Abstract
OBJECTIVE
There is limited information on whether recent improvements in the control of cardiovascular disease (CVD) risk factors among individuals with diabetes have been concentrated in particular sociodemographic groups. This article estimates racial/ethnic- and education-related disparities and examines trends in uncontrolled CVD risk factors among adults with diabetes. The main racial/ethnic comparisons made are with African Americans versus non-Latino whites and Mexican Americans versus non-Latino whites.
RESEARCH DESIGN AND METHODS
The analysis samples include adults aged ≥20 years from the National Health and Nutrition Examination Survey (NHANES) 1988–1994 and the NHANES 1999–2008 who self-reported having diabetes (n = 1,065, NHANES 1988–1994; n = 1,872, NHANES 1999–2008). By use of logistic regression models, we examined the correlates of binary indicators measuring 1) high blood glucose, 2) high blood pressure, 3) high cholesterol, and 4) smoking.
RESULTS
Control of blood glucose, blood pressure, and cholesterol improved among individuals with diabetes between the NHANES 1988–1994 and the NHANES 1999–2008, but there was no change in smoking prevalence. In the NHANES 1999–2008, racial/ethnic minorities and individuals without some college education were more likely to have poorly controlled blood glucose compared with non-Latino whites and those with some college education. In addition, individuals with diabetes who had at least some college education were less likely to smoke and had better blood pressure control compared with individuals with diabetes without at least some college education.
CONCLUSIONS
Trends in CVD risk factors among individuals with diabetes improved over the past 2 decades, but racial/ethnic- and education-related disparities have emerged in some areas.
Diabetes is a leading cause of morbidity and mortality in the U.S., and the prevalence of this disease is rising (1). The Centers for Disease Control and Prevention, based on data from the National Health Interview Survey, estimated that the age-adjusted prevalence of diagnosed diabetes increased from 3.7% in 1980 to 7.7% in 2008 (2). The total direct and indirect costs associated with diabetes in the U.S. were estimated to be $174 billion in 2007, with ~33% ($58 billion) of the total cost being attributed to treatment of medical complications (3). Cardiovascular disease (CVD) is a widely documented potential complication of diabetes and a leading cause of mortality among individuals with diabetes (4–6). Although rates of CVD events have declined in recent decades among both individuals with and without diabetes, people with diabetes still are twice as likely as those without diabetes to experience a CVD event (4), and individuals with diabetes have heart disease mortality rates that are two to four times greater than those without diabetes (6).
To prevent CVD and other complications of diabetes, the American Diabetes Association (ADA) in 2009 published updated standards for diabetes screening, diagnosis, and therapeutic care (7). These guidelines, which reflect new evidence from epidemiological studies and randomized controlled trials, included targets for glycemic control, blood pressure control, lipid control, and smoking (7). The ADA recommends that most adults with diabetes maintain an HbA1c (a measure of blood glucose) level below or around 7.0%, blood pressure under 130/80 mmHg, and LDL cholesterol under 100 mg/dL (2.6 mmol/L) (7). All patients with diabetes are advised not to smoke. In addition, the National Cholesterol Education Program Adult Treatment Panel III recommends that individuals with diabetes keep their LDL under 100 mg/dL and total cholesterol under 200 mg/dL (8).
Given that successful management of diabetes requires a coordinated team of health care providers (7) and access to health insurance (9), continuity of care (10), and patient knowledge and self-management skills (11), there may be differences in control of CVD risk factors across sociodemographic groups within the population of people with diabetes. On the basis of data from the National Health and Nutrition Examination Survey (NHANES) 1999–2000, previous researchers reported that only 7.3% of those with diagnosed diabetes achieve all three of the ADA (2009) targets for control of blood glucose, blood pressure, and total cholesterol (12). Between the NHANES 1988–1994 and the NHANES 1999–2000, trends in the control of blood cholesterol among individuals with diagnosed diabetes improved, but there was no change in the control of blood glucose and blood pressure levels (12). Poor glycemic control generally is more prevalent among African Americans and Mexican Americans with diabetes compared with non-Latino whites with diabetes (13–15), but these differences have been small in some studies (13) and limited to certain sex/race-ethnicity subgroups in other studies (14). Recent research based on individuals with diabetes interviewed in the NHANES 1999–2008 shows an overall trend of improvement in CVD risk factors and, notably, reductions in the predicted 10-year risk of coronary heart disease (16), but some findings show that socioeconomic status and racial/ethnic disparities persist (14–18).
