Abstract
PRO
The similarity of reproductive and metabolic phenotype between prenatally androgenized sheep, or monkeys, and women with PCOS provides strong supportive evidence for developmental programming being important in the etiology of PCOS.
CON
While one would not exclude altogether developmental determinants of PCOS, it is difficult to view PCOS as purely developmental or resulting only from intrauterine exposures or simply an adaptation gone astray.
Keywords: Polycystic ovary syndrome, developmental origins
Introduction and Framework
The following articles are the distillation of two necessarily opposing views about the etiology of PCOS, the most common and enigmatic endocrine disorder in women. The pros and cons of the proposition that PCOS has developmental origins are laid out based on the best available evidence. There are no certainties about the origin of PCOS, so a degree of controversy and disagreement is bound to exist. The debating format is a surprisingly constructive means of getting to the heart of a controversial issue. We start with seemingly polarized views, yet what is apparent from these postulates is the rather large area of common ground that these views share.
We share the view that PCOS is not necessarily a disease but rather it is a cluster of features that may predispose to a disease, such as anovulatory infertility and type 2 diabetes mellitus. The precise criteria for characterizing a disease or disorder as having developmental origins are explored by Dr. Berga and the important role of the intrauterine environment is discussed. We agree that the notion of fetal programming of adult disease implies epigenetic changes and it is interesting to consider whether such changes arise, as is classically described, due to the intrauterine environment or whether they may be induced by an endogenous fetal ovarian (or adrenal) source of androgen which affects gene expression during both prenatal and postnatal development. Indeed, epigenetic plasticity presages a mechanism mediating the impact of seemingly innocuous behaviors such as dietary interactions and social interactions. We agree that, whether or not epigenetic phenomena are involved, there is strong evidence for an important genetic influence on PCOS, that is, a gene X environment interaction. There are many ways to approach the question of development and natural history of PCOS. Dr. Berga introduces the intriguing concept of a very plastic set of adaptive mechanisms to endogenous and environmental stressors that may function not only during fetal life but also into childhood and beyond. And we should not forget about the brain. Dysfunction of the hypothalamic-pituitary axis is well recognized in PCOS and whether or not it is a primary etiological factor, it plays a part in the evolution of the syndrome.
Pro – Yes, PCOS Has Developmental Origins
Stephen Franks MD FMedSci
Polycystic ovary syndrome has developmental origins
Polycystic ovary syndrome (PCOS) remains an enigmatic disorder whose etiology is still unclear. In this debate, I propose that genetic factors have an important part to play and that the disorder has its origins in early, possibly prenatal, life. The hypothesis is that polycystic ovary syndrome is a genetically determined, primary ovarian disorder resulting in excess androgen production. We suggest that the capacity to hypersecrete androgens begins in fetal life and that the typical clinical and biochemical features of PCOS are “downstream” effects of exposure to androgen excess at or before puberty. The phenotype may be influenced by other genes and by environment 1.
Evidence for the genetic basis of PCOS
The evidence that PCOS is strongly dependent on genetic factors is very strong. Familial clustering of cases has been described in many studies 2–6. The most important supporting facts are that there is clear evidence of heritability of endocrine and metabolic features 7–9 and that the concordance of symptoms of PCOS is much greater in identical than in non-identical twin pairs (tetrachoric correlation 0.71 vs 0.38; estimated genetic influence 79%, environment 21%) 10. The mode of inheritance is unclear, but given the clinical and biochemical heterogeneity of the syndrome, it seems unlikely that PCOS represents a single gene defect. It is a complex endocrine disorder and is more likely to be polygenic or oligogenic 11. Attempts to identify causative loci using a candidate gene approach have been largely disappointing 11, 12; but recent data indicate that genome-wide association studies may uncover key contributory polymorphisms that have not yet been found amongst the list of nearly 100 candidate genes studied to date 13.
