Abstract
OBJECTIVE
To assess the individual financial impact of having diabetes in developing countries, whether diabetic individuals possess appropriate medications, and the extent to which health insurance may protect diabetic individuals by increasing medication possession or decreasing the risk of catastrophic spending.
RESEARCH DESIGN AND METHODS
Using 2002–2003 World Health Survey data (n = 121,051 individuals; 35 low- and middle-income countries), we examined possession of medications to treat diabetes and estimated the relationship between out-of-pocket medical spending (2005 international dollars), catastrophic medical spending, and diabetes. We assessed whether health insurance modified these relationships.
RESULTS
Diabetic individuals experience differentially higher out-of-pocket medical spending, particularly among individuals with high levels of spending (excess spending of $157 per year [95% CI 130–184] at the 95th percentile), and a greater chance of incurring catastrophic medical spending (17.8 vs. 13.9%; difference 3.9% [95% CI 0.2–7.7]) compared with otherwise similar individuals without diabetes. Diabetic individuals with insurance do not have significantly lower risks of catastrophic medical spending (18.6 vs. 17.7%; difference not significant), nor were they significantly more likely to possess diabetes medications (22.8 vs. 20.6%; difference not significant) than those who were otherwise similar but without insurance. These effects were more pronounced and significant in lower-income countries.
CONCLUSIONS
In low-income countries, despite insurance, diabetic individuals are more likely to experience catastrophic medical spending and often do not possess appropriate medications to treat diabetes. Research into why policies in these countries may not adequately protect people from catastrophic spending or enhance possession of critical medications is urgently needed.
High out-of-pocket medical spending comprises the overwhelming majority of medical spending in developing countries (1). It is associated with impoverishment and decreased spending on food (2,3). Previous studies from developing countries suggest that individuals with diabetes often delay seeking medical care until after they have developed complications, leading to high medical spending (4–6). This suggests underutilization of preventive therapies. Health insurance has been used in developed countries to increase the use of preventive health services and protect individuals against catastrophic risks (7). Given the dramatic increases in the prevalence of type 2 diabetes in many low- and middle-income countries (8), there is increased urgency to develop policies that address the health and financial risks from diabetes.
Information on patterns of medical spending and possession of medications to prevent complications among diabetic individuals in low- and middle-income countries is crucial for planning and policymaking. In addition to traditional medical and public health interventions, strategies that reduce costs and improve the availability of efficacious medications and simultaneously provide catastrophic risk protection via specific health insurance designs may be warranted. Although studies in India (9), South Africa (5), Brazil (10), and Tanzania (11) have examined spending by people with diabetes, no study has examined spending by diabetic individuals and access to medications that may prevent complications across a wide range of low- and middle-income countries and regions.
Our study uses data from 35 low- and middle-income countries included in the 2002–2003 World Health Survey (WHS) to address the following questions: 1) Do diabetic individuals have higher levels of medical spending and greater risks of catastrophic spending? 2) Do diabetic individuals possess diabetes medications? and 3) Do diabetic individuals with health insurance have either lower risks of catastrophic medical spending or higher rates of diabetes medication possession? Answers to these questions are relevant to high-level meetings organized by the United Nations that aim to galvanize country leaders to strengthen preventive care for noncommunicable diseases (12).
RESEARCH DESIGN AND METHODS
The 2002–2003 WHS, described previously (13–15), provides data on individuals from numerous low- and middle-income countries (as defined by the World Bank) (16). We restricted the analysis to respondents aged ≥18 years and to low- and middle-income countries that used the WHS long-form questionnaire (45 countries), because only these questionnaires included questions on self-reported diabetes diagnosis, health insurance status, medical spending, household spending, and indicators of household permanent income. Inclusion in the analyses was determined at the individual and country levels. Respondents were excluded if 1) they had incomplete responses to at least one of the questions used to construct variables for this analysis or 2) >90% of the respondents from their country did not report complete data on the variables of interest.
Ten countries were excluded because ≥90% of respondents were missing responses to at least one question of interest. Some countries failed to collect data on medical spending (three countries) and insurance status (one county) or did not report sampling weights (two countries). In two countries, <10% answered questions regarding health insurance status, and in two additional countries, no respondents had complete responses to all variables of interest. This reduced the original sample size from 235,988 (45 countries) to 210,118 (35 countries). For the remaining countries, 57.6% of 210,118 individuals had complete responses to all variables used in the analyses, leading to a final sample size of 121,051 respondents representing 422 million people (Supplementary Table 1).
