Abstract
Objective To prospectively examine pathways from early childhood violence exposure and trauma-related symptoms to school-age emotional health. Methods A longitudinal, birth cohort (N = 437) was assessed with parent reports of lifetime violence exposure and trauma-related symptoms at 3 years of age and later, internalizing and externalizing symptoms, and social competence at school age. Results Early family and neighborhood violence correlated significantly with early trauma-related symptoms and also significantly predicted school-age internalizing and externalizing symptoms and poorer competence, independent of sociodemographic risk and past-year violence exposure. Longitudinal pathways were significantly mediated by arousal and avoidance symptoms at 3 years of age, which increased risk for clinically significant emotional problems and lower competence at school age (adjusted odds ratios = 3.1–6.1, p < 0.01). Conclusions Trauma-related symptoms may mediate developmental pathways from early violence exposure to later emotional health. Interventions that prevent or reduce early trauma-related symptoms may ameliorate the long-term deleterious impact of violence exposure.
Keywords: longitudinal, post-traumatic stress, preschool, trauma, violence
Early childhood is now recognized to be an important period in which substrates of long-term emotional health are laid down (Shonkoff & Phillips, 2000). Basic science with animals and humans has documented that early adverse experiences may have lasting effects on organisms’ stress responses and brain structures (Crowe & Blair, 2008; De Bellis & Van Dillen, 2005; Heim & Nemeroff, 2001; Teicher, Andersen, Polcari, Anderson, & Navalta, 2002). Consonant with these basic science findings, longitudinal epidemiology studies of adolescents and adults have revealed increased risk, not only for posttraumatic stress disorder, but also for other anxiety disorders, depression, and disruptive behavior disorders among individuals exposed to serious adverse events, such as natural disasters, injuries, and violence (Copeland, Keeler, Angold, & Costello, 2007; Kessler, 2000). While data are more limited for children <5 years of age, there is increasing evidence that early childhood exposure to serious adverse experiences is associated with elevations in emotional problems, such as withdrawal and anxiety and disruptive behavior (Bogat, DeJonghe, Levendosky, Davidson, & von Eye, 2006; Briggs-Gowan, Carter, et al., 2010; English, Marshall, & Stewart, 2003; Manly, Kim, Rogosch, & Cicchetti, 2001; Mongillo, Briggs-Gowan, Ford, & Carter, 2009; cf., Scheeringa, 2009). Moreover, in very young children, a handful of studies has linked such exposures with overall posttraumatic stress symptoms (Briggs-Gowan, Carter et al., 2010) and trauma-related symptoms of hyperarousal, reexperiencing, and avoidance/numbing (Bogat et al., 2006; Scheeringa, 2009). Although epidemiologic data on trauma symptoms in young children are limited, significant cross-sectional associations between adverse events and trauma-related symptoms were recently documented in 18- to 36-month-olds in an epidemiologic birth cohort (Briggs-Gowan, Ford, et al., 2010). Evidence that the effects of adverse experiences may manifest in young children in a manner similar to that seen in older children underscores the need for prospective research into the effects of early exposures on developmentally sensitive manifestations of trauma symptoms and the role of these symptoms in developmental pathways. Yet, little is known about whether these early exposures are prospectively predictive of poorer emotional health (i.e., symptoms and poorer social functioning) over time or through what pathways early childhood exposures and later emotional health are linked.
Trauma-Related Symptoms and Developmental Pathways
Trauma-related symptoms are postulated to reflect underlying disruptions in stress response and thus heightened vulnerability for ongoing social–emotional problems (Crowe & Blair, 2008). When such symptoms emerge early in development, they may functionally impede developmental progress and impact later “emotional health” (or internalizing and externalizing symptoms and social–emotional competencies) (Lieberman, 2007; Manly et al., 2001). Early trauma-related symptoms may interfere with children's mastery of stage-salient tasks, including self-regulation, autonomy, and acquisition of age-typical prosocial skills. Consistent with the notion that trauma-related symptoms may have long-term negative sequelae, in a study of children exposed to traumatic events, preschoolers with more severe trauma symptoms were found to have greater impairment in functioning in social activities and relationships 2 years later compared with children with less severe trauma symptoms (Scheeringa, Zeanah, Myers, & Putnam, 2005). In older youth, trauma-related symptoms have been related to increased risk for psychiatric disorders (Copeland et al., 2007). Thus, it was hypothesized that early childhood trauma-related symptoms would be associated with poorer emotional health at school age and would mediate the longitudinal pathways between early exposures and later emotional health.
Family Violence and Conflict
The focus of this study is on violence exposure because it is one of the most prevalent and harmful types of adverse events experienced in childhood (Kitzmann, Gaylord, Holt, & Kenny, 2003; Knickerbocker, Heyman, Slep, Jouriles, & McDonald, 2007). An estimated 13–24% of children are exposed to interparental violence, physical child abuse, or neighborhood violence (Briggs-Gowan, Ford, Fraleigh, McCarthy, & Carter, 2010; Knickerbocker et al., 2007). A few studies have documented posttraumatic stress symptoms in young children exposed to family violence (Bogat et al., 2006; Briggs-Gowan Ford, et al., 2010; Levendosky, Huth-Bocks, Semel, & Shapiro, 2002) and emotional problems (Shahinfar, Fox, & Leavitt, 2000) and poorer social competence in preschool children exposed to neighborhood violence (Farver, Natera, & Frosch, 1999). Furthermore, although family conflict is a putatively less severe form of adverse stressor than violence, it has also been linked with emotional problems in young children (McDonald, Jouriles, Briggs-Gowan, Rosenfield, & Carter, 2007). The effects of violence may vary depending on several factors, including whether it is directly experienced versus witnessed, actual or vicarious (e.g., media violence), in the family or in the neighborhood/community, and, for older children, in a context of a delinquent peer group or not (Ferguson, San Miguel, & Hartley, 2009; Ford, Hartman, Hawke, & Chapman, 2008). Witnessing family or neighborhood violence are particularly prevalent forms of violence exposure described by caregivers of young children (Briggs-Gowan, Ford, et al., 2010).
