Abstract
The modified Hodge test has an excellent sensitivity for detecting enterobacterial isolates producing Ambler class A (KPC) and class D (OXA-48) carbapenemases. Its sensitivity is low for NDM-1 producers (50%) but is increased to 85.7% by adding ZnSO4 (100 μg/ml) in the culture medium. However, this test has a low specificity and is time-consuming.
TEXT
Carbapenemase producers are increasingly reported worldwide in Enterobacteriaceae. Their identification is of primary importance since carbapenemase producers are resistant not only to most (if not all) β-lactams but also to other main classes of antibiotics. Mostly, three types of carbapenemases are now commonly identified in Enterobacteriaceae. They are the Ambler class A of the KPC type, class B of the NDM-1, IMP, and VIM types, and class D of the OXA-48 type (1, 14, 15, 20, 23). Many techniques can be used for detecting production of carbapenemases, from phenotypic to advanced molecular-based techniques (13). The cloverleaf technique, or modified Hodge test (MHT), has been extensively used as a phenotypic technique for detecting carbapenemase activity (12, 13, www.cdc.gov/ncidod/dhqp/pdf/ar/HodgeTest_Carbapenemase_Enterobacteriaceae.pdf) since it is available in clinical microbiology routine settings and recommended by the CLSI (5). It is based on the inactivation of a carbapenem by carbapenemase-producing strains that enables a carbapenem-susceptible indicator strain to extend growth toward a carbapenem-containing disk, along the streak of inoculum of the tested strain.
Since the value of MHT for detecting the currently widespread carbapenemase producers (KPC, NDM-1, OXA-48) has been poorly documented, we have initiated a study using a collection of carbapenemase and noncarbapenemase producers with well-characterized mechanisms of resistance. Enterobacterial isolates included in our study were either resistant or of reduced susceptibility to ertapenem, according to the updated breakpoints of the CLSI guidelines (i.e., with a MIC of ertapenem of ≥0.5 μg/ml) (5) (Table 1). The isolates produced either Ambler class A (KPC-2), class B (NDM-1, VIM-1, IMP-1), or class D (OXA-48) carbapenemases. Noncarbapenemase producers were AmpC overproducers with permeability defect or clavulanic-acid inhibited extended-spectrum β-lactamase (ESBL) producers (mostly of the CTX-M type) with permeability defect (Table 1). Ertapenem (10 μg disk, Bio-Rad, Marnes-la-Coquette, France) and indicator strains Escherichia coli JM109 (Promega, Charbonnières-Les-Bains, France) and E. coli ATCC 25922 were used.
Table 1.
Influence of ZnSO4 in Mueller-Hinton agar (MHA) on the modified Hodge test for 54 carbapenemase- and/or ESBL/AmpC-producing enterobacterial isolates
| Strain | β-Lactamase(s) | MIC (μg/ml) of druga: |
Modified Hodge test result for ETP |