Of 35 included countries, the median completeness of the response rate (complete response to all variables of interest) was 60% (interquartile range 38–81). Included countries with lower completeness of response rates (range below interquartile range 10–35) generally were either poorer African countries (Swaziland, Mali, Congo, and Senegal), or several countries from Eastern Europe (Georgia, Russia, and Kazakhstan), or one country from South America (Ecuador), with the majority of partial responders (89%) having missing responses to indicators of permanent income, health care spending, and/or smoking status. However, response rates to individual questions from the 35 included countries were high, ranging from 84% (percentage who responded to the question about diabetes) to 97% (percentage indicating their sex, urban/rural location, and age range).
Population characteristics
Characteristics of respondents included in the analysis and all respondents from the 35 included studies were estimated using robust SEs, clustered by country, and probability sampling weights. Using these methods, country-level summary measures were also estimated and reported graphically in order of ascending per capita gross domestic product (GDP) (expressed in purchasing power parity 2005 international dollars [I$]) (17).
Main outcomes
The main outcomes evaluated were 1) monthly medical expenditure per person, 2) catastrophic medical spending, and 3) possession of diabetes medications. Per-person medical expenditure, expressed in 2005 I$ (17), equaled the total self-reported household medical expenditure from the previous 4 weeks divided by the number of household members. All analyses were performed using reported monthly spending; however, for clarity, we report our results multiplied by 12 to approximate yearly spending.
Because there is no standard definition of catastrophic medical spending, we performed analyses using a variety of definitions consistent with previous studies: 1) household out-of-pocket medical spending ≥40% of capacity to pay (18) and 2) medical spending ≥10, 15, 20, 25, 30, 35, or 40% of total spending. Capacity to pay is defined as the income remaining after subsistence needs are met, adjusted for household size (18). Subsistence needs are country specific and are estimated by calculating the mean spending on food when 45–55% of total spending is spent on food (18). Because results were similar across definitions, we reported on catastrophic spending defined as ≥40% of a household’s capacity to pay in the main text, with results for the remaining definitions reported in the Supplemental Materials. Possession of diabetes medications was defined as whether, upon request during the in-home survey, the interviewee showed the interviewer a diabetes medication (e.g., insulin or metformin) (19).
Main predictors
The main predictor was a self-reported diagnosis of diabetes because the WHS did not test fasting plasma glucose. It previously has been shown that this measure is reasonably specific, although somewhat insensitive, because the diagnosis of diabetes requires clinic contact and testing (6,20–22).
The second predictor was health insurance status defined as whether the interviewee reported having health insurance. Participants were asked if they are covered by any type of health insurance plan. Few studies have examined the accuracy of self-reported health insurance in developing countries, although an analysis from Taiwan found self-reported insurance status to be a reasonable indicator of insurance status (23).
Covariates
All analyses included prespecified covariates thought to influence health spending, diagnosis of diabetes, or possessing diabetes medications: age (age decade), sex, urban/rural, years of schooling (none, 1–7, 8–12, or ≥13 years), smoker or nonsmoker, log of total household spending in the previous 4 weeks, and measures of permanent income. Measures of permanent income included various household characteristics and possessions: number of rooms, tables, and chairs in the house; number of cars owned; and presence of electricity, bicycles, clocks, buckets, dishwashers, refrigerators, fixed telephone lines, cell phones, televisions, and computers. To adjust for unobserved differences between countries, such as health system characteristics and preferences for health insurance, all regressions included country fixed effects.
Out-of-pocket medical spending, diabetes, and insurance
To assess the relationship between diabetes and out-of-pocket medical spending across the distribution of spending, we used quantile regressions (24,25). Predictors included self-reported diabetes, health insurance status, and an interaction term to assess whether the relationship between spending and being a diabetic individual with health insurance was different from that of uninsured diabetic individuals. We also included all prespecified covariates. Regressions were performed at the 40th, 50th, 60th, 70th, 75th, 80th, 90th, 95th, 97th, and 99th percentiles. By using quantile regression, no distributional assumptions regarding medical spending or its predictors were required.
Catastrophic medical spending, diabetes, and insurance
We assessed the relationship between diabetes, health insurance, and catastrophic medical spending using logistic regression. We again included an interaction between diabetes and insurance as well as the prespecified covariates and country fixed effects. To report results in a more interpretable format, we estimated the probability of catastrophic medical spending for people with and without diabetes and the absolute difference between the two groups based on the regressions. This difference is calculated by estimating the probability of catastrophic spending if all people in the sample had diabetes minus the probability of the outcome if all people in the sample did not have diabetes. Likewise, we assessed the relationship between health insurance and catastrophic medical spending among patients with diabetes using logistic regression and estimated the probability of these outcomes for people with and without insurance and the difference between these two groups.