In this study, we examine prospective patterns in the representative longitudinal birth cohort previously studied cross-sectionally. This sample was followed from early childhood to Kindergarten/First grade to test three hypotheses: (i) both family and neighborhood violence exposure between birth and age 3 years will be uniquely associated with trauma-related symptoms at age 3 years; (ii) early childhood violence exposure will uniquely predict emotional problems in early elementary school, independent of recent violence exposure and sociodemographic risk; and (iii) early childhood trauma-related symptoms will mediate the effect of early family and neighborhood violence exposure on later emotional problems and competencies.
Methods
Sample and Participant Selection
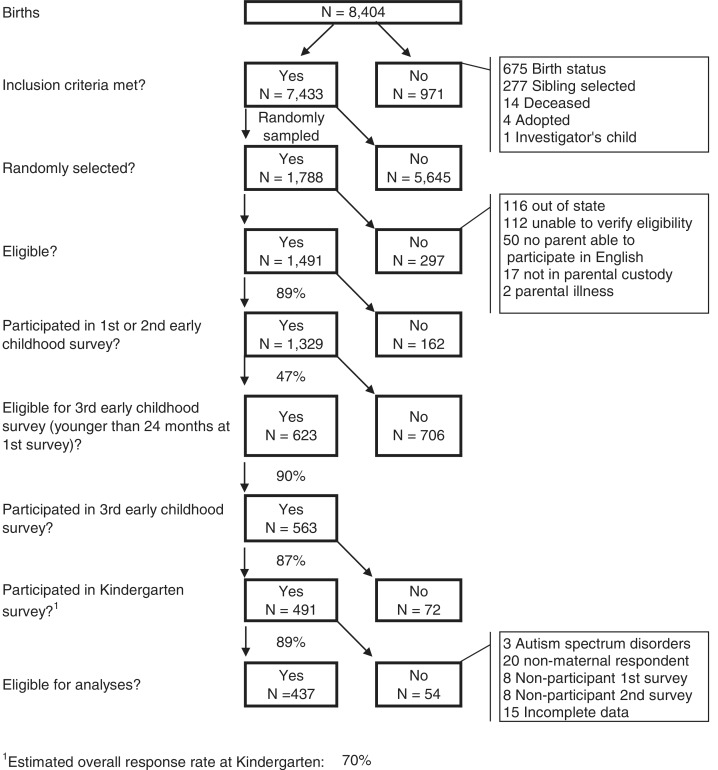
Data are from a subsample of a longitudinal representative birth cohort. Children were initially randomly selected from birth records from the State of Connecticut Department of Public Health for births at Yale-New Haven Hospital from July 1995 to September 1997 (Figure 1). This sample was stratified to have equal representation of girls and boys from 11 to 35 months of age. Eligible children were born healthy in the New Haven-Meriden Standard Metropolitan Statistical Area of the 1990 Census. Children likely to have developmental delays due to low birthweight (<2,200g), prematurity (<36 weeks), low APGAR scores (both scores below 5), or birth complications (e.g., need for resuscitation and anoxia) were excluded. A random sample of 1,788 was selected from 7,433 eligible births. After initial sampling, additional exclusions were applied (e.g., not in parental custody, unable to verify eligibility, and unable to participate in English [see Figure 1 for details]). A total of 1,329 eligible families participated in an early childhood survey (89% response rate).
Figure 1.
Sample design.
There were small but significant differences between participants and nonparticipants, with participants tending to have slightly higher maternal education (mean of 13.6 years vs. 14.1 years) and be of Caucasian ethnicity (75.3% vs. 68.3%). However, the sample was sociodemographically comparable to the Census region from which it was drawn in terms of single-parent status and race/ethnicity (Carter et al., 2010). Weights were applied in all analyses to adjust for unequal probabilities of selection and retention. These weights adjusted for the probability of selection and adjusted for differential nonresponse and attrition on the basis of background characteristics such as gestational age, birth weight, mother's and father's age, and mother's education, which were available from birth records.
This study is restricted to the younger half of this sample, because parents in this subsample completed three annual surveys in early childhood, allowing repeated assessment of lifetime exposure to violence across this period. Surveys were completed when children were approximately 1-year-olds (∼12–23 months), 2-years-old (∼24–35 months), and 3-years-old (∼36–48 months), and in Kindergarten/first grade. As shown in Figure 1, 623 parents with 1-year-olds at the time of the first survey were eligible for the third survey when children were 3-year-olds. Ninety percent (n = 563) of eligible families participated in the third survey and 87% (n = 491) participated again at school age.
Analyzed data were restricted to participants with maternal respondents in all surveys and complete data on key variables (Figure 1). Children with autism identified after original sampling were excluded. Participants in analyses (n = 437) were similar to participants from the first survey in child sex, ethnicity, parental education, single parenting, teenage motherhood, unemployment, and poverty (χ2 = .09–3.37, ns), and violence exposure and trauma-related symptoms (F = .003–2.32, ns).
The sample was sociodemographically heterogeneous (Table I). Mean child age was 39.8 months in the third survey (SD = 3.9 months) and 71.4 months (SD = 5.2 months) at school age.
Table I.
Participant Characteristics (Weighted)
| n (%) | |
|---|---|
| Boys | 218 (49.9) |
| Girls | 219 (50.1) |
| Poverty | 69 (16.1) |
| Borderline poverty | 62 (14.4) |
| Single parent home | 77 (17.6) |
| No parent in home completed high school education | 42 (9.6) |
| Race/Ethnicity | |
| Caucasian/White | 301 (68.9) |
| African American/Black | 62 (14.2) |
| Hispanic | 22 (5.0) |
| Asian | 9 (2.1) |
| Multi-ethnic minority | 38 (8.7) |
| Other | 5 (1.1) |
Procedure
Parents were invited by mail to complete surveys and received $25–$35 for each completed survey. All procedures were approved by two universities’ human subjects review boards. Informed consent was obtained.