Reference | |||
|---|---|---|---|---|---|---|---|
| IMP | ETP | MP | MHA | MHA + ZnSO4 | |||
| Class A carbapenemases | |||||||
| E. cloacae CFVL | KPC-2 + TEM-3 | 4 | 2 | 1 | + | + | 2 |
| E. coli DIN | KPC-2 + TEM-1 + OXA-1 | 1 | >32 | 2 | + | + | 2 |
| E. coli PSP | KPC-2 + TEM-1 + OXA-1 | 0.5 | 0.5 | 0.5 | + | + | 2 |
| E. coli COL | KPC-2 + TEM-1 + CTX-M-9 | 4 | 4 | 2 | + | + | This study |
| K. pneumoniae COL | KPC-2 + TEM-1 + SHV-1 + CTXM-15 | 4 | 4 | 2 | + | + | This study |
| K. pneumoniae KAM | KPC-3 + TEM-1 | 8 | 12 | 2 | + | + | This study |
| Class B carbapenemases | |||||||
| K. pneumoniae UK | NDM-1 + CTX-M-15 + CMY-4 + OXA-1 | >32 | >32 | >32 | + | + | 15 |
| K. pneumoniae 6759 GEN | NDM-1 + TEM-1 + SHV-11 + CTX-M-15 + CMY-16 + OXA-1 + OXA-9 + OXA-10 | 12 | >32 | >32 | + | + | 21 |
| K. pneumoniae 2OMA | NDM-1 + OXA-1 + SHV-11 | 1.5 | 6 | 2 | + | + | 15 |
| K. pneumoniae IND | NDM-1 + TEM-1 + SHV-28 + CTX-M-15 + CMY-6 + OXA-1 + OXA-9 | 1 | 8 | 4 | − | + | This study |
| K. pneumoniae 1OMA | NDM-1 + TEM-1 + SHV-11 + SHV-28 + CTX-M-15 + OXA-1 + OXA-9 | >32 | >32 | >32 | + | + | 15 |
| K. pneumoniae 7AFR | NDM-1 + TEM-1 + SHV-28 + CTX-M-15 + CMY-6 + OXA-1 | >32 | >32 | >32 | − | + | 15 |
| E. coli 5649 GEN | NDM-1 + OXA-1 + CMY-30 + TEM-1 | 8 | >32 | 12 | − | + | 21 |
| E. coli RIC | NDM-1 + TEM-1 + OXA-1 + OXA-10 + CMY-16 | 1 | 3 | 1 | − | + | This study |
| E. coli GUE | NDM-1 + TEM-1 + OXA-1 | 3 | 3 | 2 | − | − | 15 |
| E. coli 271 AUS | NDM-1 + TEM-1 + CTX-M-15 | 6 | 32 | 16 | + | + | 19 |
| E. coli ALL | NDM-1 + TEM-1 + OXA-1 + OXA-2 + CTX-M-15 | 4 | >32 | 8 | − | − | 16 |
| E. coli IR5 TW | NDM-1 + TEM-1 + CTX-M-15 | 16 | >32 | 16 | NDd | +/ND | 15 |
| E. cloacae IR38 | NDM-1 + CTX-M-15 | 2 | 16 | 2 | + | + | 15 |
| P. stuartii PS1 | NDM-1 + TEM-1 + OXA-1 + CMY-6 | 12 | 0.38 | 1.5 | − | + | 18 |
| E. coli MAD | VIM-1 + CTX-M-3 | 1.5 | 0.38 | 0.5 | + | + | 2 |
| K. pneumoniae MAD | VIM-1 + CTX-M-3 | 1 | 0.5 | 1 | ND | ND | 2 |
| K. pneumoniae DIH | VIM-19 + TEM-1 + SHV-1 + CTX-M-3 | 8 | 16 | 4 | ND | +/ND | This study |
| E. coli JAP | IMP-1 | 0.5 | 3 | 0.5 | + | + | 2 |
| K. pneumoniae TUR | IMP-1 + SHV-5 | 1 | 2 | 8 | ND | ND | 2 |
| Class D carbapenemases | |||||||
| K. pneumoniae BIC | OXA-48 | 0.5 | 2 | 0.5 | + | + | 2 |
| K. pneumoniae BEL | OXA-48 | 1 | 4 | 1 | + | + | 2 |
| K. pneumoniae LIB | OXA-48 | >16 | >16 | >16 | + | + | 2 |
| K. pneumoniae CHA | OXA-48 + TEM-1 | 0.38 | 1 | 0.5 | + | + | This study |
| K. pneumoniae EGY | OXA-48 + CTX-M-15 | 2 | 3 | 2 | + | + | 2 |
| E. cloacae TUR | OXA-48 + SHV-5 | 0.5 | 0.5 | 0.5 | + | + | 2 |
| E. coli HAN | OXA-48 + CTX-M-15 | 3 | 16 | 1 | + | + | This study |
| E. coli BOU | OXA-48 + CTX-M-15 | 0.5 | 0.75 | 0.125 | + | + | This study |
| E. coli BER | OXA-48 + CTX-M-15 | 0.38 | 1.5 | 0.19 | + | + | This study |
