Abstract
OBJECTIVE
It is unclear whether people with and without diabetes equally benefitted from reductions in cardiovascular disease (CVD). We aimed to compare recent trends in hospital admission rates for angina, acute myocardial infarction (AMI), stroke, percutaneous coronary intervention (PCI), and coronary artery bypass graft (CABG) among people with and without diabetes in England.
RESEARCH DESIGN AND METHODS
We identified all patients aged >16 years with cardiovascular events in England between 2004–2005 and 2009–2010 using national hospital activity data. Diabetes- and nondiabetes-specific rates were calculated for each year. To test for time trend, we fitted Poisson regression models.
RESULTS
In people with diabetes, admission rates for angina, AMI, and CABG decreased significantly by 5% (rate ratio 0.95 [95% CI 0.94–0.96]), 5% (0.95 [0.93–0.97]), and 3% (0.97 [0.95–0.98]) per year, respectively. Admission rates for stroke did not significantly change (0.99 [0.98–1.004]) but increased for PCI (1.01 [1.005–1.03]) in people with diabetes. People with and without diabetes experienced similar proportional changes for all outcomes, with no significant differences in trends between these groups. However, diabetes was associated with an ~3.5- to 5-fold risk of CVD events. In-hospital mortality rates declined for AMI and stroke, remained unchanged for CABG, and increased for PCI admissions in both groups.
CONCLUSIONS
This national study suggests similar changes in admissions for CVD in people with and without diabetes. Aggressive risk reduction is needed to further reduce the high absolute and relative risk of CVD still present in people with diabetes.
The incidence and mortality from cardiovascular disease (CVD) have declined markedly during the last several decades in the U.K. and other Western societies (1–3). Advances in understanding and control of major cardiovascular risk factors and medical care of CVD have contributed to these reductions (4). However, although previous reports from different populations and study settings have emphasized favorable trends in adults without diabetes, conflicting findings were reported in people with diabetes. Some data indicate similar reductions in CVD rates in these groups, whereas other data report that adults with diabetes had lower declines in their CVD event rates compared with the improvement experienced by people without diabetes (5–8). Some studies found no evidence that people with diabetes, particularly women, benefited from the reductions in CVD incidence (7,9). In the U.K., the considerable recent increases in obesity and diabetes, particularly among young and middle-aged adults, could increase CVD rates (10). A study showed increased coronary heart disease (CHD) mortality rates in young men in 2002 in England and Wales and explained this finding by adverse trends in CHD risk factors (11).
As part of a national strategy to reduce CVD mortality, a number of quality-improvement initiatives were introduced in the U.K. health system during the last decade, with a major emphasis on secondary prevention (12–14). However, there are no data available on whether these reforms have had a significant effect on the clinical outcomes of diabetes, such as cardiovascular events.
Although CVD remains the leading cause of death and hospitalization for CVD is one of the main users of health resources, data on recent national trends in CVD among people with and without diabetes in England are lacking. The objective of this study was to describe the trends in the rate of major cardiovascular events requiring hospital admission (myocardial infarction [MI], angina, and stroke) and cardiovascular interventions (percutaneous coronary intervention [PCI] and coronary artery bypass graft [CABG]) among people with and without diabetes between 2004 and 2009 in England. We also aimed to describe the relative risk of these events in people with diabetes.
RESEARCH DESIGN AND METHODS
We examined an extract of Hospital Episode Statistics data between the financial years 2004–2005 and 2009–2010 for all National Health Service (NHS) hospital trusts in England. The dataset covers all inpatient hospital activity and day case admissions to NHS (public) hospitals across England, including private patients treated in NHS hospitals. Data extracted for each hospital admission included patient demographics (age and sex), in-hospital mortality, length of hospital stay (LOS), principal diagnosis, and up to 13 secondary diagnoses coded using the ICD-10. Interventions were defined using the Office of Population Censuses and Surveys’ Classification of Surgical Operations (OPCS4) codes in up to 12 procedure fields. Diabetes status was based on type 1 or type 2 diabetes, ICD-10 codes E10 and E11, recorded in any diagnosis field.