Measures
Sociodemographic Risk
Composite sociodemographic risk was calculated as the sum of the following: minority, poverty, single parent, parent education less than high school, and teenage parenting. Baseline risk is used because there was minimal change over time (r between baseline and school age = .89).
Child Life Events Scale
In each early childhood survey, parents were asked to report about the child's exposure to each event in his/her “whole life.” Lifetime exposure by 3 years of age was calculated cumulatively (i.e., positive if reported in any early wave). At school age, past-year exposure was assessed. Three items addressed family violence/conflict: “Seen someone hit, push, or kick a family member”; “Seen someone use a weapon to threaten or hurt a family member”; and “Seen or heard adult family members arguing very loudly or fighting.” A composite variable was used (1 = any history of exposure to one or more event, 0 = never exposed). One item addressed neighborhood violence (“Seen violence in your neighborhood”). In a test–retest substudy conducted in the first year of the study, the Child Life Events Scale (CLES; Carter & Briggs-Gowan, 1998) demonstrated acceptable test–retest reliability (κ = .78) (Mongillo et al., 2009).
Infant-Toddler Social and Emotional Assessment Trauma-Related Symptoms
At 3 years of age, parents reported about posttraumatic stress symptoms on the Infant-Toddler Social and Emotional Assessment (ITSEA) Trauma-Related Symptoms (ITSEA-TRSS), a developmentally sensitive assessment of early childhood manifestations of symptoms consistent with posttraumatic stress (Mongillo et al., 2009). Sample arousal items are as follows: “Easily startled,” “Irritable or grouchy,” and “Nervous, tense, or fearful.” Sample reexperiencing items are “Acts out same pretend theme over and over,” “Wakes up from scary dreams” and “When upset, gets very still, freezes or doesn't move.” Sample avoidance items are “Avoids physical contact,” “Does not react when hurt,” and “Seems withdrawn.” In this sample, the TRSS scales have acceptable model fit, low to moderate internal consistency (α = .49–.79), good test–retest reliability (intraclass correlations = .67–.84), and have been shown to be positively associated with exposure to potentially traumatic events (Mongillo et al., 2009). Continuous and dichotomous (reflecting scores ≥80th percentile) scores were used.
Child Behavior Checklist (CBCL/6–18)
At school age, parent reports of child internalizing and externalizing symptoms were measured with the CBCL, which has established reliability and validity (Achenbach & Rescorla, 2001). Internal consistency was acceptable in this sample (αInternalizing = .85, αExternalizing = .93). Continuous and dichotomous subclinical/clinical (T ≥ 60) scores were used.
Adaptive Social Behavior Ratings Scale
School-age social competence was assessed with parent reports on a questionnaire about social problem-solving, social flexibility, affiliation, and consideration of others, comprising items from multiple developmentally appropriate measures. At school age, the Adaptive Social Behavior Ratings Scale (ASBR) demonstrated acceptable model fit, reliability, and validity (Carter et al., 2010) and the global score had excellent internal consistency (α = .95).
Analytic Plan
Primary analyses consisted of two series of multivariate linear regression models. The dependent variables for the first series (Testing hypothesis 1) were trauma-related symptoms at 3 years of age. Independent variables were child age and sex (Block 1), followed by individual steps for early family and neighborhood violence exposure variables and sociodemographic risk. Entry order enabled examination of associations between exposures and symptoms with and without sociodemographic risk controlled. In the second series (Testing hypotheses 2 and 3), the dependent variables were school-age outcomes (internalizing symptoms, externalizing symptoms, and competence). Independent variables were age, sex, early exposures, school-age exposures, early trauma symptoms, and sociodemographic risk. Entry order enabled examination of associations between exposures and symptoms before and after early trauma-related symptoms entered the model (Block 6) (allowing examination of whether trauma symptoms mediated the effects of exposure on outcomes) and before and after sociodemographic risk was controlled (Block 7). Finally, in a similar fashion, the clinical significance of longitudinal models was examined with logistic regressions predicting clinical status on the CBCL and ASBR. Bonferroni-adjusted p-values were used to reduce the likelihood of chance findings due to multiple comparisons.
Results
Lifetime exposures to family violence/conflict and neighborhood violence were common in early childhood and at school age (Table II). The two forms of exposure were related (χ2 = 16.40, p < .0001). Eighty-eight percent of children exposed to neighborhood violence also experienced family violence/conflict and 8.8% of those exposed to family violence/conflict also experienced neighborhood violence.
Table II.
Descriptive Statistics for Key Variables (n = 437)
| 3 years of age (lifetime) n (%) | Early elementary school (past year) n (%) | |
|---|---|---|
| Violence exposure | ||
| Neighborhood violence | 20 (4.6) | 8 (1.9) |
| Any family violence/conflicta | 203 (46.1) | 107 (24.4) |
| Weapon use toward family | 6 (1.3) | 1 (0.2) |
| Hit, push, kick family | 80 (18.2) | 13 (2.9) |
| Seen/heard angry adult conflict | 185 (42.1) | 106 (24.2) |
| Subclinical/clinical cut-scores | ||
| Any trauma-related scale | 92 (20.8) | Not applicable |
| CBCL internalizing | Not applicable | 39 (9.0) |
| CBCL externalizing | Not applicable | 42 (9.6) |
| Social competence low | Not applicable | 36 (8.3) |
Note. No sex differences in exposure or sociodemographic risk were present.
aDichotomous “any” family violence/conflict variable used in models.
Nearly all symptom variables were significantly intercorrelated within and across time. Early violence exposure was positively associated with trauma-related symptoms at 3 years of age and later symptoms and competencies (Table III).
Table III.
