whitson JM, Ferrell LD, Carroll PR, Konety BR. Effect of a minimum lymph node policy in radical cystectomy and pelvic lymphadenectomy on lymph node yields, lymph node positivity rates, lymph node density, and survivorship in patients with bladder cancer. Cancer. 2010;116(8):1901–1908. doi: 10.1002/cncr.25011. [DOI] [PubMed] [Google Scholar]
- 51.Shirotake S, Kikuchi E, Matsumoto K, et al. Role of pelvic lymph node dissection in lymph node-negative patients with invasive bladder cancer. Japanese Journal of Clinical Oncology. 2009;40(3):247–251. doi: 10.1093/jjco/hyp147. [DOI] [PubMed] [Google Scholar]
- 52.Huang WC, Bochner BH. Current status of establishing standards for lymphadenectomy in the treatment of bladder cancer. Current Opinion in Urology. 2005;15(5):315–319. doi: 10.1097/01.mou.0000173777.41262.7d. [DOI] [PubMed] [Google Scholar]
- 53.Hollenbeck BK, Ye Z, Wong SL, Montie JE, Birkmeyer JD. Hospital lymph node counts and survival after radical cystectomy. Cancer. 2008;112(4):806–812. doi: 10.1002/cncr.23234. [DOI] [PubMed] [Google Scholar]
- 54.Wiesner C, Salzer A, Thomas C, et al. Cancer-specific survival after radical cystectomy and standardized extended lymphadenectomy for node-positive bladder cancer: prediction by lymph node positivity and density. British Journal of Urology International. 2009;104(3):331–335. doi: 10.1111/j.1464-410X.2009.08403.x. [DOI] [PubMed] [Google Scholar]
- 55.Kassouf W, Leibovici D, Luongo T, et al. Relevance of extracapsular extension of pelvic lymph node metastases in patients with bladder cancer treated in the contemporary era. Cancer. 2006;107(7):1491–1495. doi: 10.1002/cncr.22139. [DOI] [PubMed] [Google Scholar]
- 56.Pruthi RS, Wallen EM. Robotic-assisted laparoscopic pelvic lymphadenectomy for bladder cancer: a surgical atlas. Journal of Laparoendoscopic and Advanced Surgical Techniques. 2009;19(1):71–74. doi: 10.1089/lap.2008.0207. [DOI] [PubMed] [Google Scholar]
- 57.Lavery HJ, Martinez-Suarez HJ, Abaza R. Robotic extended pelvic lymphadenectomy for bladder cancer with increased nodal yield. doi: 10.1111/j.1464-410X.2010.09789.x. British Journal of Urology International. In press. [DOI] [PubMed] [Google Scholar]
- 58.Herr HW. Extent of pelvic lymph node dissection during radical cystectomy: where and why! European Urology. 2010;57(2):212–213. doi: 10.1016/j.eururo.2009.10.028. [DOI] [PubMed] [Google Scholar]
- 59.Shariat SF, Palapattu GS, Karakiewicz PI, et al. Discrepancy between clinical and pathologic stage: impact on prognosis after radical cystectomy. European Urology. 2007;51(1):137–151. doi: 10.1016/j.eururo.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 60.Ghavamian R, Hakimi AA. Lymph node dissection for bladder cancer: the issue of extent and feasibility in the minimally invasive era. Expert Review of Anticancer Therapy. 2009;9(12):1783–1792. doi: 10.1586/era.09.147. [DOI] [PubMed] [Google Scholar]
- 61.Kasraeian A, Barret E, Cathelineau X, et al. Robot-assisted laparoscopic cystoprostatectomy with extended pelvic lymphadenectomy, extracorporeal enterocystoplasty, and intracorporeal enterourethral anastomosis: initial montsouris experience. Journal of Endourology. 2010;24(3):409–413. doi: 10.1089/end.2009.0209. [DOI] [PubMed] [Google Scholar]
- 62.Woods M, Thomas R, Davis R, et al. Robot-assisted extended pelvic lymphadenectomy. Journal of Endourology. 2008;22(6):1297–1302. doi: 10.1089/end.2008.0075. [DOI] [PubMed] [Google Scholar]