Using data from the NHANES 1988–1994 and the NHANES 1999–2008, we built on these important new results by 1) examining trends in the prevalence of diagnosed diabetes and the sociodemographic characteristics of the diagnosed diabetic population and 2) testing for racial/ethnic- and education-related disparities in poorly controlled risk factors for CVD among individuals with diagnosed diabetes. Given the mounting body of evidence showing the importance of controlling CVD risk factors (7) and the increasing focus on prevention in the 2010 health care reform law (19), it is critical to document current trends in the control of CVD risk factors among individuals with diabetes and to examine whether any improvements have been concentrated in particular sociodemographic groups.
RESEARCH DESIGN AND METHODS
Study population and analysis samples
We used two samples, a sample from the NHANES 1988–1994 and a sample from the NHANES 1999–2008. The NHANES used a stratified, multistage probability-sampling frame and represented the civilian, noninstitutionalized U.S. population. The NHANES 1988–1994 interviewed 18,825 individuals aged ≥20 years. We limited our NHANES 1988–1994 sample to 1,503 of these respondents who reported having been diagnosed with diabetes. In the NHANES 1999–2008, 26,246 individuals aged ≥20 years were interviewed, and we limited our NHANES 1999–2008 sample to 2,802 of these respondents who reported having been diagnosed with diabetes. Among those who reported having diabetes, we further limited NHANES 1988–1994 and NHANES 1999–2008 samples to those who had information regarding all four CVD risk factors (blood glucose, blood pressure, lipids, and current smoking). Blood glucose, blood pressure, and lipid information are available only for those NHANES respondents who participated in the medical examination portion of the survey, which included a blood draw. Smoking information was obtained from the interview.
These sample restrictions yielded 1,149 respondents in the NHANES 1988–1994 sample and 2,056 respondents in the NHANES 1999–2008 sample. After excluding respondents with missing sociodemographic characteristics used in the analysis, our final analysis samples included 1,065 respondents from the NHANES 1988–1994 and 1,872 respondents from the NHANES 1999–2008. The main racial/ethnic comparisons made were between African Americans versus non-Latino whites and Mexican-Americans versus non-Latino whites. Latinos from countries of origin other than Mexico are included in the “other” race/ethnicity category.
The age- and sex-adjusted proportion of respondents with nonmissing information on control of CVD risk factors decreased from 93.7% in the NHANES 1988–1994 to 81.1% in the NHANES 1999–2008. We tested for differences in observed characteristics between those included in the sample and those excluded from the sample because of missing data. In both the NHANES 1988–1994 and the NHANES 1999–2008, minority individuals were overrepresented among missing cases. In addition, in the NHANES 1999–2008, those with less than a high-school education were overrepresented among missing cases. When we ran a probit regression model with “missing from sample” as the dependent variable, we found that in both the NHANES 1988–1994 and in the NHANES 1999–2008, the only statistically significant predictor of being missing from the sample was African American race. We emphasize, however, that there is no statistically significant difference in the estimated coefficient on African American race in the NHANES 1988–1994 versus the NHANES 1999–2008, suggesting that the possible bias resulting from excluding observations with incomplete information is likely to be minimal.
Definitions and measures
We considered an individual to have diagnosed diabetes if he or she answered “yes” to the interview question, “Have you ever been told by a doctor or health professional that you have diabetes or sugar diabetes?” We did not consider respondents who reported having gestational diabetes to have diagnosed diabetes. When we estimated the prevalence rates of diagnosed diabetes, we used all respondents from the NHANES 1988–1994 and the NHANES 1999–2008 samples who provided a response to this question.
To define poor control of blood glucose and blood pressure, we followed the ADA 2009 guidelines. We defined poor glycemic control using a binary indicator of having an HbA1c ≥7%. To define poor blood pressure control, we used a binary indicator of having a systolic blood pressure ≥130 mmHg or diastolic blood pressure ≥80 mmHg. The NHANES 1988–1994 medical examination included three readings of systolic and diastolic blood pressure. For this sample, we used the average of the second and third readings. In the NHANES 1999–2008, three or four blood pressure readings were available for each respondent. Thus, for this sample, we used the average of the second and third readings when they were both available, and we used the average of the third and fourth measure or the average of the second and fourth measure of blood pressure in 193 case subjects for whom the second or third measure of blood pressure was missing and a fourth measure was available. We defined a dichotomous indicator of current smoking, which equaled 1 if a respondent reported “yes” to the question, “Have you smoked at least 100 cigarettes in your entire life?” and did not answer “not at all” to the question, “Do you now smoke cigarettes…” in the NHANES 1999–2008. In the NHANES 1988–1994, we defined a current smoker as someone who reported “yes” to both “Have you smoked at least 100 cigarettes during your entire life?” and “Do you smoke cigarettes now?”