Pearson and Point-Biserial Correlations Between Violence Exposure and Symptoms (n = 437)
| Trauma-related symptoms (3 years) |
Emotional health (school-age) |
||||||
|---|---|---|---|---|---|---|---|
| Arousal | Avoidance | Reexperiencing | Internalizing | Externalizing | Competence | MN (SD) | |
| Sociodemographic risk | .32* | .27* | .29* | .25* | .21* | −.23* | 1.01 (1.54) |
| Arousal (3 years) | – | .42* | .45* | .52* | .52* | −.40* | 0.45 (0.26) |
| Avoidance (3 years) | – | – | .35* | .40* | .33* | −.37* | 0.12 (0.17) |
| Re-experiencing (3 years) | – | – | – | .36* | .22* | −.15 | 0.39 (0.26) |
| Internalizing (school age) | .64* | −.36* | 3.61 (4.10) | ||||
| Externalizing (school age) | −.51* | 4.78 (5.23) | |||||
| Competence (school age) | 3.08 (0.50) | ||||||
| Lifetime exposure (3 years) | |||||||
| Family violence/conflict | .25* | .14* | .08 | .20* | .25* | −.19* | – |
| Neighborhood violence | .24* | .26* | .19* | .25* | .18* | −.20* | – |
| Past year exposure (school age) | |||||||
| Family violence/conflict | .10 | .02 | .04 | .15 | .16 | −.04 | – |
| Neighborhood violence | .21* | .10 | .18* | .24* | .14 | −.09 | – |
*p < .0012 (Bonferroni correction for α = .05).
Multivariate Models for Early Trauma-Related Symptoms
Family violence/conflict and neighborhood violence exposure by 3 years of age were significantly associated with arousal and avoidance, but only neighborhood violence was associated with re-experiencing (Table IV). When sociodemographic risk was added to the models, arousal was still associated with both types of exposure (partial Rfamily violence/conflict = .037; partial R2neigbhorhood violence = .017) and avoidance was associated with neighborhood violence (partial R2 = .061). Thus, these forms of exposure explained unique variance in arousal and avoidance symptoms independent of socioeconomic adversity.
Table IV.
Models Examining Associations Between Violence Exposure and Trauma-Related Symptoms Within Early Childhood (Linear Regression)
| Values at entry block |
Final model | |||||
|---|---|---|---|---|---|---|
| Block | Standardized beta (SE) | t-value | Adj. R2 | ΔR2 | t-value | |
| Model 1A: Arousal | ||||||
| 1 | Child sex | .00 (0.02) | 0.09 | −0.08 | ||
| Child age | .04 (0.00) | 0.85 | −.003 | .000 | 0.52 | |
| 2 | Family violence/conflict | .25 (0.02) | 5.39** | .058 | .061 | 3.91** |
| 3 | Neighborhood violence | .21 (0.06) | 4.43** | .097 | .039 | 2.95* |
| 4 | Sociodemographic risk | .14 (0.01) | 5.25** | .149 | .052 | 5.25** |
| Model 1B: Avoidance | ||||||
| 1 | Child sex | .06 (0.02) | 1.18 | 1.29 | ||
| Child age | .06 (0.00) | 1.19 | .003 | 1.21 | ||
| 2 | Family violence/conflict | .13 (0.02) | 2.74* | .017 | .015 | 1.20 |
| 3 | Neighborhood violence | .25 (0.04) | 5.38** | .077 | .059 | 4.16** |
| 4 | Sociodemographic risk | .19 (0.01) | 4.01** | .108 | .031 | 4.01** |
| Model 1C: Re-experiencing | ||||||
| 1 | Child sex | −.14 (0.02) | −3.05 | −3.35* | ||
| Child age | .10 (0.00) | 2.14 | .024 | 2.23 | ||
| 2 | Family violence/conflict | .07 (0.02) | 1.47 | .027 | .003 | −0.02 |
| 3 | Neighborhood violence | .18 (0.06) | 3.83** | .057 | .029 | 2.33 |
| 4 | Sociodemographic risk | .26 (0.01) | 5.47** | .116 | .059 | 5.52** |
*p < .0083 (Bonferroni correction for α = .05), ** p < .0001.
Multivariate Models Predicting School-Age Symptoms
Violence exposure that occurred in early childhood significantly predicted school-age internalizing and externalizing symptoms (Table V). Specifically, family and neighborhood violence accounted for small to moderate amounts of variance in internalizing and externalizing symptoms (ΔR2 = .024–.054). Consistent with mediation, these effects were not significant after early trauma-related symptoms entered the models in Block 6. Notably, in the final models, arousal at 3 years of age explained substantial variance in school-age internalizing (partial R2 = .11) and externalizing symptoms (partial R2 = .15). Avoidance symptoms also explained unique variance in later internalizing symptoms (partial R2 = .03). These effects were independent of sociodemographic risk and past-year violence exposure. Sociodemographic risk was not predictive of school-age symptoms independent of trauma-related symptoms, despite the bivariate associations observed.
Table V.