| E. coli AME | OXA-48 + TEM-1 + CTX-M-24 | 0.25 | 0.5 | 0.19 | + | + | 17 |
| AmpC ± reduced permeability | |||||||
| P. mirabilis PMA | ACC-1 | 0.25 | 0.12 | 0.12 | Weak positive | Weak positive | 9 |
| E. coli ECA | ACC-1 | 0.12 | 0.12 | 0.12 | Weak positive | Weak positive | 9 |
| K. pneumoniae KDH | DHA-2 | 0.12 | 0.5 | 0.12 | Weak positive | Weak positive | 8 |
| E. coli MET | ESAC | 0.12 | 0.12 | 0.12 | ND | ND | This study |
| E. coli Ec13 SYD | CMY-2 | 0.12 | 0.12 | 0.12 | ND | ND | This study |
| E. coli MARb | AmpC | 16 | >32 | 2 | − | − | This study |
| E. cloacae BLAb | AmpC | 0.12 | 1 | 0.12 | − | − | This study |
| E. cloacae CONb | AmpC | 0.12 | 1 | 0.12 | + | + | This study |
| E. cloacae AZAb | AmpC | 0.5 | 1 | 0.12 | + | + | This study |
| E. cloacae POGb | AmpC | 4 | 1.5 | 2 | + | + | This study |
| ESBL ± reduced permeability | |||||||
| K. pneumoniae COOc | CTX-M-15 + SHV28 | 4 | >32 | 4 | − | − | This study |
| K. pneumoniae BERc | TEM-1 + SHV-28 | 1 | 4 | 1 | − | − | This study |
| K. pneumoniae 648236c | SHV-2a | 0.25 | 2 | 0.38 | Weak positive | − | This study |
| K. pneumoniae MEKc | CTX-M-15 + SHV-11 | 1.5 | >32 | 6 | Weak positive | − | This study |
| K. pneumoniae SIMc | CTX-M-15 + TEM-1 + SHV-1 | 3 | >32 | 3 | − | − | This study |
| K. pneumoniae BEDc | CTX-M-15 + TEM-1 + SHV-1 | 1.5 | >32 | 4 | Weak positive | Weak positive | This study |
| K. pneumoniae SHMc | CTX-M-15 + TEM-1 + SHV-11 | 3 | >32 | 1 | − | Weak positive | This study |
| K. pneumoniae FOSc | CTX-M-15 + TEM-1 + SHV-11 | 6 | >32 | >32 | + | Weak positive | This study |
| K. pneumoniae LEGc | CTX-M-15 + TEM-1 + SHV-12 | 0.75 | >32 | 3 | − | − | This study |
Abbreviations: IMP, imipenem; ETP, ertapenem; MP, meropenem.
Reduced susceptibility to ertapenem due to overexpressed AmpC.
Reduced susceptibility to ertapenem due to porin deficiency.
ND, not determinable, due to inhibition of growth of the E. coli JM109 strain along the tested isolate.
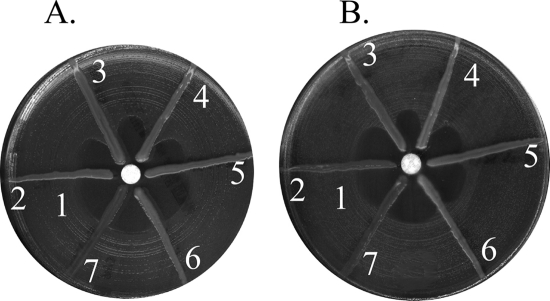
Among the 35 carbapenemase producers, 24 gave positive results, 7 gave negative results, and 4 gave noninterpretable results (Table 1). Class A and class D carbapenemase producers were detected by the MHT. False-negative results were obtained for 7 out of 14 NDM-1 producing Enterobacteriaceae (Table 1; Fig. 1A), which is in accordance with what had been previously observed for NDM-1 producers (4). The overall sensitivity and specificity of the MHT was low (77.4% and 38.9%, respectively). Those noninterpretable results could correspond to isolates producing a substance, such as colicin, that may inhibit the growth of E. coli JM109 (Table 1). False detection of carbapenemase production was observed for 11 out of 20 isolates (Table 1). This result was in accordance with those from previous studies (3, 10, 13, 22).
Fig 1.