To measure lipid control, we used the total cholesterol level, which follows the Adult Treatment Panel III guidelines, instead of LDL cholesterol, as suggested by the ADA in 2009, because of the small sample sizes with available LDL cholesterol information in the NHANES (n = 335 in the NHANES 1988–1994, n = 785 in the NHANES 1999–2008). The small sample sizes resulted from the LDL cholesterol measurement only being available for those who were assigned a NHANES medical examination scheduled in the morning. We used a binary indicator for total cholesterol of ≥200 mg/dL as an indicator for poor lipid control.
Analyses
Initially, we examined trends in the prevalence of diagnosed diabetes and the sociodemographic characteristics of the diagnosed diabetic populations in the NHANES 1988–1994 and the NHANES 1999–2008 samples. We reported age- and sex-adjusted as well as unadjusted prevalence rates of diagnosed diabetes (Table 1). Standardization was based on the 2000 U.S. Census population, using sex and age (5-year age categories for those aged 20–79 years and a category for those aged ≥80 years). We then examined sample characteristics of the population with diagnosed diabetes in the NHANES 1988–1994 and the NHANES 1999–2008 (Table 2) and, in Table 3, estimated the rates of poor control of CVD risk factors in the NHANES 1988–1994 and the NHANES 1999–2008 samples and by racial/ethnic and education groups. In Tables 2–3, the NHANES 1988–1994 percentages were standardized according to the NHANES 1999–2008 population of individuals with diagnosed diabetes, using age-sex groups and their corresponding weights (12). We compared the rates of poor control of CVD risk factors between the NHANES 1988–1994 and the NHANES 1999–2008 (Table 3) (20).
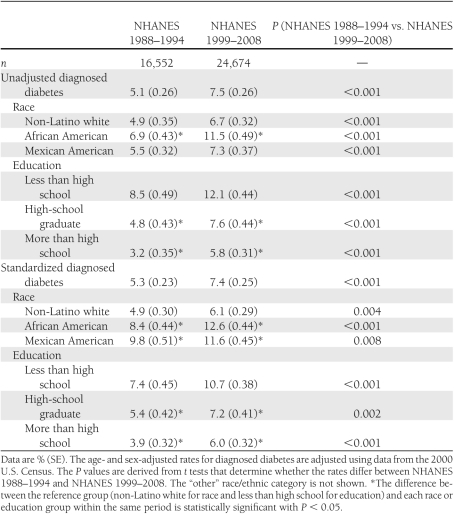
Table 1.
Prevalence rates of diagnosed diabetes among adults aged ≥20 years
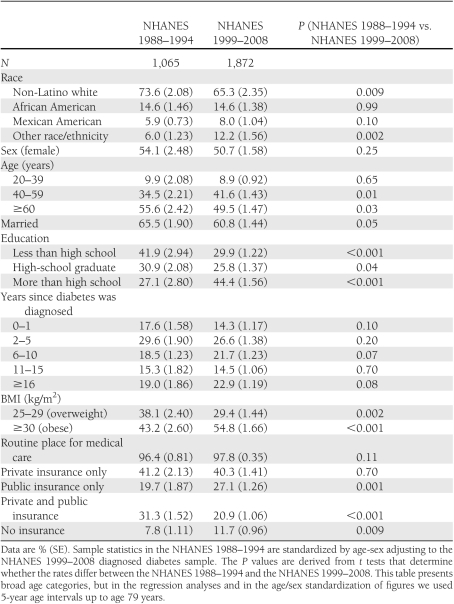
Table 2.