Prenatal exposure to excess androgen results in a PCOS phenotype
There is now very firm evidence from animal studies that exposure to excess androgen during key developmental windows results, in adult life, in pathophysiological changes that closely resemble the features of PCOS in women. Thus, Rhesus monkeys and sheep, exposed to high concentrations of androgens during fetal life, as adults show hypersecretion of LH with abnormal LH pulsatility, ovarian hyperandrogenism and metabolic abnormalities including insulin resistance and hepatic dysfunction. The animals are frequently anovulatory (especially if they also have increased body weight) 14–16. Rodent models of PCOS have also proved useful although in this case it is exposure to high levels of androgen in postnatal life, typically around the time of puberty, that is associated with metabolic abnormalities 17, 18. The reproductive consequences of androgen excess are less consistent in rodents than in sheep or primates which very probably reflects differences in the timing and characteristics of ovarian follicle development.
There are important similarities between the prenatally androgenised sheep and women with PCOS in early follicle development in the ovary. PCOS is characterised by an increase in the proportion of preantral follicles in the ovarian cortex that have initiated growth (ie have been recruited from the primordial pool) 19, 20 and this is reflected in the findings of studies of ovaries taken from adult ewes who had been exposed prenatally to excess androgen 21. Taken together, these data strongly support the concept that prenatal exposure to high levels of androgen result in programming of reproductive and metabolic function in the adult. These data from animal experiments are robust but how does that translate to human PCOS?
A model for the developmental origin of PCOS in women
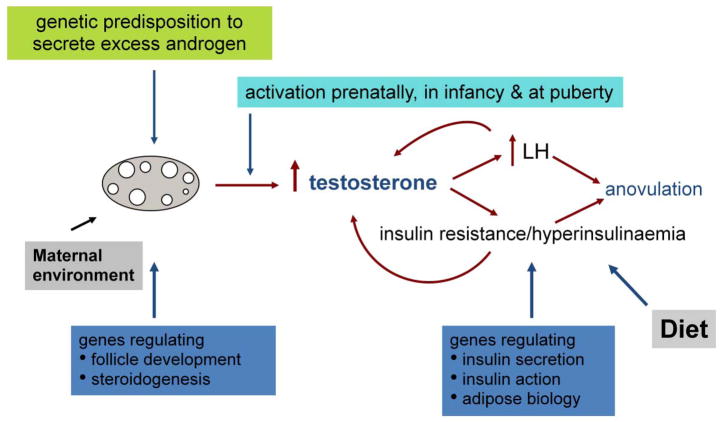
The data from primate and sheep models highlight the importance of the effects of exposure to androgen on the genesis of PCOS-like features in the adult, but the key questions in the context of PCOS in women are (1) what is the source of excess androgen and (2) at what stage of development is it likely to exert its effects? It is very unlikely that maternal androgen excess has a significant impact on fetal testosterone levels because of the efficient “buffering” firstly, by high circulating concentrations of sex hormone binding globulin (SHBG reducing the biologically available fraction of testosterone) and secondly, by the activity of placental aromatase which converts androgen to estrogen. A more plausible source of excess androgen is the fetal ovary (and/or the fetal adrenal). We suggest that the fetal ovary in PCOS is genetically predisposed to secrete higher than normal levels of androgen (Figure 1) and that androgen excess could be manifest, and exert its effects, at one or more susceptible stages during development. These stages include fetal life, early infancy (when there is transient activation of the hypothalamic-pituitary-gonadal axis), or at the onset of puberty. Androgen excess during these stages of development will then result in programming of both the reproductive and metabolic features of PCOS. Intriguingly, data from studies of the human fetal ovary indicate that the “machinery” for androgen production and action within the ovary is present during fetal life. Protein expression of P450c17 (a key enzyme in androgen production) has been reported in follicles of human fetal ovaries 22 and recent data point to the abundance of androgen receptor during follicle formation in the human ovary 23.
Fig 1.