Cardiovascular complications, identified as the principal or primary diagnosis on admission, were acute MI (AMI; ICD-10 I21 and I22), angina (ICD-10 I20), and stroke (ICD-10 I60–I64). Cardiovascular interventions were identified using procedure codes for PCI (OPCS4 K49, K50, and K75) or CABG (OPCS4 K40–K46) in any procedure field. We used a combination of date of birth, sex, and full postcode to distinguish patients.
To assess comorbidity in the population, the Charlson Comorbidity Index was used, derived from ICD-10 diagnoses (15). The index is based on a number of medical conditions, each with original weights ranging from 1 to 6; we derived England-specific weights ranging from −1 to +18. Higher scores represent a greater burden of comorbidity.
Admission rates in people with diabetes were calculated for each year using the total number of admissions for CVD as the numerator and the total number of people with diabetes in England as the denominator. Data on the number of people aged >16 years who were diagnosed with diabetes in England were obtained from the Quality Management and Analysis System (QMAS) for each study year (14). The QMAS is the financial database for the Quality and Outcomes Framework (QOF) and contains diabetes counts and prevalence data for virtually all (>99%) general practices in England. Because the QMAS does not hold information on the age and sex distribution of the population with diabetes, we obtained this information from the Health Survey for England 2006 (10). When calculating age- and sex-specific rates, we assumed that the age and sex distribution of the population with diabetes remained constant between 2004 and 2009 (10). For 2004–2005 and 2005–2006, when diabetes figures were available for the total population, we calculated diabetes prevalence for patients aged >16 years for both years, using the age- and sex-standardized diabetes prevalence in children and young adults (16). This enabled us to calculate age- and sex-specific admission rates for each event and intervention for each year during the study period. The estimated resident population of England was used to calculate the admission rate of CVD events in people without diabetes for each year (17). The number of people with diabetes was deducted from each corresponding age and sex stratum of the total population. Therefore, the denominator for people without diabetes did not include the total population (both people with and without diabetes), only the number of people without diabetes. Rates were expressed per 100,000 people with or without diabetes.
To test time trends in CVD rates, we fitted separate Poisson regression models for patients with and without diabetes, using age, sex, and year as independent variables. Interactions between sex and year and between age and year were tested, and Poisson models were fitted for sex and age subgroups if P < 0.05 for the interactions. We estimated the risk of a person with diabetes being admitted to the hospital for CVD compared with a person without diabetes. Statistical analyses were performed using Stata (College Station, TX).
RESULTS
Between 2004 and 2009, 519,433 admissions for angina (100,978 [19.4%] with diabetes), 430,356 for AMI (80,578 [18.7%] with diabetes), and 466,650 for stroke (70,081 [15.0%] with diabetes) were identified. There were 353,205 PCIs (59,238 [16.8%] with diabetes) and 133,676 CABGs (29,571 [22.1%] with diabetes). Table 1 shows the absolute number of admissions and characteristics of people admitted for CVD by recorded diabetes status in 2004 and 2009. In people with diabetes, a larger number of admissions for cardiovascular interventions and stroke were recorded in 2009 compared with 2004, and the number of admissions for angina and AMI were comparable in 2004 and 2009. By contrast, the number of admissions for angina, AMI, and CABG decreased in people without diabetes, whereas there was an increase in PCIs and an unchanged number of stroke admissions.
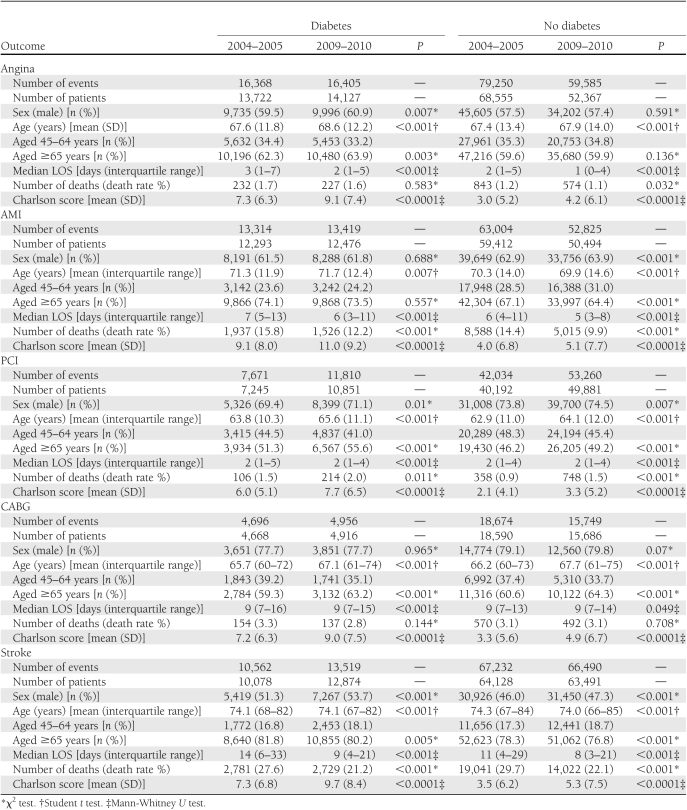
Table 1.