Prediction of School-Age Emotional Health from Early Violence Exposure and Trauma-Related Symptoms
| Values at entry block |
Block 6 | Final model | ||||
|---|---|---|---|---|---|---|
| Block | Standardized beta (SE) | Adjusted R2 | ΔR2 change | t-value | t-value | |
| Dependent variable: Internalizing | ||||||
| 1 | Sex | −.08 (0.39) | −1.74 | −1.81 | ||
| Age | .08 (0.05) | 1.19 | 1.19 | |||
| Block | .008 | NA | ||||
| 2 | Family violence/conflict (3 years) | .20 (0.39)*** | .045 | .037 | 0.99 | 0.87 |
| 3 | Neighborhood violence (3 years) | .22 (0.91)*** | .090 | .046 | 1.12 | 0.97 |
| 4 | Family violence/conflict (past year) | .07 (0.46) | .092 | .002 | 1.18 | 1.26 |
| 5 | Neighborhood violence (past year) | .15 (1.47)** | .110 | .018 | 2.24* | 2.20* |
| 6 | Arousal (3 years) | .35 (0.76)*** | 7.30*** | 7.12*** | ||
| Avoidance (3 years) | .19 (1.11)*** | 4.31*** | 4.23*** | |||
| Re-experiencing (3 years) | .09 (0.71) | 1.87 | 1.73 | |||
| Block | .334 | .224 | ||||
| 7 | Sociodemographic risk | .04 (0.12) | .334 | .000 | NA | 0.81 |
| Dependent variable: Externalizing | ||||||
| 1 | Sex | .18 (0.49)** | 4.44** | 4.41** | ||
| Age | .07 (0.06) | 0.76 | 0.76 | |||
| Block | .035 | NA | ||||
| 2 | Family violence/conflict (3 years) | .24 (0.48)** | .089 | .054 | 1.71 | 1.69 |
| 3 | Neighborhood violence (3 years) | .16 (1.15)** | .113 | .024 | 1.07 | 1.04 |
| 4 | Family violence/conflict (past year) | .10 (0.58) | .121 | .007 | 2.08 | 2.07 |
| 5 | Neighborhood violence (past year) | .10 (1.86) | .123 | .002 | 0.35 | 0.35 |
| 6 | Arousal (3 years) | .47 (0.97)** | 9.03** | 8.93** | ||
| Avoidance (3 years) | .11 (1.43) | 2.45 | 2.43 | |||
| Re-experiencing (3 years) | −.01 (0.91) | −0.23 | −0.24 | |||
| Block | .326 | .203 | ||||
| 7 | Sociodemographic risk | .00 (0.15) | .324 | .000 | NA | 0.08 |
| Dependent variable: Competence Independent variables | ||||||
| 1 | Sex | −.19 (0.05)** | −4.04** | −3.92** | ||
| Age | −.14 (0.01)* | −2.95 | −2.96 | |||
| Block | .058 | NA | ||||
| 2 | Family violence/conflict (3 years) | −.18 (0.05)** | .088 | .030 | −1.41 | −1.25 |
| 3 | Neighborhood violence (3 years) | −.20 (0.11)** | .123 | .035 | −2.23 | −2.00 |
| 4 | Family violence/conflict (past year) | −.00 (0.06) | .121 | −.002 | 0.16 | 0.03 |
| 5 | Neighborhood violence (past year) | −.01 (0.18) | .119 | −.002 | 0.50 | 0.55 |
| 6 | Arousal (3 years) | −.30 (0.10)** | −5.89** | −5.70** | ||
| Avoidance (3 years) | −.22 (0.14)** | −4.65** | −4.54** | |||
| Re-Experiencing (3 years) | .06 (0.09) | 1.31 | 1.46 | |||
| Block | .265 | .146 | ||||
| 7 | Sociodemographic risk | −.05 (0.02) | .265 | .001 | −1.13 | |
p < .0028 (Bonferroni correction for α = .05); **p < .0001
Similarly, early family and neighborhood violence, but not past-year exposure, significantly predicted lower school-age competence. These associations were nonsignificant when early trauma symptoms were in the model. In the final model, early arousal and avoidance symptoms significantly predicted poorer school-age competence, with effects in the small to moderate range (partial R2 = .09 and .04, respectively).
Statistical tests for mediation indicated that the relationships between early family violence and later internalizing and externalizing symptoms and competence were mediated by early childhood arousal and avoidance (Sobel = 1.39–4.93, ps < .05–.0001) but not reexperiencing (Sobel = 0.09–1.35, ns). The relationship between early neighborhood violence and later internalizing symptoms was partially mediated by arousal and avoidance (Sobel = 4.69–4.82, ps < .01).
Longitudinal Models Predicting Clinical Status
In logistic regression models, high levels of trauma-related symptoms at 3 years of age (i.e., any ITSEA-TRSS score above the cut point) independently predicted CBCL externalizing, adjusted odds ratio (AOR) = 6.5, 95% CI (3.0, 13.8), p < .0001, and internalizing subclinical/clinical cut points, AOR = 6.8, CI (3.1, 14.8), p < .0001, with large effects. These effects were independent of early violence and sociodemographic risk, which did not significantly predict later symptoms in the final model, χ2 = .05–2.67, ns. Trauma-related symptoms also were prospectively associated with poorer competence, AOR = 3.1, CI (1.4, 6.5), p < 0.01, independent of sociodemographic risk and violence.
Discussion
As hypothesized, exposure to neighborhood violence and family violence/conflict reported by parents in early childhood were associated with more severe parent-reported trauma-related symptoms at 3 years of age and were prospectively associated with poorer emotional health (greater symptoms, lower competence) in elementary school. These patterns were independent of strong associations between sociodemographic risk and symptoms, suggesting a traumatic impact distinguishable from socioeconomic adversity. Such associations in this representative healthy birth cohort extend findings previously identified in studies that focused the effects of violence on clinically referred children or those known to have experienced domestic violence (Bogat et al., 2006; Briggs-Gowan, Carter et al., 2010) to a more normative sample.
Notably, trauma-related symptoms at 3 years of age appeared to partially or fully mediate the pathways from early exposure to later emotional health, consistent with the idea that early trauma symptoms may impede developmental progress (Crowe & Blair, 2008). Specifically, young children who manifested avoidance and arousal symptoms were at heightened risk for later internalizing symptoms and poorer social competence and those with early arousal were at heightened risk for later externalizing symptoms. The association between early violence and later emotional health was mediated by early trauma symptoms; exposure was not significantly associated with later emotional health once trauma-related symptoms entered these models. Thus, early life exposures do not impact all children similarly. Rather, they appear to have specific and unique effects on children's subsequent emotional and behavioral health and early trauma-related symptoms may play a mediational role in these developmental pathways. Careful inquiry is needed to elucidate the manner through which trauma-related symptoms may influence these early pathways.
The clinical significance of this prospective pattern is underscored by the finding that children with high levels of early trauma-related symptoms (>80th percentile) experienced a nearly 7-fold increase in risk for later subclinical/clinical levels of internalizing and externalizing symptoms. Thus, in keeping with evidence that PTSD symptoms predict heightened risk of psychosocial morbidity in adolescents and adults (Breslau, 2001; Giaconia et al., 1994), the emergence of PTSD symptoms by 3 years appears to place children at-risk for later impairment. More broadly, these prospective findings suggest that the psychosocial morbidity observed in adolescents and adults who retrospectively reported adverse childhood experiences (Anda et al., 2006; Copeland et al., 2007) may begin in the form of potentially preventable traumatic stress symptoms early in childhood.