MHT on MHA (A) and on MHA added with zinc sulfate (100 μg/ml) (B). Organisms tested: 1, E. coli JM109; 2, K. pneumoniae COO (CTX-M-15 + porin loss); 3, K. pneumoniae BIC (OXA-48); 4, K. pneumoniae POZ (KPC-2); 5, E. coli GEN (NDM-1); 6, E. coli RIC (NDM-1); 7, E. coli ALL (NDM-1). Zinc sulfate improved the MHT for E. coli RIC and not for E. coli ALL.
Taking into account the high rate of false negatives among NDM producers, we tried to modify this MHT technique for improving its detection limits. Although Lee et al. suggested that a bile compound contained in MacConkey agar may improve the sensitivity of the MHT for detecting metallo-β-lactamase (MBL) producers (11), we did not observe changes in the sensitivity detection of the NDM producers by using this medium (data not shown). As MBLs are zinc dependent (23), zinc sulfate was added to Mueller-Hinton agar (MHA) (BBL, Le Pont-de-Claix, France) at different concentrations (from 25 to 100 μg/ml). Previous studies showed that commercially available MHA media contained concentrations of zinc varying from 1- to 15-fold, depending on the manufacturer (7). Cooper et al. determined zinc concentration as being 2.61 μg/ml in MHA from BBL in 1993 (7). The addition of 100 μg/ml of zinc sulfate inhibited partially the growth of E. coli ATCC 25922, giving rise to difficult interpretations of the MHT. E. coli JM109 was then used instead of E. coli ATCC 25922 because growth of E. coli JM109 was homogeneous on ZnSO4-containing agar. The addition of zinc sulfate improved test sensitivity for 5 of the 7 false-negative results obtained with NDM producers using non-zinc-supplemented MHA (Table 1; Fig. 1). Notably, two false-negative NDM-producing E. coli isolates remained negative despite the addition of zinc sulfate (Table 1; Fig. 1B). As suggested for detection of the IMP- or VIM-producing Pseudomonas aeruginosa and Acinetobacter sp. (12), zinc addition improved the sensitivity of the MHT (from 77.4 to 94%), in particular with NDM-1-producing Enterobacteriaceae (Table 1). The effect of zinc might be multiplied by increasing the stability of the enzyme and/or by modifying porin expression (6). The addition of zinc sulfate did not modify the specificity of the test (38.9% with or without zinc sulfate).
This study showed that the MHT technique is highly sensitive for detecting class A, B, and D carbapenemases after addition of zinc in the culture medium. However, the limitations of the MHT in terms of clinical performance remain its lack of specificity and the delay in obtaining the results (24 to 48 h) after isolation of a bacterial colony.
ACKNOWLEDGMENTS
This work was funded by a grant from the INSERM (U914) and from the Ministère de l'Education Nationale et de la Recherche (UPRES-EA 3539), Université Paris XI, Paris, France, and mostly by grants from the European Community (TEMPOtest-QC, HEALTH-2009-241742).
We report no conflict of interest.
Footnotes
Published ahead of print 23 November 2011
REFERENCES
- 1. Ambler RP, et al. 1991. A standard numbering scheme for the class A β-lactamases. Biochem. J. 276: 269– 272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Carrër A, Fortineau N, Nordmann P. 2010. Use of ChromID extended-spectrum β-lactamase medium for detecting carbapenemase-producing Enterobacteriaceae. J. Clin. Microbiol. 48: 1913– 1914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Carvalhaes CG, Picao R, Nicoletti AG, Xavier DE, Gales AC. 2010. Cloverleaf test (modified Hodge test) for detecting carbapenemase production in Klebsiella pneumoniae: be aware of false positive results. J. Antimicrob. Chemother. 65: 249– 251 [DOI] [PubMed] [Google Scholar]
- 4. Castanheira M, et al. 2011. Early dissemination of NDM-1- and OXA-181-producing Enterobacteriaceae in Indian hospitals: report from the SENTRY Antimicrobial Surveillance Program, 2006–2007. Antimicrob. Agents Chemother. 55: 1274– 1278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Clinical Laboratory Standards Institute 2011. Performance standards for antimicrobial susceptibility testing: nineteenth informational supplement M100–S21. CLSI, Wayne, PA [Google Scholar]