Sample characteristics of adults with diagnosed diabetes
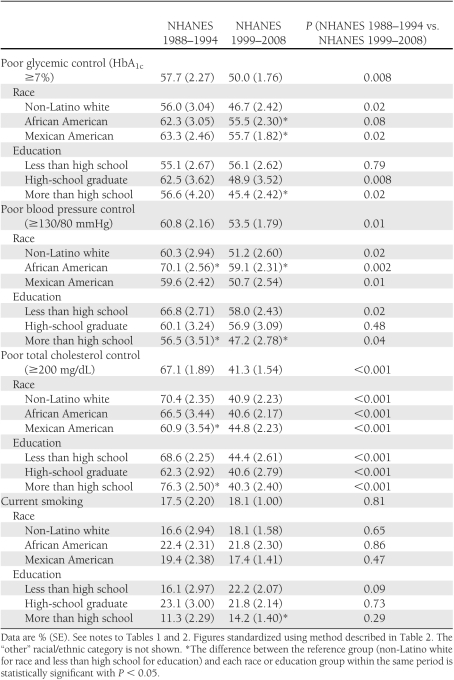
Table 3.
Poor control of risk factors among adults with diagnosed diabetes
We used logistic models estimated with survey weights to test for racial/ethnic- and education-related disparities in poorly controlled risk factors for CVD among individuals with diagnosed diabetes (Table 4). The models included controls for race/ethnicity (African American, Mexican American, other race/ethnicity versus non-Latino whites), age categories (5-year age categories for those aged 20–79 years and a category for those aged ≥80 years), sex (female vs. male), marital status (married vs. not married), years since diagnosis of diabetes (2–5, 6–10, 11–15, and ≥16 years vs. 0–1 years), obesity (BMI 25–29 kg/m2 [overweight], BMI ≥30 kg/m2 [obese] vs. BMI <25 kg/m2 [normal]), access to routine care (has routine access vs. does not have routine access), health insurance type (public, public and private, or uninsured vs. private only), and indicators for survey year. All analyses in this article were performed using Stata software, version 11.1 (StataCorp, College Station, TX).
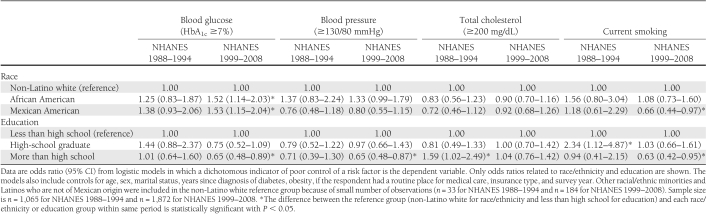
Table 4.
Poorly controlled CVD risk factors among adults with diagnosed diabetes in NHANES 1988–1994 and NHANES 1999–2008
RESULTS
Trends in diagnosed diabetes and characteristics of the population with diagnosed diabetes
As others have reported (2,21), the prevalence of diagnosed diabetes has increased appreciably over time (Table 1). The age- and sex-standardized prevalence rate of diagnosed diabetes in the NHANES 1999–2008 was 7.4%, whereas it was 5.3% in the NHANES 1988–1994 (P < 0.001). The unadjusted prevalence of diagnosed diabetes shows the same pattern, increasing from 5.1% in the NHANES 1988–1994 to 7.5% in the NHANES 1999–2008 (P < 0.001), which is consistent with previous research (22). Between the NHANES 1988–1994 and the NHANES 1999–2008, the incidence of diabetes (diagnosed and undiagnosed) increased from 7.9 to 10.1% (results not shown). We found that among those with diabetes (diagnosed and undiagnosed), the rate of undiagnosed diabetes decreased from 38.2 to 28.4% (results not shown), suggesting that diagnosis has improved over time.
One of the most significant changes in the characteristics of the population with diagnosed diabetes between the NHANES 1988–1994 and the NHANES 1999–2008 is the race/ethnicity distribution. Table 2 shows the increases over time in the proportions of Mexican Americans (from 5.9 to 8.0%, P = 0.10) and individuals from the “other” race/ethnicity group (from 6.0 to 12.2%, P = 0.002) in the population with diagnosed diabetes, whereas the proportion of non-Latino whites declined (from 73.6 to 65.3%, P = 0.009). For African Americans, there is no statistically significant change between the NHANES 1988–1994 and the NHANES 1999–2008 (Table 2).
The age distribution of the population with diagnosed diabetes also changed between the NHANES 1988–1994 and the NHANES 1999–2008 (Table 2). The proportion of middle-aged individuals increased over time (aged 40–59 years, from 34.5 to 41.6%, P = 0.01), whereas the proportion of elderly individuals declined (aged ≥60 years, from 55.6 to 49.5%, P = 0.03). This trend may have resulted from an earlier diagnosis of diabetes and/or an earlier onset of diabetes in recent years. In fact, we found that mean age at the time of diabetes diagnosis is higher in the NHANES 1988–1994 than in the NHANES 1999–2008 (aged 49.3 vs. 46.8 years, P < 0.001), and the number of years since diabetes was diagnosed was 9.1 years in the NHANES 1988–1994 versus 11.4 years in the NHANES 1999–2008 (P < 0.001).