Proposed developmental origin of PCOS (from Franks S, Int J Obes 2008 32:1035–41)
Once in train, the consequent hypersecretion of LH and hyperinsulinemia may further amplify androgen production by ovarian theca cells, thus creating a vicious circle of events. As well as the initial genetic ”insult”, there are likely to be other points at which genes have an effect on phenotype eg in genetic predisposition to obesity and insulin resistance. And, of course, environmental factors, particularly dietary, come into play to influence the clinical and biochemical abnormalities.
Evidence that the proposed programming actions of androgen occur in human PCOS is inevitably more difficult to establish than it is animal models, but there are strong hints of such an action from observation of PCOS-like symptoms in girls before and during puberty particularly if there is a family history 24 and studies which shows that typical features of PCOS occur during adolescence in girls with adrenal androgen excess due to congenital adrenal hyperplasia (CAH) 25.
Summary
The similarity of reproductive and metabolic phenotype between prenatally androgenised sheep, or monkeys, and women with PCOS provides strong supportive evidence for developmental programming being important in the etiology of PCOS. The human fetal ovary has the “machinery” for androgen production and reception, suggesting that androgen can exert its effects during fetal life as well as during other key developmental windows. The appearance of PCOS-like symptoms before and during puberty in girls again lend weight to the notion of the developmental origin of PCOS and the role of excess androgen in this process is supported by the observation that girls with CAH have a predisposition to development of clinical and biochemical features of PCOS. In conclusion, there is strong evidence that polycystic ovary syndrome has developmental origins.
Con – No, PCOS Does Not Have Developmental Origins
Sarah L. Berga, MD
Developmental Origins as Adaptation Gone Astray
To address the question as to whether polycystic ovary syndrome (PCOS) has developmental origins, one must begin with a consideration of the conceptual framework and nomenclature. No one would argue against the notion that polycystic ovary syndrome is a condition with high heterogeneity of clinical presentation. Indeed, diagnostic criteria remain controversial and there is no consensus regarding pathognomonic features. Similarly, the phrase “developmental origins” evokes a variety of interpretations and certainly it is not universally understood as engaging a single mechanism. Gluckman and Hanson define the “developmental origins of disease” as a paradigm that posits the persistence of once adaptive mechanisms in humans who now live in very different environments from those within which they evolved [26]. However, the same phrase is also understood to indicate the interaction between the fetal genome and the maternal-placental milieu, which would put PCOS into the category of an imprinted disorder with a restricted window of exposure and a limited number of putative mechanisms mediating the association. Further, to fully address the topic as to whether PCOS is developmental in origin, one must also decide if PCOS is a disease or an adaptation. A disease is defined as “a pathological condition of the body that presents a group of symptoms peculiar to it and which sets the condition apart as an abnormal entity differing from the other normal or pathological body states” [27] whereas an adaptation is defined as “in biology, the ability of an organism to adjust to a change in environment” [27]. With these concepts in mind, we can consider whether PCOS is a disease, that is, (1) a fixed set of genetic variants such as snps (small nucleotide polymorphisms), mutations, or altered regulatory regions with variable phenotypic penetrance, (2) a developmental disorder triggered in response to a deleterious intrauterine environment, (3) a fixed change in an encoding region of the genome such as sickle cell hemoglobinopathy that was once an adaptive but is now mostly an adaptation gone astray, or (4) an admixture of any of the above. Further, we must also consider if the only potential “developmental window” for PCOS is during fetal life. Lastly, for the distinction as to whether PCOS is a development disorder or not to be relevant, it must carry diagnostic or therapeutic implications.
Either PCOS has a multiplicity of etiologies or any single pathogenetic explanation must account for all of the cardinal features, namely, chronic anovulation, ovarian morphology, gonadotropin aberrations, insulin resistance, dyslipidemia, hyperandrogenism, and android habitus. If this constellation of features were purely developmental in origin, then all female fetuses exposed to an “unfavorable” milieu in utero would be expected to develop PCOS and only those fetuses. If not all fetuses exposed to an abnormal milieu develop PCOS, then one would have to conclude that there are other determinants that are either genetic in origin or that involve postnatal adaptations. Likewise, one must consider whether all male fetuses exposed to a comparable unfavorable intrauterine milieu develop the male analog of PCOS and only those male fetuses. If not, then there must be other determinants of PCOS that are either genetic or epigenetic and entail postnatal modification. Although it was once thought that epigenetic marks were primarily conferred during fertilization, embryogenesis, and pregnancy, we now know that epigenetic regulation exhibits plasticity indefinitely during postnatal life [28].