Diabetes medication possession and insurance
We assessed the relationship between health insurance and possession of diabetes medications among diabetic individuals using logistic regression and included the interaction between diabetes and insurance as well as the prespecified covariates and country fixed effects. Again, we estimated the probability of diabetes medication possession for diabetic individuals with and without insurance and the absolute difference between the two groups. This difference is calculated by estimating the probability of medication possession if all diabetic individuals in the sample had insurance minus the probability of the outcome if all diabetic individuals in the sample did not have insurance.
We also examined whether relationships between the outcomes and predictors differed between low- and middle-income countries and between geographic regions by repeating the main analyses on catastrophic spending and medication possession among these groups. To stratify by country income, we ordered all included countries by GDP and then sequentially added each country to the low-income group until the number of people with diabetes in the low- and middle-income groups were approximately equal (Supplementary Table 1).
Sensitivity analyses
We assessed the possibility of bias attributed to an incomplete response to all variables of interest in three ways. First, we compared the characteristics of the included respondents with the characteristics of the total population responding to that question for 26 variables. Second, we removed each country one at a time from the analyses of catastrophic spending and medication possession to assess the influence of any one country on results. Finally, we repeated the analyses without indicators of permanent income, because these were frequently incomplete, on samples that included 1) complete responders to all variables included in the main analyses (n = 121,051) and 2) complete responders to all variables included in the main analyses except indicators of permanent income (n = 144,149).
Statistical methods
Analyses were undertaken using Stata/SE 11.1 for Windows (StataCorp, College Station, TX). Sampling weights, based on selection probability, nonresponse, and poststratification, were used to compute descriptive statistics and in all regression analyses. Robust SEs, clustered by country, were reported for the descriptive statistics and for the logistic regressions.
RESULTS
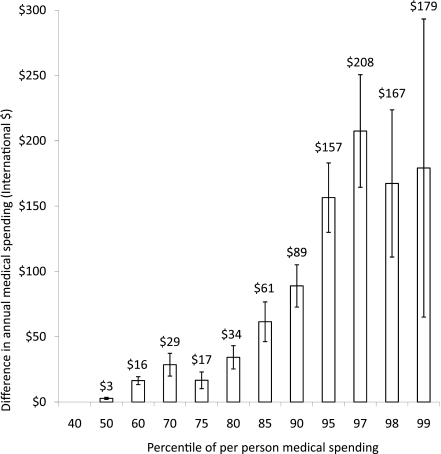
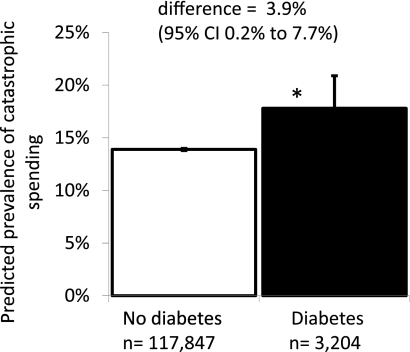
In this analysis of low- and middle-income countries, diabetic individuals were more likely to spend substantial amounts on their health, although they were relatively unlikely to possess diabetes medications. Health insurance was not significantly related to reduced risks of catastrophic medical spending for diabetic individuals or to increased diabetes medication possession. The out-of-pocket medical spending of diabetic individuals, compared with otherwise similar nondiabetic individuals, became differentially and substantially higher for those with high levels of medical spending after adjusting for other covariates and country fixed effects (Fig. 1) (at the 95th percentile: people with diabetes spend $157 per year more [95% CI 130–184] than those without diabetes). Diabetic individuals had a significantly higher predicted risk of catastrophic medical spending compared with otherwise similar people without diabetes (17.8 vs. 13.9%; difference 3.9% [95% CI 0.2–7.7]; P < 0.05) (Fig. 2). Insured diabetic individuals had a low predicted rate of medication possession that was not significantly higher than otherwise similar diabetic individuals without insurance (22.8 vs. 20.6%; difference 2.1% [−4.0–8.3]; P = 0.49).
Figure 1.