Characteristics of people with and without diabetes affected by CVD between 2004 and 2009 in England
There was a considerable male excess of CVD admissions overall in both groups, except for stroke, among people without diabetes (Table 1). This male predominance was most pronounced for cardiovascular interventions in both individuals with and without diabetes. Most CVD events occurred in individuals aged ≥65 years, with a significantly higher proportion in people with diabetes (P < 0.001 for all), except for CABG (P = 0.17). In 2009, the median LOS was significantly lower for all admissions in both groups compared with 2004. However, the size of this decrease was small for cardiovascular procedures. The mean Charlson Comorbidity Index score was significantly higher in 2009 in both groups for all admissions compared with 2004 (Table 1).
In-hospital mortality rates
Changes in in-hospital mortality rates showed similar patterns in people with and without diabetes, with a significant decline for AMI and stroke, increased rates for PCI, and unchanged rates for CABG admissions (Table 1). For angina admissions, there was a significant decline in mortality rates in people without diabetes, whereas rates in patients with diabetes did not significantly change.
Changes in admission rates
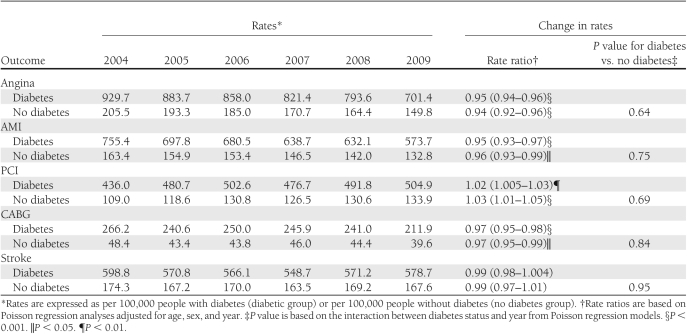
Between 2004 and 2009, admission rates for angina, AMI, and CABG decreased significantly in people with diabetes in England, with rate ratios of 0.95 (95% CI 0.94–0.96), 0.95 (0.93–0.97), and 0.97 (0.95–0.98) (P < 0.001 for all) per year, respectively (i.e., decreases of 5, 5, and 3% annually) (Table 2). PCI rates in people with diabetes increased significantly, and the incidence of stroke did not significantly change. Over the study period, people without diabetes experienced similar proportional changes for all CVD outcomes as those with diabetes, with no statistically significant differences in trends between these groups (Table 2).
Table 2.
Rates of hospital admissions for CVD events and interventions in people with and without diabetes for each year between 2004 and 2009 in England
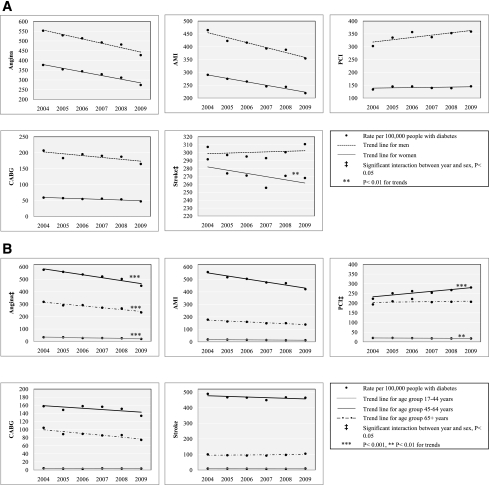
The trend in stroke admissions in individuals with diabetes varied by sex, but this was not evident for other outcomes (Fig. 1A). In women with diabetes, there was a significant decline in admissions for stroke (rate ratio 0.99 per year [95% CI 0.97–0.99]; P = 0.005), whereas there was a nonsignificant increase in rates in men (1.00 per year [0.99–1.01]; P = 0.47).