Is PCOS An Adaptation Gone Astray?
Given these considerations, it seems unlikely that PCOS is purely developmental in origin or that the developmental window is strictly intrauterine. While there may be certain genotypic predispositions that confer greater reactivity to certain intrauterine conditions and thereby produce a PCOS phenotype, it seems unlikely that all PCOS phenotypes occur only in response to adverse intrauterine exposures. Certainly, not all fetuses exposed to intrauterine adversity develop PCOS. Thus, the situation must be more interactive. Further, it would be difficult to argue that when the interaction of a given genotype with a certain intrauterine environment yields a PCOS phenotype that this result is always strictly maladaptive or was once adaptive but is now an adaptation gone astray. Indeed, women with PCOS often display a number of adaptive features, including stress resistance [29], athleticism [30], and later in life fertility [31]. To put this line of reasoning into perspective, it might be worth considering an analogous situation, namely, adrenal activation by environmental stressors. Too little or too short of a cortisol response and too much or too prolonged of a cortisol response can be maladaptive. Since adversity is not confined to any one time in one’s life, the hypothalamic-pituitary-adrenal axis must remain functional and reactive and bouts of intermittent hypercortisolism may imprint the genome epigenetically throughout the lifespan. Hypercortisolemia, even when prolonged, may well be an adaptive response with longer-term negative health sequel, but no one would argue that having a responsive hypothalamic-pituitary-adrenal (HPA) axis is an adaptation gone astray. Further, comparable stress exposures will not elicit comparable stress reactivity in all individuals so exposed and will not elicit the same health consequences in all so exposed. Clearly our genetic and acquired epigenetic heterogeneity produces a range of responses among individuals. We are just beginning to discover the multiple molecular mechanisms that create this heterogeneity as we seek to develop ever more “personalized medicine”. Further, it is worth highlighting that we retain adaptive mechanisms even though we do not need them on a daily basis. The same argument could be made for the immune system. Immunity can go astray as in the case of autoimmunity, but we need our immune system to remain reactive. In certain circumstances, both overactivity and underactivity of the immune system may pose a hazard to the host. Certainly, the activity of both the immune system and HPA axis engendered by a new challenge will be gated in part by past experiences and exposures. In this sense, the developmental window remains open for as long as we live as our epigenome is continuously remodeled.
If PCOS Is Not Developmental in Origin, What Causes PCOS?
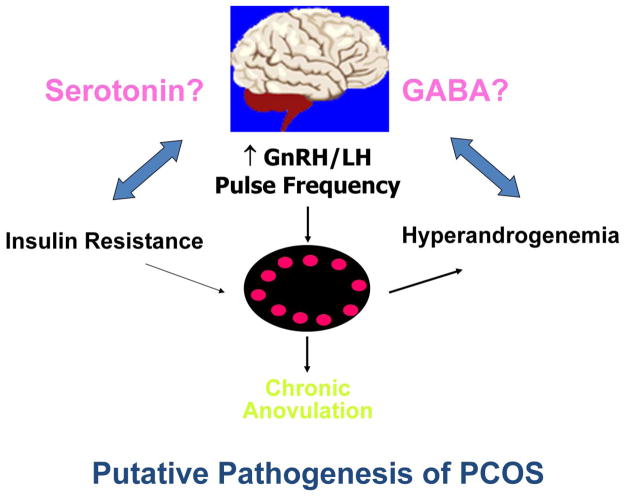
If PCOS is not purely developmental in origin, what might be the genotypic features that predispose to PCOS in response to certain intrauterine and extrauterine conditions? I offer the notion that insulin resistance and hyperandrogenism are the twin manifestations of a metabolic genotype that slows apoptosis and aging, thereby promoting mitosis and (1) increased oocyte endowment and/or slowed atresia, that manifests as polycystic ovarian morphology; (2) increased thecal cell endowment, which manifests as stromal echogenicity on ultrasound imaging and hyperandrogemia; (3) more GnRH neurons and/or greater GnRH neuronal connectivity leading to increased GnRH drive that manifests as increased LH pulse frequency and amplitude as well as decreased FSH with resultant anovulation; and (4) increased number of adipocytes that amplify insulin resistance and hyperandrogenism. As shown in Figure 2, centrally, these signaling systems appear to be integrated via the GABAergic system, which we have shown to be altered, as reflected by increased CSF concentrations of GABA, in women with polycystic ovary syndrome [32].