- 6.Conejo MC, Garcia I, Martinez-Martinez L, Picabea L, Pascual A. 2003. Zinc eluted from siliconed latex urinary catheters decreases OprD expression, causing carbapenem resistance in Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 47: 2313– 2315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cooper GL, et al. 1993. Influence of zinc on Pseudomonas aeruginosa susceptibilities to imipenem. J. Clin. Microbiol. 31: 2366– 2370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fortineau N, Poirel L, Nordmann PP. 2001. Plasmid-mediated and inducible cephalosporinase DHA-2 from Klebsiella pneumoniae. J. Antimicrob. Chemother. 47: 207– 210 [DOI] [PubMed] [Google Scholar]
- 9. Girlich D, Karim A, Spicq C, Nordmann P. 2000. Plasmid-mediated cephalosporinase ACC-1 in clinical isolates of Proteus mirabilis and Escherichia coli. Eur. J. Clin. Microbiol. Infect. Dis. 19: 893– 895 [DOI] [PubMed] [Google Scholar]
- 10. Giske CG, et al. 2011. A sensitive and specific phenotypic assay for detection of metallo-β-lactamases and KPC in Klebsiella pneumoniae with the use of meropenem disks supplemented with aminophenylboronic acid, dipicolinic acid and cloxacillin. Clin. Microbiol. Infect. 17: 552– 556 [DOI] [PubMed] [Google Scholar]
- 11. Lee K, et al. 2010. Improved performance of the modified Hodge test with MacConkey agar for screening carbapenemase-producing Gram-negative bacilli. J. Microbiol. Methods 83: 149– 152 [DOI] [PubMed] [Google Scholar]
- 12. Lee K, Lim YS, Yong D, Yum JH, Chong Y. 2003. Evaluation of the Hodge test and the imipenem-EDTA double-disk synergy test for differentiating metallo-β-lactamase-producing isolates of Pseudomonas spp. and Acinetobacter spp. J. Clin. Microbiol. 10: 4623– 4629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Miriagou V, et al. 2010. Acquired carbapenemases in Gram-negative bacterial pathogens: detection and surveillance issues. Clin. Microbiol. Infect. 16: 112– 122 [DOI] [PubMed] [Google Scholar]
- 14. Nordmann P, Naas T, Poirel L. 2011. Global spread of carbapenemase-producing Enterobacteriaceae. Emerg. Infect. Dis. 17: 1791– 1798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nordmann P, Poirel L, Carrër A, Toleman MA, Walsh TR. 2011. How to detect NDM-1 producers. J. Clin. Microbiol. 49: 718– 721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pfeifer Y, et al. 2011. NDM-1-producing Escherichia coli in Germany. Antimicrob. Agents Chemother. 55: 1318– 1319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Poirel L, et al. 2011. Emergence of OXA-48-producing Escherichia coli clone ST38 in France. Antimicrob. Agents Chemother. 55: 4937– 4938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Poirel L, Dortet L, Bernabeu S, Nordmann P. 2011. Genetic features of blaNDM-1-positive Enterobacteriaceae. Antimicrob. Agents Chemother. 55: 5403– 5407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Poirel L, Lagrutta E, Taylor P, Pham J, Nordmann P. 2010. Emergence of metallo-β-lactamase NDM-1-producing multidrug-resistant Escherichia coli in Australia. Antimicrob. Agents Chemother. 54: 4914– 4916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Poirel L, Naas T, Nordmann P. 2010. Diversity, epidemiology and genetics of class D β-lactamases. Antimicrob. Agents Chemother. 54: 24– 38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Poirel L, et al. 2011. Molecular analysis of NDM-1-producing enterobacterial isolates from Geneva, Switzerland. J. Antimicrob. Chemother. 66: 1730– 1733 [DOI] [PubMed] [Google Scholar]
- 22. Seah C, Low DE, Patel SN, Melano RG. 2011. Comparative evaluation of a chromogenic agar medium, the modified Hodge test, and a battery of meropenem-inhibitor discs for detection of carbapenemase activity in Enterobacteriaceae. J. Clin. Microbiol. 49: 1965– 1969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Walsh TR, Toleman MA, Poirel L, Nordmann P. 2005. Metallo-β-lactamases: the quiet before the storm? Clin. Microbiol. Rev. 18: 306– 325 [DOI] [PMC free article] [PubMed] [Google Scholar]