Figure 1.
Rates of admissions for CVD in people with diabetes by sex (A) and age (B) groups between 2004 and 2009 in England. Rates are expressed as 100,000 people with diabetes. Trends were tested separately for men and women and different age-groups if P < 0.05 for the sex-year or age-group–year interaction.
When examining trends across different age-groups, significant variations were found in people with diabetes for angina admissions and PCI (Fig. 1B). With regard to angina, a similar but more pronounced decline was seen among older subjects with diabetes (aged ≥65 years: 0.91 per year [95% CI 0.89–0.93]; P < 0.001) compared with those aged 17–44 years and 45–64 years (0.95 per year for both [0.94–0.96]; P < 0.001). For PCI, rates increased in older individuals with diabetes (aged ≥65 years: 1.04 per year [1.02–1.05]; P < 0.001), whereas there was a significant decline in younger patients (aged 17–44 years: 0.97 [0.94–0.98]; P = 0.001), and rates remained unchanged for those aged 45–64 years (1.004 [0.99–1.02]; P = 0.60). Trends in rates in people without diabetes did not vary by age (not shown).
Relative risk
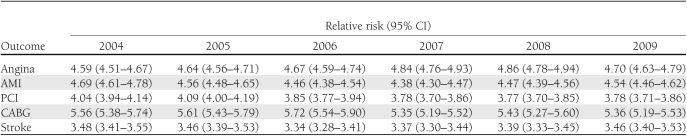
People with diabetes were approximately five times more likely to be admitted for angina, AMI, and CABG; four times more likely to undergo a PCI; and three and a half times more likely to be admitted for a stroke than those without diabetes (Table 3). These figures did not significantly change during the study period.
Table 3.
Risk of CVD events in people with diabetes compared with those without diabetes between 2004 and 2009 in England
CONCLUSIONS
These national data show a considerable decline in hospital admission rates for angina, AMI, and CABG; unchanged rates for stroke; and an increase in PCI procedure rates among both people with and without diabetes in England between financial years 2004–2005 and 2009–2010. The results also suggest that individuals with diabetes experienced similar proportional changes in all CVD outcomes as people without diabetes.
However, people with diabetes continue to remain at ~3.5- to 5-fold higher risk of hospitalization for major CVD events and interventions than people without diabetes.
In-hospital mortality rates declined significantly for AMI and stroke, remained unchanged for CABG, and increased for PCI admissions in both individuals with and without diabetes.
Since the late 1970s, there have been marked reductions in CVD event and mortality rates in most industrialized countries (1,3,4). However, these improvements attenuated during the 1990s among adults aged <55 years compared with previous trends (11,18). When examining population subgroups, one study showed reversed trends in CHD mortality rates in young men aged 35–44 years in the U.K. during the 1990s (11). Some studies suggested that the benefits of population changes in CVD rates might not be shared equally among people with and without diabetes, and diabetes might be a major contributor to the slowdown of improvement seen in the population (7,9). Although it is important to understand whether people with and without diabetes are affected differently by CVD, there is little information on recent trends in CVD rates in people with and without diabetes in England. The majority of previous studies have not reported diabetes-specific CVD outcome rates because of the lack of accurate information on diabetes prevalence (11,19,20). The results of cohort or local studies also might not reflect national trends (6,21). This is the first study we are aware of that identifies recent admission rates for major CVD events in people with diabetes using a national sample that covers the entire population of England.