In addition, the education profile of individuals with diagnosed diabetes changed remarkably between the NHANES 1988–1994 and the NHANES 1999–2008 (Table 2). The proportion of high-school dropouts among individuals with diagnosed diabetes decreased from 41.9 to 29.9% (P = 0.001), whereas the percentage with some postsecondary education increased from 27.1 to 44.4% (P < 0.001). To some extent, this change resulted from an increasing level of education in the population as a whole. Between the NHANES 1988–1994 and the NHANES 1999–2008, the age- and sex-standardized percentage of NHANES respondents aged ≥20 years with at least some postsecondary education rose from 27.1% in the NHANES 1988–1994 to 44.4% in the NHANES 1999–2008 (P < 0.001). Finally, the population with diagnosed diabetes has become more obese over time, with obesity levels increasing from 43.2% in the NHANES 1988–1994 to 54.8% in the NHANES 1999–2008 (P < 0.001). The percentage of people who were either obese or overweight also increased between the NHANES 1988–1994 (81.3%) and the NHANES 1999–2008 (84.2%).
Trends in poor control of CVD risk factors
Our findings suggest that control of CVD risk factors among individuals with diagnosed diabetes has improved markedly over the past two decades (Table 3). The percentage of those with diagnosed diabetes not achieving glycemic control (HbA1c >7%) was 50.0% in the NHANES 1999–2008, an improvement from the NHANES 1988–1994, when 57.7% of people with diagnosed diabetes did not meet this target (P = 0.008). The percentage of individuals with diagnosed diabetes who do not achieve blood pressure control (≥130/80 mmHg) decreased from 60.8% in the NHANES 1988–1994 to 53.5% in the NHANES 1999–2008 (P = 0.01). The percentage of people with diagnosed diabetes who did not have total cholesterol <200 mg/dL also significantly fell from 67.1% in the NHANES 1988–1994 to 41.3% in the NHANES 1999–2008. Rates of current smoking among individuals with diagnosed diabetes, however, did not change between the NHANES 1988–1994 (17.5%) and the NHANES 1999–2008 (18.1%, P = 0.81).
Of note, our analyses show a trend of improvement not only in the control of each risk factor individually but also in the number of controlled risk factors. In the NHANES 1988–1994, only 5.2% of those with diagnosed diabetes had control of all of the four risk factors we examined. In the NHANES 1999–2008, however, 13.6% of individuals with diagnosed diabetes had control of all four risk factors (P < 0.001) (results not shown). In addition, the percentage of people with diagnosed diabetes who had control of three of four risk factors increased from 24.1 to 31.0% (P = 0.003) between the NHANES 1988–1994 and the NHANES 1999–2008. Nevertheless, in the NHANES 1999–2008, more than one-half of the population with diagnosed diabetes (54.4%) still had more than two uncontrolled risk factors (results not shown).
Racial/ethnic- and education-related disparities in poor control of CVD risk factors
In the NHANES 1988–1994, there were no statistically significant racial/ethnic or education-related disparities in glycemic control among individuals with diagnosed diabetes, although some of the CIs were wide (Table 4, Blood glucose column). In the NHANES 1999–2008, however, we found that African Americans and Mexican Americans with diagnosed diabetes were ~50% more likely than non-Latino whites with diagnosed diabetes to be in poor glycemic control (African American vs. non-Mexican white: odds ratio 1.52 [95% CI 1.14–2.03]; Mexican vs. non-Mexican white: 1.53 [1.15–2.04]). Also, in the NHANES 1999–2008, we found that individuals with postsecondary education were less likely to be in poor glycemic control compared with those without postsecondary education (0.65 [0.48–0.89]). In summary, our results indicate that although glycemic control has improved in the population of individuals with diagnosed diabetes at large, these improvements may have been, to some extent, concentrated among non-Latino white and more-educated individuals, such that new health disparities have emerged.