Differential medical spending among self-reported diabetic individuals vs. otherwise similar nondiabetic individuals. The graph shows that diabetic individuals have higher medical spending compared with otherwise similar nondiabetic individuals from the same country, particularly among individuals with high levels of medical spending (percentiles ≥95). Differentially high medical spending is statistically significant throughout. Annual medical spending was estimated by multiplying spending in the previous 4 weeks by 12. Medical spending is per-person medical spending, expressed in 2005 I$ (17).
Figure 2.
Diabetes status significantly associated with catastrophic medical spending. Catastrophic spending is defined as medical spending exceeding 40% of household capacity to pay (18). The prevalence of catastrophic spending is predicted based on adjustments for prespecified covariates and country fixed effects. Similar findings using alternate definitions (see Supplementary Table 4 for the difference in the predicted prevalence of catastrophic spending between people with and without diabetes using alternate definitions of catastrophic spending). *P < 0.05.
Country characteristics
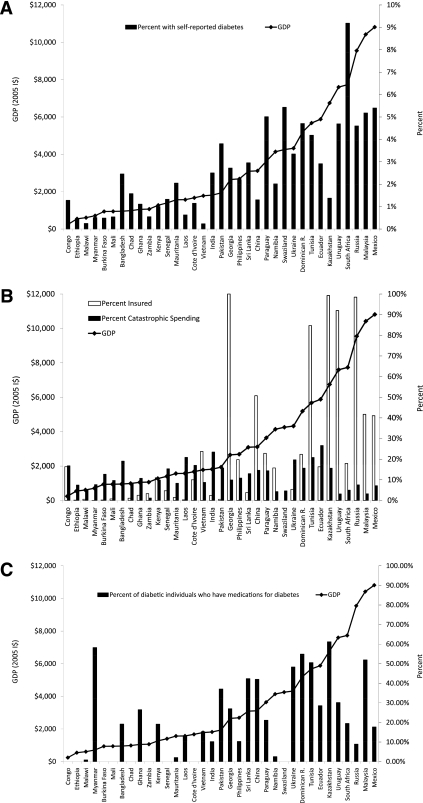
Almost 3% of respondents included in the analyses reported a diagnosis of diabetes (Table 1), ranging from 0.23% (Vietnam) to 9.18% (South Africa) (Fig. 3A). These prevalence estimates were not age standardized and did not adjust for underdiagnosis. The risk of catastrophic medical spending, or spending on medical care ≥40% of capacity to pay, was not uncommon across countries in the developing world (mean 14% [SE 2.5]), ranging from 1.7% (Zambia) to 26.6% (Ecuador) (Fig. 3B). Nearly 17% of included respondents reported some form of health insurance, ranging from 0% (Bangladesh and Swaziland) to 100% (Georgia). In most countries (71%), <30% of those with diabetes possessed diabetes medications (Fig. 3C).
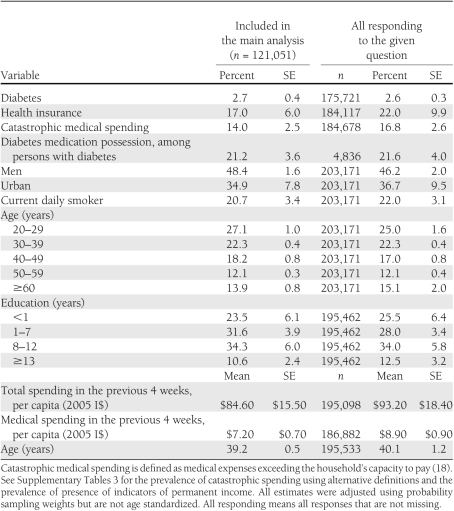
Table 1.
Characteristics of WHS respondents from 35 included countries
Figure 3.
Prevalence of diabetes, catastrophic spending, health insurance, and possession of diabetes medication by country. Countries are listed from left to right by ascending GDP (17). Rates are crude, adjusted only for probability sampling weights. A: Prevalence of diabetes. B: Prevalence of catastrophic spending and health insurance. C: Prevalence of possession of diabetes medications. USD, US dollars.
Respondent characteristics
A total of 48% of included respondents were men. Mean age was 39.2 years, 35.7% lived in urban areas, and 46% had at least 8 years of schooling. A total of 21% were current daily smokers (Table 1). A total of 17% of included respondents indicated that they were covered by health insurance. Compared with people without diabetes, those with diabetes were likely to be older, live in urban areas, have more schooling, have health insurance, and incur catastrophic medical spending (Supplementary Table 2). Respondents included in the analyses were similar to the overall population of respondents (Table 1; Supplementary Table 3).
