Abstract
Twenty-one fourth-year medical students were given a brief lecture on ultrasound of the knee and fifteen minutes of supervised ultrasound scanning of three cadavers which had been injected with saline to give varying degrees of knee effusions. Each student was then individually observed and required to scan both knees of a cadaver different from the practice cadavers and identify the patella, the femur, the quadriceps tendon and if a suprapatellar effusion was present, and which knee had the larger effusion. All twenty-one students correctly identified all anatomical structures, suprapatellar effusions, and which knee had the larger effusion. Identifying a knee effusion can be an important clinical finding in diagnosing and managing a patient with knee complaints. Fourth-year medical students can learn to identify knee effusions with ultrasound following a brief introductory lecture and hands-on scanning practice session.
1. Introduction
Recognizing an effusion in a symptomatic knee is an important finding in many rheumatologic conditions. It is not always easy to determine if a knee effusion is present on physical examination, especially if the effusion is small or the patient is obese. Ultrasound is a safe, quick, and accurate method to identify a knee effusion. A study was conducted to determine if after a brief musculoskeletal ultrasound workshop, fourth-year medical students with little ultrasound experience could learn to scan and identify anatomical landmarks in the knee, and determine if an effusion was present.
2. Subjects and Methods
Twenty-one fourth-year medical students volunteered to participate in the study. Each student completed a short questionnaire about their prior ultrasound experience. The group attended a thirty-minute didactic PowerPoint presentation consisting of a brief introduction of the physics of ultrasound, the anatomy of the knee, ultrasound scanning techniques of the knee and a review of normal and abnormal ultrasound images, including knee effusions. After the presentation, students observed a faculty member performing a suprapatellar longitudinal scan of the knee of a cadaver that had previously been injected with normal saline to produce a small effusion in the suprapatellar bursa. The students then had approximately 15 minutes of supervised scanning on three cadavers which had been injected with saline to give varying degrees of knee effusions. Students were taught to identify the femur, the quadriceps tendon, the patella, and a suprapatellar bursa effusion, if present.
After the instructional session, each student was individually observed scanning a cadaver different from the practice cadavers. The knees of the test cadaver had previously been injected with normal saline in the suprapatellar bursa to produce small ultrasound detectable effusions but with one effusion slightly larger than the other. On visual inspection of the knees, there was no evidence of effusion in either knee (i.e., no suprapatellar bulge sign). Each student was observed for the proper scanning technique of the suprapatellar longitudinal view of each knee. The student was required to identify the quadriceps tendon, the patella, and the area of the suprapatellar bursa, and to state if an effusion was present and, if so, which knee had the larger effusion (Figure 1). After the workshop and testing, the students had the opportunity to anonymously comment and rate the value of the workshop.
Figure 1.
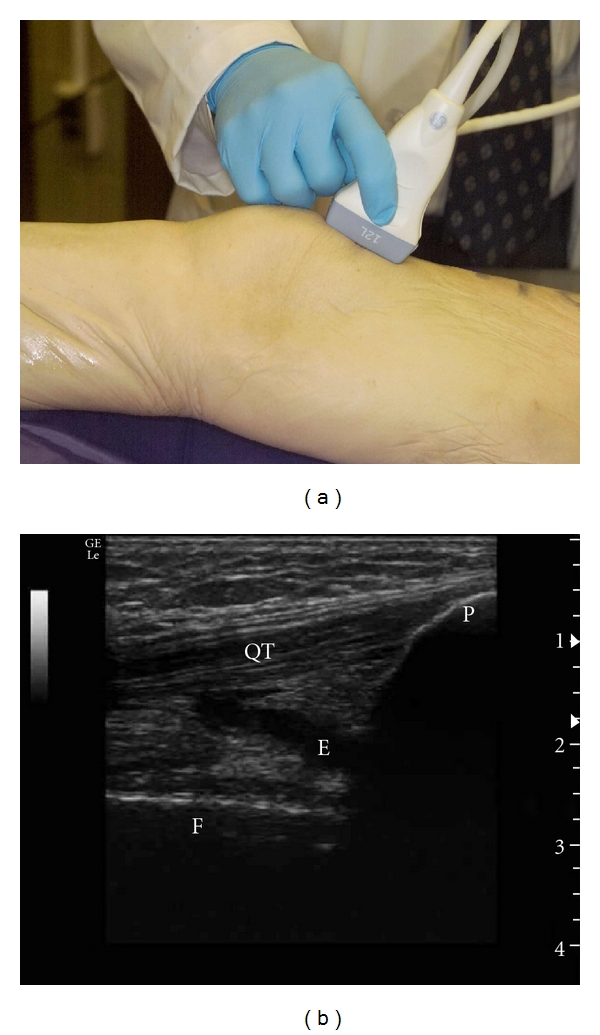
(a) Suprapatellar longitudinal scan of the knee. (b) Ultrasound image of the suprapatellar longitudinal view of the test cadaver knee with a small effusion (P: patella; QT: quadriceps tendon; E: effusion; F: femur).