Numerous factors could explain the favorable trends in hospital admissions for acute coronary syndrome and intervention rates over the study period. The prevention and treatment of CVD and its risk factors have assumed increasing importance in U.K. health policy during the last decade (12,14). The U.K. government has made considerable investments in health services and introduced a wide range of initiatives, including national treatment standards for the management of major chronic conditions with a special focus on secondary prevention (14,22). The introduction of the QOF, a major pay-for-performance program in 2004, was associated with accelerated improvements in CVD risk factors, including blood pressure and cholesterol control in people with diabetes (14). Favorable trends in cigarette smoking, physical activity levels, and increased use of ACE inhibitors and antihypertensive and lipid-lowering medications also might have contributed to these changes (10). Furthermore, better treatment of CVD itself also could have translated into reductions in admission and readmission rates for CVD (4).
Our results correspond with studies reporting similar reductions in CVD rates among people with and without diabetes (5,6,21). Some earlier studies found smaller improvement in CVD events in those with diabetes (7,9,23). There are several potential explanations for this discrepancy beyond differences in study design and case definition. People with diabetes often were less likely to receive intensive treatment for their CVD and CVD risk factors and were less likely to undergo therapeutic interventions compared with those without diabetes (24,25). For example, several studies demonstrated that people with diabetes presenting with an AMI were less likely to receive evidence-based treatments, including β-blockers, aspirin, thrombolysis, and revascularization procedures compared with those without diabetes (24,25). Furthermore, the intensity of the management showed inverse association with increasing cardiovascular risk, further disadvantaging older individuals and those with more comorbidities (24,26). Hence, the higher baseline cardiovascular risk was compounded by a suboptimal treatment of the condition and its risk factors in individuals with diabetes. In previous studies, the lower level of improvement in CVD outcomes in people with diabetes may have partly followed from these disparities.
Our results might reflect changes in historical patterns of care in England. People with diabetes now get more aggressive management for their condition than during previous years as a result of increased awareness of diabetes and various nationwide targeted interventions (14,27). This is supported by a number of recent studies showing substantial improvement in diabetes management and cardiovascular risk factor control in U.K. primary care as a result of targeted interventions (14,27,28). Recent studies from the U.K. show that people with diabetes with a higher number of comorbid conditions receive more intensive treatment and are more likely to achieve established treatment targets compared with counterparts with less comorbidities, which indicate changes in previous patterns (24,26,28,29). These findings are further supported by our results showing increasing PCI rates and a parallel decline in CABG rates in people with diabetes, a similar manner to people without diabetes.
As in other studies, we found that PCI rates increased significantly, whereas CABG rates declined, during the study period (30,31). Changes in practice patterns could be attributable to CABG being the more invasive procedure and advances in PCI such as the introduction of drug-eluting stents and considerable improvements in the short- and long-term outcomes of PCI, among other factors (32). Despite substantial evidence that for patients with severe forms of CHD, particularly patients with diabetes, CABG offers advantages in terms of survival and need for repeat revascularization, we found a similar shift from CABG to PCI in people with diabetes as in individuals without diabetes. The increases in in-hospital mortality rates for PCI, despite technological advances in interventional techniques and improvements in periprocedural care, might be attributable to the increasing complexity of cases referred for PCI.
We found similar proportional changes in admission rates for AMI, stroke, and CABG in elderly when compared with younger individuals with diabetes. The overall increase in PCI rates in people with diabetes could largely be explained by the expansion of PCI in the elderly. Furthermore, people aged ≥75 years with diabetes experienced a larger annual decline in admission rates for angina than younger patients. These findings might reflect more aggressive treatment applied in higher-risk patients compared with previous years, as earlier studies described inverse associations between treatment propensity and age. A recent study showed largely attenuating differences in the measurement and achievement of established treatment targets between elderly patients aged ≥75 years and younger individuals with diabetes after the introduction of the QOF (27).
Our observation of stable admission rates of stroke in people with and without diabetes differs from earlier studies (5,33). However, it is difficult to make direct comparisons, because most studies did not report trends by diabetes status, had considerably longer follow-up time, were conducted a long time ago, or reported rates from small geographic areas (34,35). There are limited data on temporal changes in stroke incidence from the U.K. A recent systematic review only could identify one article reporting trends in stroke incidence in the U.K., which showed a decline in south London over the period of 1995–2004 (35). A local study reported a decrease in the number and incidence of major stroke in Oxfordshire between 1981 and 2004 (34). The reason of the significant decline found in women but not in men with diabetes is unclear. The World Health Organization MONICA (Multinational Monitoring of Trends and Determinants in Cardiovascular Disease) project showed decreased stroke rates among men in 13 populations and among women in 15 of 17 MONICA populations in 1997. However, this study did not report stroke rates for people with and without diabetes, and the number of populations with statistically significant trends were small (33). It is possible that the larger recent improvements in blood pressure and cholesterol control in women with diabetes since the introduction of the QOF, particularly in the elderly, could partly explain our finding (27).