Relationship of diabetes and insurance status to medical spending
Diabetic individuals in low- and middle-income countries had greater out-of-pocket medical expenses (Fig. 1) and higher predicted probability of catastrophic medical spending than otherwise similar people without diabetes (17.8 vs. 13.9%; difference 3.9% [95% CI 0.2–7.7]) (Fig. 2). Results were similar using the alternate definitions of catastrophic medical spending (difference ranging from 1.6% [medical spending ≥40% of total spending; P = 0.016] to 5.2% [medical spending ≥10% of total spending; P = 0.013]) (Supplementary Table 4). The differential in spending between diabetic individuals and otherwise similar nondiabetic individuals widens at higher levels of medical expenditure (Fig. 1). For example, at the median (50th percentile) diabetic individuals spend $3 (95% CI 2–4) more per year than otherwise similar nondiabetic individuals, whereas at the 95th percentile of spending, diabetic individuals spend $157 more (130–184). This is substantial compared with the per capita GDP of included countries, which ranged from $244 (Congo) to $10,815 (Mexico) (2005 I$) (17). Diabetic individuals with health insurance did not have a significantly lower risk of catastrophic spending compared with otherwise similar uninsured diabetic individuals (18.6 vs. 17.7%; difference 0.8% [95% CI −7.3 to 8.8]), even when using alternate definitions of catastrophic medical spending (difference ranged from −0.8% [medical spending ≥30% of total spending; P = 0.80] to 1.3% [medical spending ≥10% of total spending; P = 0.79]) (Supplementary Table 4).
Relationship of diabetes and insurance status to medication possession
Diabetes medication possession was not significantly higher among insured diabetic individuals than it was among uninsured diabetic individuals (22.8 vs. 20.6%; difference 2.1% [95% CI −4.0 to 8.3]), after adjusting for other covariates and country fixed effects. In 10 countries, all in sub-Saharan Africa, no diabetic individuals in our sample possessed medications to treat diabetes (Supplementary Table 1). Hence, these countries could not inform this analysis. These African countries had low rates of health insurance (Fig. 3B).
Analyses stratified by country per capita GDP and country geographic region
Among low-income countries, results were very similar to the main results. Diabetic individuals were more likely to have catastrophic spending compared with nondiabetic individuals (21.4 vs. 15.4%; P = 0.005). Insured individuals were not less likely to have catastrophic spending (16.2 vs. 15.5%; P = 0.496) and were no more likely to have pills to treat their condition (22.9 vs. 22.2%; P = 0.852) compared with the uninsured (Supplementary Table 5).
However, the pattern was different among the seven middle-income countries: diabetic individuals were no more likely to have catastrophic spending than nondiabetic individuals (6.7 vs. 7.6%; P = 0.691), and the overall prevalence of catastrophic spending was lower compared with the low-income countries. Insured individuals were significantly less likely to have catastrophic medical spending (7.1 vs. 8.1%; difference −1.01%; P = 0.025) and more likely to have diabetes medications than the uninsured (23.1 vs. 16.5%; difference 6.6%; P = 0.011) (Supplementary Table 5).
Likewise, in the analyses by geographic region, we found that in the Europe/Latin America region (with generally higher per capita income), insurance was associated with less catastrophic spending (difference −1.5%; P = 0.000) and greater possession of diabetes medications (difference 9.0%; P = 0.000), and the difference in spending between people with and without diabetes was not significant.
However, in countries where catastrophic spending is prevalent (countries in the Asia region with generally lower per capita GDP), insurance is not associated with less catastrophic spending or increased possession of medications, and diabetic individuals are more likely to suffer catastrophic medical spending than nondiabetic individuals (difference 7.2%; P = 0.002). The number of people in the sample with diabetes or health insurance in Africa was small (477 people with diabetes and 1,855 people with insurance), making drawing conclusions about this region difficult (Supplementary Table 5).
Sensitivity analyses
In general, we found that removal of individual countries did not change our main findings that diabetes is associated with a greater chance of catastrophic spending and that insurance is not associated with greater medication possession rates or lower rates of catastrophic spending (Supplementary Table 6). When we repeated the analyses without covariates relating to permanent income and included individuals who were excluded from the main analyses because of incomplete responses to questions about permanent income, we found that the main findings were unchanged (Supplementary Table 7).