Four LOGIQ e (General Electric Healthcare) hand-carried ultrasound machines with high-frequency (12 MHz) linear probes were used for the demonstration, practice, and the testing.
3. Results
3.1. Previous Ultrasound Experience
Of the 21 students participating in the study, 11 had no prior hands-on experience with ultrasound and 19 of the 21 had no musculoskeletal ultrasound experience.
3.2. Practical Examination
All 21 students correctly performed suprapatellar longitudinal scans on both knees of the test cadaver. All students identified all anatomic structures correctly on both knees, and all students correctly identified the knee with the larger effusion.
3.3. Workshop Evaluation
Twenty students rated the workshop as very good or outstanding. Ten students added comments, all of which were positive.
4. Discussion
The first report of musculoskeletal ultrasound was in 1958 when Dussik used ultrasound waves to evaluate articular and periarticular tissues [1]. Much has changed since that time with respect to the technology of ultrasound and its application to clinical medicine including rheumatologic diseases [2]. Hand-carried ultrasound machines are now available which produce high-quality digital images that rival the larger, more expensive ultrasound machines. These machines are also more user-friendly, making ultrasound easier to learn and less operator dependent. Ultrasound has been successfully introduced into medical school curricula in various courses such as gross anatomy and physiology [3–5]. Tshibwabma et al. reported a four-year experience with second-year medical students that used ultrasound to help learn musculoskeletal anatomy and physical examination skills [6]. Ultrasound education has been introduced across all four years of medical education in an integrated ultrasound curriculum [7].
In the present study of 21 fourth-year medical students, it was demonstrated that in a relatively short period of time (total time of less than one hour), all students learned the suprapatellar longitudinal scan of the knee and correctly identified all anatomical landmarks, the presence of an effusion, and the knee with the larger effusion. They performed well at this level despite the fact that just over half of them had no hands-on ultrasound experience prior to the workshop and 19 of the 21 students had no previous musculoskeletal ultrasound experience.
The knee was chosen as the focus of the workshop because it is a common site of musculoskeletal pathology, and the ability to determine if an effusion is present can be critical in diagnosing and managing patients. Ultrasound determined the location and size of an effusion which can also facilitate the aspiration of an effusion [8]. Septic arthritis and crystal-induced arthritis such as gout and pseudogout commonly involve the knee, and the early detection of a joint effusion and fluid aspiration are crucial to the diagnosis and management of these cases. Thus, learning to scan a symptomatic knee for an effusion should prove highly beneficial for these future physicians.
It should be noted that even though the study cohort of students quickly and accurately learned to identify a knee effusion by ultrasound, it is not the authors' intent to suggest that ultrasound should replace the appropriate physical examination of the knee. Ultrasound should be considered complementary to a good musculoskeletal physical examination and not a replacement for that examination. In fact, ultrasound can be a good teaching tool for the physical examination [6, 9, 10]. As Day et al. have reported, medical students presently lack confidence in their musculoskeletal physical examination skills [11]. Ultrasound may be an important tool to improve their skills and their confidence. Because cadaver specimens were used and are difficult to physically manipulate, no attempt was made to assess the students ability to identify an effusion by physical examination in this study.