Our national study used a sample that covers the entire population of England and therefore is likely to provide an accurate reflection on population changes in CVD rates. Previous studies are limited by the lack of available or accurate data on diabetes prevalence. By contrast, the diabetes denominator for our study was derived from a national database. Given that ~99% of the U.K. population is registered with a general practitioner, and nearly all practices participate in the pay-for-performance program that financially incentivizes disease registers, our estimations likely are to be robust (14).
Limitations of our study need to be considered when interpreting our results. Although concerns about the accuracy of routinely collected datasets have been raised, these data are continuously audited, and the quality and validity of this dataset has been assessed and proved useful for health research (19,36,37). A systematic review of discharge coding evaluated it as high, especially for operations and procedures (36). Better ascertainment and recording of diabetes after the implementation of the QOF might explain some of the increase in diabetes prevalence during the study period, because general practices are financially incentivized to identify and report all diabetes cases. However, the increase was consistent during the study period, and most of the improved ascertainment likely is to have occurred immediately before the study period as practices responded to the incentives in the QOF. Furthermore, the increase in the mean Charlson Comorbidity Index score, which would indicate the admission of more complex cases for CVD, is likely to also reflect better coding of less common comorbid conditions on hospital records since the introduction of payment by results, a new payment regimen for hospitals introduced in 2005–2006 (38). We did not distinguish between type 1 and type 2 diabetes because separate data on national prevalence were not available.
Our data provide recent national information on changes in the burden of CVD events across England. Our results show a considerable recent decline in admissions for angina, AMI, and CABG; unchanged stroke rates; and increasing PCI rates in people with and without diabetes. However, despite significant declines, people with diabetes still are at an ~3.5- to 5-fold risk of CVD events compared with those without diabetes. Furthermore, the absolute population burden of CVD is expected to further rise, given the rapidly increasing prevalence of diabetes and the aging population. Hence, these findings emphasize the ongoing need for aggressive risk reduction and primary prevention of CVD in people with diabetes.
Acknowledgments
The research leading to these results received funding from the European Community Seventh Framework Programme (grant no. 277047). C.M. is funded by the Higher Education Funding Council for England and the National Institute for Health Research (NIHR). C.P., P.A., A.B., and the Dr. Foster Unit at Imperial are principally funded with a research grant by Dr. Foster Intelligence, an independent health care information company and joint venture with the Information Centre of the National Health Service (NHS). The Dr. Foster Unit is affiliated with the Centre for Patient Safety and Service Quality at Imperial College Healthcare NHS Trust, which is funded by the NIHR.
No potential conflicts of interest relevant to this article were reported.
E.P.V. researched the data and wrote the manuscript. C.M., P.A., and A.M. contributed to the discussion and reviewed and edited the manuscript. C.P. researched the data. A.B. researched the data, contributed to the discussion, and reviewed and edited the manuscript. A.M. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Parts of this study were presented in abstract form at the 47th Annual Meeting of the European Association for the Study of Diabetes, Lisbon, Portugal, 12–16 September 2011.
The Department of Primary Care and Public Health at Imperial College is grateful for support from the NIHR Collaboration for Leadership in Applied Health Research and Care Scheme, the NIHR Biomedical Research Centre Scheme, and the Imperial Centre for Patient Safety and Service Quality.