In this community sample, consistent with other studies, witnessing family conflict/violence was common, witnessing neighborhood violence was relatively rare, and different forms of exposure often overlapped (cf., Fairbank, Putnam, & Harris, 2007; Mechanic & Hansell, 1989; Menard, Bandeen-Roche, & Chilcoat, 2004). Notably, many more children had witnessed violence than were reported to have lasting problems, highlighting the need to investigate factors that may mediate or moderate pathways, including—but certainly not limited to—genetic vulnerability (e.g., Kim-Cohen et al., 2006), relational factors (Foster & Brooks-Gunn, 2009), individual differences in biologically based stress reactivity (cf., De Bellis & Van Dillen, 2005), and changes in affective information processing (Pollak, 2008).
Given theoretical and empirical evidence that more proximal processes often exert stronger effects (Tolan, Gorman-Smith, & Henry, 2003), the finding that neighborhood violence exposure appeared to have a more robust relationship than family violence/conflict with avoidance at 3 years of age and (when occurring in the past year) with school-age internalizing symptoms was unexpected. This finding has several potential explanations. As assessed in this study, neighborhood violence was more severe and rarer than family conflict/violence, thus possibly having a stronger, more observable traumatic impact. Neighborhood violence also may reflect more pervasive socio-environmental adversity than family conflict/violence (Foster & Brooks-Gunn, 2009), but sociodemographic risk was controlled, thus this explanation is less likely. Finally, neighborhood violence rarely occurred in the absence of family conflict/violence, thus it may be a proxy for sociodemographic adversity or poly-victimization (Finkelhor, Ormrod, & Turner, 2007). Children who witness violence in both the neighborhood and the home may be at risk for impaired development and adverse outcomes because they have no safe base from which to optimize their adaptive capacities (Bronfenbrenner & Ceci, 1994).
Finally, the absence of any unique relationship between violence exposure and intrusive reexperiencing symptoms at age 3 or between reexperiencing and subsequent emotional problems, raises several questions. In adolescence and adulthood, individuals who recall having been exposed to violence in childhood tend to report intrusive reexperiencing symptoms, as well as avoidance and arousal symptoms (Anda et al., 2006; Copeland et al., 2007). Parents of young children may be less able to recognize reexperiencing symptoms than other trauma-related symptoms. It may also be that intrusive reexperiencing symptoms emerge with the development of more elaborate information processing capacities later in childhood (Pine, 2007).
Limitations
This study had several limitations. First, only lifetime violence exposure was assessed in early childhood. Thus, the influence of other aspects of violence exposure on pathways could not be examined. Assessment of violence exposure in a manner that articulates not only different contexts (family and neighborhood) but also different forms (physical, verbal, and psychological) and variations in severity, chronicity, and perpetrator relationship would strengthen future work. Indeed, while many studies have focused on extreme forms of violence exposure, particularly child abuse, the current findings and others (Kitzmann et al., 2003) reveal the need to elucidate the effects of a spectrum of violence exposure, including putatively less severe forms such as family conflict. Second, this study relied on maternal reports of exposure, symptoms, and social competencies. Some mothers may have denied that their children had witnessed violence, due to concerns about adverse consequences of disclosure (e.g., triggering investigation). Thus, although the four repeated assessments of exposure across the study waves should have helped to optimize detection of exposure, underreporting may have occurred. Similarly, mothers’ own histories of violence or other traumas may have influenced their reports, making them more (or perhaps less) attuned to the presence of trauma-related symptoms in their young children. The current study should be extended by a multimethod, multi-informant design, as well as more thorough assessment of children's posttraumatic stress symptoms (e.g., via diagnostic interview). Third, the effects of being the victim of violence (e.g., physical abuse; assaults in the neighborhood or school in the context of bullying or crimes) also require study. Furthermore, media violence has not been found to be associated with behavior problems in older children (Ferguson et al., 2009), but its effects in the developmentally sensitive period of early childhood warrant examination. Finally, important family processes known to influence outcomes in young children, such as parental psychological functioning (affective symptoms, alcohol or substance use, trauma history) and the quality of the parent–child relationship (Scheeringa, 2009) were not examined.
Implications for Practice
Based on these findings, clinicians working with elementary school-age children with internalizing or externalizing symptoms who have impaired social and academic competence should take into account the possible contribution of traumatic stress reactions in assessment and treatment planning. Children exposed to violence may develop PTSD symptoms as toddlers that are not identified as such because the child's trauma history was not ascertained systematically or the symptoms were presumed to be due to other anxiety or affective disorders (Scheeringa et al., 2005). Several years later, these children's symptoms may appear unrelated to trauma due to an absence of recent traumatic exposure. However, left untreated, the earlier traumatic stress symptoms may lead to, or exacerbate, emotional and behavioral problems that become evident later in childhood as internalizing or externalizing symptoms and problems in school and relationships (Fairbank et al., 2007). Interventions that prevent or reduce early trauma-related symptoms may not only enhance early life development and functioning but also ameliorate the long-term deleterious impact of violence exposure (Fairbank et al., 2007; Lieberman, 2007).
Although exposure to family violence in infancy and toddlerhood has been found to be associated with psychosocial symptoms and impairment (Kitzman et al., 2003; Levendosky et al., 2002; McDonald et al., 2007), and has been a focus of important developments in therapeutic practice and research (Lieberman, 2007), the present study's findings also suggest that exposure to neighborhood violence in early childhood also warrants attention clinically and scientifically. Living in a violent community may have not only an immediate deleterious impact on young children (Scheeringa, 2009), but may place children who develop traumatic stress symptoms at risk for continued or worsened internalizing and externalizing problems that can compromise their competence many years later in the school years. Children living in violent neighborhoods also are at risk for exposure to family violence and may require treatment addressing the often complex sequelae of poly-victimization (Finkelhor et al., 2005).