These racial/ethnic- and education-related disparities in glycemic control persisted when we limited the sample to the most recent two waves of the NHANES (2005–2006 and 2007–2008) (results not shown). In these models, we tried including covariates that may have captured quality-of-care mechanisms of disparities, specifically whether the respondent had seen a diabetes specialist in the past year, whether the respondent usually saw a particular doctor for diabetes, and whether the respondent checked his or her own blood glucose level. These additional variables are available in the latest two waves of the NHANES only. After these covariates were included, both racial/ethnic-related disparities and education-related disparities were not changed appreciably, suggesting that these mechanisms (if they indeed were capturing quality of care) did not explain the disparities we observed in recent years. However, we interpreted these findings with caution because the additional covariates included may have captured the severity of disease instead of or in addition to quality of care. In that case, there may have been a reverse-causality problem, with poor control of diabetes driving severity instead of the other way around.
We did not find racial/ethnic differences in blood pressure control among individuals with diagnosed diabetes in either the NHANES 1988–1994 or the NHANES 1999–2008 (Table 4, Blood pressure column). Individuals with diagnosed diabetes who had some postsecondary education were less likely than those without postsecondary education to be in poor control of blood pressure, but this association was statistically significant only in the NHANES 1999–2008 data. There were no racial/ethnic disparities in total cholesterol control among individuals with diagnosed diabetes in either the NHANES 1988–1994 or the NHANES 1999–2008 (Table 4, Total cholesterol column). The association between postsecondary education and control of cholesterol approached statistical significance in the NHANES 1988–1994 but essentially disappeared by the NHANES 1999–2008. In the case of smoking, postsecondary education and Mexican American ethnicity were associated with a lower risk of smoking in the NHANES 1999–2008 (Table 4, Current smoking column; Mexican American vs. non-Latino whites: odds ratio 0.66 [95% CI = 0.44–0.97]; postsecondary education vs. no postsecondary education: 0.63 [0.42–0.95]). We did not find these odds ratios in the NHANES 1988–1994; surprisingly, having 12 years of education (compared with <12 years) is associated with a higher risk of smoking in the NHANES 1988–1994, although the CI is very wide for this estimate (Table 4, Current smoking column; 2.34 [1.12–4.87]).
The models in Table 4 focus on poor control of CVD risk factors only among individuals with diagnosed diabetes. Recent work shows education-related disparities in the likelihood of having undiagnosed diabetes in the NHANES 1999–2002 and African American vs. non-Latino white disparities in undiagnosed diabetes in the NHANES 1988–1994 (23). Thus, as a sensitivity check, we examined whether our results on disparities were affected if we considered undiagnosed cases. We reestimated all of the models in Table 4, including individuals with undiagnosed diabetes. The general pattern of findings was similar to those presented in Table 4. The only significant change was that including undiagnosed individuals in the blood pressure control models caused African American/non-Latino white disparities to grow somewhat larger, reaching statistical significance (results not shown).
CONCLUSIONS
In the newly released Healthy People 2020, three objectives in the area of diabetes are to improve glycemic, lipid, and blood pressure control among individuals with diagnosed disease (24). These objectives reflect mounting evidence that the control of these risk factors prevents CVD complications and mortality among people with diabetes (7,25,26). In addition, reducing smoking is a Healthy People 2020 objective for all adults. Our results show favorable trends in all of these areas except smoking rates. Between the NHANES 1988–1994 and the NHANES 1999–2008, the proportion of individuals with diagnosed diabetes with poor glycemic, blood pressure, and lipid control fell by 13, 12, and 38%, respectively. The prevalence of current smoking among individuals with diagnosed diabetes, however, remained stable during the time period we examined.
Our results suggest that, in some areas, improvements in the control of CVD risk factors seem to have benefitted all racial/ethnic and education groups. In the case of cholesterol levels, for example, all racial/ethnic and education groups experienced significant improvements in control between the NHANES 1988–1994 and the NHANES 1999–2008. In fact, we found no evidence of racial/ethnic- or education-related disparities in poor control of cholesterol in either the NHANES 1988–1994 or the NHANES 1999–2008. In addition, there were no racial/ethnic disparities in blood pressure control in the NHANES 1988–1994 or the NHANES 1999–2008.
However, in the case of glycemic control, improvements over time may have been driven by improvements among more educated individuals with diabetes and, to some extent, by improvements among non-Latino whites. Rates of poor glycemic control fell by 20% among those with >12 years of education between the NHANES 1988–1994 and the NHANES 1999–2008, but rates of glycemic control remained stable during this time period among those with less than a high-school education. Results from our regression analysis, which includes controls for a number of confounding factors, suggest that African Americans and Mexican Americans with diagnosed diabetes in the NHANES 1999–2008 were 50% more likely to have poor glycemic control than non-Latino whites with diagnosed diabetes.