References
- 1.Lampe FC, Morris RW, Walker M, Shaper AG, Whincup PH. Trends in rates of different forms of diagnosed coronary heart disease, 1978 to 2000: prospective, population based study of British men. BMJ 2005;330:1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kesteloot H, Sans S, Kromhout D. Dynamics of cardiovascular and all-cause mortality in Western and Eastern Europe between 1970 and 2000. Eur Heart J 2006;27:107–113 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. World health statistics 2009 [article online], 2009. Available from http://www.who.int/whosis/whostat/EN_WHS09_Full.pdf Accessed 10 December 2011
- 4.Unal B, Critchley JA, Capewell S. Explaining the decline in coronary heart disease mortality in England and Wales between 1981 and 2000. Circulation 2004;109:1101–1107 [DOI] [PubMed] [Google Scholar]
- 5.Booth GL, Kapral MK, Fung K, Tu JV. Recent trends in cardiovascular complications among men and women with and without diabetes. Diabetes Care 2006;29:32–37 [DOI] [PubMed] [Google Scholar]
- 6.Fox CS, Coady S, Sorlie PD, et al. Trends in cardiovascular complications of diabetes. JAMA 2004;292:2495–2499 [DOI] [PubMed] [Google Scholar]
- 7.Gu K, Cowie CC, Harris MI. Diabetes and decline in heart disease mortality in US adults. JAMA 1999;281:1291–1297 [DOI] [PubMed] [Google Scholar]
- 8.Gulliford MC, Charlton J. Is relative mortality of type 2 diabetes mellitus decreasing? Am J Epidemiol 2009;169:455–461 [DOI] [PubMed] [Google Scholar]
- 9.Jansson SP, Andersson DK, Svärdsudd K. Mortality trends in subjects with and without diabetes during 33 years of follow-up. Diabetes Care 2010;33:551–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Department of Health. Health survey for England 2006 [article online], 2007. Available from http://www.dh.gov.uk/en/publicationsandstatistics/publishedsurvey/healthsurveyforEngland/healthsurveyresults/index.htm Accessed 30 August 2011
- 11.O’Flaherty M, Ford E, Allender S, Scarborough P, Capewell S. Coronary heart disease trends in England and Wales from 1984 to 2004: concealed levelling of mortality rates among young adults. Heart 2008;94:178–181 [DOI] [PubMed] [Google Scholar]
- 12.Department of Health. The NHS plan: a plan for investment, a plan for reform [article online], 2000. Available from http://www.dh.gov.uk/en/publicationsandstatistics/publications/publicationspolicyandguidance/dh_4002960 Accessed 30 August 2011
- 13.Department of Health. The National Service Framework for Coronary Heart Disease: winning the war on heart disease [article online], 2004. Available from http://www.dh.gov.uk/en/publicationsandstatistics/publications/publicationspolicyandguidance/dh_4077154 Accessed 30 August 2011
- 14.The NHS Information Centre. Quality and outcomes framework: audits and performance [article online], 2011. Available from http://www.ic.nhs.uk/statistics-and-data-collections/audits-and-performance/the-quality-and-outcomes-framework Accessed 30 August 2011
- 15.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–383 [DOI] [PubMed] [Google Scholar]
- 16.Royal College of Paediatrics and Child Health. NHS Diabetes: growing up with diabetes: children and young people with diabetes in England [article online], 2009. Available from http://www.diabetes.org.uk/documents/reports/cyp_diabetes_survey_report.pdf Accessed 30 August 2011
- 17.Office for National Statistics (ONS). Publication hub: gateway to U.K. national statistics [Web site], 2011. Available from http://www.statistics.gov.uk Accessed 10 December 2011
- 18.Ford ES, Capewell S. Coronary heart disease mortality among young adults in the U.S. from 1980 through 2002: concealed leveling of mortality rates. J Am Coll Cardiol 2007;50:2128–2132 [DOI] [PubMed] [Google Scholar]
- 19.Bottle A, Millett C, Khunti K, Majeed A. Trends in cardiovascular admissions and procedures for people with and without diabetes in England, 1996-2005. Diabetologia 2009;52:74–80 [DOI] [PubMed] [Google Scholar]