Research is needed to clarify how alterations in biological (De Bellis & Van Dillen, 2005; Heim & Nemeroff, 2001; Teicher et al., 2002) and psychological (Pine, 2007; Pollak, 2008) functioning and development associated with violence exposure in early childhood either persist or lead to additional adverse sequelae years later in school age children. Findings from this study and other investigations with trauma-exposed infants and toddlers (Scheeringa, 2009) show that exposure to traumatic stressors increases risk but alone is not sufficient to cause immediate or lasting symptoms or impairment. Establishing biological and psychological markers of risk and resilience and identifying and mapping the longitudinal trajectories of young children exposed to violence, represents a crucial scientific and public health challenge.
Conclusions
Findings in the present study suggest that exposure to violence in early childhood may have lasting effects on children's emotional health and that early trauma-related symptoms may mediate longitudinal pathways. Evidence of lasting problems associated with early childhood exposure underscores the potential need for primary prevention of violence, not only in the family but also, in the neighborhood. Finding that violence exposure alone did not put young children at risk for school-age psychosocial problems, but that children with more severe posttraumatic arousal and avoidance symptoms in the first 3 years of life were at risk, highlights the need for secondary or tertiary prevention programs in order to disrupt maladaptive longitudinal pathways and ameliorate the lasting effects of early childhood violence exposure in the children who are most affected. These findings also contribute to a growing foundation for translational investigation of mechanisms by which early life stressor exposures may affect emotional health over the lifespan.
Funding
The original study was funded by the National Institute of Mental Health (R01MH55278 to A. S. C.). Additional funding from the National Institute of Mental Health partially supported the writing of this manuscript (R01MH090301, PI M. J. B.-G.).
Conflicts of interest: None declared.
Acknowledgments
We thank study participants for making this study possible, and express our gratitude to Lauren Wakschlag, Phd, of Northwestern University for insightful comments about this article.
References
- Achenbach T M, Rescorla L A. Manual for the ASEBA School-Age Forms & Profiles: Child Behavior Checklist. Burlington, VT: University of Vermont, Research Center of Children, Youth, & Families; 2001. [Google Scholar]
- Anda R F, Felitti V J, Bremner J D, Walker J D, Whitfield C, Perry B D. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience. 2006;256:174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogat G A, DeJonghe E, Levendosky A A, Davidson W S, von Eye A. Trauma symptoms among infants exposed to intimate partner violence. Child Abuse and Neglect. 2006;30:109–125. doi: 10.1016/j.chiabu.2005.09.002. [DOI] [PubMed] [Google Scholar]
- Breslau N. Outcomes of posttraumatic stress disorder. Journal of Clinical Psychiatry. 2001;62:55–59. [PubMed] [Google Scholar]
- Briggs-Gowan M J, Carter A S, Clark R, Augustyn M, McCarthy K J, Ford J D. Exposure to potentially traumatic events in early childhood: Differential links to emergent psychopathology. Journal of Child Psychology and Psychiatry. 2010;51:1132–1140. doi: 10.1111/j.1469-7610.2010.02256.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan M J, Ford J D, Fraleigh L, McCarthy K, Carter A S. Prevalence of exposure to potentially traumatic events in a healthy birth cohort of very young children in the northeastern United States. Journal of Traumatic Stress. 2010;23:725–733. doi: 10.1002/jts.20593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U, Ceci S J. Nature-nurture reconceptualized in developmental perspective: A bioecological model. Psychological Review. 1994;101:568–586. doi: 10.1037/0033-295x.101.4.568. [DOI] [PubMed] [Google Scholar]
- Carter A S, Briggs-Gowan M J. Child Life Events Screener. New Haven, CT: Yale University; 1998. [Google Scholar]
- Carter A S, Wagmiller R J, Gray S A, McCarthy K J, Horwitz S M, Briggs-Gowan M J. Prevalence of DSM-IV disorder in a representative, healthy birth cohort at school entry: Sociodemographic risks and social adaptation. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:686–698. doi: 10.1016/j.jaac.2010.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland W E, Keeler G, Angold A, Costello E J. Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry. 2007;64:577–584. doi: 10.1001/archpsyc.64.5.577. [DOI] [PubMed] [Google Scholar]
- Crowe S L, Blair R J. The development of antisocial behavior: What can we learn from functional neuroimaging studies? Developmental Psychopathology. 2008;20:1145–1159. doi: 10.1017/S0954579408000540. [DOI] [PubMed] [Google Scholar]
- De Bellis M D, Van Dillen T. Childhood post-traumatic stress disorder: An overview. Child and Adolescent Psychiatric Clinics of North America. 2005;14:745–772. doi: 10.1016/j.chc.2005.05.006. [DOI] [PubMed] [Google Scholar]
- English D J, Marshall D B, Stewart A J. Effects of family violence on child behavior and health during early childhood. Journal of Family Violence. 2003;18:43–57. [Google Scholar]
- Fairbank J A, Putnam F W, Harris W W. The prevalence and impact of child traumatic stress. In: Friedman M J, Keane T M, Resick P A, editors. Handbook of PTSD. New York, NY: Guilford Press; 2007. pp. 229–251. [Google Scholar]
- Farver J A, Natera L X, Frosch D L. Effects of community violence on inner-city preschoolers and their families. Journal of Applied Developmental Psychology. 1999;20:143–158. [Google Scholar]