Moreover, in the NHANES 1999–2008, individuals with diabetes who had at least some college education were less likely to have uncontrolled blood pressure than those without any college education, controlling for other factors. This association existed in the NHANES 1988–1994 as well, but it was not statistically significant. It also is notable that smoking rates among individuals with diagnosed diabetes have not improved over time and remain high in some subgroups; in the NHANES 1999–2008, 22% of individuals with diagnosed diabetes without a high-school education were current smokers. This high rate of smoking among the least educated individuals with diabetes is consistent with other data (27).
In summary, our findings show that important progress has been made in reducing CVD risk factors among individuals with diagnosed diabetes over the past decade, but this progress, in some cases, has been uneven across sociodemographic groups. There are several potential reasons why improvements in glycemic control may have been concentrated among non-Latino white and more educated populations. First, some groups may have better access than other groups to the type of integrated, comprehensive medical care that individuals with diabetes need in order to successfully manage their illness. Although we adjusted for insurance status and access to routine care in our main regression models, as well as experimented with models based on the latest two waves of the NHANES that included more extensive covariates, there still may exist unmeasured aspects of quality and access that are correlated with race/ethnicity and education. Second, individuals with diabetes who are more educated may have been better able to obtain and understand new information related to diabetes treatment compared with individuals with diabetes who are less educated. In our sample limited to the 2005–2008 NHANES, 44% of individuals with diagnosed diabetes with more than a high-school education reported that their doctor recommended that they maintain an HbA1c <7% (the recommended level), whereas only 12% of respondents with less than a high-school education reported that their doctors recommended this level. There also is evidence that people who are more educated adopt medical technologies more rapidly than people who are less educated (28). Third, culture and language may play a role in diabetes management practices, and these factors may underlie racial/ethnic disparities in outcomes (11).
Although the mechanisms through which sociodemographic characteristics affect control of CVD risk factors are unclear, our findings underscore the need to remediate these emerging racial/ethnic- and education-related disparities in this area of health care. Moreover, although our findings show marked improvements in the control of CVD risk factors among individuals with diabetes, it also is true that only a small group (13.6%) of individuals with diagnosed diabetes in the NHANES 1999–2008 had control of all four CVD risk factors we examined. Continued public health efforts need to be made to address the large majority of individuals with diagnosed diabetes with uncontrolled risk factors for CVD.
Acknowledgments
This research was supported by the National Institute on Minority Health and Health Disparities, National Institutes of Health (grant no. 1-P20-MD-003373).
No potential conflicts of interest relevant to this article were reported.
P.C., H.J., and K.L. contributed to the data analysis, interpretation of findings, and writing of the manuscript and are the guarantors of the article.
Parts of this study were presented at the AcademyHealth Annual Research Meeting, Seattle, Washington, 11–14 June 2001, and at the 139th Annual Meeting and Exposition of the American Public Health Association, Washington, DC, 29 October–2 November 2011.
Footnotes
The opinions expressed in this article are those of the authors and do not necessarily reflect the views of the National Institute on Minority Health and Health Disparities or the National Institutes of Health.