In addition to ultrasound being a valuable teaching and clinical tool, virtually all studies involving medical students including this study have shown that the students enjoy the addition of the hands-on component of ultrasound to their educational experience. Introducing ultrasound into musculoskeletal education, especially in teaching rheumatology, may generate interest in the subspecialty of rheumatology early in their training. This may be important considering the predicted rheumatology workforce shortages for the next two decades [12].
Acknowledgment
GE Healthcare provided the ultrasound systems used in the study.
References
- 1.Kane D, Grassi W, Sturrock R, Balint PV. A brief history of musculoskeletal ultrasound: ’From bats and ships to babies and hips’. Rheumatology. 2004;43(7):931–933. doi: 10.1093/rheumatology/keh004. [DOI] [PubMed] [Google Scholar]
- 2.Grassi W, Filippucci E. Ultrasonography and the rheumatologist. Current Opinion in Rheumatology. 2007;19(1):55–60. doi: 10.1097/BOR.0b013e3280119648. [DOI] [PubMed] [Google Scholar]
- 3.Teichgräber UKM, Meyer JMA, Nautrup CP, Von Rautenfeld DB. Ultrasound anatomy: a practical teaching system in human gross anatomy. Medical Education. 1996;30(4):296–298. doi: 10.1111/j.1365-2923.1996.tb00832.x. [DOI] [PubMed] [Google Scholar]
- 4.Tshibwabwa ET, Groves HM. Integration of ultrasound in the education programme in anatomy. Medical Education. 2005;39(11):1143–1172. doi: 10.1111/j.1365-2929.2005.02288.x. [DOI] [PubMed] [Google Scholar]
- 5.Brunner M, Moeslinger T, Spieckermann PG. Echocardiography for teaching cardiac physiology in practical student courses. The American Journal of Physiology. 1995;268(6):S2–S9. doi: 10.1152/advances.1995.268.6.S2. [DOI] [PubMed] [Google Scholar]
- 6.Tshibwabwa ET, Groves HM, Levine MA. Teaching musculoskeletal ultrasound in the undergraduate medical curriculum. Medical Education. 2007;41(5):505–526. doi: 10.1111/j.1365-2929.2007.02745.x. [DOI] [PubMed] [Google Scholar]
- 7.Hoppmann R, Cook T, Hunt P, et al. Ultrasound in medical education: a vertical curriculum at the University of South Carolina School of Medicine. Journal of the South Carolina Medical Association. 2006;102(10):330–334. [PubMed] [Google Scholar]
- 8.Fessell DP, Jacobson JA, Craig J, et al. Using sonography to reveal and aspirate joint effusions. American Journal of Roentgenology. 2000;174(5):1353–1362. doi: 10.2214/ajr.174.5.1741353. [DOI] [PubMed] [Google Scholar]
- 9.Barloon TJ, Brown BP, Abu-Yousef MM, et al. Teaching physical examination of the adult liver with use or real-time sonography. Academic Radiology. 1998;5(2):101–103. doi: 10.1016/s1076-6332(98)80129-3. [DOI] [PubMed] [Google Scholar]
- 10.Butter J, Grant TH, Egan M, et al. Does ultrasound training boost Year 1 medical student competence and confidence when learning abdominal examination? Medical Education. 2007;41(9):843–848. doi: 10.1111/j.1365-2923.2007.02848.x. [DOI] [PubMed] [Google Scholar]
- 11.Day CS, Yeh AC, Franko O, Ramirez M, Krupat E. Musculoskeletal medicine: an assessment of the attitudes and knowledge of medical students at Harvard medical school. Academic Medicine. 2007;82(5):452–457. doi: 10.1097/ACM.0b013e31803ea860. [DOI] [PubMed] [Google Scholar]
- 12.Deal CL, Hooker R, Harrington T, et al. The United States rheumatology workforce: supply and demand, 2005–2025. Arthritis and Rheumatism. 2007;56(3):722–729. doi: 10.1002/art.22437. [DOI] [PubMed] [Google Scholar]