CONCLUSIONS
In our analysis, diabetic individuals have greater out-of-pocket medical expenses and a higher risk of catastrophic medical spending compared with otherwise similar individuals without diabetes. Despite higher spending, relatively few diabetic individuals in these settings possess medications to manage their diabetes and prevent serious secondary complications. Health insurance was not significantly related to lower risks of catastrophic medical spending or to higher rates of medication possession for diabetic individuals. These findings were most pronounced among low-income countries. In middle-income countries, insurance was associated with protection from catastrophic spending and increased possession of medications for diabetes.
Our findings in low-income countries of low possession of diabetes medications despite high spending are consistent with patterns of care focusing on expensive treatment after secondary complications have occurred, consistent with previous findings (4). The long-term health implications of uncontrolled diabetes and its complications are of concern. In low- and middle-income countries, ischemic heart disease and stroke account for >25% of total disability-adjusted life-years (26); diabetes is a major risk factor for these disabling conditions. It has been estimated that 22% of all ischemic heart disease deaths and 14% of stroke deaths are attributable to high glucose in low- and middle-income countries, in addition to the deaths directly attributable to diabetes. These deaths generally occur at younger ages in low- and middle-income countries compared with high-income countries, increasing the loss of healthy life-years in these countries (27).
Our analyses have several limitations. First, our analyses were based on observational data; we could not conclude causality. Although we adjusted for income using measures of spending and other indicators of wealth, there may be other unobserved characteristics that account for why diabetic individuals have more catastrophic spending. We included country fixed effects to adjust for unobserved characteristics of countries that may affect individual choices to enroll in health insurance as well as covariates for health status, health risks, and preferences. However, it is possible that health plans in these settings with certain characteristics do provide risk protection and/or promote access to essential medications. For example, evidence from Colombia’s Régimen Subsidiado suggests that the program is providing risk protection and has increased the use of preventive services (28). Detailed data on the health insurance benefits in all countries included in our analysis are not available, although efforts are underway to document the scope of benefits included in national health programs (29). Additional research is needed to assess which policies are or are not successful in achieving stated goals and why some policies may be ineffective.
Second, results should be interpreted cautiously because of the level of incomplete responses in our sample. However, included respondents were similar on the observed characteristics to incomplete responders, and findings were unchanged when we no longer required complete reporting of indicators of permanent income.
Third, our main outcome of interest, self-reported medical spending over the previous 4 weeks, has not been validated as a measure of medical spending in low- and middle-income countries. If higher-income families tend to underreport medical spending and are more likely to be insured, lower spending among the insured could be attributed to this underreporting rather than to insurance status. Additional work is necessary to validate measures of out-of-pocket spending in low- and middle-income countries. Although there is not agreement in the literature on the definition of spending that makes spending “catastrophic,” we used two different definitions of catastrophic spending and six different thresholds of catastrophic spending. Main findings were similar when catastrophic spending was defined narrowly versus more broadly to include less severe levels of spending.
Finally, diabetes was determined by self-report and not by glucose measurement, leading to underestimation of the prevalence of diabetes in this sample. Rates of undiagnosed diabetes, especially in rural areas, may be as high as 70–80% (30). The low prevalence in our analyses may also be partly attributable to the relatively young population of adults in the sample because we reported rates adjusted for sampling weights not age-adjusted rates. The misclassification of people as not having diabetes may bias results toward the null if people with undiagnosed diabetes consume more medical care than people without diabetes, on average. For this reason, our estimate of the difference in spending between diabetic versus nondiabetic individuals may underestimate differences in spending. However, people with diagnosed diabetes may also be sicker than people with undiagnosed diabetes, biasing results toward larger differences in spending between people with and without diabetes. Hence, the net direction of bias is unclear. The exact magnitude of differences should be interpreted with caution, and we can only conclude that people with a self-reported diagnosis of diabetes have significantly greater medical spending than people without diabetes. However, if people with diabetes and major comorbidities are more likely to be diagnosed, our finding of relatively low prevalence of possession of diabetes medications in these potentially sicker individuals with diabetes is even more striking.
Reasons for lack of possession of essential medication are complex. Local pricing policies, inefficient drug procurement systems, transport costs, and regulatory, scientific, or technological manufacturing capabilities of low-income countries may all contribute to the low possession of essential medications (31,32). Effective financing and insurance schemes may only ameliorate some of these barriers to access.
A strength of this analysis is the use of individual data from a large international survey to assess spending using standardized questionnaires and field procedures that allow reasonable comparability across many low- and middle-income countries. Standardized information about health insurance status and disease and economic outcomes of interest, such as medical spending or use of medical services, are not readily available from other sources for large numbers of people in the developing world, although there is increasing need for such information.