References
- 1.Engelgau MM, Geiss LS, Saaddine JB, et al. The evolving diabetes burden in the United States. Ann Intern Med 2004;140:945–950 [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Data and trends [article online], 2011. Available from http://www.cdc.gov/diabetes/statistics/prev/national/figageadult.htm Accessed 23 March 2011
- 3.American Diabetes Association Economic costs of diabetes in the U.S. In 2007. Diabetes Care 2008;31:596–615 [DOI] [PubMed] [Google Scholar]
- 4.Fox CS, Coady S, Sorlie PD, et al. Trends in cardiovascular complications of diabetes. JAMA 2004;292:2495–2499 [DOI] [PubMed] [Google Scholar]
- 5.Buse JB, Ginsberg HN, Bakris GL, et al. ; American Heart Association; American Diabetes Association Primary prevention of cardiovascular diseases in people with diabetes mellitus: a scientific statement from the American Heart Association and the American Diabetes Association. Circulation 2007;115:114–126 [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States, 2011. Atlanta, GA, U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2011 [Google Scholar]
- 7.American Diabetes Association Standards of medical care in diabetes: 2009. Diabetes Care 2009;32(Suppl. 1):S13–S61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Cholesterol Education Program Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Washington, DC, U.S. Govt. Printing Office, 2002. (NIH publ. no. 02-5215) [Google Scholar]
- 9.Zhang JX, Huang ES, Drum ML, et al. Insurance status and quality of diabetes care in community health centers. Am J Public Health 2009;99:742–747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mainous AG, 3rd, Koopman RJ, Gill JM, Baker R, Pearson WS. Relationship between continuity of care and diabetes control: evidence from the Third National Health and Nutrition Examination Survey. Am J Public Health 2004;94:66–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Two Feathers J, Kieffer EC, Palmisano G, et al. Racial and Ethnic Approaches to Community Health (REACH) Detroit partnership: improving diabetes-related outcomes among African American and Latino adults. Am J Public Health 2005;95:1552–1560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA 2004;291:335–342 [DOI] [PubMed] [Google Scholar]
- 13.Harris MI. Racial and ethnic differences in health care access and health outcomes for adults with type 2 diabetes. Diabetes Care 2001;24:454–459 [DOI] [PubMed] [Google Scholar]
- 14.Harris MI, Eastman RC, Cowie CC, Flegal KM, Eberhardt MS. Racial and ethnic differences in glycemic control of adults with type 2 diabetes. Diabetes Care 1999;22:403–408 [DOI] [PubMed] [Google Scholar]
- 15.Saydah S, Cowie C, Eberhardt MS, De Rekeneire N, Narayan KM. Race and ethnic differences in glycemic control among adults with diagnosed diabetes in the United States. Ethn Dis 2007;17:529–535 [PubMed] [Google Scholar]
- 16.Ford ES. Trends in the risk for coronary heart disease among adults with diagnosed diabetes in the U.S.: findings from the National Health and Nutrition Examination Survey, 1999-2008. Diabetes Care 2011;34:1337–1343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boltri JM, Okosun IS, Davis-Smith M, Vogel RL. Hemoglobin A1c levels in diagnosed and undiagnosed black, Hispanic, and white persons with diabetes: results from NHANES 1999-2000. Ethn Dis 2005;15:562–567 [PubMed] [Google Scholar]
- 18.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: U.S. trends from 1999 to 2006 and effects of Medicare coverage. Ann Intern Med 2009;150:505–515 [DOI] [PubMed] [Google Scholar]
- 19.The Henry J. Kaiser Family Foundation. Focus on health reform [article online], 2010. Available from http://www.kff.org/healthreform/upload/8061.pdf Accessed 23 March 2011
- 20.Heeringa SG, West BT, Berglund PA. Comparing means over time. In Applied Survey Data Analysis. Boca Raton, FL, Chapman & Hall/CRC Press, 2010, p. 143–144 [Google Scholar]
- 21.Gregg EW, Cheng YJ, Cadwell BL, et al. Secular trends in cardiovascular disease risk factors according to body mass index in US adults. JAMA 2005;293:1868–1874 [DOI] [PubMed] [Google Scholar]
- 22.Cowie CC, Rust KF, Ford ES, et al. Full accounting of diabetes and pre-diabetes in the U.S. population in 1988-1994 and 2005-2006. Diabetes Care 2009;32:287–294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smith JP. Nature and causes of trends in male diabetes prevalence, undiagnosed diabetes, and the socioeconomic status health gradient. Proc Natl Acad Sci USA 2007;104:13225–13231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.HealthyPeople 2020: 2020 topics and objectives. Available from http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicid=8 Accessed 23 March 2011
- 25.Stamler J, Vaccaro O, Neaton JD, Wentworth D. Diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care 1993;16:434–444 [DOI] [PubMed] [Google Scholar]
- 26.DECODE Study Group; European Diabetes Epidemiology Group Is the current definition for diabetes relevant to mortality risk from all causes and cardiovascular and noncardiovascular diseases? Diabetes Care 2003;26:688–696 [DOI] [PubMed] [Google Scholar]
- 27.Karter AJ, Stevens MR, Gregg EW, et al. Educational disparities in rates of smoking among diabetic adults: the Translating Research Into Action for Diabetes Study. Am J Public Health 2008;98:365–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lleras-Muney A, Lichtenberg FR. Are the more educated more likely to use new drugs? In Contributions in Memory of Zvi Griliches. Miresse J, Trajtenberg M, Eds. Malakoff, France, Annales D D'Économie et de Statistique, 2010, p. 671–696 [Google Scholar]