Figure 2.
PCOS as the interaction of insulin resistance and hyperandrogenism altering central processes that subserve reproduction and metabolism.
Summary
In summary, while one would not exclude altogether developmental determinants of PCOS, it is difficult to view PCOS as purely developmental or resulting only from intrauterine exposures or simply an adaptation gone astray. Even in the modern era, there may be benefits to the constellation of features we variably recognize as and label PCOS. Certainly, a more nuanced perspective of the physiology of PCOS may help us to recognize when and how to intervene. A more refined perspective regarding the spectrum of PCOS may help us avoid reductionistic classification schemes that lead to false dichotomies and stigmatization. Humans have an abundance of redundant physiological mechanisms that confer plasticity in the face of an ever changing and ever challenging milieu. To view these adaptive mechanisms as disease is to make static that which is meant to be protean. Further, if we are able to identify and then modify environmental determinants, then we will be better able to safeguard the health of those whose genotype or previous exposures put them most at risk to develop to outright disease.
Acknowledgments
Funded in part by NIH/NCRR-00056 and NIH/NICHD U54 08610
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Stephen Franks, Email: s.franks@imperial.ac.uk, Institute of Reproductive & Developmental Biology, Imperial College London, Hammersmith Hospital, London W12 0NN.
Sarah L. Berga, Email: sberga@wakehealth.edu, Department of Obstetrics and Gynecology, Associate Dean of Women’s Health Research, Wake Forest University School of Medicine, Vice President of Women’s Health, Wake Forest University Baptist Medical Center, Winston-Salem, North Carolina, 27157 USA.
References
- 1.Abbott DH, Dumesic DA, Franks S. Developmental origin of polycystic ovary syndrome - a hypothesis. J Endocrinol. 2002;174(1):1–5. doi: 10.1677/joe.0.1740001. [DOI] [PubMed] [Google Scholar]
- 2.Ferriman D, Purdie AW. The inheritance of polycystic ovarian disease and a possible relationship to premature balding. Clin Endocrinol (Oxf) 1979;11(3):291–300. doi: 10.1111/j.1365-2265.1979.tb03077.x. [DOI] [PubMed] [Google Scholar]
- 3.Givens JR. Familial polycystic ovarian disease. Endocrinol Metab Clin North Am. 1988;17(4):771–83. [PubMed] [Google Scholar]
- 4.Hague WM, Adams J, Reeders ST, Peto TE, Jacobs HS. Familial polycystic ovaries: a genetic disease? Clin Endocrinol (Oxf) 1988;29(6):593–605. doi: 10.1111/j.1365-2265.1988.tb03707.x. [DOI] [PubMed] [Google Scholar]
- 5.Lunde O, Magnus P, Sandvik L, Hoglo S. Familial clustering in the polycystic ovarian syndrome. Gynecol Obstet Invest. 1989;28(1):23–30. doi: 10.1159/000293493. [DOI] [PubMed] [Google Scholar]
- 6.Carey AH, Chan KL, Short F, White D, Williamson R, Franks S. Evidence for a single gene effect causing polycystic ovaries and male pattern baldness. Clin Endocrinol (Oxf) 1993;38(6):653–8. doi: 10.1111/j.1365-2265.1993.tb02150.x. [DOI] [PubMed] [Google Scholar]