Although our data were collected in 2002–2003, they are still likely relevant to the present situation. In most of the countries included in our analysis, large new programs to manage chronic diseases or to protect people from catastrophic spending have not been widely implemented in the last 10 years. For example, India and China have recently committed new public funds into health care programs for noncommunicable diseases (33), although implementation and scale-up are ongoing.
In our analysis, health insurance was not associated with a decrease in the probability of catastrophic medical spending nor was it associated with an increase in the probability of diabetic individuals having appropriate medications in the home, particularly in low-income countries. Additional research is needed to understand why policies in these settings may be ineffective and to understand which policies may be successful in improving risk protection and access to essential medications and services.
Supplementary Material
Acknowledgments
J.D.G.-F. was supported in part by a National Institute on Aging, National Institutes of Health, Career Development Award (K01-AG-037593-01A1) and was the principal investigator. C.M.S.-S. was supported in part by the Veterans Affairs Post-Residency Fellowship in Health Services Research and Development.
The Department of Veterans Affairs and the National Institutes of Health had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the manuscript for publication.
No potential conflicts of interest relevant to this article were reported.
C.M.S.-S. developed the study concept, developed the statistical model with input from J.B., analyzed health survey data and prepared results, and wrote the first draft of the manuscript. J.B. developed the study concept and provided critical review of the manuscript. J.D.G.-F. developed the study concept, developed the statistical model with input from J.B., and wrote the first draft of the manuscript. As the corresponding author and guarantor of this article, C.M.S.-S. takes full responsibility for the work as a whole, including the study design, access to data, and the decision to submit and publish the manuscript.
Parts of this study were presented in abstract form at the annual meeting of the Society of Medical Decision Making, Toronto, Canada, 24–27 October 2010.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc11-1770/-/DC1.
References
- 1.Pauly MV, Zweifel P, Scheffler RM, Preker AS, Bassett M. Private health insurance in developing countries. Health Aff (Millwood) 2006;25:369–379 [DOI] [PubMed] [Google Scholar]
- 2.Wagstaff A, Yu S. Do health sector reforms have their intended impacts? The World Bank’s Health VIII project in Gansu province, China. J Health Econ 2007;26:505–535 [DOI] [PubMed] [Google Scholar]
- 3.Wagstaff A. The economic consequences of health shocks: evidence from Vietnam. J Health Econ 2007;26:82–100 [DOI] [PubMed] [Google Scholar]
- 4.Goldhaber-Fiebert JD, Li H, Ratanawijitrasin S, et al. Inpatient treatment of diabetic patients in Asia: evidence from India, China, Thailand and Malaysia. Diabet Med 2010;27:101–108 [DOI] [PubMed] [Google Scholar]
- 5.Pepper DJ, Levitt NS, Cleary S, Burch VC. Hyperglycaemic emergency admissions to a secondary-level hospital: an unnecessary financial burden. S Afr Med J 2007;97:963–967 [PubMed] [Google Scholar]
- 6.Shobhana R, Rao PR, Lavanya A, Vijay V, Ramachandran A. Cost burden to diabetic patients with foot complications: a study from southern India. J Assoc Physicians India 2000;48:1147–1150 [PubMed] [Google Scholar]
- 7.Newhouse JP. Free for All? Lessons From the Rand Health Insurance Experiment. Cambridge, MA, Harvard University Press, 1993 [Google Scholar]
- 8.Danaei G, Finucane MM, Lu Y, et al. ; Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Glucose) National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet 2011;378:31–40 [DOI] [PubMed] [Google Scholar]
- 9.Ramachandran A, Ramachandran S, Snehalatha C, et al. Increasing expenditure on health care incurred by diabetic subjects in a developing country: a study from India. Diabetes Care 2007;30:252–256 [DOI] [PubMed] [Google Scholar]