- 20.Vamos EP, Bottle A, Majeed A, Millett C. Trends in lower extremity amputations in people with and without diabetes in England, 1996-2005. Diabetes Res Clin Pract 2010;87:275–282 [DOI] [PubMed] [Google Scholar]
- 21.Preis SR, Hwang SJ, Coady S, et al. Trends in all-cause and cardiovascular disease mortality among women and men with and without diabetes mellitus in the Framingham Heart Study, 1950 to 2005. Circulation 2009;119:1728–1735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Institute for Health and Excellence (NICE). Prevention of cardiovascular disease [article online], 2010. Available from http://guidance.nice.org.uk/phg/wave17/26 Accessed 30 August 2011
- 23.Thomas RJ, Palumbo PJ, Melton LJ, 3rd, et al. Trends in the mortality burden associated with diabetes mellitus: a population-based study in Rochester, Minn, 1970-1994. Arch Intern Med 2003;163:445–451 [DOI] [PubMed] [Google Scholar]
- 24.Alter DA, Khaykin Y, Austin PC, Tu JV, Hux JE. Processes and outcomes of care for diabetic acute myocardial infarction patients in Ontario: do physicians undertreat? Diabetes Care 2003;26:1427–1434 [DOI] [PubMed] [Google Scholar]
- 25.Brophy JM, Diodati JG, Bogaty P, Théroux P; Quebec Acute Coronary Care Working Group The delay to thrombolysis: an analysis of hospital and patient characteristics. CMAJ 1998;158:475–480 [PMC free article] [PubMed] [Google Scholar]
- 26.Redelmeier DA, Tan SH, Booth GL. The treatment of unrelated disorders in patients with chronic medical diseases. N Engl J Med 1998;338:1516–1520 [DOI] [PubMed] [Google Scholar]
- 27.Hamilton FL, Bottle A, Vamos EP, et al. Impact of a pay-for-performance incentive scheme on age, sex, and socioeconomic disparities in diabetes management in UK primary care. J Ambul Care Manage 2010;33:336–349 [DOI] [PubMed] [Google Scholar]
- 28.Millett C, Bottle A, Ng A, et al. Pay for performance and the quality of diabetes management in individuals with and without co-morbid medical conditions. J R Soc Med 2009;102:369–377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alshamsan R, Majeed A, Vamos EP, et al. Ethnic differences in diabetes management in patients with and without comorbid medical conditions: a cross-sectional study. Diabetes Care 2011;34:655–657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hassan A, Newman A, Ko DT, et al. Increasing rates of angioplasty versus bypass surgery in Canada, 1994-2005. Am Heart J 2010;160:958–965 [DOI] [PubMed] [Google Scholar]
- 31.Gerber Y, Rihal CS, Sundt TM, 3rd, et al. Coronary revascularization in the community. A population-based study, 1990 to 2004. J Am Coll Cardiol 2007;50:1223–1229 [DOI] [PubMed] [Google Scholar]
- 32.Silber S, Albertsson P, Avilés FF, et al. ; Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology Guidelines for percutaneous coronary interventions. Eur Heart J 2005;26:804–847 [DOI] [PubMed] [Google Scholar]
- 33.Thorvaldsen P, Kuulasmaa K, Rajakangas AM, Rastenyte D, Sarti C, Wilhelmsen L. Stroke trends in the WHO MONICA project. Stroke 1997;28:500–506 [DOI] [PubMed] [Google Scholar]
- 34.Rothwell PM, Coull AJ, Giles MF, et al. ; Oxford Vascular Study Change in stroke incidence, mortality, case-fatality, severity, and risk factors in Oxfordshire, UK from 1981 to 2004 (Oxford Vascular Study). Lancet 2004;363:1925–1933 [DOI] [PubMed] [Google Scholar]
- 35.Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol 2009;8:355–369 [DOI] [PubMed] [Google Scholar]
- 36.Campbell SE, Campbell MK, Grimshaw JM, Walker AE. A systematic review of discharge coding accuracy. J Public Health Med 2001;23:205–211 [DOI] [PubMed] [Google Scholar]
- 37.Vamos EP, Bottle A, Edmonds ME, Valabhji J, Majeed A, Millett C. Changes in the incidence of lower extremity amputations in individuals with and without diabetes in England between 2004 and 2008. Diabetes Care 2010;33:2592–2597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Audit Commission. Payment by results data assurance framework [article online], 2011. Available from http://www.audit-commission.gov.uk/health/audit/paymentbyresults/assuranceframework/pages/default.aspx Accessed 10 October 2011