- 7.Legro RS, Driscoll D, Strauss JF, 3rd, Fox J, Dunaif A. Evidence for a genetic basis for hyperandrogenemia in polycystic ovary syndrome. Proc Natl Acad Sci U S A. 1998;8;95(25):14956–60. doi: 10.1073/pnas.95.25.14956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Legro RS, Bentley-Lewis R, Driscoll D, Wang SC, Dunaif A. Insulin resistance in the sisters of women with polycystic ovary syndrome: association with hyperandrogenemia rather than menstrual irregularity. J Clin Endocrinol Metab. 2002;87(5):2128–33. doi: 10.1210/jcem.87.5.8513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Franks S, Webber LJ, Goh M, Valentine A, White DM, Conway GS, et al. Ovarian morphology is a marker of heritable biochemical traits in sisters with polycystic ovaries. J Clin Endocrinol Metab. 2008;93(9):3396–402. doi: 10.1210/jc.2008-0369. [DOI] [PubMed] [Google Scholar]
- 10.Vink JM, Sadrzadeh S, Lambalk CB, Boomsma DI. Heritability of polycystic ovary syndrome (PCOS) in a Dutch twin-family study. J Clin Endocrinol Metab. 2006;11;91:2100–4. doi: 10.1210/jc.2005-1494. [DOI] [PubMed] [Google Scholar]
- 11.Urbanek M. The genetics of the polycystic ovary syndrome. Nat Clin Pract Endocrinol Metab. 2007;3(2):103–11. doi: 10.1038/ncpendmet0400. [DOI] [PubMed] [Google Scholar]
- 12.Franks S, McCarthy M. Genetics of ovarian disorders: polycystic ovary syndrome. Rev Endocr Metab Disord. 2004;5(1):69–76. doi: 10.1023/B:REMD.0000016125.05878.96. [DOI] [PubMed] [Google Scholar]
- 13.Chen ZJ, Zhao H, He L, Shi Y, Qin Y, Li Z, et al. Genome-wide association study identifies susceptibility loci for polycystic ovary syndrome on chromosome 2p16.3, 2p21 and 9q33.3. Nat Genet. 2011;43(1):55–9. doi: 10.1038/ng.732. [DOI] [PubMed] [Google Scholar]
- 14.Dumesic DA, Abbott DH, Padmanabhan V. Polycystic ovary syndrome and its developmental origins. Rev Endocr Metab Disord. 2007;8(2):127–41. doi: 10.1007/s11154-007-9046-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Padmanabhan V, Veiga-Lopez A, Abbott DH, Recabarren SE, Herkimer C. Developmental programming: impact of prenatal testosterone excess and postnatal weight gain on insulin sensitivity index and transfer of traits to offspring of overweight females. Endocrinology. 2010;151(2):595–605. doi: 10.1210/en.2009-1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hogg K, McNeilly AS, Duncan WC. Prenatal androgen exposure leads to alterations in gene and protein expression in the ovine fetal ovary. Endocrinology. 2011;152(5):2048–59. doi: 10.1210/en.2010-1219. [DOI] [PubMed] [Google Scholar]
- 17.Manneras L, Cajander S, Holmang A, Seleskovic Z, Lystig T, Lonn M, et al. A new rat model exhibiting both ovarian and metabolic characteristics of polycystic ovary syndrome. Endocrinology. 2007;148(8):3781–91. doi: 10.1210/en.2007-0168. [DOI] [PubMed] [Google Scholar]
- 18.Demissie M, Lazic M, Foecking EM, Aird F, Dunaif A, Levine JE. Transient prenatal androgen exposure produces metabolic syndrome in adult female rats. Am J Physiol Endocrinol Metab. 2008;295(2):E262–8. doi: 10.1152/ajpendo.90208.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Webber LJ, Stubbs S, Stark J, Trew GH, Margara R, Hardy K, et al. Formation and early development of follicles in the polycystic ovary. Lancet. 2003;27;362(9389):1017–21. doi: 10.1016/s0140-6736(03)14410-8. [DOI] [PubMed] [Google Scholar]