- Ferguson C J, San Miguel C, Hartley R D. A multivariate analysis of youth violence and aggression: The influence of family, peers, depression, and media violence. Journal of Pediatrics. 2009;155:904–908. doi: 10.1016/j.jpeds.2009.06.021. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Ormrod R K, Turner H A. Poly-victimization: A neglected component in child victimization. Child Abuse and Neglect. 2007;31:7–26. doi: 10.1016/j.chiabu.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Ford J D, Hartman J K, Hawke J, Chapman J C. Traumatic victimization posttraumatic stress disorder, suicidal ideation, and substance abuse risk among juvenile justice-involved youths. Journal of Child and Adolescent Trauma. 2008;1:75–92. [Google Scholar]
- Foster H, Brooks-Gunn J. Toward a stress process model of children's exposure to physical family and community violence. Clinical Child and Family Psychological Review. 2009;12:71–94. doi: 10.1007/s10567-009-0049-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giaconia R M, Reinherz H Z, Silverman A B, Pakiz B, Frost A K, Cohen E. Ages of onset of psychiatric disorders in a community population of older adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;35:706–717. doi: 10.1097/00004583-199406000-00012. [DOI] [PubMed] [Google Scholar]
- Heim C, Nemeroff C B. The role of childhood trauma in the neurobiology of mood and anxiety disorders: Preclinical and clinical studies. Biological Psychiatry. 2001;49:1023–1039. doi: 10.1016/s0006-3223(01)01157-x. [DOI] [PubMed] [Google Scholar]
- Kessler R C. Posttraumatic stress disorder: The burden to the individual and to society. Journal of Clinical Psychiatry. 2000;61(Suppl. 5):4–12. discussion 13–14. [PubMed] [Google Scholar]
- Kim-Cohen J, Caspi A, Taylor A, Williams B, Newcombe R, Craig I W. MAOA, maltreatment, and gene-environment interaction predicting children's mental health: New evidence and a meta-analysis. Molecular Psychiatry. 2006;11:903–913. doi: 10.1038/sj.mp.4001851. [DOI] [PubMed] [Google Scholar]
- Kitzmann K M, Gaylord N K, Holt A R, Kenny E D. Child witnesses to domestic violence: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2003;71:339–352. doi: 10.1037/0022-006x.71.2.339. [DOI] [PubMed] [Google Scholar]
- Knickerbocker L, Heyman R E, Slep A M, Jouriles E N, McDonald R. Co-occurrence of child and partner maltreatment: Definitions, prevalence, theory, and implications for assessment. European Psychologist. 2007;12:36–44. [Google Scholar]
- Levendosky A A, Huth-Bocks A C, Semel M A, Shapiro D L. Trauma symptoms in preschool-age children exposed to domestic violence. Journal of Interpersonal Violence. 2002;17:150–164. [Google Scholar]
- Lieberman A F. Ghosts and angels: Intergenerational patterns in the transmission and treatment of the traumatic sequelae of domestic violence. Infant Mental Health Journal. 2007;28:422–439. doi: 10.1002/imhj.20145. [DOI] [PubMed] [Google Scholar]
- Manly J T, Kim J E, Rogosch F A, Cicchetti D. Dimensions of child maltreatment and children's adjustment: Contributions of developmental timing and subtype. Developmental Psychopathology. 2001;13:759–782. [PubMed] [Google Scholar]
- Margolin G, Vickerman K A, Ramos M C, Serrano S D, Gordis E B, Iturralde E. Youth exposed to violence: Stability, co-occurrence, and context. Clinical Child and Family Psychological Review. 2009;12:39–54. doi: 10.1007/s10567-009-0040-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald R, Jouriles E N, Briggs-Gowan M J, Rosenfield D, Carter A S. Violence toward a family member, angry adult conflict, and child adjustment difficulties: Relations in families with 1- to 3-year-old children. Journal of Family Psychology. 2007;21:176–184. doi: 10.1037/0893-3200.21.2.176. [DOI] [PubMed] [Google Scholar]
- Mechanic D, Hansell S. Divorce, family conflict, and adolescents' well-being. Journal of Health and Social Behavior. 1989;30:105–116. [PubMed] [Google Scholar]
- Menard C B, Bandeen-Roche K J, Chilcoat H D. Epidemiology of multiple childhood traumatic events: Child abuse, parental psychopathology, and other family-level stressors. Social Psychiatry and Psychiatric Epidemiology. 2004;39:857–865. doi: 10.1007/s00127-004-0868-8. [DOI] [PubMed] [Google Scholar]
- Mongillo E A, Briggs-Gowan M, Ford J D, Carter A S. Impact of traumatic life events in a community sample of toddlers. Journal of Abnormal Child Psychology. 2009;37:455–468. doi: 10.1007/s10802-008-9283-z. [DOI] [PubMed] [Google Scholar]
- Pine D S. Research review: A neuroscience framework for pediatric anxiety disorders. Journal of Child Psychology and Psychiatry. 2007;48:631–648. doi: 10.1111/j.1469-7610.2007.01751.x. [DOI] [PubMed] [Google Scholar]
- Pollak S. Mechanisms linking early experience and the emergence of emotions. Current Directions in Psychological Science. 2008;17:370–375. doi: 10.1111/j.1467-8721.2008.00608.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheeringa M S. Posttraumatic stress disorder. In: Zeanah C H, editor. Handbook of Infant Mental Health. 3rd. New York: Guilford Press; 2009. pp. 345–361. [Google Scholar]
- Scheeringa M S, Zeanah C H, Myers L, Putnam F W. Predictive validity in a prospective follow-up of PTSD in preschool children. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:899–906. doi: 10.1097/01.chi.0000169013.81536.71. [DOI] [PubMed] [Google Scholar]
- Shahinfar A, Fox N A, Leavitt L A. Preschool children's exposure to violence: Relation of behavior problems to parent and child reports. American Journal of Orthopsychiatry. 2000;70:115–125. doi: 10.1037/h0087690. [DOI] [PubMed] [Google Scholar]
- Shonkoff J, Phillips D. From Neurons to Neighborhoods: The Science of Early Childhood Development. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- Teicher M H, Andersen S L, Polcari A, Anderson C M, Navalta C P. Developmental neurobiology of childhood stress and trauma. Psychiatric Clinics of North America. 2002;25:397–426, vii–viii. doi: 10.1016/s0193-953x(01)00003-x. [DOI] [PubMed] [Google Scholar]
- Tolan P H, Gorman-Smith D, Henry D B. The developmental ecology of urban males’ youth violence. Developmental Psychology. 2003;39:274–291. doi: 10.1037//0012-1649.39.2.274. [DOI] [PubMed] [Google Scholar]