- 10.Codogno JS, Fernandes RA, Sarti FM, Freitas Júnior IF, Monteiro HL. The burden of physical activity on type 2 diabetes public healthcare expenditures among adults: a retrospective study. BMC Public Health 2011;11:275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chale SS, Swai AB, Mujinja PG, McLarty DG. Must diabetes be a fatal disease in Africa? Study of costs of treatment. BMJ 1992;304:1215–1218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alwan AD, Galea G, Stuckler D. Development at risk: addressing noncommunicable diseases at the United Nations high-level meeting. Bull World Health Organ 2011;89:546–546A [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 2007;370:851–858 [DOI] [PubMed] [Google Scholar]
- 14.Ustun T, Chatterji S, Mechbal A. The World Health Surveys. In Health Systems Performance Assessment: Debates, Methods, and Empiricism. Murray C, Evans D, Eds. Geneva, World Health Org., 2003 [Google Scholar]
- 15.World Health Organization. World Health Survey: current status of the World Health Survey [article online], 2011. Available from http://www.who.int/healthinfo/survey/en/index.html Accessed 21 October 2009
- 16.The World Bank. How we classify countries [article online], 2011. Available from http://data.worldbank.org/about/country-classifications Accessed 9 December 2011
- 17.World Bank World Development Indicators. WDI online: database [Internet], 2011 Available from http://ddp-ext.worldbank.org/ext/DDPQQ/member.do?method=getMembers&userid=1&queryId=6 Accessed 10 August 2011
- 18.Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, Evans T. Protecting households from catastrophic health spending. Health Aff (Millwood) 2007;26:972–983 [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization. WHO model list of essential medicines: 12th List, April 2001 [article online], 2002. Available from http://apps.who.int/medicinedocs/en/d/Jh3003e/3.html Accessed 16 June 2011
- 20.El Fakiri F, Bruijnzeels MA, Hoes AW. No evidence for marked ethnic differences in accuracy of self-reported diabetes, hypertension, and hypercholesterolemia. J Clin Epidemiol 2007;60:1271–1279 [DOI] [PubMed] [Google Scholar]
- 21.Goldman N, Lin IF, Weinstein M, Lin YH. Evaluating the quality of self-reports of hypertension and diabetes. J Clin Epidemiol 2003;56:148–154 [DOI] [PubMed] [Google Scholar]
- 22.Wu SC, Li CY, Ke DS. The agreement between self-reporting and clinical diagnosis for selected medical conditions among the elderly in Taiwan. Public Health 2000;114:137–142 [DOI] [PubMed] [Google Scholar]
- 23.Yu ST, Chang HY, Lin MC, Lin YH. Agreement between self-reported and health insurance claims on utilization of health care: a population study. J Clin Epidemiol 2009;62:1316–1322 [DOI] [PubMed] [Google Scholar]
- 24.Cook BL, Manning WG. Measuring racial/ethnic disparities across the distribution of health care expenditures. Health Serv Res 2009;44:1603–1621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koenker R, Hallock KF. Quantile regression. J Econ Perspect 2001;15:143–156 [Google Scholar]
- 26.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 2006;367:1747–1757 [DOI] [PubMed] [Google Scholar]
- 27.Danaei G, Lawes CM, Vander Hoorn S, Murray CJ, Ezzati M. Global and regional mortality from ischaemic heart disease and stroke attributable to higher-than-optimum blood glucose concentration: comparative risk assessment. Lancet 2006;368:1651–1659 [DOI] [PubMed] [Google Scholar]
- 28.Miller G, Pinto D, Vera-Hernandez M. High-Powered Incentives in Developing Country Health Insurance: Evidence From Colombia's Regimen Subsidiado. Cambridge, MA, National Bureau of Economic Research, 2009. ([NBER working paper no. 15456]) [Google Scholar]
- 29.Hornberger J, Shewade A, Gutierrez H. How are coverage decisions made in publicly funded healthcare programs in low- and middle-income countries? Abstract presented at the 16th Annual International Meeting of the International Society for Pharmacoeconomics and Outcomes Research, 21–25 May 2011, at the Hilton Baltimore, Baltimore, Maryland. [Google Scholar]
- 30.Sadikot SM, Nigam A, Das S, et al. The burden of diabetes and impaired fasting glucose in India using the ADA 1997 criteria: prevalence of diabetes in India study (PODIS). Diabetes Res Clin Pract 2004;66:293–300 [DOI] [PubMed] [Google Scholar]
- 31.Lage A. Global pharmaceutical development and access: critical issues of ethics and equity. MEDICC Rev 2011;13:16–22 [DOI] [PubMed] [Google Scholar]
- 32.World Health Organization. Health systems financing: the path to universal coverage [article online], 2010. Available from http://www.who.int/whr/2010/en/index.html Accessed 27 October 2011 [DOI] [PMC free article] [PubMed]
- 33.Yip W, Mahal A. The health care systems of China and India: performance and future challenges. Health Aff (Millwood) 2008;27:921–932 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.