- 20.Maciel GA, Baracat EC, Benda JA, Markham SM, Hensinger K, Chang RJ, et al. Stockpiling of transitional and classic primary follicles in ovaries of women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2004;89(11):5321–7. doi: 10.1210/jc.2004-0643. [DOI] [PubMed] [Google Scholar]
- 21.Forsdike RA, Hardy K, Bull L, Stark J, Webber LJ, Stubbs S, et al. Disordered follicle development in ovaries of prenatally androgenized ewes. J Endocrinol. 2007;192(2):421–8. doi: 10.1677/joe.1.07097. [DOI] [PubMed] [Google Scholar]
- 22.Cole B, Hensinger K, Maciel GA, Chang RJ, Erickson GF. Human fetal ovary development involves the spatiotemporal expression of p450c17 protein. J Clin Endocrinol Metab. 2006;91(9):3654–61. doi: 10.1210/jc.2006-0641. [DOI] [PubMed] [Google Scholar]
- 23.Fowler PA, Anderson RA, Saunders PT, Kinnell H, Mason JI, Evans DB, et al. Development of steroid signaling pathways during primordial follicle formation in the human fetal ovary. J Clin Endocrinol Metab. 2011;96(6):1754–62. doi: 10.1210/jc.2010-2618. [DOI] [PubMed] [Google Scholar]
- 24.Sir-Petermann T, Codner E, Perez V, Echiburu B, Maliqueo M, Ladron de Guevara A, et al. Metabolic and reproductive features before and during puberty in daughters of women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2009;94(6):1923–30. doi: 10.1210/jc.2008-2836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barnes RB, Rosenfield RL, Ehrmann DA, Cara JF, Cuttler L, Levitsky LL, et al. Ovarian hyperandrogynism as a result of congenital adrenal virilizing disorders: evidence for perinatal masculinization of neuroendocrine function in women. J Clin Endocrinol Metab. 1994;79(5):1328–33. doi: 10.1210/jcem.79.5.7962325. [DOI] [PubMed] [Google Scholar]
- 26.Gluckman PD, Hanson MA. Developmental origins of disease paradigm: a mechanistic and evolutionary perspective. Pediatr Res. 2004;56:311–317. doi: 10.1203/01.PDR.0000135998.08025.FB. [DOI] [PubMed] [Google Scholar]
- 27.Taber’s Cyclopedic Medical Dictionary. 12 [Google Scholar]
- 28.Lester BM, Tronick E, Nestler E, Abel T, Kosofsky B, Kuzawa CW, et al. Behavioral epigenetics. Ann N Y Acad Sci. 2011;1226:14–33. doi: 10.1111/j.1749–6632.2011.06037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berga SL, Daniels TL, Giles DE. Women with functional hypothalamic amenorrhea but not other forms of anovulation display amplified cortisol concentrations. Fertil Steril. 1997;67(6):1024–30. doi: 10.1016/s0015-0282(97)81434-3. [DOI] [PubMed] [Google Scholar]
- 30.Rickenlund A, Carlström K, Ekblom B, Brismar TB, von Schoultz B, Hirschberg AL. Hyperandrogenicity is an alternative mechanism underlying oligomenorrhea or amenorrhea in female athletes and may improve physical performance. Fertil Steril. 2003;79(4):947–55. doi: 10.1016/s0015-0282(02)04850-1. [DOI] [PubMed] [Google Scholar]
- 31.Mellembakken JR, Berga SL, Kilen M, Tanbo TG, Abyholm T, Fedorcsák P. Sustained fertility from 22 to 41 years of age in women with polycystic ovarian syndrome. Hum Reprod. 2011;26(9):2499–504. doi: 10.1093/humrep/der214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Loucks TL, Berga SL. Abstract # OR-33–1, 84th Annual Meeting of the Endocrine Society; San Francisco, CA. June 21, 2002. [Google Scholar]